Abstract
Objective
To test the relationships between worry and perceptions of likelihood and severity (two indicators of risk perception) across eight common diseases, and to examine contributions of individual and disease variability in worry and risk perceptions.
Methods
Participants were 294 people recruited through the Multiplex Initiative, in which a genetic susceptibility test for 8 common diseases was offered to healthy adults. Participants completed a baseline telephone survey and Web-based surveys measuring the variables for this ancillary study, without a commitment to be tested.
Results
Between- and within-subjects analyses yielded the following findings: 1) worry is more related to likelihood perceptions than to severity perceptions; 2) severity perceptions add significantly to explained worry variances above and beyond likelihood perceptions; 3) the likelihood × severity perception does not add to explained variance in worry above its components; 4) risk perceptions and worries form two identifiable clusters: cancer diseases and cardiovascular-metabolic diseases; 5) there are significant differences in risk perceptions and worry among diseases; 6) there are significant gender differences in risk perceptions and worry about common diseases; 7) variance in risk perception and worry is explained by a combination of between- and within-subjects variances, with the latter being more powerful.
Conclusions
Risk perception research should pay attention to severity perceptions, within-subjects variability and inter-disease differences should not be ignored, gender perspectives on illness perceptions should be acknowledged, and health psychologists must prepare for considering groups of illnesses in addition to single diseases.
Keywords: risk perception, worry, severity, likelihood, within-subjects
Evidence accumulated in recent years suggests that risk perceptions – a keystone of most health behavior theories – can be successfully replaced by worry as a predictor of various health behaviors (e.g.: Cameron & Reeve, 2006; Cameron et al., 2009; Schmiege et al., 2009). The advantage of worry over risk for predicting health behaviors was suggested to be its affective component, a component missing from risk perception (Schmiege et al., 2009). However, the cognitive-affective distinction between worry and risk perception is neither clear-cut, nor sufficient for understanding the difference between them. Worry is indeed often viewed as an affective construct. For example, women's responses to measures of worry, fear, and anxiety about breast cancer were highly correlated (Lipkus et al., 2005). But, interestingly, non-pathological worry has been defined as a cognitive mechanism that maintains awareness of potential threat (Tallis & Eysenck, 1994). As for risk perception, the view that it is purely cognitive has also been challenged by assertions that people rely on feelings when judging risk (Loewenstein et al., 2001).
The first aim of the present study was to examine the nature of the relationships between worry and risk perception across multiple diseases. Risk perception and worry are undoubtedly interrelated constructs. Positive correlations between them were found with regard to various diseases (e.g.: lung cancer and smoking-related diseases, Park et al., 2009; gastric cancer, Kwak et al., 2009). However, the experience of risk is different from the experience of worry (Sjöberg, 1998). A review of the literature on cancer worry (Hay et al., 2005) turned up only moderate correlations (0.30 to 0.40) between perceived cancer risk and cancer worry. Similar moderate correlations (0.30 to 0.53) were found between perceived risk and worry for coronary heart disease, stroke, diabetes, and breast, ovarian, and colon cancers (Acheson et al., 2010). Several explanations were proposed to account for the relatively weak relationship between worry and risk perception. The risk-as-feelings hypothesis (Loewenstein et al. 2001) postulates that emotional reactions to risks (including worry) respond to situational variables, such as the immediacy of a risk, which have minimal effect on cognitive evaluations. At the same time, risk perceptions at a cognitive level are largely based on the probability and desirability of associated consequences. Sjöberg (1998) suggested that people can feel worried about a risk without believing that it is especially large, due to risk denial.
These accounts direct attention to the structure of risk perception. There is a general agreement that risk, as a future event, is defined by a combination of the likelihood or probability of a negative event, and the size and quality of its harmful consequences, should they occur (Drottz-Sjöberg, 1991). However, in the health psychology literature, risk perceptions are almost always defined as estimates of likelihood / chances, or beliefs about vulnerability / susceptibility (e.g., Hay et al., 2006; Klein, 2003; Kwak, et al., 2009; Lipkus, et al., 2005; Park, et al., 2009). Perceived severity of a disease, if measured in the same study, is usually treated as a separate construct. For example, a recent study in which participants received information about a genetic test of varying lifetime risks for diabetes, heart disease, colon cancer, or lung cancer (Cameron et al., 2009) found that worry was weakly correlated with perceived severity (r=.20) and moderately (r=.59) with perceived likelihood of these diseases. Still, most reports about modest correlations between worry and risk perception result from studying the relationship between worry and only one component of perceived risk, i.e., likelihood perceptions.
The need for a systematic examination of the relationships between worry and both components of risk perception (likelihood and severity), separately and in combination, is especially justified in view of a recent meta-analysis on the effects of manipulating vulnerability and severity contents in fear-arousing communications (de Hoog et al., 2007). The conclusion was that both vulnerability and severity (but not their interaction) had medium strong effects on perceived fear and more general measures of negative affect. The current study aimed to examine whether similar effects would be found for perceptions of likelihood and severity, as for message contents. Moreover, it was especially interesting to examine whether likelihood perceptions relate to worry independently of severity perceptions or by interaction, following findings that the impact of probability depends strongly on the nature of the outcome (Rottenstreich & Hsee, 2001).
The second aim of the study was to determine the roles of disease variability versus person variability in the distributions of worry and risk perception. Both risk perceptions and worry relate to persons who experience them and to objects (diseases) toward which these experiences refer. The person × situation issue (Mischel, 1979) is therefore at the core of the matter here. People vary in their general tendencies to worry about diseases and to perceive risks in their lives. Perceived risk across several diseases was found to be associated with perceived risk for a specific disease (DiLorenzo, et al 2006; Gerend, 2004). Worry about a specific disease was also shown to generalize to other similar diseases (DiLorenzo et al., 2006; Schnur, et al., 2006). Sjöberg (2004) suggested that judgments of the probability of experiencing one risk may in some way influence the judgment of other risks. He suggested that a general tendency to estimate risks as large or small - called risk sensitivity - is a common and strong phenomenon that may represent basic personality traits.
In addition, diseases vary in how they are perceived (e.g., Acheson et al., 2010; Cameron et al., 2009; Scharloo et al., 1998; Wang et al., 2009), and this variability may impact the amounts of worry and risk perceptions they elicit. For example, variations in prevalence rates and beliefs about treatment control may affect severity perceptions (Jemmott, Ditto, & Croyle, 1986). Nevertheless, the extensive literature on illness perceptions deals mainly with individual differences in perceptions within one single disease. Our aim was to examine how person dispositional variability and variability among diseases combine meaningfully to explain variability in disease worries and risk perceptions.
Summary and overview of the study
This study investigated the relationships between worry and both components of risk perception (likelihood and severity) separately and together, across eight common diseases. While positive correlations were predicted among all variables based on theoretical considerations and available research findings, their relative strengths were uncertain and therefore no hypothesis was formulated about them. The study also examined the separate and combined effects of individual variability and disease variability on worry and risk perceptions, with the expectation that both factors would contribute significantly. Again, no hypothesis was formed about the relative strengths of person and disease variances on worry and risk perceptions.
The data for this study was collected as part of the Multiplex Initiative (Alford, et al., 2010; McBride et al., 2008, 2009; Wade et al., 2008), which was designed to examine the uptake and impact of multiplex genetic testing. All participants were offered a multiplex genetic test that assessed risk for eight conditions: type 2 diabetes, osteoporosis, hypertension, coronary heart disease, hypercholesterolemia, skin cancer, lung cancer and colorectal cancer. Their risk perceptions and worry about each of these conditions were measured in a Web-based questionnaire prior to their decision whether to be tested.
Methods
Participants and procedures
The Multiplex Initiative was a collaborative transdisciplinary research project of the National Human Genome Research Institute (Bethesda, MD), the Cancer Research Network funded by the National Cancer Institute, the Group Health Cooperative (Seattle, WA), and the Henry Ford Health System (Detroit, MI). The participants were recruited from a sample of 350,000 members of the Henry Ford Health System. Enrollment required that participants be 25-40 years old, self-identified as white or African American, and not affected with type 2 diabetes, atherosclerotic cardiovascular disease, osteoporosis, or cancer (Alford, et al., 2010; McBride et al., 2008, 2009).
Participants were recruited by a telephone call, during which they completed a baseline questionnaire about demographics, family history of diseases, and perspectives on health. They were then sent a brochure introducing the multiplex genetic test (Wade, et al., 2008) and referred to the Multiplex Initiative Website. Interested participants could access the site to learn more about testing without a commitment to be tested. On this site, they were asked to complete a number of additional surveys, including the one for this ancillary study. Participants were offered a financial incentive ($20.00) to complete the questionnaires.
The present study focused on the subset of multiplex initiative participants (n=294) who completed the relevant questions on the baseline and ancillary Web-based surveys. Their average age was 34.61 years (SD=4.00), 51% were female, and 47% were white. Forty-six percent had at least a college degree, another 34% had some college education and 20% had 12 or fewer school years. Sixty-three percent were married or partnered. Demographic variables were the same in our sample and the sample of those who entered the Website but did not fill-out our survey (n=612).
Measures
Socio-demographic characteristics
were assessed at the baseline interview. Gender and age were obtained from the Henry Ford Health System electronic health record. Participants' race, marital status and educational level were obtained from the baseline survey.
Risk perception and worry
were measured by three 7-point scales for each of the 8 diseases in the study. Scales with that number of response categories were found preferable for discriminating between levels of perceived risks (Sjöberg, 2000). The diseases were: type 2 diabetes, osteoporosis, hypertension, coronary heart disease, hypercholesterolemia, skin cancer, lung cancer and colorectal cancer.
The question pertaining to the likelihood component of risk perception was: “On a scale from 1 to 7, where 1 is certain not to happen and 7 is certain to happen, what do you think is your chance of getting the following conditions in your lifetime?” (Each disease name asked). For the severity component of risk perception the question was: “On a scale from 1 to 7, where 1 is not at all serious and 7 is very serious, how serious do you think it is to have the following diseases?” (Each disease name asked). Worry was assessed individually for each of the eight health conditions. The text of the worry item was: “On a scale from 1 to 7, where 1 is not at all worried and 7 is very worried, how worried are you about getting the following conditions in your lifetime?” (Each disease name asked).
Data analysis
Pearson correlations were computed between risk components (including their interaction) and worry for each of the diseases. The significance of differences between correlations was tested by Fisher r-to-z transformations. Correlations among those variables were computed also within individuals (across the 8 diseases) following the case-study approach for studying risk perceptions advocated by Weinstein (2000). Hierarchical regression analyses were performed to predict worry for each of the diseases by its risk perception components (perceived likelihood and severity). Risk perceptions were assumed to predict worry rather than the opposite, based on strong evidence supporting this direction of influence (DiLorenzo et al., 2006; Lipkus et al., 2005). Differences between diseases in the amounts of worry and risk perceptions they elicit were tested by analyses of variance. Principal component factor analyses with Varimax rotation were used to identify underlying factors in worry and risk perceptions across the 8 diseases. Finally, a componential model that examines multiple people in multiple situations (diseases) was applied (Krueger, 2009). Specifically, we applied the density distribution approach (Fleeson, 2007), to explore a possible integration between disease variance and individual differences in worry and risk perceptions. Unconditional models from multilevel modeling were used to account for estimation variation, in which disease level was predicted from a grand mean, a deviation for the participant's mean, and a deviation specific to that disease. These analyses were conducted using the SPSS-17 ‘mixed models’ command.
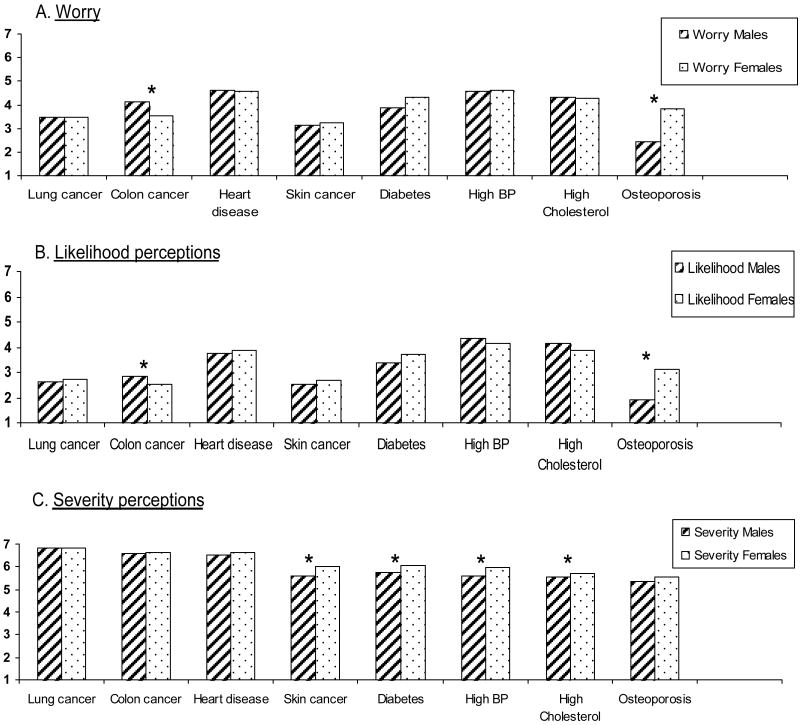
Results
Data on worry, perceived likelihood and perceived severity by diseases and gender are presented in Table 1 and Fig. 1. Significant differences were found between diseases on all three variables in both genders. Participants of the total sample were most worried about heart disease, high BP, high cholesterol and diabetes, and those same diseases were also perceived as most likely to occur. The diseases perceived as most severe differed somewhat: lung cancer, colon cancer, heart disease and diabetes. Multivariate tests showed significant gender differences in worry (F(8,283)=12.27, p=.00), severity perceptions (F(8,284)=2.00, p=.04), and likelihood perceptions (F(8,283)=9.23, p=.00). Specifically, women were more worried than men about osteoporosis and perceived it as more likely to happen, while men worried more than women about colon cancer and perceived it as more likely to happen. Women also perceived most diseases as more severe than men, particularly skin cancer, diabetes, high blood pressure and high cholesterol.
Table 1. Means and SDs of worry, perceived likelihood and perceived severity by gender (male=144; female=149) and diseases.
| Disease | Worry | Perceived Severity | Perceived likelihood | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Colon cancer | 3.52 | 2.13 | 4.11 | 2.04 | 6.62 | .83 | 6.58 | .75 | 2.51 | 1.49 | 2.85 | 1.47 |
| Skin cancer | 3.25 | 1.90 | 3.15 | 1.88 | 6.04 | 1.24 | 5.62 | 1.44 | 2.69 | 1.67 | 2.49 | 1.53 |
| Lung cancer | 3.49 | 2.22 | 3.47 | 2.26 | 6.85 | .52 | 6.85 | .44 | 2.74 | 1.67 | 2.61 | 1.70 |
| Heart disease | 4.57 | 1.98 | 4.60 | 1.90 | 6.62 | .71 | 6.56 | .72 | 3.89 | 1.76 | 3.77 | 1.72 |
| Osteoporosis | 3.81 | 1.97 | 2.44 | 1.73 | 5.53 | 1.16 | 5.34 | 1.41 | 3.13 | 1.80 | 1.94 | 1.23 |
| Diabetes | 4.32 | 2.09 | 3.89 | 2.08 | 6.07 | 1.02 | 5.74 | 1.32 | 3.72 | 1.91 | 3.36 | 1.92 |
| High BP | 4.62 | 2.13 | 4.56 | 2.05 | 5.99 | 1.19 | 5.60 | 1.33 | 4.12 | 2.05 | 4.36 | 1.98 |
| High cholesterol | 4.27 | 1.95 | 4.34 | 1.93 | 5.71 | 1.24 | 5.35 | 1.42 | 3.87 | 1.91 | 4.11 | 1.87 |
| F | 12.56** | 37.67** | 37.67** | 35.74** | 17.04** | 37.67** | ||||||
p<.01
Figure 1. Means of worry, severity and likelihood perceptions by disease and gender.
Next, we investigated the relationships between worry, likelihood and severity perceptions. The Spearman's Rho correlation between the rank-orders of the 8 diseases on worry and likelihood (based on the total sample) was very high (r=0.95). Rank-order correlations by worry and severity and by likelihood and severity were negligible (r's = 0.08 and −0.04 correspondingly). Correlations computed within diseases (Table 2) show that for every disease, worry was moderately to highly correlated with likelihood perceptions (range of correlations: .54 to .78). A similar range of correlations were found between worry and the interaction term (likelihood × severity), which is a closer index of the formal definitions of risk. The correlations between worry and severity perceptions were significantly positive (except for lung cancer), but their range was much lower (0.09 to 0.32). For each disease, worry was more strongly correlated with likelihood perceptions than with severity perceptions. Correlations computed within individuals among the same variables (across 8 diseases) yielded similar results.
Table 2. Correlations between worry, perceived likelihood and perceived severity by disease type.
| Disease | A. Worry - Likelihood | B. Worry - Severity | C. Likelihood - Severity | Worry - Like.×Sever. | Z difference A-B |
|---|---|---|---|---|---|
| Colon cancer | .54** | .19** | .11* | .55** | 5.09** |
| Skin cancer | .62** | .16** | -.03 | .63** | 6.50** |
| Lung cancer | .66** | .09 | .01 | .67** | 8.33** |
| Heart disease | .69** | .10* | .02 | .68** | 8.89** |
| Osteoporosis | .73** | .26** | .14** | .72** | 8.13** |
| Diabetes | .77** | .26** | .19** | .76** | 9.47** |
| High BP | .78** | .32** | .20** | .78** | 8.90** |
| High cholesterol | .70** | .27** | .09 | .72** | 7.06** |
|
| |||||
| Mean correlation within individuals | .72 (n=267) |
.14 (n=239) |
.01 (n=242) |
.71 (n=270) |
|
p<.05
p<.01
Subsequently, hierarchical regression analyses were performed to predict worry by likelihood perceptions (first step), severity perceptions (second step), and likelihood × severity interactions (third step) for each disease separately (Table 3). As the analyses show, between 31% (for colon cancer) and 64% (for high blood pressure) of the variance in worry could be explained by likelihood and severity perceptions. While most of the variance was explained by likelihood perceptions, severity perceptions had a significant independent contribution (between 1% for lung cancer and heart disease and 5% for high cholesterol) to explaining worry above and beyond likelihood perceptions for each of the diseases. The likelihood × severity interaction terms did not add to explaining variance in worry beyond its components in any of the diseases.
Table 3. Regression analyses findings for predicting worry by perceived likelihood (Step 1), perceived severity (Step 2), and perceived likelihood × severity (Step 3) by diseases.
| R | R2 | F for R change | df | Sig. | |
|---|---|---|---|---|---|
| Colon Cancer | |||||
| Step 1 – Perceived likelihood | .54 | .29 | 118.15 | 1,291 | .000 |
| Step 2 – Perceived severity | .55 | .31 | 7.70 | 1,290 | .006 |
| Step 3 – likelihood × severity | .55 | .31 | 0.79 | 1,289 | .375 |
|
| |||||
| Skin Cancer | |||||
| Step 1 – Perceived likelihood | .62 | .38 | 178.69 | 1,292 | .000 |
| Step 2 – Perceived severity | .64 | .41 | 14.60 | 1,291 | .000 |
| Step 3 – likelihood × severity | .64 | .41 | 0.09 | 1,290 | .762 |
|
| |||||
| Lung Cancer | |||||
| Step 1 – Perceived likelihood | .66 | .44 | 227.65 | 1,291 | .000 |
| Step 2 – Perceived severity | .67 | .45 | 3.61 | 1,290 | .059 |
| Step 3 – likelihood × severity | .67 | .45 | 1.46 | 1,289 | .228 |
|
| |||||
| Heart Disease | |||||
| Step 1 – Perceived likelihood | .68 | .47 | 258.72 | 1,292 | .000 |
| Step 2 – Perceived severity | .69 | .48 | 4.26 | 1,291 | .040 |
| Step 3 – likelihood × severity | .69 | .48 | 0.08 | 1,290 | .773 |
|
| |||||
| Osteoporosis | |||||
| Step 1 – Perceived likelihood | .73 | .53 | 324.08 | 1,292 | .000 |
| Step 2 – Perceived severity | .74 | .55 | 17.08 | 1,291 | .000 |
| Step 3 – likelihood × severity | .74 | .55 | 0.27 | 1,290 | .604 |
|
| |||||
| Diabetes | |||||
| Step 1 – Perceived likelihood | .77 | .59 | 422.41 | 1,292 | .000 |
| Step 2 – Perceived severity | .78 | .61 | 10.23 | 1,291 | .002 |
| Step 3 – likelihood × severity | .78 | .61 | 0.02 | 1,290 | .891 |
|
| |||||
| High Blood Pressure | |||||
| Step 1 – Perceived likelihood | .78 | .61 | 456.95 | 1,292 | .000 |
| Step 2 – Perceived severity | .80 | .64 | 21.67 | 1,291 | .000 |
| Step 3 – likelihood × severity | .80 | .64 | 0.09 | 1,290 | .768 |
|
| |||||
| High Cholesterol | |||||
| Step 1 – Perceived likelihood | .70 | .48 | 274.25 | 1,292 | .000 |
| Step 2 – Perceived severity | .73 | .53 | 25.95 | 1,291 | .000 |
| Step 3 – likelihood × severity | .73 | .53 | 2.95 | 1,290 | .087 |
Factor analyses were performed next to determine the structure of worries and risk perceptions (likelihood and severity perceptions) across the 8 investigated diseases (Table 4). Two factors above 1 eigenvalue were extracted in each analysis. The first factor consisted of heart disease, diabetes, high BP, and high cholesterol, and the second factor consisted of colon cancer, skin cancer and lung cancer. Osteoporosis represented a different pattern: it joined the cancer factor with regard to worry and likelihood perceptions, and the cardiovascular-metabolic factor with regard to severity perceptions.
Table 4. Rotated Component Matrices for worry, severity and likelihood across diseases (n=293).
| Eigenvalue | Worry | Severity | Likelihood | |||
|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 1 | Factor 2 | |
| 4.20 | 1.15 | 4.37 | 1.09 | 3.54 | 1.28 | |
| Colon cancer | .33 | .65 | .30 | .68 | .19 | .63 |
| Skin cancer | .08 | .86 | .36 | .65 | .06 | .79 |
| Lung cancer | .32 | .69 | .04 | .87 | .27 | .59 |
| Heart disease | .72 | .46 | .53 | .49 | .75 | .41 |
| Osteoporosis | .25 | .74 | .65 | .40 | .15 | .72 |
| Diabetes | .78 | .28 | .88 | .19 | .78 | .23 |
| High BP | .89 | .11 | .90 | .24 | .87 | .03 |
| High cholesterol | .77 | .24 | .88 | .20 | .77 | .19 |
Extraction method: Principal Component Analysis; Rotation method: Varimax with Kaiser Normalization; rotation converged in 3 iterations
Finally, results of three unconditional multilevel mixed models – for worry, severity and likelihood perceptions (293 individuals by 8 diseases) – are presented in Table 5. The average level shows the typical participant's mean level of worry / perceived severity / perceived likelihood across diseases. Percentages indicate that the percents of total variance that occurred within participants were greater than the percentage of total variation that occurred between participants. As can be seen, 58% to 70% of the variance in worry and risk perceptions occurred within individuals and 30% to 42% of the variance occurred between individuals. While both within- and between-participants' variances contributed to worry and risk perceptions, these findings mean that people switch their worry and risk perceptions considerably between diseases.
Table 5. Density distributions of worry, severity and likelihood perceptions.
| Distribution parameter | Worry | Severity | Likelihood |
|---|---|---|---|
| Average level | 3.90 | 6.07 | 3.27 |
| Variance within individuals | 2.59 (58%) | 0.94 (65%) | 2.47 (70%) |
| Variance between individuals | 1.87 (42%) | 0.52 (35%) | 1.08 (30%) |
Discussion
Our findings indicate that worry is particularly related to one component of risk perception – likelihood perception. The correlations of worry with likelihood perceptions were much stronger than with severity perceptions, although both are equal components of risk definitions. This was demonstrated both at the disease level across individuals, and at the personal level across diseases. These findings are compatible with previous reports. While there are ample reports of positive correlations between worry and likelihood perceptions, often presented as ‘risk perceptions’ (e.g., Acheson et al., 2010; Kwak et al., 2009; Lipkus et al., 2000; Lipkus et al., 2005; Park et al., 2009; Schwartz et al., 1995), there are many fewer reports of associations between worry and severity perceptions, and all of them show much lower correlations (Cameron et al., 2009; Ness & Klaas, 1994; Wang, personal communication). These findings are in contrast to the ‘risk as feeling’ hypothesis, which asserts that feelings of worry are sensitive to the possibility of negative consequences, which elicit concrete images of outcomes, and insensitive to a large range of changes in the probability of events leading to those outcomes (Loewenstein et al., 2001). The inconsistency of findings with this contention may stem from using measures of likelihood perceptions that capture ‘feelings of risk’ (Weinstein et al., 2007), which represent affective, gut-level indicators of likelihood that are distinct from cognitive appraisals of likelihood. These ‘feelings of risk’ may be more associated with worry than severity perceptions.
The closer similarity of worry to likelihood perceptions in contrast to severity perceptions was also evident from their distributions. Perceptions of severity were high, while worry and likelihood perceptions were much lower. Similar findings across 6 common diseases were reported by Wang et al. (2009). Optimistic perceptions of risk (likelihood) are well documented (e.g., Rothman et al., 1996), and the predominance of low levels of disease worry in the general population was also noted (Acheson et al., 2010; Hay et al., 2005). These optimistic appraisals can be interpreted as defensive processes that help preserve a positive and unthreatened self image (Rothman et al., 1996). We suggest that the dimension by which worry and likelihood perceptions diverge from severity perceptions is ‘self relevance’. While severity perceptions represent ‘cool’ cognitions about diseases that can be alienated from the self, worry and likelihood perceptions are self directed. As such, they are more prone to defensive processing and downward biases than severity perceptions.
However, despite the closer relationship between worry and likelihood perceptions, perceived severity had an independent small but significant contribution to explaining worry variance, above and beyond likelihood perceptions. This finding, which was replicated across diseases, may indicate that worry captures the concept of ‘risk’ more comprehensively than just likelihood perceptions. This may partly explain the advantage of worry over risk (defined narrowly) in predicting health behaviors, in addition to other unique aspects of worry (e.g., Cameron & Reeve, 2006; Cameron et al., 2009; Schmiege et al., 2009).
We also found that individual differences in worry and risk perception clustered around two identifiable groups of diseases: cancer diseases and cardiovascular-metabolic diseases. People who worried about one cancer disease, tended to worry about other cancer conditions more than about cardiovascular-metabolic diseases, and participants who worried about one cardiovascular-metabolic disease tended to worry about other diseases in the same category more than about cancer diseases. Osteoporosis showed a different pattern: it joined the cancer factor with regard to worry and likelihood perceptions, and the cardiovascular-metabolic factor with regard to severity perceptions. The explanation for this can be found in a study about prevalence and correlates of illness worry in a representative sample of the American population (Noyes et al., 2005), in which participants were asked about diseases they had worried about in the past year. Correlates of worry about physical conditions made up three clusters: cancer diseases, heart disease (including high blood pressure and diabetes), and other diseases (lung disease, neurological disease, bone or joint disease, other serious diseases). Despite the methodological difference between their and our study, our findings replicated the cancer and the heart (cardiovascular - metabolic) clusters. The relative instability of osteoporosis in our findings may have resulted from the fact that among the eight diseases included in the Multiplex Testing project, it was the only disease related to the third (‘other’) cluster identified by Noyes et al. (2005). More research with wider samples of diseases is needed to refine the clustering of risk perceptions and worries identified so far.
While both within- and between-participants' variances contributed to worry and risk perceptions, our findings indicated that the specific disease being considered is more powerful in predicting worry and risk perception of the average individual compared to personal propensity to worry about diseases. This finding underscores the importance of disease variability in health psychology research. Examining perceptions for multiple conditions enabled us making comparisons among them. Diseases raising highest worries were those perceived as most likely to occur: heart disease, high blood pressure, high cholesterol and diabetes. Diseases perceived as most severe were somewhat different: lung cancer, colon cancer, heart disease and diabetes.
These findings can only be weighted against a small number of studies that have provided comparative reports of perceptions across diseases. Some reported higher risk perception for cancer, specifically breast cancer among women, compared to heart disease (Mosca et al., 2004; Wang et al., 2009; Wilcox et al., 2002). Others found that men perceived their risks for heart disease the greatest, followed by prostate cancer, diabetes and colorectal cancer (DiLorenzo et al., 2006). In other studies, perceived severity has not been shown to differ between various diseases including breast cancer and heart disease (Gerend et al., 2004). We think that two related factors can explain the conflicting findings: the set of diseases investigated and the moderation of gender. Health and illness perceptions are known to be sensitive to framing effects, contrast effects, anchoring effects and priming effects (Brewer & Chapman, 2003; Gana et al., 2010; Henderson et al., 2007; Senay & Kaphingst, 2009). Consequently, it can be expected that risk perceptions and worry about a specific disease would be affected by the set of diseases in which it is included for evaluation. For example, the set of diseases investigated in our study did not include distinctive gender-related conditions like breast and prostate cancers that might have provided strong anchors for evaluating other diseases included in the same set.
Nevertheless, gender differences were found even in our supposedly gender-neutral set of diseases. Women perceived most diseases as more severe than men, and perceived osteoporosis as more likely and worried about it more than men. Men perceived colon cancer as more likely and worried about it more than women. These findings add to the limited literature on gender differences in perceived risk and worry for common diseases. There are some reports that women had higher risk perceptions and worries about cancer than men (DiLorenzo et al., 2006; McQueen et al., 2008; Robb et al., 2004). Wang et al. (2009) found that, compared to men, women had higher perceived risk and worry for heart disease, diabetes, and stroke. More research on gender differences in risk perceptions and worry will clarify the reasons for them and their potential impact on health behaviors.
Limitations of the study
One limitation of the study is the limited number (8) of diseases examined. Sampling other common health conditions is needed in order to replicate and generalize from our findings. Another limitation is the context in which perceptions were measured: a genetic testing offer, that may have stimulated specific perceptions and worries, calling for replication of the study in other settings. The use of one-item scales per disease for measuring perceptions and worry is also a limitation given that different measures for these constructs are not interchangeable (Ranby, 2010). The diseases were also presented in a fixed order, which may have introduced order effects. Thus, replications using different measures and methods of presentations are needed to substantiate our findings.
Conclusions and implications
This study has shown that disease worries are closely related to likelihood perceptions, which constitute one component of risk perception, and to a lesser degree to perceived severity of diseases. Thus, risk perception research would benefit from attending to the perceived severity component of risk perception, which is often ignored.
Research in health psychology is based predominantly on between-subjects designs whereby individual differences in various variables and the relationships among them are investigated. Such methodology is most appropriate when looking into a specific disease and examining relevant patient differences. Within-subjects designs are quite rare in health psychology (Cohen & Lemay, 2007; Finlay et al., 1997; Weinstein, 2000), which is unfortunate because people are quite sensitive to situational changes and, as indicated in the current study, react differently to different diseases. A case in point is the study by Harris et al. (2008) in which individual differences and event characteristics contributed jointly to understanding optimistic biases. Taken together, these findings argue for a within-subjects approach to issues that are not disease-specific – one that will measure variables of interest across several illnesses, yielding both within- and between-subjects variances. The advantages of this approach are underscored in the present study.
Our results also justify giving more attention to gender perspectives on illness perceptions. Women tended to perceive diseases differently than men, and some common diseases (e.g., osteoporosis, colon cancer) seem to involve gender stereotypes. Such perceptual sex-differences may result in important behavioral implications. For example, a recent meta-analytic review of the literature about acute coronary syndrome (ACS) found substantive gender differences in reporting and interpreting of ACS symptoms with significant implications for clinical and public-health practices (Shin et al., 2010).
With the growing availability of multiplex genetic testing for several diseases at once, it is important to extend our understanding of intrapersonal variances in perceptions of diseases and mutual influences among perceptions of various diseases. Unlike in the past when people normally had to deal with one disease (or information about it) at a time, they will soon need to react, decide upon and cope with multiple diseases at once. A recently published model delineated mutual links between disease-specific perceived risk and worry, and worries about other diseases (DiLorenzo et al., 2006). It is an example of the next generation of complexity in theory and research that health psychologists need to develop in order to deal with the new challenges.
Acknowledgments
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The proposed research was made possible through a collaboration with the Cancer Research Network funded by the National Cancer Institute (U19CA 079689). Group Health Research Institute and Henry Ford Hospital provided additional resources. Additionally, this research was supported in part by an appointment to the Senior Fellowship Program at the National Institutes of Health. This program is administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and the National Institutes of Health.
We would like to thank the study participants, members of the Henry Ford Health System and members of the Multiplex Initiate Steering Committee for their efforts in making the Multiplex Initiative Ancillary Studies possible. We would also like to thank Yasmin Alkalay for her excellent assistance in statistical analyses.
References
- Acheson LS, Wang C, Zyzanski SJ, Lynn A, Ruffin MT, Gramling R, Rubinstein WS, O'Neill SM, Nease DE., Jr Family history and perceptions about risk and prevention for chronic diseases in primary care: A report from the Family Healthware (TM) Impact Trial. Genetics in Medicine. 2010;12:212–218. doi: 10.1097/GIM.0b013e3181d56ae6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alford SH, McBride CM, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Participation in genetic testing research varies by social group. Public Health Genomics. 2010 doi: 10.1159/000294277. on line first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB. Contrast effects in judgments of health hazards. The Journal of Social Psychology. 2003;143:341–354. doi: 10.1080/00224540309598449. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Reeve J. Risk perceptions, worry, and attitudes about genetic testing for breast cancer susceptibility. Psychology and Health. 2006;21:211–230. doi: 10.1080/14768320500230318. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Sherman KA, Marteau TM, Brown PM. Impact of Genetic Risk Information and Type of Disease on Perceived Risk, Anticipated Affect, and Expected Consequences of Genetic Tests. Health Psychology. 2009;28:307–316. doi: 10.1037/a0013947. [DOI] [PubMed] [Google Scholar]
- Cohen S, Lemay EP. Why would social networks be linked to affect and health practices? Health Psychology. 2007;26:410–417. doi: 10.1037/0278-6133.26.4.410. [DOI] [PubMed] [Google Scholar]
- de Hoog N, Stroebe W, de Wit JBF. The impact of vulnerability to and severity of a health risk on processing and acceptance of fear-arousing communications: A meta-analysis. Review of General Psychology. 2007;11:258–285. [Google Scholar]
- Drottz-Sjöberg BM. Perception of Risk. Studies of Risk Attitudes, Perceptions and Definitions. Stockholm: Stockholm School of Economics, Center for Risk Research; 1991. [Google Scholar]
- DiLorenzo TA, Schnur J, Montgomery GH, Erblich J, Winkel G, Bovbjerg DH. A model of disease-specific worry in heritable disease: the influence of family history, perceived risk and worry about other illnesses. Journal of Behavioral Medicine. 2006;29:37–49. doi: 10.1007/s10865-005-9039-y. [DOI] [PubMed] [Google Scholar]
- Finlay KA, Trafimow D, Jones D. Predicting health behaviors from attitudes and subjective norms: Between-subjects and within-subjects analyses. Journal of Applied Social Psychology. 1997;27:2015–2031. [Google Scholar]
- Fleeson W. Situation-based contingencies underlying trait-content manifestation in behavior. Journal of Personality. 2007;75:825–861. doi: 10.1111/j.1467-6494.2007.00458.x. [DOI] [PubMed] [Google Scholar]
- Gana K, Lourel M, Trouillet R, Fort I, Mezred D, Blaison C, Boudjemadi V, K'Delant P, Ledrich J. Judgment of riskiness: Impact of personality, naive theories and heuristic thinking among female students. Psychology and Health. 2010;25:131–147. doi: 10.1080/08870440802207975. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Aiken LS, West SG. Personality factors in older women's perceived susceptibility to diseases of aging. Journal of Personality. 2004;72:243–270. doi: 10.1111/j.0022-3506.2004.00262.x. [DOI] [PubMed] [Google Scholar]
- Hay JL, Buckley TR, Ostroff JS. The role of cancer worry in cancer screening: A theoretical and empirical review of the literature. Psycho-Oncology. 2005;14:517–534. doi: 10.1002/pon.864. [DOI] [PubMed] [Google Scholar]
- Hay JL, Coups E, Ford J. Predictors of perceived risk for colon cancer in a national probability sample in the United States. Journal of Health Communication. 2006;11:71–92. doi: 10.1080/10810730600637376. [DOI] [PubMed] [Google Scholar]
- Henderson CJ, Hagger MS, Orbell S. Does priming a specific illness schema result in an attentional information-proces sing bias for specific illnesses? Health Psychology. 2007;26:165–173. doi: 10.1037/0278-6133.26.2.165. [DOI] [PubMed] [Google Scholar]
- Jemmott JB, Ditto PH, Croyle RT. Judging health status: Effects of perceived prevalence and personal relevance. Journal of Personality and Social Psychology. 1986;50:899–905. doi: 10.1037//0022-3514.50.5.899. [DOI] [PubMed] [Google Scholar]
- Klein WMP. Self-prescriptive, perceived, and actual attention to comparative risk information. Psychology and Health. 2003;18:625–643. [Google Scholar]
- Krueger JI. A componential model of situation effects, person effects, and situation-by-person interaction effects on social behavior. Journal of Research in Personality. 2009;43:127–136. [Google Scholar]
- Kwak MS, Choi KS, Park S, Park EC. Perceived risk for gastric cancer among the general Korean population: a population-based survey. Psycho-Oncology. 2009;18:708–715. doi: 10.1002/pon.1458. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Klein WMP, Skinner CS, Rimer BK. Breast cancer risk perceptions and breast cancer worry: what predicts what? Journal of Risk Research. 2005;8:439–452. [Google Scholar]
- Lipkus IM, Kuchibhatla M, McBride CM, Bosworth HB, Pollak KI, Siegler IC, Rimer BK. Relationships among breast cancer perceived absolute risk, comparative risk, and worries. Cancer Epidemiology Biomarkers & Prevention. 2000;9:973–75. [PubMed] [Google Scholar]
- Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychological Bulletin. 2001;127:267–286. doi: 10.1037/0033-2909.127.2.267. [DOI] [PubMed] [Google Scholar]
- McBride CM, Alford SH, Reid RJ, et al. Putting science over supposition in the arena of personalized genomics. Nature Genetics. 2008;40:939–942. doi: 10.1038/ng0808-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Alford SH, Reid RJ, et al. Characteristics of users of online personalized genomic risk assessments: Implications for physician-patient interactions. Genetics in Medicine. 2009;11:582–587. doi: 10.1097/GIM.0b013e3181b22c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen A, Vernon SW, Meissner HI, Rakowski W. Risk perceptions and worry about cancer: does gender make a difference? Journal of Health Communication. 2008;13:56–79. doi: 10.1080/10810730701807076. [DOI] [PubMed] [Google Scholar]
- Mischel W. Interface of cognition and personality - beyond the person-situation debate. American Psychologist. 1979;34:740–754. [Google Scholar]
- Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women's awareness of heart disease: An American Heart Association national study. Circulation. 2004;109:573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- Ness RM, Klaas R. Risk perception by patients with anxiety disorders. Journal of Nervous and Mental Disease. 1994;182:466–470. doi: 10.1097/00005053-199408000-00008. [DOI] [PubMed] [Google Scholar]
- Noyes R, Jr, Carney CP, Hillis SL, Jones LE, Langbehn DR. Prevalence and correlates of illness worry in the general population. Psychosomatics. 2005;46:529–539. doi: 10.1176/appi.psy.46.6.529. [DOI] [PubMed] [Google Scholar]
- Park ER, Ostroff JS, Rakowski W, Gareen IF, Diefenbach MA, Feibelmann S, Rigotti NA. Risk perceptions among participants undergoing lung cancer screening: Baseline results from the National Lung Screening Trial. Annals of Behavioral Medicine. 2009;37:268–279. doi: 10.1007/s12160-009-9112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranby KW, Aiken LS, Gerend MA, Erchull MJ. Perceived susceptibility measures are not interchangeable: Absolute, direct comparative, and indirect comparative risk. Health Psychology. 2010;29:20–28. doi: 10.1037/a0016623. [DOI] [PubMed] [Google Scholar]
- Robb K, Miles A, Wardle J. Demographic and psychosocial factors associated with perceived risk for colorectal cancer. Cancer Epidemiology Biomarkers & Prevention. 2004;13:366–372. [PubMed] [Google Scholar]
- Rothman AJ, Klein WM, Weinstein ND. Absolute and relative biases in estimations of personal risk. Journal of Applied Social Psychology. 1996;26:1213–1236. [Google Scholar]
- Rottenstreich Y, Hsee CK. Money, kisses, and electric shocks: On the affective psychology of risk. Psychological Science. 2001;12:185–190. doi: 10.1111/1467-9280.00334. [DOI] [PubMed] [Google Scholar]
- Scharloo M, Kaptein AA, Weinman J, Hazes JM, Willems LNA, Bergman W, Rooijmans HGM. Illness perceptions, coping and functioning in patients with rheumatoid arthritis, chronic obstructive pulmonary disease and psoriasis. Journal of Psychosomatic Research. 1998;44:573–585. doi: 10.1016/s0022-3999(97)00254-7. [DOI] [PubMed] [Google Scholar]
- Schmiege SJ, Bryan A, Klein WMP. Distinctions between worry and perceived risk in the context of the Theory of Planned Behavior. Journal of Applied Social Psychology. 2009;39:95–119. [Google Scholar]
- Schnur JB, DiLorenzo TA, Montgomery GH, Erblich J, Winkel G, Hall SJ, Bovbjerg DH. Perceived risk and worry about prostate cancer: A proposed conceptual model. Behavioral Medicine. 2006;32:89–96. doi: 10.3200/BMED.32.3.89-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz M, Lerman C, Miller SM, Daly M, Masny A. Coping disposition, perceived risk, and psychological distress among women at increased risk for ovarian cancer. Health Psychology. 1995;14:232–235. doi: 10.1037//0278-6133.14.3.232. [DOI] [PubMed] [Google Scholar]
- Senay I, Kaphingst KA. Anchoring-and-Adjestment bias in communication of disease risk. Medical Decision Making. 2009;29:193–201. doi: 10.1177/0272989X08327395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjöberg L. Worry and risk perception. Risk Analysis. 1998;18:85–93. doi: 10.1111/j.1539-6924.1998.tb00918.x. [DOI] [PubMed] [Google Scholar]
- Sjoberg L. The methodology of risk perception research. Quality & Quantity. 2000;34:407–418. [Google Scholar]
- Sjöberg L. Editorial: Asking questions about risk and worry: dilemmas of the pollsters. Journal of Risk Research. 2004;7:671–674. [Google Scholar]
- Tallis F, Eysenck MW. Worry: Mechanisms and modulating influences. Behavioral and Cognitive Psychotherapy. 1994;22:37–56. [Google Scholar]
- Wade CH, McBride CM, Alford SH, Baxevanis AD, Reid R, Larson EB, Brody LC. When genetic susceptibility testing is offered for multiple common health conditions, who is interested? Annals of Behavioral Medicine. 2008;35:S19–S19. [Google Scholar]
- Wang C, O'Neill SM, Rothrock N, Gramling R, Sen A, Acheson LS, Rubinstein WS, Nease DE, Jr, Ruffin MT. Comparison of risk perceptions and beliefs across common chronic diseases. Preventive Medicine. 2009;48:197–202. doi: 10.1016/j.ypmed.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND. Perceived probability, perceived severity, and health-protective behavior. Health Psychology. 2000;19:65–74. doi: 10.1037//0278-6133.19.1.65. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychology. 2007;26:146–151. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Ainsworth BE, LaMonte MJ, DuBose KD. Worry regarding major diseases among older African-American, Native-American and Caucasian women. Women & Health. 2002;36:83–99. doi: 10.1300/J013v36n03_06. [DOI] [PubMed] [Google Scholar]