Abstract
The purpose of surgery for adolescent idiopathic scoliosis, which characteristically includes thoracic hypokyphosis and all three columns of the spine, is the achievement of a balanced spine while preserving as many motion segments as possible and avoiding neurologic damage. Many approaches have been defined in the treatment of this common disease. Posterior-only surgery, instrumentation and fusion have become the preferred technique in many centers throughout the world due to simplicity of approach, decreased risk of certain complications and the correction power of pedicle screws. This review attempts to summarize the advantages and disadvantages related to posterior instrumentation and fusion in adolescent idiopathic scoliosis.
Keywords: Idiopathic, Scoliosis, Posterior instrumentation, Deformity, Vertebra, Surgery
Adolescent idiopathic scoliosis (AIS) is a deformity characteristically including thoracic hypokyphosis and a three-dimensional spinal component. Vertebral rotation plays a major part in the development of the deformity and affects treatment choices. When conservative measures fail, surgery is necessary. Indications for surgery include unacceptable deformity causing cosmetic problems and documented curve progression. The factors influencing curve progression have been extensively studied and include curve size at diagnosis, peak growth velocity, curve type, age and sex [1, 2].
The purpose of AIS surgery is the achievement of a balanced spine while avoiding neurologic damage and preserving as many motion segments as possible (Fig. 1a, b). This is performed by fusion of the spine following correction of the deformity. Deformity correction may be performed through an anterior, a posterior or a combined approach, all of which possess their unique advantages and disadvantages. Beginning with Harrington distraction rods introduced in the 1960s, spinal instrumentation has become the mainstay for the achievement of deformity correction. While the Harrington rod provided good correction for the scoliotic segment in the coronal plane, its distraction-based force did not control vertebral rotation and caused the loss of normal sagittal alignment [3, 4]. Cotrel–Dubousset (CD) instrumentation was introduced in the 1980s in order to address limited three-dimensional control of deformity. By achieving segmental purchase in the deformed spine and converting the coronal curve into a physiologic sagittal curve with concave rod derotation, CD instrumentation allowed superior correction and control of sagittal contours [5, 6]. Hooks, the primary anchor implant used in CD instrumentation are easily integrated into the rod system and minimize the risk of root injury. Their insertion, however, is time consuming and by taking up space inside the canal, they pose a risk of spinal injury especially during derotation maneuvering. Reports of hook dislodgement and unloading during derotation maneuvers have also been published [7].
Fig. 1.
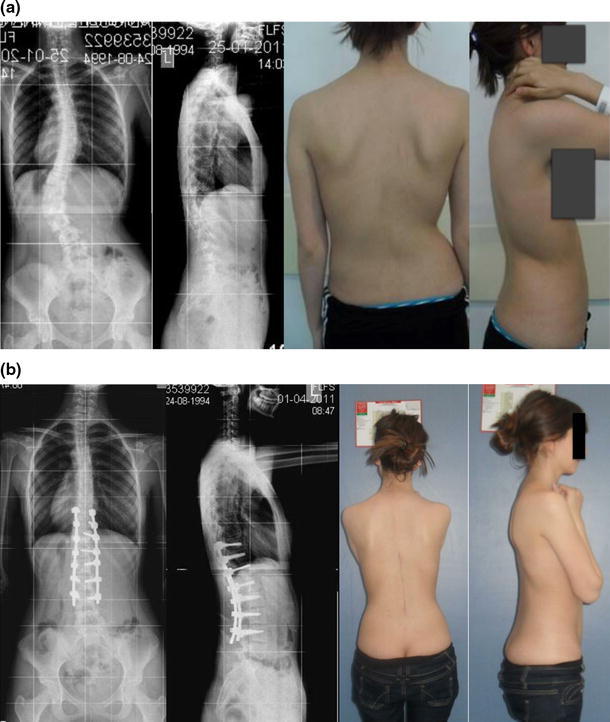
a, b 16 year-old girl with Lenke type 5CN adolescent idiopathic scoliosis. Instrumentation of only the structural curve using a posterior approach was sufficient for the nonstructural curve to correct spontaneously. Postoperative images show excellent correction and overall alignment
Pedicle screws have revolutionized spinal instrumentation by allowing secure segmental three-column fixation through the more familiar posterior approach [8, 9] (Fig. 2a, b). Once their use in the thoracic spine and AIS became widespread, pedicle screws have become the mainstay of posterior instrumentation, providing better and more stable purchase in the bone compared to hooks which led to increased rates of correction. Bilateral segmental instrumentation increases the rigidity of the construct and may increase correction rates and be used safely in severe curves [10–12]. The average operative stats and blood loss for pedicle screws have been shown to be similar to hook systems in previous studies. Sagittal contour is also better maintained with the use of pedicle screws. A recent study has also shown that pedicle screws increased scores in functional outcome measures, contrary to previous studies where no positive effect of screw use was found on patients’ subjective satisfaction [13].
Fig. 2.
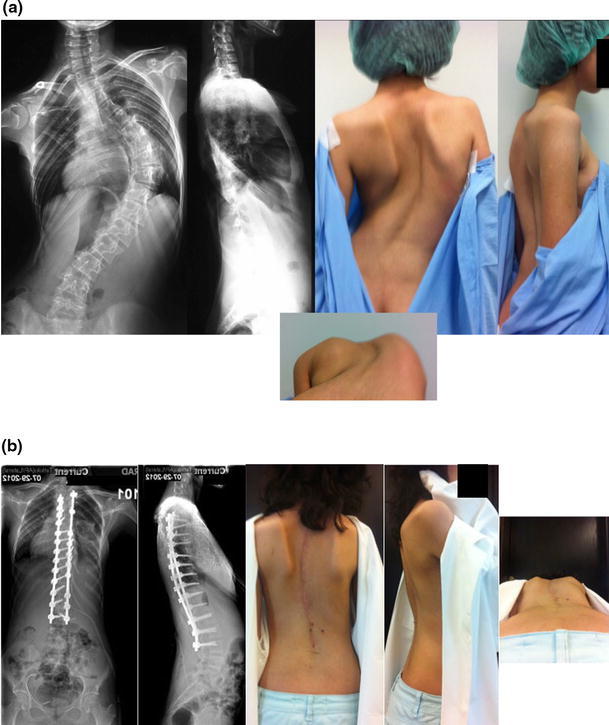
a, b 15 year-old girl with Lenke type1B- adolescent idiopathic scoliosis. Patient has a very prominent preoperative right thoracic hump which required thoracoplasty despite derotation and correction using a pedicle screw-only construct. Postoperative images show excellent alignment
Screw-based posterior segmental instrumentation has multiple anchorage points throughout the spine, all of which span the three columns of the spine by entering from the posterior elements and traveling through the pedicle to purchase the anterior half of the vertebral body. This allows for increased control at the apex of the deformity (Fig. 3a, b). By reducing the spine to a pre-contoured rod with physiological sagittal contours, correction is achieved without the need for distraction.
Fig. 3.
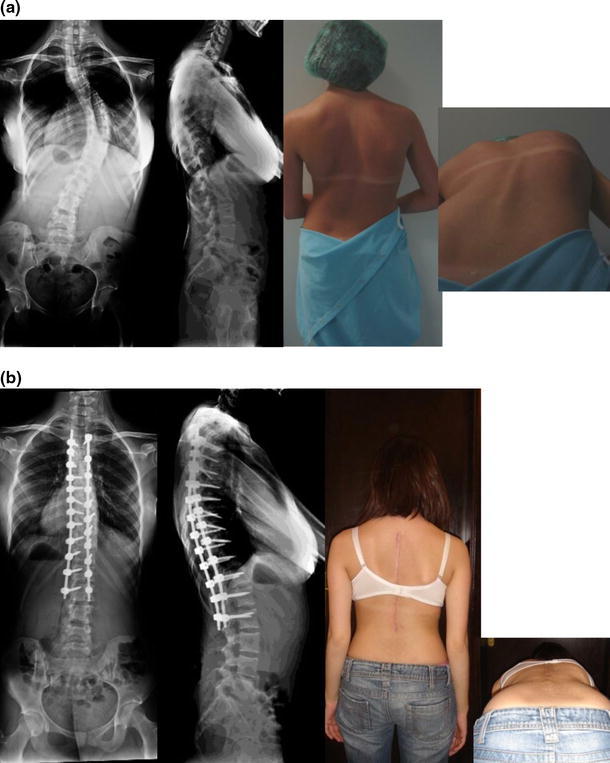
a, b 14 year-old girl with Lenke type 1AN adolescent idiopathic scoliosis. Note the prominent right thoracic hump preoperatively. Posterior-only surgery was performed using a pedicle screw-only construct. Note correction of thoracic hump without the need for thoracoplasty. This indicates three-column fixation and successful derotation using pedicle screws
Types of posterior instrumentation include all-hook, all-pedicle screw and hybrid systems. The biomechanical properties of all have been extensively studied and all-pedicle screw constructs have consistently achieved better results when compared to hook and hybrid systems.
Anterior versus posterior surgery
The posterior approach has many advantages. Aside from being a simple exposure where the operative field is easily reached with little risk of neurovascular compromise, it provides a good control of the sagittal plane of the spinal column. As there is no violation of the thoracic cage under normal circumstances, pulmonary functions are preserved. By allowing the use of direct vertebral rotation and in situ contouring, coronal plane deformity is addressed more thoroughly and the hump well-controlled. Despite its advantages, the posterior approach does have its drawbacks as well. The posterior musculature is violated and due to the lack of soft tissue coverage at this location, infection rates are higher than those of the anterior approach. Another drawback that should be mentioned is that the posterior-only approach requires the inclusion of more motion segments for the achievement of the same correction when compared with the anterior approach.
Techniques for deformity correction in the posterior approach start with proper patient positioning and include compression/distraction, rod rotation, translation, cantilever reduction and direct vertebral rotation with or without in situ contouring. Although not commonly encountered, very severe and rigid curves may require additional interventions in order to increase their flexibility, ranging from a spectrum of discectomy to Chevron/Ponte osteotomies and posterior vertebral column resection. Halo-gravity traction is another important adjunct to the surgical treatment of severe, rigid or neglected curves.
Type of approach and pulmonary function
Scoliosis as a disorder has been shown to impair pulmonary function by itself. While the anterior approach using a thoracotomy has been reported to lead to a need for shorter instrumentation and fusion, less blood loss and better correction of compensatory curves, its negative effect on remains a significant disadvantage. Although the correction of deformity should at least theoretically cause an improvement in pulmonary function, the surgical technique chosen still plays a major role in the postoperative course of the patient.
The reported effect of Harrington posterior spinal fusion on pulmonary function has been variable, from postoperative improvement to a decline in pulmonary function, which was addressed by the meta-analysis by Kinnear and Johnston in 1993, where the authors concluded that Harrington instrumentation leads to a small but statistically significant improvement in vital capacity. Studies evaluating the effect of current posterior spinal fusion with modern segmental implants have shown consistently improved pulmonary functions [14, 15].
The effects of four surgical approaches (posterior fusion only, posterior fusion with thoracoplasty, thoracoscopic anterior fusion and open anterior thoracolumbar fusion) on pulmonary function in AIS patients have been studied before. The return of pulmonary function to preoperative baseline did not occur for at least 3 months for any approach where the chest cage was violated (anterior, thoracoscopic or posterior with thoracoplasty) while the posterior fusion-only group never demonstrated any significant difference from baseline at any point in follow-up. The authors of this study concluded that approaches that violate the chest wall demonstrate a significant decline in postoperative pulmonary function [16]. Others have reported that any kind of chest cage violation, including posterior thoracoplasty, give rise to a significant decline in the percent-predicted value of pulmonary functions at a 5-year follow up [14].
In a 2011 paper by Gitelman et al. [17] the authors reported on the pulmonary function in AIS relative to the surgical procedure after a 10-year follow-up. Patients who had some form of chest wall violation demonstrated a significant decrease in FVC and FEV(1) values while the posterior spinal fusion group showed significant increase in both values. The authors concluded that intraoperative chest wall violation resulted in reduced percent-predicted values at 10 year follow-up.
Video-assisted thoracoscopy presents an alternative to the traditional anterior approach where it is hoped that the disadvantage of a large thoracic incision can be avoided. The VATS has gained popularity in the treatment of curves appropriate for anterior instrumentation alone and several studies regarding its effects have been done. Compared to anterior or posterior spinal fusion, VATS procedures showed an initial decline in pulmonary function, which resolved fully at 12 months follow-up [18]. However, long-term data regarding VATS is still lacking in the literature.
The mechanism with which anterior surgery causes pulmonary compromise has been theorized to include increases in chest cage stiffness, impairment of diaphragmatic movement on the thoracotomy side, nonunion and uneven air distribution following surgery [14]. While these do improve with time, numerous studies have reported significant decline in longer-term follow up .
Type of approach and the capability for correction
However, the anterior approach is not without its merits. As mentioned before, due to the ease of access to the anterior elements of the spine, releases are performed more readily, leading to better correction with shorter fusion and instrumentation, which in turn leads to a decrease in cost. As the anterior instrumentation does not employ distraction on the posterior elements of the spine, thoracic kyphosis is also said to be better preserved [19–21]. However, radiographic and clinical outcomes of both approaches have been comparable in the past.
Betz et al. [22] in a 1999 multicenter prospective study compared AIS patients, 78 of whom were operated on using anterior instrumentation and 100 of whom were operated on using posterior segmental hook instrumentation. Coronal correction rates were similar (58 % anterior vs. 59 % posterior), in the two groups while hyperkyphosis was a more commonly encountered complication in the anterior instrumentation group. Also, an average of 2.5 fewer segments were instrumented in the anterior group. The anterior group did suffer a higher amount of complications (pseudoarthrosis, loss of correction and implant failure).
In a 2009 study by Davis, a decision analysis was performed by using a model based on current literature [23]. In this study, posterior-alone surgery was compared with anterior-posterior combined surgery from a postoperative curve progression angle. The results of this model showed that anterior/posterior combined surgery was the preferred technique for treating skeletally immature female patients. However, the author advised future observational studies as the data used in this particular study was based on outdated surgical instrumentation (i.e. no pedicle screw constructs).
In another study, Dobbs et al. [24] retrospectively analyzed data of AIS patients with curves exceeding 90° who were treated with either a combined anterior/posterior spinal fusion (20 patients) or a posterior spinal fusion alone (34 patients). Correction rates were found to be similar between the two groups while the posterior group showed less of a negative effect on pulmonary function. No reoperations or complications were observed in either group. The authors concluded that all-pedicle screw constructs in such challenging curves have the advantage of providing the same correction without the need for entering the thorax and negatively impacting pulmonary function.
Type of approach and sagittal plane restoration
Rhee et al. [25] compared the effects of anterior versus posterior instrumentation on sagittal plane parameters by evaluating 110 consecutive patients who underwent surgery for AIS with a minimum of 24 month follow-up, 50 of whom underwent anterior surgery with single screw-rod constructs and 60 of whom were instrumented posteriorly with segmental implants. At final follow-up, proximal junctional measurement was found to increase most with posterior instrumentation, while kyphosis increased significantly with anterior instrumentation and lumbar lordosis was enhanced with both methods. Thirty-five percent of patients had an increase in proximal junctional measurement of 10°, while 17 % had an increase of 15 %. None of these patients required revision. The authors concluded that while the two methods had differing effects on the sagittal plane, the overall magnitude of these changes was small and if properly performed, both approaches can result in acceptable sagittal profiles. Possibly due to the lack of distraction-based maneuvering in anterior fusion, it has been previously found to be superior in the restoration of thoracic kyphosis in the treatment of adolescent idiopathic scoliosis [26]. However, newer implants such as pedicle screws that provide secure fixation of all three columns abolish the requirement for distraction being the main corrective force and allow for better restoration of sagittal profile.
Type of approach and segment preservation
Selection of the correct levels for fusion is the most important factor that affects results in spinal surgery for idiopathic scoliosis. Inappropriate selection of fusion segments may cause under- or overcorrection of structural and compensatory curves, failure to maintain the correction of the index curve, aggravate compensatory curves that were not included within the fusion and cause trunk imbalance. Previously accepted guidelines for fusion in adolescent idiopathic scoliosis were developed during the era of Harrington instrumentation and are based on the ‘stable’ vertebra in order to place the fusion mass on a stable basis. These guidelines, however, have been revised after the introduction of superior segmental instrumentation systems [27].
In curves where the thoracic component is structural and larger than the lumbar compensatory curve, and if the apical rotation of the lumbar curve is less than Nash-Moe grade II, it has been proposed that a selective fusion may be appropriate [27–30]. The lumbar curve is expected to follow the correction of the thoracic curve, allowing the preservation of up to two motion segments according to the relation between the end vertebra and the neutral vertebra [10]. In a 1999 study by Betz et al. where anterior instrumentation was compared to posterior segmental hook systems, the authors concluded that an average of 2.5 lumbar levels could be saved with the anterior approach and that no anterior fusion was longer than posterior fusion.
Another controversial issue is the termination of fusion in double major curves where the lumbar curve is larger than the thoracic curve and the apical rotation of the lumbar curve is higher than grade II (Lenke type 5 and 6). While it is undoubtedly necessary for both of these curves to be fused, L3 can be chosen as the end vertebra in cases where L3 crosses the central sacral line in side-bending radiographs and there is less than Nash-Moe grade II rotation [10].
Although anterior surgery has consistently been reported to require fewer segments for fusion in selected curve types as compared to posterior-only surgery, Kim et al. [31] have determined in their report comparing similar idiopathic curves operated on with hooks and pedicle screws that pedicle screw instrumentation saved on average 0.8 levels as compared to hook instrumentation.
Potter et al. [32] in a 2005 study compared curve correction and derotation following anterior spinal fusion with posterior spinal fusion with thoracic pedicle screws using a matched patient cohort of Lenke type I curves. They observed that with only one additional spinal segment fused in the posterior group (6.5 vs. 7.7 levels), posterior instrumentation provided superior instrumented correction of main thoracic curves and spontaneous correction of thoracolumbar and lumbar curves. Posterior instrumentation also provided improved correction of thoracic torsion and rotation as compared with anterior surgery.
Type of approach and immaturity
In the presence of open anterior growth plates and isolated posterior fusion, there is a risk of curve progression after surgery following posterior instrumentation alone for adolescent idiopathic scoliosis. Known as the crankshaft phenomenon, it has been suggested that combined anterior-posterior fusion be performed in order to avoid it in patients with greater growth potential remaining. However, pedicle screws with their three-column fixation have been thought to avoid this complication. In a 2012 report by Tao et al. [33] 67 patients with an average of 36-months follow-up were followed for scoliosis progression following isolated posterior instrumentation and fusion with hybrid, interval pedicle screw or consecutive screw constructs. The authors observed that the crankshaft phenomenon occurred in 33 % of hybrid instrumentation patients but in none of the patients where screws alone were used. Consistently good rates of the maintenance of correction in patients where pedicle screws were used in instrumentation can also be viewed as proof that pedicle screws have significantly lowered if not eliminated the risk of crankshaft in adolescent idiopathic scoliosis [32, 34, 35].
Type of approach and curve severity
The traditionally suggested treatment for rigid and severe curves requires anterior release before the application of posterior surgery. However, recent years have seen an increase in reports of posterior-only surgery and good results. The treatment of these deformities have been divided into three stages: anchor placement, mobilization of the spine and correction strategies [36]. The instrumentation preferred for severe rigid curves remains pedicle screws through a posterior approach. The presence of reduction screws with long tulip heads are also a valuable asset during severe curve surgery. Some method of releasing the spine will always be necessary during the surgical treatment of these curves. With the more widespread use of pedicle screws in the thoracic spine, the necessity for performing anterior releases and rib resections has been on the decline [37, 38].
In a 2005 study by Burton et al. [38] the authors retrospectively reviewed 46 patients with idiopathic curves exceeding 70° and treated with isolated posterior instrumentation (third-generation segmental spinal instrumentation consisting of hooks, wires and screws) in order to establish indications for anterior release. The authors reported coronal correction rates of 64 % with low complication rates and favorable surgical statistics. The authors concluded that by using newer implants, isolated posterior instrumentation and fusion can achieve satisfactory cosmetic, radiographic and patient-based outcomes without the added expense and morbidity of anterior release. Also, pedicle screw systems showed significantly better rates of Cobb correction with no significant difference in the number of levels fused in severe curves when compared to patients undergoing combined fusion [37].
Conclusion
It appears that with the introduction of superior fixation systems such as pedicle screws, posterior surgery provides today most, if not all, of the advantages of the anterior approach without the negative effects on pulmonary functions. Regarding sagittal plane restoration, while it cannot be said that posterior surgery has a clear advantage to the anterior approach, it is most certainly not inferior to it. Although older studies have indicated that anterior surgery is superior to conventional posterior techniques, newer research has not encountered such a difference. Also by being easier to perform and with improved correction rates, posterior surgery has gained a clear edge over the anterior approach. However, the slight increased rates of infection and the violation of the posterior musculature remain problems to be solved.
In conclusion, as with most things regarding surgery, both posterior and anterior approaches have their own unique advantages and drawbacks. The correct choice of technique depends, as it always does, on the unique qualities of the curve to be operated on, the equipment and facilities available, the experience and education and, perhaps most importantly, the preference of the surgeon.
References
- 1.Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine (Phila Pa 1976) 1986;11(8):773–776. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1061–1071. [PubMed] [Google Scholar]
- 3.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am Vol. 1962;44:591–610. [PubMed] [Google Scholar]
- 4.Goldstein LA. Treatment of idiopathic scoliosis by Harrington instrumentation and fusion with fresh autogenous iliac bone grafts. J Bone Joint Surg Am Vol. 1969;51(2):209–222. [PubMed] [Google Scholar]
- 5.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10–23. [PubMed] [Google Scholar]
- 6.Labelle H, Dansereau J, Bellefleur C, de Guise J, Rivard CH, Poitras B. Peroperative three-dimensional correction of idiopathic scoliosis with the Cotrel-Dubousset procedure. Spine. 1995;20(12):1406–1409. [PubMed] [Google Scholar]
- 7.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18(6):341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 8.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976) 2001;26(18):2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 9.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine (Phila Pa 1976) 1996;21(10):1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 10.Suk SI. Pedicle screw instrumentation for adolescent idiopathic scoliosis: the insertion technique, the fusion levels and direct vertebral rotation. Clin Orthoped Surg. 2011;3(2):89–100. doi: 10.4055/cios.2011.3.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Margulies JY, Floman Y, Robin GC, et al. An algorithm for selection of instrumentation levels in scoliosis. Eur Spine J Off Pub Eur Spine Soc Eur Spinal Def Soc Eur Sect Cerv Spine Res Soc. 1998;7(2):88–94. doi: 10.1007/s005860050036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Jr, Polly DW, Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine (Phila Pa 1976) 2005;30(2):222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 13.Luhmann SJ, Lenke LG, Erickson M, Bridwell KH, Richards BS. Correction of moderate (<70 degrees) Lenke 1A and 2A curve patterns: comparison of hybrid and all-pedicle screw systems at 2-year follow-up. J Pediatr Orthop. 2012;32(3):253–258. doi: 10.1097/BPO.0b013e3182471c74. [DOI] [PubMed] [Google Scholar]
- 14.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87(7):1534–1541. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 15.Vedantam R, Lenke LG, Bridwell KH, Haas J, Linville DA. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine (Phila Pa 1976) 2000;25(1):82–90. doi: 10.1097/00007632-200001010-00015. [DOI] [PubMed] [Google Scholar]
- 16.Yaszay B, Jazayeri R, Lonner B. The effect of surgical approaches on pulmonary function in adolescent idiopathic scoliosis. J Spinal Disord Tech. 2009;22(4):278–283. doi: 10.1097/BSD.0b013e31816d2530. [DOI] [PubMed] [Google Scholar]
- 17.Gitelman Y, Lenke LG, Bridwell KH, Auerbach JD, Sides BA. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure: a 10-year follow-up analysis. Spine (Phila Pa 1976) 2011;36(20):1665–1672. doi: 10.1097/BRS.0b013e31821bcf4c. [DOI] [PubMed] [Google Scholar]
- 18.Verma K, Lonner BS, Kean KE, Dean LE, Valdevit A. Maximal pulmonary recovery after spinal fusion for adolescent idiopathic scoliosis: how do anterior approaches compare? Spine (Phila Pa 1976) 2011;36(14):1086–1095. doi: 10.1097/BRS.0b013e3182129d62. [DOI] [PubMed] [Google Scholar]
- 19.Lonner BS, Auerbach JD, Estreicher MB, et al. Pulmonary function changes after various anterior approaches in the treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech. 2009;22(8):551–558. doi: 10.1097/BSD.0b013e318192d8ad. [DOI] [PubMed] [Google Scholar]
- 20.Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2006;88(5):1022–1034. doi: 10.2106/JBJS.E.00001. [DOI] [PubMed] [Google Scholar]
- 21.Verma K, Auerbach JD, Kean KE, Chamas F, Vorsanger M, Lonner BS. Anterior spinal fusion for thoracolumbar scoliosis: comprehensive assessment of radiographic, clinical, and pulmonary outcomes on 2-years follow-up. J Pediatr Orthop. 2010;30(7):664–669. doi: 10.1097/BPO.0b013e3181ec931b. [DOI] [PubMed] [Google Scholar]
- 22.Betz RR, Harms J, Clements DH, 3rd, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24(3):225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 23.Davis MA. Posterior spinal fusion versus anterior/posterior spinal fusion for adolescent idiopathic scoliosis: a decision analysis. Spine (Phila Pa 1976) 2009;34(21):2318–2323. doi: 10.1097/BRS.0b013e3181adb296. [DOI] [PubMed] [Google Scholar]
- 24.Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine (Phila Pa 1976) 2006;31(20):2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 25.Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine (Phila Pa 1976) 2002;27(21):2350–2356. doi: 10.1097/00007632-200211010-00008. [DOI] [PubMed] [Google Scholar]
- 26.Sucato DJ, Agrawal S, O’Brien MF, Lowe TG, Richards SB, Lenke L. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine (Phila Pa 1976) 2008;33(24):2630–2636. doi: 10.1097/BRS.0b013e3181880498. [DOI] [PubMed] [Google Scholar]
- 27.Lenke LG, Betz RR, Bridwell KH, Harms J, Clements DH, Lowe TG (1999) Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine 24(16):1663–1671; discussion 1672 [DOI] [PubMed]
- 28.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20(12):1399–1405. [PubMed] [Google Scholar]
- 29.Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine. 2003;28(5):484–491. doi: 10.1097/01.BRS.0000048653.75549.40. [DOI] [PubMed] [Google Scholar]
- 30.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am Vol. 1983;65(9):1302–1313. [PubMed] [Google Scholar]
- 31.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29(18):2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 32.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curves. Spine (Phila Pa 1976) 2005;30(16):1859–1866. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 33.Tao F, Zhao Y, Wu Y, et al. The effect of differing spinal fusion instrumentation on the occurrence of postoperative crankshaft phenomenon in adolescent idiopathic scoliosis. J Spinal Disord Tech. 2010;23(8):e75–e80. doi: 10.1097/BSD.0b013e3181d38f63. [DOI] [PubMed] [Google Scholar]
- 34.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20(12):1399–1405. [PubMed] [Google Scholar]
- 35.Rose PS, Lenke LG, Bridwell KH et al (2009) Pedicle screw instrumentation for adult idiopathic scoliosis: an improvement over hook/hybrid fixation. Spine 34(8):852–857; discussion 858 [DOI] [PubMed]
- 36.Sucato DJ. Management of severe spinal deformity: scoliosis and kyphosis. Spine (Phila Pa 1976) 2010;35(25):2186–2192. doi: 10.1097/BRS.0b013e3181feab19. [DOI] [PubMed] [Google Scholar]
- 37.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976) 2005;30(18):2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 38.Burton DC, Sama AA, Asher MA, et al. The treatment of large (>70 degrees) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: when is anterior release indicated? Spine (Phila Pa 1976) 2005;30(17):1979–1984. doi: 10.1097/01.brs.0000176196.94565.d6. [DOI] [PubMed] [Google Scholar]


