Abstract
Adolescent idiopathic scoliosis is a common disease with an overall prevalence of 0.47–5.2 % in the current literature. The female to male ratio ranges from 1.5:1 to 3:1 and increases substantially with increasing age. In particular, the prevalence of curves with higher Cobb angles is substantially higher in girls than in boys: The female to male ratio rises from 1.4:1 in curves from 10° to 20° up to 7.2:1 in curves >40°. Curve pattern and prevalence of scoliosis is not only influenced by gender, but also by genetic factors and age of onset. These data obtained from school screening programs have to be interpreted with caution, since methods and cohorts of the different studies are not comparable as age groups of the cohorts and diagnostic criteria differ substantially. We do need data from studies with clear standards of diagnostic criteria and study protocols that are comparable to each other.
Keywords: Epidemiology, Adolescent idiopathic scoliosis, Prevalence, Scoliosis, School screening
Introduction
The term “scoliosis” derives from the ancient Greek word “skolios” (curved, crooked) and was first established by Galen (130–201 AD).
Scoliosis is the most common spinal disorder in children and adolescents. A scoliosis is characterized by a side-to-side curvature of the spine >10°, usually combined with a rotation of the vertebrae and most often a reduced kyphosis in thoracic curves [1].
Scoliosis patients are classified in different types according to age of onset, etiology, severity and type of curve. Each type shows different characteristics as rate of curve progression, degree and pattern of the three-dimensional deformity. High rate of curve progression and early onset of scoliosis are negative predictive parameters for a poor outcome in idiopathic scoliosis like a thoracic insufficiency syndrome [2].
The two major groups of scoliosis are idiopathic scoliosis and non-idiopathic scoliosis. The diagnosis of an idiopathic scoliosis is made if a non-idiopathic one has been excluded.
Non-idiopathic scoliosis is classified into the following subgroups:
Congenital scoliosis:
Congenital scoliosis is caused by malformation of vertebrae like hemivertebra, unilateral bar or block vertebra (Fig. 1). It may not be clinically evident at birth but develops until adolescence [3]. Genes that are associated with vertebral malformation have been identified in several studies [4–6], and similar defects have been induced in animal models by hypoxia or toxic agents [7, 8].
Fig. 1.
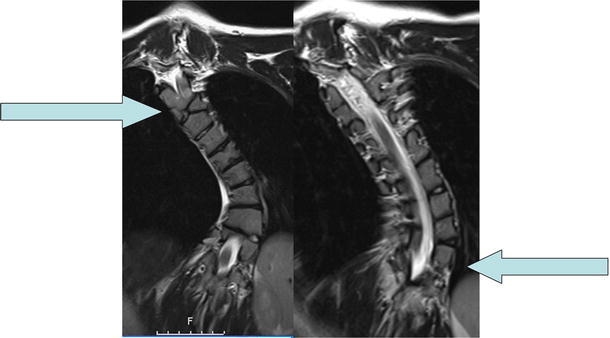
MRI of the spine of a patient with a congenital scoliosis. The arrows indicate malformations of vertebra (hemivertebra, butterfly vertebra)
Neuromuscular scoliosis:
Neuromuscular scoliosis is caused by insufficiency of active (muscular) stabilizers of the spine, like in cerebral palsy, spinal muscular atrophy, spina bifida, muscular dystrophies or spinal cord injuries.
Surgical treatment of neuromuscular scoliosis is associated with the highest rate of complications compared to other types of scoliosis [9].
Mesenchymal scoliosis:
Mesenchymal scoliosis is caused by insufficiency of passive stabilizers of the spine, like in Marfan’s syndrome, mucopolysaccharidosis, osteogenesis imperfecta, inflammatory diseases or postoperative after thoracic surgery (open heart surgery).
Idiopathic scoliosis is classified into the following subgroups:
Infantile scoliosis:
Infantile scoliosis develops at the age of 0–3 years and shows a prevalence of 1 %. Mau and McMaster [10, 11] report about a radical decrease in number of infantile scoliosis in The 1980s, probably related to the recommendation of prone position for the infants. McMaster and Diedrich [11, 12] describe that, in contrast to adolescent idiopathic scoliosis (AIS), there is a regression of scoliosis in more than half of the cases. Mehta [13] described the rib–vertebra angle difference and identified that an angle difference of more than 20° indicates a poor prognosis and rapid progression.
Juvenile scoliosis:
Juvenile scoliosis develops at the age of 4–10 years and comprises 10–15 % of all idiopathic scoliosis in children [14], untreated curves may cause serious cardiopulmonary complications, and curves of 30° and more tend to progress, 95 % of these patients need a surgical procedure [14].
Adolescent scoliosis:
Adolescent scoliosis develops at the age of 11–18 years and accounts for approximately 90 % of cases of idiopathic scoliosis in children (Fig. 2).
Fig. 2.
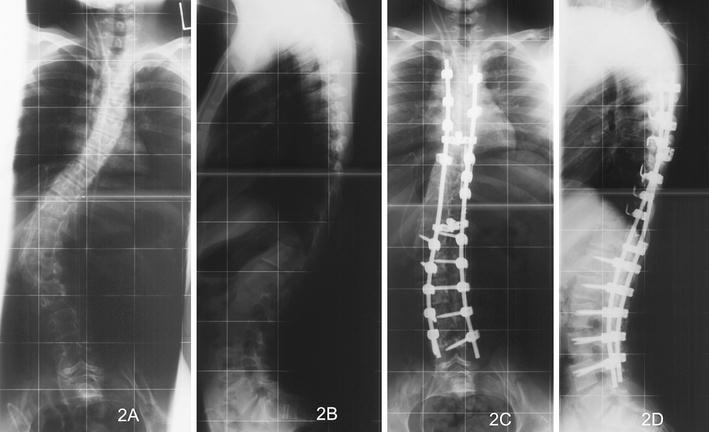
16-year-old female patient with an adolescent idiopathic scoliosis. a, b Preoperative Cobb angle 50°, c, d Postoperative Cobb angle 10°
Adult scoliosis (de novo scoliosis in adults):
Scoliosis has a prevalence of more than 8 % in adults over the age of 25 and rises up 68 % in the age of over 60 years, caused by degenerative changes in the aging spine [15, 16].
In this article we present an overview on reported data on epidemiology of AIS with special attention to prevalence and rate of curve progression according to race, age of onset, gender, and severity of scoliosis.
Prevalence of AIS
Overall prevalence
There are not many studies that provide data of high relevance regarding prevalence of AIS. Several studies that do provide such data have substantial weaknesses like varying definitions of scoliosis, study protocols, and age-groups, missing standards for comparison and inclusion of curves <10°, although international consensus is given that per definition scoliosis is a deformity ≥10°.
The study of Kamtsiuris [17] was conducted in Germany by the Robert Koch Institute (RKI). 17,641 children (8,656 girls, 8,995 boys) were interviewed and examined for chronicle diseases, children from 0 to 17 years participated.
The study of Suh [18] was conducted in Korea. 1,134,890 children participated (584,554 boys and 550,336 girls). Two age groups were investigated: 10–12 years and 13–14 years.
The study of Nery [19] was conducted in Brasil. 1,340 children participated (684 boys, 656 girls). Mean age was 12.7 years.
The study of Daruwalla [20] was conducted in Singapore. 110,744 children were examined (60,167 girls, 50,577 boys). Three age groups were investigated: 6–7, 11–12 and 16–17 years (only girls were investigated in the last group).
Twenty years later Wong [21] conducted another study in Singapore and investigated 72,699 children (37,141 girls and 35,558 boys).
The study of Cilli [22] was conducted in Turkey. 3,175 children participated (1,538 girls, 1,637 boys). Children from 10 to 15 years were enrolled.
The study of Soucacos [23] was conducted in Greece. 82,901 children participated (41,939 boys and 40,962 girls). Children from 9 to 14 years were enrolled.
Data from these studies indicate a prevalence of 0.47–5.2 % for AIS. (Table 1).
Table 1.
| Study | Country | Children | Girls | Boys | Age (years) | Prevalence combined (%) | Prevalence girls % | Prevalence boys % |
|---|---|---|---|---|---|---|---|---|
| Kamtsiuris [17] | Germany | 17,641 | 8,656 | 8,995 | 0–17 | 5.2 | 6.0 11–13 years:8.3 14–17 years:13.5 |
4.4 11–13 years: 5.0 14–17 years:9.0 |
| Daruwalla [20] | Singapore | 110,744 | 60,167 | 50,577 | 6–7 11–12 16–17 |
1.0 | 6–7 years: 0.15 11–12 years: 1.67 16–17 years:3.12 |
6–7 years: 0.10 11–12 years: 0.44 16–17 years: not tested |
| Wong [21] | Singapore | 72,699 | 37,141 | 35,558 | 6–7 9–10 11–12 13–14 |
0.59 | 6–7 years: 0.05 9–10 years: 0.24 11–12 years: 1.37 13–14 years: 2.22 |
6–7 years: 0.02 9–10 years: 0.15 11–12 years: 0.21 13–14 years: 0.66 |
| Nery [19] | Brasil | 1,340 | 684 | 656 | 10–14 | 1.4 | 1.98 | 0.87 |
| Suh [18] | Korea | 1,134,890 | 550,336 | 584,554 | 10–12 13–14 |
3.26 | 4.65 | 1.97 |
| Cilli [22] | Turkey | 3,175 | 1,538 | 1,637 | 10–15 | 0.47 | 0.65 | 0.31 |
| Soucacos [23] | Greece | 82,901 | 40,962 | 41,939 | 9–14 | 1.7 | 2.6 | 0.9 |
Comparing these results prevalence to the prevalence of measles (7.4 %) and mumps (4.0 %) [17], it is obvious that AIS is a common disease in children (we have to consider that the actual prevalence of measles and mumps in Germany is substantially diminished by vaccination).
Prevalence according to “race”/genetic factors
Genetic factors do influence the incidence [24] and progression [25] of scoliosis. 97 % of AIS patients are related to other family members with AIS [26], in Prader–Willi syndrome patients, scoliosis is found up to 40 % [27]. The influence of genetic factors in scoliosis is also apparent in epidemiologic studies:
Kamtsiuris et al. [17] found a higher prevalence of scoliosis in German children (5.5 %) than among immigrant children (3.5 %). That difference in prevalence can be attributed to genetic factors and not to malnutrition or other factors like a lower social status, because children of families of a high or middle social status had a higher prevalence (6.2 % high status, 5.6 % middle status) than children of a lower social status (3.5 %).
Ratahi et al. [28] described that AIS is more frequent in Europeans than in Polynesians, and that scoliosis secondary to syringomyelia is more frequent in Polynesians than in Europeans.
A study that investigated pupils in Singapore [20] found a higher prevalence for Chinese girls than for Malay and Indian girls.
Carter [15] described a higher prevalence of scoliosis in the Afroamerican population (9.7 %) than in the Caucasian population (8.1 %). As he investigated the adult population, his findings are of a lower relevance for AIS.
Prevalence according to age
Daruwalla [20] found a higher prevalence for adolescents than for young children: 0.12 % in the 6–7 years-group, 1.0 % in the 11–12 years group and 3.12 % in the 16–17 years group (only girls investigated in the latter group). Cilli [22] did not find any significant relationship of the curvature with age groups, but they investigated only children from 10 to 15 years. In Germany Kamtsiuris [17] found a prevalence of 6.5 % in the age of 11–13 years and a prevalence of 11.1 % in the age of 14–17 years.
These data indicate a higher prevalence of scoliosis in patients older than 15 years (after puberty).
Prevalence according to gender
Kamtsiuris [17] found a prevalence ratio of 1.5:1, with slight increase with age (Table 1). Daruwalla [20] found a prevalence ratio female to male of 2:1, rising up to 3:1 in the age of 11–12 years. Cilli [22] and Nery [19] found a prevalence ratio of 2:1 without differentiation of different age groups. These data indicate an overall prevalence ratio of 2:1 female to male with an increase with age.
Gender and severity:
Prevalence does not seem to be the only character of scoliosis that is influenced by gender: Several studies [18, 20, 29–31] report about higher Cobb angels in girls than in boys (Table 2), indicating that scoliosis in girls progresses to a higher grade of severity. For patients with a Cobb angle of more than 30° the prevalence ratio gets as high as 10:1 [23, 32–37]. The prevalence of severe scoliosis is much higher for girls than for boys; however, Weijun [38] reports a higher prevalence of atypical curve types in boys with Cobb angles of more than 20° than in girls, and a higher risk of progression in the main thoracic right convex curve.
Table 2.
| Cobb angle of curve | Prevalence (%) | Female:male ratio |
|---|---|---|
| 11°–20° | 1.5–3 | 1.4:1 |
| 21°–40° | 0.2–0.5 | 2.8–5.4:1 |
| >40° | 0.04–0.3 | 7.2:1 |
The overall prevalence of different grades of severity is given in table 2.
Curve types
Overall prevalence of different curve types:
Thoracic curves are the most common (48 %), followed by thoracolumbar/lumbar curves (40 %). Double curves (9 %) and double thoracic curves (3 %) are less common [18]. 80 % of all children have thoracic or thoracolumbar/lumbar curves [18].
Curve type according to gender:
Boys have a higher proportion of thoracolumbar/lumbar curves, girls have a higher prevalence of thoracic and double curves [18] (Table 3).
Table 3.
Prevalence of different curve types according to gender [18]
| Curve type | Thoracic | Thoracolumbar/lumbar | Double | Double thoracic |
|---|---|---|---|---|
| Prevalence boys % | 44.06 | 49.55 | 4.26 | 2.14 |
| Prevalence girls % | 49.10 | 36.09 | 11.10 | 3.71 |
Curve type according to age:
Infantile scoliosis (0–3 years) has a much higher prevalence of left sided curves (56–88 %) than adolescent scoliosis [39–41]; in juvenile idiopathic scoliosis the left and right sides curves are evenly divided [42, 43]. Janssen [44] investigated the reason for that distribution of curve types: he found a pattern of pre-existent vertebral rotation in the normal spine that depends on age. In the infantile age, rotation is predominantly to the left, in the adolescent age it is to the right, and in the juvenile age there is no predominant rotation to either side. These results [44] match the curve direction of scoliosis in infantile, juvenile and adolescent scoliosis.
Discussion
Present data show an overall prevalence of AIS of 0.47–5.2 %. The prevalence and severity of scoliosis is higher in girls than in boys. All data were obtained by school screening, and yet school screening is the most effective method for creating epidemiological data of adolescent scoliosis. However, school screening programs have many limitations which have been well described by Fong et al. [45]: The overall positive predictive value for detecting curves ≥10° and ≥20° were low, indicating that school screening has not been conducted effectively, and they showed a high heterogeneity of study designs across all screening programmes [45]. They also investigated the effectiveness of the Adams forward-bending test [46] and concluded that it was very low! If additional tests like angle of trunk rotation or Moiré topography were used, the effectiveness of screening could be improved, but so far no test could produce substantial benefit with a sufficient level of evidence [45].
Main individual limitations of the screening studies we cited:
Kamtsiuris [17] provided very good epidemiologic data, but they did not provide exact criteria of diagnosis of scoliosis. It also remains unclear who established the diagnosis of scoliosis: General practitioner or orthopedic surgeon.
Cilli [22] and Nery [19] only investigated children in the age range of 10–15 years, excluding important other age groups.
The lower prevalence of scoliosis in the study of Cilli [22] could be related to the age group investigated: They enrolled children from 10 to 15 years, whereas Daruwalla [20] showed that the highest prevalence of scoliosis is in girls that are older than 15 years. Kamtsiuris [17] also found highest prevalence in children of 14–17 years. Daruwalla [20] did only investigate age groups (6–7, 11–12 and 16–17 years) and they only enrolled females in the group of 16–17 years, and Suh [18] investigated only two age groups (10–12 and 13–14 years). Wong [21] also enrolled only children from 9 to 14 years and included curves <10°. The other epidemiologic studies mentioned above also did not explicitly exclude curves <10°.
Soucacos [23] conducted a very good study in Greece, describing his exact parameters for diagnosis of scoliosis. All listed epidemiologic studies used the Adams forward-bending test [46] for primary screening and performed radiologic diagnostics only when this test was positive, but Soucacos [23] was the only one who explicitly had the school screening tests performed by orthopedic surgeons, and not by nurses or other non-academic medical staff, diminishing the bias of his results.
However, the limitation of his study is again the investigated age group (9–14 years), excluding older adolescent children.
Investigation of comparable age groups is difficult because of differences in culture and school systems in the individual countries. In Singapore, for example, in the age group of 16–17 years there are only girls at school because the boys have to attend military service at that age [20].
Another bias mentioned in nearly all epidemiologic studies is that they do not consider the psychological impact of scoliosis on children, although it has been described extensively in current literature [47–49]. Young girls particularly, but also boys, that have deformities might feel embarrassed when being examined in school. When these children fall “ill” because of this embarrassment or beg their parents to refuse the examination and miss the school screening, a substantial bias is the consequence. Only one study [23] deals with that important potential bias and describes how the children are prepared psychologically for the examination and how fears and anxieties are dealt with.
Conclusion
Idiopathic adolescent scoliosis is a common disease with a prevalence of 0.47–5.2 %. Prevalence and curve severity are higher for girls than for boys, and the female to male ratio increases with increasing age of the children.
The current epidemiologic data have to be interpreted with caution since methods and cohorts of the existing studies are not comparable.
References
- 1.Grivas TB, Vasiliadis E, Chatzizrgiropoylos T, Polyzois VD, Gatos K. The effect of a modified Boston Brace with antirotatory blades on the progression of curves in idiopathic scoliosis: aetiologic implications. Pediatr Rehabil. 2003;6:237–242. doi: 10.1080/13638490310001636808. [DOI] [PubMed] [Google Scholar]
- 2.Campbell RM, Jr, Hell-Vocke AK. Growth of the thoracic spine in congenital scoliosis after expansion thoracoplasty. J Bone Joint Surg Am. 2003;85-A(3):409–420. doi: 10.2106/00004623-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Master Mc. Congenital scoliosis. In: Weinstein SL, editor. The pediatric spine: principles and practices. New York: Raven Press; 1994. pp. 227–244. [Google Scholar]
- 4.Bulman MP, Kusumi K, Frayling TM, et al. Mutations in the human delta homologue, DLL3, cause axial skeletal defects in spondylocostal dysostosis. Nat Genet. 2000;24:438–441. doi: 10.1038/74307. [DOI] [PubMed] [Google Scholar]
- 5.Li L, Krantz ID, Deng Y, et al. Alagille syndrome is caused by mutations in human jagged 1, which encodes a ligand for Notch 1. Nat Genet. 1997;16:243–251. doi: 10.1038/ng0797-243. [DOI] [PubMed] [Google Scholar]
- 6.Oda T, Elkahloun AG, Pike BL, et al. Mutations in the human jagged1 gene are responsible for Alagille syndrome. Nat Genet. 1997;16:235–242. doi: 10.1038/ng0797-235. [DOI] [PubMed] [Google Scholar]
- 7.Ingalls TH, Curley FJ. Principles governing the genesis of congenital malformations induced in mice by hypoxia. N Engl J Med. 1957;257:1121–1127. doi: 10.1056/NEJM195712052572306. [DOI] [PubMed] [Google Scholar]
- 8.Loder RT, Hernandez MJ, Lerner AL, et al. The induction of congenital spinal deformities in mice by maternal carbon monoxide exposure. J Pediatr Orthop. 2000;20:662–666. doi: 10.1097/01241398-200009000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Reames DL, Smith JS, Fu KM, Polly DW, Jr, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp RD, Jr, Heary R, Shaffrey CI, Scoliosis Research Society Morbidity and Mortality Committee Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 2011;36(18):1484–1491. doi: 10.1097/BRS.0b013e3181f3a326. [DOI] [PubMed] [Google Scholar]
- 10.Mau H. The changing concept of infantile scoliosis. Int Orthop. 1981;5:131–137. doi: 10.1007/BF00267843. [DOI] [PubMed] [Google Scholar]
- 11.McMaster M. Infantile idiopathic scoliosis: can it be prevented? J Bone Joint Surg Br. 1983;65:612–617. doi: 10.1302/0301-620X.65B5.6643567. [DOI] [PubMed] [Google Scholar]
- 12.Diedrich O, von Strempel A, Schloz M, et al. Long-term observation and management of resolving infantile scoliosis. J Bone Joint Surg Br. 2002;84:1030–1103. doi: 10.1302/0301-620X.84B7.13005. [DOI] [PubMed] [Google Scholar]
- 13.Mehta MH. The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg Br. 1972;54(2):230–243. [PubMed] [Google Scholar]
- 14.Coillard C, Circo AB, Rivard CH (2010) SpineCor treatment for juvenile idiopathic scoliosis: SOSORT award 2010 winner. Scoliosis 5:25 [DOI] [PMC free article] [PubMed]
- 15.Carter OD, Haynes S. Prevalence rates for scoliosis in US adults: results from the first national health and nutrition examination survey. Int J Epidemiol. 1987;16:537–544. doi: 10.1093/ije/16.4.537. [DOI] [PubMed] [Google Scholar]
- 16.Schwab F, Ashok D, Lorenzo G, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30:1083–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 17.Kamtsiuris P, Atzpodien K, Ellert U, Schlack R, Schlaud M. Prevalence of somatic diseases in German children and adolescents. Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50(5–6):686–700. doi: 10.1007/s00103-007-0230-x. [DOI] [PubMed] [Google Scholar]
- 18.Suh SW, Modi HN, Yang JH, Hong JY. Idiopathic scoliosis in Korean schoolchildren: a prospective screening study of over 1 million children. Eur Spine J. 2011;20(7):1087–1094. doi: 10.1007/s00586-011-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nery LS, Halpern R, Nery PC, Nehme KP, Stein AT. Prevalence of scoliosis among school students in a town in southern Brazil. Sao Paulo Med J. 2010;128(2):69–73. doi: 10.1590/S1516-31802010000200005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daruwalla JS, Balasubramaniam P, Chay SO, Rajan U, Lee HP. Idiopathic scoliosis. Prevalence and ethnic distribution in Singapore schoolchildren. J Bone Joint Surg Br. 1985;67(2):182–184. doi: 10.1302/0301-620X.67B2.3980521. [DOI] [PubMed] [Google Scholar]
- 21.Wong HK, Hui JH, Rajan U, Chia HP. Idiopathic scoliosis in Singapore schoolchildren: a prevalence study 15 years into the screening program. Spine (Phila Pa 1976) 2005;30(10):1188–1196. doi: 10.1097/01.brs.0000162280.95076.bb. [DOI] [PubMed] [Google Scholar]
- 22.Cilli K, Tezeren G, Taş T, Bulut O, Oztürk H, Oztemur Z, Unsaldi T. School screening for scoliosis in Sivas, Turkey. Acta Orthop Traumatol Turc. 2009;43(5):426–430. doi: 10.3944/AOTT.2009.426. [DOI] [PubMed] [Google Scholar]
- 23.Soucacos PN, Soucacos PK, Zacharis KC, Beris AE, Xenakis TA. School-screening for scoliosis. A prospective epidemiological study in northwestern and central Greece. J Bone Joint Surg Am. 1997;79(10):1498–1503. doi: 10.2106/00004623-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Wynne-Davies R. Familial (idiopathic) scoliosis. A family survey. J Bone Joint Surg Br. 1968;50:24–30. [PubMed] [Google Scholar]
- 25.Ward K, Ogilvie JW, Singleton MV, Chettier R, Engler G, Nelson LM (2010) Validation of DNA-based prognostic testing to predict spinal curve progression in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35(25):E1455–1464 [DOI] [PubMed]
- 26.Ogilvie JW, Braun J, Argyle V, Nelson L, Meade M, Ward K. The search for idiopathic scoliosis genes. Spine (Phila Pa 1976) 2006;31(6):679–681. doi: 10.1097/01.brs.0000202527.25356.90. [DOI] [PubMed] [Google Scholar]
- 27.Nakamura Y, Nagai T, Iida T, Ozeki S, Nohara Y. Epidemiological aspects of scoliosis in a cohort of Japanese patients with Prader-Willi syndrome. Spine J. 2009;9(10):809–816. doi: 10.1016/j.spinee.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 28.Ratahi ED, Crawford HA, Thompson JM, Barnes MJ. Ethnic variance in the epidemiology of scoliosis in New Zealand. J Pediatr Orthop. 2002;22(6):784–787. [PubMed] [Google Scholar]
- 29.Lonstein JE, Bjorklund S, Wanninger MH. Voluntary school screening for scoliosis in Minnesota. J Bone Joint Surg (Am) 1982;64:481–488. [PubMed] [Google Scholar]
- 30.Rogala EJ, Drummond DS, Gurr J. Scoliosis: incidence and natural history. A prospective epidemiological study. J Bone Joint Surg Am. 1978;60(2):173–176. [PubMed] [Google Scholar]
- 31.Asher M, Green P, Orrick J. A six-year report: spinal deformity screening in Kansas school children. J Kans Med Soc. 1980;81(12):568–571. [PubMed] [Google Scholar]
- 32.Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527–1537. doi: 10.1016/S0140-6736(08)60658-3. [DOI] [PubMed] [Google Scholar]
- 33.Raggio CL. Sexual dimorphism in adolescent idiopathic scoliosis. Orthop Clin North Am. 2006;37:555–558. doi: 10.1016/j.ocl.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 34.Luk KD, Lee CF, Cheung KM, Cheng JC, Ng BK, Lam TP, Mak KH, Yip PS, Fong DY. Clinical effectiveness of school screening for adolescent idiopathic scoliosis: a large population-based retrospective cohort study. Spine (Phila Pa 1976) 2010;35:1607–1614. doi: 10.1097/BRS.0b013e3181c7cb8c. [DOI] [PubMed] [Google Scholar]
- 35.Ueno M, Takaso M, Nakazawa T, Imura T, Saito W, Shintani R, Uchida K, Fukuda M, Takahashi K, Ohtori S, Kotani T, Minami S. A 5-year epidemiological study on the prevalence rate of idiopathic scoliosis in Tokyo: school screening of more than 250,000 children. J Orthop Sci. 2011;16:1–6. doi: 10.1007/s00776-010-0009-z. [DOI] [PubMed] [Google Scholar]
- 36.Richards BS, Herring JA, Johnston CE, Birch JG, Roach JW. Treatment of adolescent idiopathic scoliosis using Texas Scottish Rite Hospital instrumentation. Spine (Phila Pa 1976) 1994;19:1598–1605. doi: 10.1097/00007632-199407001-00008. [DOI] [PubMed] [Google Scholar]
- 37.Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL. Cotrel-Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1992;74:1056–1067. [PubMed] [Google Scholar]
- 38.Wang W, Zhu Z, Zhu F, Sun C, Wang Z, Sun X, Qiu Y (2012) Different curve pattern and other radiographic characteristics in male and female patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 37(18):1586–1592 [DOI] [PubMed]
- 39.Thompson SK, Bentley G. Prognosis in infantile idiopathic scoliosis. J Bone Joint Surg Br. 1980;62(B-2):151–154. doi: 10.1302/0301-620X.62B2.7364824. [DOI] [PubMed] [Google Scholar]
- 40.Wynne-Davies R. Familial (idiopathic) scoliosis. A family survey. J Bone Joint Surg Br. 1968;50(1):24–30. [PubMed] [Google Scholar]
- 41.James JI, Lloyd-Roberts GC, Pilcher MF. Infantile structural scoliosis. J Bone Joint Surg Br. 1959;41-B:719–735. doi: 10.1302/0301-620X.41B4.719. [DOI] [PubMed] [Google Scholar]
- 42.Figueiredo UM, James JI. Juvenile idiopathic scoliosis. J Bone Joint Surg Br. 1981;63(B-1):61–66. doi: 10.1302/0301-620X.63B1.7204475. [DOI] [PubMed] [Google Scholar]
- 43.Chiu YL, Huang TJ, Hsu RW. Curve patterns and etiologies of scoliosis: analysis in a university hospital clinic in Taiwan. Changgeng Yi Xue Za Zhi. 1998;21(4):421–428. [PubMed] [Google Scholar]
- 44.Janssen MM, Kouwenhoven JW, Schlösser TP, Viergever MA, Bartels LW, Castelein RM, Vincken KL. Analysis of preexistent vertebral rotation in the normal infantile, juvenile, and adolescent spine. Spine (Phila Pa 1976) 2011;36(7):E486–E491. doi: 10.1097/BRS.0b013e3181f468cc. [DOI] [PubMed] [Google Scholar]
- 45.Fong DY, Lee CF, Cheung KM, Cheng JC, Ng BK, Lam TP, Mak KH, Yip PS, Luk KD. A meta-analysis of the clinical effectiveness of school scoliosis screening. Spine (Phila Pa 1976) 2010;35(10):1061–1071. doi: 10.1097/BRS.0b013e3181bcc835. [DOI] [PubMed] [Google Scholar]
- 46.Adams W (1885) Lectures on the pathology and treatment of lateral and other forms of curvature of the spine in 1865, Lecture 10 [PMC free article] [PubMed]
- 47.Zhang J, He D, Gao J, Yu X, Sun H, Chen Z, Li M (2011) Changes in life satisfaction and self-esteem in patients with adolescent idiopathic scoliosis with and without surgical intervention. Spine (Phila Pa 1976) 36(9):741–745 [DOI] [PubMed]
- 48.Kahanovitz N, Weiser S. The psychological impact of idiopathic scoliosis on the adolescent female. A preliminary multi-center study. Spine. 1989;14:483–485. doi: 10.1097/00007632-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 49.Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10:278–288. doi: 10.1007/s005860100309. [DOI] [PMC free article] [PubMed] [Google Scholar]


