Abstract
Background
Donor selection criteria for adult-to-adult living donor liver transplantation vary with the medical center of evaluation. Living donor evaluation utilizes considerable resources and the non-maturation of potential into actual donors may sometimes prove fatal for patients with end stage liver disease. On the contrary, a thorough donor evaluation process is mandatory to ensure safe outcomes in otherwise healthy donors. We aimed to study the reasons for non-maturation of potential right lobe liver donors at our transplant center.
Methods
A retrospective data analysis of all potential living liver donors evaluated at our center from 1998 to 2010 was done.
Results
Overall 324 donors were evaluated for 219 potential recipients and 171 (52.7%) donors were disqualified. Common reasons for donor non-maturation included: (1) Donor reluctance, 21% (2) >10% macro-vesicular steatosis, 16% (3) assisted donor withdrawal, 14% (4) inadequate remnant liver volume, 13% (5) psychosocial issues, 7% and thrombophilia, 7%. Ten donors (6%) were turned down due to anatomical variations (8 biliary and 2 arterial anomalies). Donors older than 50 years and those with BMI over 25 were less likely to be accepted for donation.
Conclusions
We conclude that donor reluctance, hepatic steatosis and assisted donor withdrawal are major reasons for non-maturation of potential into actual donors. Anatomical variations and underlying medical conditions were not a major cause of donor rejection. A system in practice to recognize these factors early in the course of donor evaluation to improve the efficiency of the selection process and ensure donor safety is proposed.
Keywords: living donor transplantation, liver transplantation, donor selection, right lobe liver donation, donor evaluation
Introduction
Adult-to-adult living donor liver transplantation (LDLT) using the right lobe has become a viable option for patients with end stage liver disease. It is associated with lower waiting list mortality and a graft-patient survival that is comparable to deceased donor liver transplantation (1). Adult-to-adult LDLT was adopted by a few centers in the United States after 1998 to address the problem of organ shortage. The number of procedures performed peaked in 2001 at approximately 10% of total adult liver transplants but subsequently waned to approximately 4% of the total due to concerns about donor morbidity and mortality. Between 2001 and 2004, the number of living donor liver transplants declined by 45% (2) and one of the reasons was the adverse publicity from the death of a living liver donor (3).
Donor evaluation is one of the most important aspects of adult-to-adult living donor liver transplantation (4–6). The evaluation process should reveal any conditions that may predispose the healthy donor to any intra and post-operative complications. A cost-effective evaluation procedure should also systematically rule out the unsuitable candidates at an early stage while selecting those who will likely yield an appropriate graft for the intended recipient. It has been observed that while one-third of recipients may have a potential living donor, only less than half will successfully proceed to be donors. Results from Adult-to-Adult Living Donor Liver (A2ALL) Transplant consortium showed a wide variation in the donor rejection rates between the nine evaluating centers within the United States (7). In this study, the strongest predictor of donor acceptance was the medical center of evaluation. It is expected that lessons from the learning curves of experienced LDLT programs would help centers with limited experience (< 20 procedures) in improving their outcomes of adult-to-adult LDLT.
For adult-to-adult living donor liver transplantation, we have preferred the right lobe (segment V, VI, VII and VIII) since the inception of our program. One of the aims of our single center, retrospective analysis was to share over thirteen years of experience in evaluating and selecting donors for right lobe living donor liver transplantation. The second aim of our study was to outline the reasons that contribute to non-maturation of potential donors into successful living donors and propose practical measures to improve the efficiency of the donor selection process.
Results
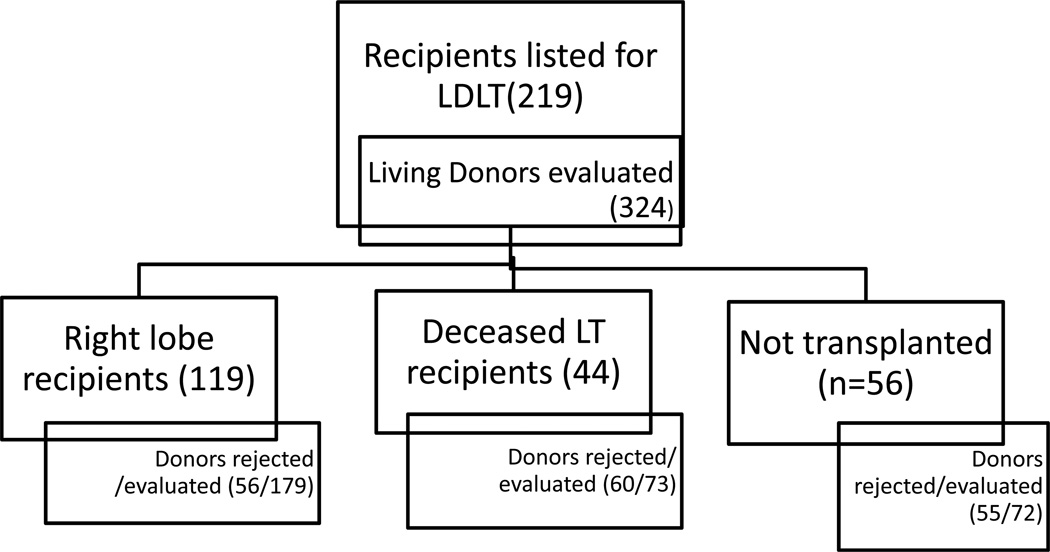
Since 1998, we evaluated 324 potential donors for 219 potential recipients. The outcomes of donor evaluation for patients that were listed for living donor liver transplantation are shown in figure 1. Of the 324 potential donors, 171 (52.7%) were rejected. There were 179 potential donors for 119 adult recipients who successfully received a right lobe living liver transplant and 56 donors (31.3%) were rejected. The donor rejection rate for patients who got a deceased donor liver transplant (n=44) was 82.2% while for patients who failed to receive a liver transplantation (n=56) 76.4% of the donors were turned down.
Figure 1.
Outcomes of donor evaluation in patients listed for living donor liver transplantation
The demographics of 119 donors who successful donated their right lobes were compared with those of 164 rejected donors (table 1, complete demographic data was not available for 7 rejected donors). A significantly higher proportion of older (age >50 vs. <50 years, p <0.03) and obese (BMI <25 vs. >25, p=0.005) candidates were turned down for donation as compared to donors who successfully donated. There were no differences in donor profiles between accepted and rejected donors for sex, race or relationship to potential recipient.
Table 1.
Demographics of accepted and rejected donors
| Accepted donors (n= 119) |
Rejected donors (n= 164) |
p-value | |
|---|---|---|---|
| Age <50 yr | 107 | 131 | |
| Age >50 yr | 12 (10.2%) | 33 (20.1%) | 0.03 |
| Males | 69 (57.9%) | 101 (61.5%) | |
| Females | 50 | 63 | 0.62 |
| Caucasian | 102 (85.6%) | 134 (81.7%) | |
| Non-Caucasian | 17 | 30 | 0.42 |
| BMI< 25 | 37 (31.6%) | 22 (16.4%) | |
| BMI ≥ 25 | 78 (68.4%) | 111 (83.6%) | 0.005 |
| Related | 75 | 99 | |
| Unrelated | 43 | 62 | 0.80 |
The reasons for disqualifying potential living liver donors along with the time-points at which they were rejected during the evaluation process are shown in table 2. The five most common reasons for donor disqualification included: (1) donor reluctance in 21%, (2) evidence of >10% macro-vesicular steatosis on a liver biopsy in 16%, (3) assisted donor withdrawal in 14%, (4) inadequate remnant liver volume in 13%, (5) poor psychosocial evaluation and thrombophilic conditions in 7% each, of the potential donors. Ten donors (6%) were turned down due to hilar anatomical variations. Approximately 15% of the donors were rejected early during step 1 of the evaluation process while 68% were turned down after step 2. Assisted medical withdrawal was the commonest cause (14%) for late rejections during step 3 or 4 of the evaluation process. Only 2% donations were aborted during the donor surgery.
Table 2.
Reasons for non-maturation of potential right liver lobe living donors
| Reasons for donor non- maturation |
Time-point during evaluation process¶ |
Donors (n=171) |
|---|---|---|
| Donor reluctance | Step 2 | 36 (21%) |
| Fatty liver (biopsy) | Step 2 | 28 (16%) |
| Assisted medical withdrawal | Step 3, 4 | 24 (14%) |
| Inadequate remnant liver volume (<30% of total) | Step 2 | 22(13%) |
| Psychosocial | Step 2 | 12 (7%) |
| Hypercoagulable states | Step 1 | 12 (7%) |
| Anatomical variations | Step 2 or 3 | 10 (6%) |
| Poor cardiac function | Step 2 | 8 (5%) |
| Blood group mismatch* | Step 1 | 6 (3 %) |
| Aborted donations | After step 4 | 4 (2%) |
| Hepatitis B core antibody positive | Step 1 | 2 (1%) |
| Diabetes | Step 1 | 1(<1%) |
| Obesity | Step 1 | 1(<1%) |
| Poor pulmonary function | Step 2 | 1(<1%) |
| Allergy to anesthetic drug | Step 1 | 1(<1%) |
| Elevated serum PTH | Step 1 | 1(<1%) |
This was detected at our institute since the initial blood group screening is done at primary care level prior to the telephonic interview with the transplant coordinator.
Refer to table 4 for details of the time-points during the evaluation process.
Of the 10 donors that were turned down due to anatomical reasons; 8 had bile duct variations: dorso-caudal branch of right hepatic duct crossing the midline and draining into the left hepatic duct (4 donors), dorso-caudal branch of right hepatic duct draining into the common hepatic duct (3 donors) and dorso-caudal duct draining into the confluence of right and left hepatic ducts with a short right hepatic duct (1 donor). One donor had intra-luminal occlusion of the celiac axis with collaterals to the liver from the superior mesenteric artery and another had celiac-hepatic artery stenosis detected on angiogram. No donor was rejected due to variations in hepatic or portal veins.
Discussion
We have shared our experience in selecting donors for adult- to- adult- living donor liver transplantation and discussed the important reasons resulting in non-maturation of potential donors. Based on this experience, we recommend a few prospective strategies (table 3) to further improve the selection process in living donor liver transplantation.
Table 3.
Problems and recommendations in selecting living liver donors
| Common problems | Recommendations |
|---|---|
| Donor ambivalence | Impartial donor advocate, interviews with previous living donors |
| Psychosocial causes leading to donor rejection and costly work-up | Earlier interview with dedicated transplant psychologist (at step 1 of evaluation instead of step 2, table 4) |
| Donor consent | Get two informed consents, consent to donate the liver lobe to a back-up recipient or for hepatocyte isolation in order to avoid ‘orphan liver lobe’ |
| Aborted surgeries | Avoid donors with upper abdominal surgeries especially during early ‘learning curve’, rule out hepatic steatosis pre-operatively in patients with BMI >25, detect bile duct variations on pre-operative MRCP, perform intra-operative cholangiogram, dedicated radiologist for accurate liver lobe volumetrics to avoid small-for-size syndrome |
| Deep venous thrombosis | Avoid donors with thrombophilic conditions, Enoxaparin for 6 weeks |
In our study, 52% of evaluations for right lobe donation resulted in disqualification. We did not include donors rejected on initial telephonic interview or donors rejected for recipient reasons. When these factors were included our rejection rate approached close to 80% and these are comparable to rejection rates (86%) from another study (8). In a multi-center study 60% of the donors were rejected (606/1011) and there was a wide variation in the donor rejection rates between the nine evaluating centers. Pascher et al. (9) found distinct contraindications in 29% (26/89) of their right lobe donors in Germany compared to 52% (171/324) at our center. These included steatosis >10% in 16, psychological contraindications in 7, one vascular variation (replaced right and left hepatic arteries with predominant perfusion of the left lobe via the right hepatic artery and intrahepatic collaterals), one heterozygous factor V deficiency (Leiden mutation) and one donor with hepatitis B. The top five reasons for donor disqualification at our center included (table 3): (a) donor reluctance (b) evidence of >10% macro-vesicular steatosis on a liver biopsy (c) assisted donor withdrawal (d) inadequate remnant liver volume (e) failed psychosocial evaluation and thrombophilic conditions.
Living donor evaluation must ensure that the donors are ‘competent’ to make a decision and that decision is made voluntarily without any coercion. We do not consider donor ambivalence as a reason for disqualification but reluctant donors are turned down at our center. In our experience, younger donors may particularly wane during the evaluation process and thus require additional scrutiny. Psychosocial contraindications were seen in 7% of our potential donors and 2.4% (10) and 5% (7) of the donors in other studies. The incidence of psychiatric complications after right lobe donation ranges between 4–10% (7). Highly motivated donors may conceal their underlying psychopathology that can result in devastating consequences (suicide/attempted suicides) for the donor (11). At our center, one donor committed suicide seven years after an uneventful donation and one altruistic donor had recurrent factitious wound infections (12). The costs for these admissions after liver lobe donation were billed to the recipient, creating a threat to the recipient's lifetime benefits. Therefore, potential donors with significant psychiatric issues are routinely rejected and provided health care referral and resources by our hospital approved agreement.
Evidence of >10% macro-vesicular steatosis on a liver biopsy resulted in 16% of potential donors being disqualified at our center compared to 18% (9) and 22% (10) in other studies. It has been hypothesized that each percentage of fat in the donor graft decreases its functional mass by 1% (13) and may also disrupt the microcirculation or alter the cell membrane fluidity (14). One donor surgery at our center was aborted due to detection of >30% macro-vesicular steatosis intra-operatively. We now perform a pre-operative liver biopsy only in a sub-group of potential right lobe liver donors who have: (a) high BMI, (b) suspected steatosis on imaging, and (c) elevated aminotransferases (15). While there is a significant correlation between BMI and degree of hepatic steatosis, 74% of overweight donors (BMI >25) had 0–10% steatosis in one series (16). Ultrasound and computerized tomography of the liver also have limited (80%) sensitivity to detect >30% hepatic steatosis in comparison to a liver biopsy (16).
Calculated inadequate remnant liver volume was the cause of disqualification in 13% of our potential right liver lobe donors. Concerns for inadequate residual liver volume resulted in disqualification of 19.5% (10) and 31% (8) of the donors in two other studies while none of the donors were turned down for this reason by Pascher et al. (9) and Trotter et al. (17). While a graft-to-recipient body weight ratio of < 0.8 increases the risk of graft loss in the recipient, an inadequate residual volume (<35% of total liver volume or residual liver volume < 50% of donor body weight) in the healthy donor is not an acceptable option (15).
Hypercoagulable states (Factor V Leiden, pro-thrombin mutation G20210A, anti-thrombin III and protein C & S deficiencies, Factor VIII elevation, anti-phospholipid or anti-cardiolipin antibodies) are relative contraindications at some centers for donation for fear of increase donor mortality from pulmonary emboli or significant morbidity of portal vein or hepatic artery thrombosis (18). We have rejected twelve candidates (7%) due to abnormalities in hemostatic profiles: five with factor V Leiden, three with anti-cardiolipin antibodies and four having homocysteinemia. In-addition, all our donors are started on enoxaparin (0.5 to 1.5 mg/kg body weight, subcutaneously once daily for 6 weeks) on the first post-operative day for deep vein thrombosis prophylaxis.
In a multi-center study, 11% of donors in United States had anatomical contraindications to donation (7) similar to the 10% in a study from Taiwan (19). Hepatic arterial variations were observed in 57%, portal and hepatic venous variations in 42% each and right hepatic duct variations were seen in 60% of our successful donors (data not shown). We rejected 10 potential donors due to anatomical reasons that we perceived as ‘high risk’ for the donor. None of our donors were turned down due to portal or hepatic venous variations. Biliary complications in the donor and recipient remain the Achilles heel in LDLT and ‘classical’ biliary anatomy of the intra-hepatic bile ducts may be observed in only two-thirds of the potential donors (20). Most biliary variants are not a contraindication to donation. However, some including a right hepatic duct branch draining into the left hepatic duct or into the common hepatic duct or a dorso-caudal duct draining into the confluence of right and left hepatic ducts in presence of a short right hepatic duct, deserve special consideration (21). Identification of these variants before liver resection helps prevent accidental ligation of bile duct branches draining the right hepatic lobe or the remnant lobe that could lead to atrophy of the involved portions of the liver.
Aborted donations have been considered by some authors as non-maturation of donors since the donor evaluation continues until the right lobe is taken out. The donor surgery had to be aborted in four instances (2%) at our center. Two donor surgeries were aborted due to dense adhesions secondary to a previous cholecystectomy. One donor had significant macro-vesicular steatosis (>30%) detected on intra-operative liver biopsy. In another case the recipient decompensated secondary to refractory arrhythmias and left ventricle global dyskinesia. Transplant was abandoned and the patient died post-operatively. In this case, the donor right lobe had intact vascularity and the bile duct was reconstructed using roux-en-Y jejunostomy. Since then all our potential donors are consented to donate the right lobe to the next recipient on the list or for hepatocyte isolation, in order to avoid an ‘orphan graft’ in the unfortunate event of intra-operative decompensation or death of the intended recipient. Our strategies in dealing with some common practical problems during donor selection are summarized in table 3 and these have enabled us to improve the efficacy and cost-effectiveness of our donor selection process for LDLT.
Refinement of methods to identify reasons for donor rejection earlier during the course of the evaluation process would make the evaluation process (table 4) more time and cost-effective. In our analysis, assisted medical withdrawal was the commonest cause (14%) for late rejection of donors (step 3 or 4). These could be minimized by early recognition of donors with ambivalence and reluctance by a team of experienced transplant coordinators, dedicated social worker and transplant psychologist. Out of the 15% donors that were rejected after step 1 of the evaluation process, about 10% could have been excluded by performing the relevant laboratory testing (blood group, blood sugars, hypercoagulation workup) with their primary care physician. A majority of donors (68%) were turned down after step 2 of the evaluation process and a few strategies to reduce these are summarized in table 3. Aborted donations (2%) could be further minimized by avoiding donors with history of upper abdominal surgeries, especially during the learning curve of LDLT.
Table 4.
Evaluation protocol for potential right lobe liver donors
| Step 1 | First informed consent Clinical evaluation: history and physical examination (transplant coordinator) Laboratory: blood group; hematologic tests; chemistry 12; glucose tolerance test*; coagulation profile; protein C; anti-thrombin III; factor V, VII and VIII; C-reactive protein; thyroid function test (TSH, T3, T4); substances of abuse panel Serology: hepatitis A,B (surface Ag, core Ab, surface Ab) and C Imaging studies: chest radiograph (PA and lateral), abdominal ultrasound |
| Step 2 | Clinical evaluation (transplant hepatologist), psychological evaluation, discussion with donor advocate Laboratory: HLA typing, cross-match, alpha1-antitrypsin, transferrin, ferritin, tumor markers (AFP, CEA), urine sediment, pregnancy test Serology: CMV IgG and IgM, HSV, EBV IgG and IgM, VDRL test, HIV (PCR) Imaging studies: MRI with liver volume measurement, MRA, MRC Special studies: pulmonary function tests, ECG, echocardiography, stress test* Histology: liver biopsy |
| Step 3 | Imaging studies: celiac angiography with portal phase |
| Step 4 | Clinical evaluation: planning of surgical date and availability of ICU facilities Blood bank: autologous blood donation Second informed consent, blood transfusion consent |
Abbreviations: TSH, thyroid-stimulating hormone; T3, triiodothyronine; T4, thyroxine; Ag, antigen; Ab, antibody; PA, postero-anterior; AFP, alphafetoprotein; CEA, carcinoembryonic antigen; CMV, cytomegalovirus; IgG, immunoglobulin; HSV, herpes simplex virus; EBV, Ebstein-Barr virus; VDRL, Venereal Disease Research Laboratory; HIV, human immunodeficiency virus; PCR, polymerase chain reaction; MRI, magnetic resonance imaging; MRA, magnetic resonance angiography; MRC, magnetic resonance cholangiography; ECG, electrocardiogram; ICU, intensive care unit.
Only performed if indicated.
One of the drawbacks of this descriptive study is its retrospective nature. While our study provides an overview of the evaluation process and summarizes our experience, details about each step and complications in donors were beyond the scope of this discussion. We also recognize that excessive defense for the healthy donor may deprive a potentially sick recipient the opportunity to get a liver transplant and survive.
We conclude that approximately one half of the potential right lobe donors are acceptable after thorough pre-operative medical, psychosocial and radiological evaluation. Older (> 50 years) and donors with BMI >25 are more likely to be turned down for donation. In this analysis, surgical anatomical variations were not a major reason for exclusion of potential donors for adult right lobe living liver donation. Since the medical center of evaluation (4) is one of the strongest predictors of donor acceptance (and hence outcomes), each center should be encouraged to periodically review and improve their living donor selection practices.
Materials and Methods
Study subjects
The study protocol was approved by the Institutional Review Board. Between January 1998 and December 2010, 324 potential donors were evaluated at our center for 219 potential living donor liver transplant recipients. Only those donors who cleared the initial telephonic interview with the transplant coordinator and underwent further evaluation were considered for this analysis. Outcomes of donor evaluation from 1998 to 2003 were previously included in the A2ALL publication by Trotter et al. on this subject (7).
Donor evaluation
The steps in the donor evaluation process at our center have been described in detail earlier (22) and are summarized in table 4. Briefly, the evaluation process typically begins with the potential candidate contacting a dedicated liver transplant coordinator. The intended recipient must be listed with United Network for Organ Sharing (UNOS) prior to donor evaluation. The initial donor exclusion criteria at this time include age <18 years, blood group incompatibility, obesity (body mass index >30kg/m2), significant medical co-morbidity or upper abdominal surgery.
Although some centers require that the potential donor should be genetically or emotionally related to the recipient, we will accept Good Samaritan donors after a third party donor advocate excludes any evidence of financial gain (23). During the subsequent interactions complete information is provided about the evaluation process, the surgery and its complications and the expected outcomes, both for the donors and the recipients. The length of disability, its effects on donor’s financial and social responsibilities is discussed in detail by an expert member of the evaluation team.
Donor consent
The inclusion of a consent form, which is mailed to the potential donors a few days before surgery, ensures that candidates have ample time before making a final decision to donate. In addition at step 2 of evaluation (table 4); we encourage all potential donors to interview with past donors who have volunteered to offer their experience, thus serving as donor advocates (23).
Psychosocial evaluation
Psychosocial evaluation of the donors (24) includes assessment of their overall understanding of the entire donation process. Donors are evaluated for presence or absence of past and present psychiatric disorders including substance abuse and to rule out any financial incentives or other ulterior motives (e.g. publicity) to donate. Active smokers who pass all other criteria are medically aided to quit smoking, with two months of abstinence before the right lobe liver donation. In female donors, oral contraceptive cessation along with counseling for an alternative method is encouraged four weeks prior to surgery.
Donor ambivalence (simultaneous and contradictory attitudes and/feelings towards a person or an action) and reluctance (a consistent unwillingness to donate) may be part of the decision making process for any potential donor. Any donor ambivalence perceived by the evaluating team is addressed by the social worker, psychologist and the transplant coordinator. In our practice, we do not consider ambivalence to be a contraindication to donation but reluctant donors are excluded (25).
Every attempt is made to ensure that there is no coercion (the imposition of the will of another person such as a family member or the recipient on the donor candidate) for donation. Some potential donors, without any perceived ambivalence or reluctance, may later feel that they cannot gracefully withdraw especially when the evaluation process has progressed considerably. Such donors who choose to back out at any stage of the evaluation process are provided a ‘medical excuse’ (assisted medical withdrawal).
Donor outcomes
Chart reviews were done to study the reasons for non-maturation of potential right lobe living donors. Although some donors had more than one reason for disqualification, for data analysis purposes, we considered only the reason that was most singled out by the donor evaluation committee. The following were not considered as disqualifications during evaluation: donors whose recipients got a deceased donor liver transplant during donor work-up, donors whose recipients either improved or expired during evaluation or back-up donors not fully evaluated. We have included aborted donations as a reason for non-maturation since the donor continues to be evaluated intra-operatively till the liver lobe is procured for transplantation.
Statistical analysis
Data retrieved from divisional databases was collaborated by medical chart review. Data are reported as mean ± standard deviation. Categorical data was compared using the Chi-square test and continuous data were compared with a Student’s t-test. A probability of <0.05 was considered to be statistically significant.
Acknowledgements
This project was supported by award number U01DK062531 from the National Institute of Diabetes And Digestive And Kidney Diseases.
Abbreviations
- LDLT
living donor liver transplantation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflict of interest.
References
- 1.Berg CL, Gillespie BW, Merion RM, et al. Improvement in survival associated with adult-to-adult living donor liver transplantation. Gastroenterology. 2007;133(6):1806. doi: 10.1053/j.gastro.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verna EC, Hunt KH, Renz JF, et al. Predictors of candidate maturation among potential living donors. Am J Transplant. 2005;5(10):2549. doi: 10.1111/j.1600-6143.2005.01066.x. [DOI] [PubMed] [Google Scholar]
- 3.Miller C, Florman S, Kim-Schluger L, et al. Fulminant and fatal gas gangrene of the stomach in a healthy live liver donor. Liver Transpl. 2004;10(10):1315. doi: 10.1002/lt.20227. [DOI] [PubMed] [Google Scholar]
- 4.Brandhagen D, Fidler J, Rosen C. Evaluation of the donor liver for living donor liver transplantation. Liver Transpl. 2003;9(10 Suppl 2):S16. doi: 10.1053/jlts.2003.50222. [DOI] [PubMed] [Google Scholar]
- 5.Rudow DL, Brown RS., Jr. Evaluation of living liver donors. Prog Transplant. 2003;13(2):110. doi: 10.1177/152692480301300207. [DOI] [PubMed] [Google Scholar]
- 6.Trotter JF. Selection of donors for living donor liver transplantation. Liver Transpl. 2003;9(10 Suppl 2):S2. doi: 10.1053/jlts.2003.50221. [DOI] [PubMed] [Google Scholar]
- 7.Trotter JF, Wisniewski KA, Terrault NA, et al. Outcomes of donor evaluation in adult-to-adult living donor liver transplantation. Hepatology. 2007;46(5):1476. doi: 10.1002/hep.21845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valentin-Gamazo C, Malago M, Karliova M, et al. Experience after the evaluation of 700 potential donors for living donor liver transplantation in a single center. Liver Transpl. 2004;10(9):1087. doi: 10.1002/lt.20223. [DOI] [PubMed] [Google Scholar]
- 9.Pascher A, Sauer IM, Walter M, et al. Donor evaluation, donor risks, donor outcome, and donor quality of life in adult-to-adult living donor liver transplantation. Liver Transpl. 2002;8(9):829. doi: 10.1053/jlts.2002.34896. [DOI] [PubMed] [Google Scholar]
- 10.Pomfret EA, Pomposelli JJ, Gordon FD, et al. Liver regeneration and surgical outcome in donors of right-lobe liver grafts. Transplantation. 2003;76(1):5. doi: 10.1097/01.TP.0000079064.08263.8E. [DOI] [PubMed] [Google Scholar]
- 11.Trotter JF, Hill-Callahan MM, Gillespie BW, et al. Severe psychiatric problems in right hepatic lobe donors for living donor liver transplantation. Transplantation. 2007;83(11):1506. doi: 10.1097/01.tp.0000263343.21714.3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levenson JL, Valverde R, Olbrisch ME. Factitious wound infections in an altruistic living liver donor. Prog Transplant. 2008;18(1):22. doi: 10.1177/152692480801800106. [DOI] [PubMed] [Google Scholar]
- 13.Marcos A, Ham JM, Fisher RA, Olzinski AT, Posner MP. Single-center analysis of the first 40 adult-to-adult living donor liver transplants using the right lobe. Liver Transpl. 2000;6(3):296. doi: 10.1053/lv.2000.6354. [DOI] [PubMed] [Google Scholar]
- 14.Fukumori T, Ohkohchi N, Tsukamoto S, Satomi S. The mechanism of injury in a steatotic liver graft during cold preservation. Transplantation. 1999;67(2):195. doi: 10.1097/00007890-199901270-00002. [DOI] [PubMed] [Google Scholar]
- 15.Brown RS, Jr., Russo MW, Lai M, et al. A survey of liver transplantation from living adult donors in the United States. N Engl J Med. 2003;348(9):818. doi: 10.1056/NEJMsa021345. [DOI] [PubMed] [Google Scholar]
- 16.Ryan CK, Johnson LA, Germin BI, Marcos A. One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transpl. 2002;8(12):1114. doi: 10.1053/jlts.2002.36740. [DOI] [PubMed] [Google Scholar]
- 17.Trotter JF, Wachs M, Trouillot T, et al. Evaluation of 100 patients for living donor liver transplantation. Liver Transpl. 2000;6(3):290. doi: 10.1002/lt.500060323. [DOI] [PubMed] [Google Scholar]
- 18.Mas VR, Fisher RA, Maluf DG, Wilkinson DS, Garrett CT, Ferreira-Gonzalez A. Hepatic artery thrombosis after liver transplantation and genetic factors: prothrombin G20210A polymorphism. Transplantation. 2003;76(1):247. doi: 10.1097/01.TP.0000072017.19075.2E. [DOI] [PubMed] [Google Scholar]
- 19.Tsang LL, Chen CL, Huang TL, et al. Preoperative imaging evaluation of potential living liver donors: reasons for exclusion from donation in adult living donor liver transplantation. Transplant Proc. 2008;40(8):2460. doi: 10.1016/j.transproceed.2008.07.075. [DOI] [PubMed] [Google Scholar]
- 20.Huang TL, Cheng YF, Chen CL, Chen TY, Lee TY. Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc. 1996;28(3):1669. [PubMed] [Google Scholar]
- 21.Fulcher AS, Szucs RA, Bassignani MJ, Marcos A. Right lobe living donor liver transplantation: preoperative evaluation of the donor with MR imaging. AJR Am J Roentgenol. 2001;176(6):1483. doi: 10.2214/ajr.176.6.1761483. [DOI] [PubMed] [Google Scholar]
- 22.Marcos A, Fisher RA, Ham JM, et al. Selection and outcome of living donors for adult to adult right lobe transplantation. Transplantation. 2000;69(11):2410. doi: 10.1097/00007890-200006150-00034. [DOI] [PubMed] [Google Scholar]
- 23.Fisher RA. Enabling altruism: evaluating the adult living liver donor. Liver Transpl. 2007;13(4):478. doi: 10.1002/lt.21012. [DOI] [PubMed] [Google Scholar]
- 24.Dew MA, Jacobs CL, Jowsey SG, Hanto R, Miller C, Delmonico FL. Guidelines for the psychosocial evaluation of living unrelated kidney donors in the United States. Am J Transplant. 2007;7(5):1047. doi: 10.1111/j.1600-6143.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- 25.Simpson MA, Kendrick J, Verbesey JE, et al. Ambivalence in living liver donors. Liver Transpl. 17(10):1226. doi: 10.1002/lt.22342. [DOI] [PubMed] [Google Scholar]