Abstract
We established a model of chronic portal vein catheterization in an awake nonhuman primate to provide a comprehensive evaluation of the metabolic response to low-carbohydrate/high-fat (LCHF; 20% carbohydrate and 65% fat) and high-carbohydrate/low-fat (HCLF; 65% carbohydrate and 20% fat) meal ingestion. Each meal was given 1 wk apart to five young adult (7.8 ± 1.3 yr old) male baboons. A [U-13C]glucose tracer was added to the meal, and a [6,6-2H2]glucose tracer was infused systemically to assess glucose kinetics. Plasma areas under the curve (AUCs) of glucose, insulin, and C-peptide in the femoral artery and of glucose and insulin in the portal vein were higher (P ≤ 0.05) after ingestion of the HCLF compared with the LCHF meal. Compared with the LCHF meal, the rate of appearance of ingested glucose into the portal vein and the systemic circulation was greater after the HCLF meal (P < 0.05). Endogenous glucose production decreased by ∼40% after ingestion of the HCLF meal but was not affected by the LCHF meal (P < 0.05). Portal vein blood flow increased (P < 0.001) to a similar extent after consumption of either meal. In conclusion, a LCHF diet causes minimal changes in the rate of glucose appearance in both portal and systemic circulations, does not affect the rate of endogenous glucose production, and causes minimal stimulation of C-peptide and insulin. These observations demonstrate that LCHF diets cause minimal perturbations in glucose homeostasis and pancreatic β-cell activity.
Keywords: stable isotope tracers, portal vein catheterization, β-cell function
the typical diet in the US provides ∼50% of ingested calories as carbohydrate, 35% as fat, and 15% as protein (4). However, data from several studies have shown that a low-carbohydrate diet containing 35–40% of calories as carbohydrate can have therapeutic effects in patients with type 2 diabetes by lowering plasma glucose, triglyceride, and very low-density lipoprotein (VLDL) cholesterol, by increasing plasma high-density lipoprotein (HDL) cholesterol concentrations, and by decreasing insulin requirements (17–19). In addition, low-carbohydrate diets are often used to help induce weight loss in obese people (15). Although the use of low-carbohydrate diets continues to be a popular dietary therapy, the metabolic response to high- and low-carbohydrate meals has not been carefully evaluated.
The metabolic response to a meal is carefully coordinated among several organ systems to prevent large excursions in plasma glucose concentration and to deliver ingested nutrients to appropriate tissues for storage or utilization. The normal regulation of postprandial plasma glucose involves an increase in insulin secretion from pancreatic β-cells into the portal vein, insulin-mediated suppression of endogenous (primarily hepatic) glucose production, and insulin-mediated stimulation of glucose uptake by peripheral tissues (primarily skeletal muscle). In fact, abnormalities in plasma glucose concentration after an oral glucose load is ingested are used as a clinical tool to diagnose impaired glucose tolerance and type 2 diabetes (3).
After meal ingestion, glucose consumed in the meal and insulin secreted from the pancreas are delivered directly into the portal vein for transport to the liver. Accordingly, the ability to sample portal vein blood is important for understanding postprandial metabolic regulation. Several studies conducted in animal models have used portal vein catheterization to evaluate the effect of intraportal nutrient delivery on hepatic and whole body metabolism (11, 43, 49). However, we are not aware of any studies that have used portal vein catheterization to evaluate the effect of differences in dietary macronutrient composition on the metabolic response to a meal.
The purpose of the present study was to establish a chronic portal vein catheterization model in an awake nonhuman primate to assess the metabolic responses to a high-carbohydrate/low-fat (HCLF) and low-carbohydrate/high-fat (LCHF) meal. These experiments were performed in baboons because of their similarity to humans, thereby reducing the chance of a confounding effect of interspecies differences in our assessment of metabolic outcomes (6, 7, 33, 34). The metabolic response to each meal was evaluated by using stable, isotopically labeled tracer methods in conjunction with mathematical modeling to assess glucose kinetics and insulin secretion.
METHODS
Animals.
Five young adult (7.8 ± 1.3 yr old) male baboons (Papio hamadryas Sp.) were studied. Prior to the study, animals were housed in groups in outdoor enclosures in the Southwest National Primate Research Center (SNPRC; San Antonio, TX) according to established National Research Council guidelines. A licensed veterinarian performed a standard health assessment, including a physical examination and serum chemistry and hematology profiling in all animals before their participation in this study. All animals were considered to be healthy, and none had any history of medical illness.
For this study, all animals were housed individually in indoor facilities at the SNPRC. In order for animals to acclimate to the indoor laboratory conditions, they were housed in large individual aluminum cages inside the facility, which was kept at constant room temperature and humidity in a 12:12-h light-dark cycle for 7 days before the experimental protocol began. During this period, the animals were also habituated to the presence of the tether jacket and coil system (9). Each animal was fitted to a cotton tether jacket connected to a stainless-steel coil via a molded plastic box attached to the rear of the jacket. The stainless-steel coil provided a conduit through which blood sampling lines, infusion lines, and flow probe monitor wiring were later passed from the animal to the sampling, infusion, and recording equipment at the top of the cage. Animals were fed a standard nonhuman primate diet (5LE0 solid feed, LabDiet; PMI, St. Louis, MO) ad libitum and had continuous access to water. All study procedures were submitted to and approved by the Institutional Animal Care and Use Committee of the Texas Biomedical Research Institute, San Antonio, TX.
Catheters and flow probe placement.
One week after indoor housing and tether jacket acclimation, laparotomy was performed under general anesthesia to implant a polyurethane catheter (5 Fr Hydrocoat; Access Techonologies, Skokie, IL) in the portal vein and to place a 6-mm-diameter perivascular flow probe (MC6PSS ultrasound transit time chronic flow probe; Transonic Systems, Ithaca, NY) on the portal vein. Animals were sedated with ketamine HCl (10 mg/kg im), and gas anesthesia was induced and maintained by using isoflurane (1.5%). During surgery, animals were given a prophylactic analgesic (0.2 mg/kg Metacam) and prophylactic antibiotic (25 mg/kg cephazolin). The probe was fitted around the vessel so that the vessel would lie in the space between the probe body and the reflector piece without impeding blood flow through the portal vein. The location of the flow probe and integrity of the portal vasculature and surrounding tissue was confirmed by fluoroscopy immediately after implantation. The catheters and flow probe were routed subcutaneously to the midscapular region of the back, where they exited the skin into a molded plastic box (backpack) attached to a tether jacket. Catheters were then implanted in the femoral artery and vein (5 Fr Hydrocoat; Access Technologies) via a skin incision over the femoral vessels in the femoral triangle of the inner thigh. These catheters were also routed subcutaneously to the midscapular region of the back to exit the skin at the location of the tether jacket backpack box.
After surgery, analgesic (0.01 mg/kg qid buprinex for 3 days) and prophylactic antibiotic treatments (25 mg/kg bid cephazolin for 7 days) were provided. In addition, a single dose of midazolam (0.1 mg/kg) was administered intravenously after the animals regained consciousness after surgery. Parenteral nutrition support was also provided after the surgery and was continued for ≤96 h until the animals began to eat solid foods. Catheters were kept patent by using continuous heparinized saline (5 U/ml) infusion from volumetric infusion pumps maintained at the top of the cage, as described previously (9).
Acclimation of the animals to the presence of a technician was conducted at regular intervals for 4 wk after surgery. In addition, food and water intake were monitored daily, and animals were sedated weekly (10 mg/kg ketamine) to perform health assessments, which included a physical examination, inspection of catheter and flow probe exit sites, body weight measurement, and routine blood tests. The flow probe cabling was extended ∼12 m from the cage top to an adjacent monitoring room to connect to a three-channel transit time flow meter (TS403 Console with TS420 Perivascular Flow Meter Modules; Transonic Systems). The flow probes were precalibrated with a specified calibration gain programmed into a calibration key sent directly from the manufacturer. Manufacturer-recommended performance testing of the received signal was undertaken weekly by using the flow meter's test mode. The received signal testing was conducted across the range of measured voltage. Chronic portal flow measurements were recorded and logged using the Ponemah Physiology Platform with P3 Plus Software for Windows (LDS Test Measurement and Gould Instrument Systems, Valley View, OH). All animals adapted well to the tether system, had normal food and water intakes, and were weight stable before initiation of the mixed-meal metabolic studies.
Body composition.
Three weeks after placement of catheters and flow probe, animals were sedated with ketamine HCl (10 mg/kg) to assess body composition. Body weight was measured by using an electronic scale (GSE 665; Texas Scales, Cibolo, TX). Total body fat mass and fat-free mass were determined by using dual-energy X-ray absorptiometry (Lunar Prodigy densitometer; GE Healthcare, Madison, WI). Animals were placed in the supine position on the dual-energy X-ray absorptiometry bed, and extremities were positioned within the scanning region. Scans were analyzed by using encore2007 software version 11.40.004 (GE Healthcare).
Mixed-meal metabolic study.
Two mixed-meal metabolic studies (LCHF and HCLF) were performed ∼1 wk and again ∼2 wk after body composition was determined. Animals were randomized to receive either a 350-kcal HCLF (65% of calories as carbohydrates, 15% as protein, and 20% as fat) or a 350-kcal LCHF (20% of calories as carbohydrate, 15% as protein, and 65% as fat) meal at each study. The calorie content and macronutrient composition of each of the two test meals were chosen to 1) provide isocaloric meals that contained about one-third of the animals' daily energy requirements and 2) provide a large range in carbohydrate loads, representing the macronutrient content of a low-carbohydrate diet (e.g., the Atkins diet) and a conventional low-fat diet (1, 2) used to treat obesity to maximize the differences in β-cell response and glucose metabolism elicited by each meal. The HCLF meal was prepared by using crushed brown rice krispies, water, glucose powder, butter, and whey protein isolate. Glucose powder (53 g) was dissolved in heated water to form a syrup, and [U-13C]glucose tracer (2% of total glucose content) was added and dissolved in this syrup. The solution was mixed by using a magnetic stirring rod and sonicated to ensure homogeneity. Butter (9.9 g), whey protein (14 g), and crushed brown rice krispies (8.5 g) were then added to the solution (56.9 g total carbohydrate), and the ingredients were mixed by using a spatula. The mixture was then allowed to solidify and refrigerated at 4°C until used the following day. The LCHF meal was prepared by using butter, smooth peanut butter, honey crackers, whey protein, and dextrose. Glucose powder (9.4 g) was dissolved in heated water to form a syrup, and a [U-13C]glucose tracer (10% of total glucose) was added and dissolved in this syrup. This solution was mixed by using a magnetic stirring rod and sonicated to ensure homogeneity. Butter (17.5 g), crushed honey crackers (5 g), whey protein (8.1 g), and smooth peanut butter (22 g) were added to the syrup solution (17.5 g total carbohydrate), and the ingredients were mixed by using a spatula and refrigerated at 4°C until they were used for the study the following day.
At 0700 on the day before the mixed meal, the heparinized saline infusion was discontinued, and 0.45% saline was infused at 20 ml/h to keep catheters patent. The following day, the mixed-meal metabolic study was performed. Low-dose midazolam was infused intravenously as needed to ensure that the animals were awake but resting quietly in the study cage. At 0800, a primed continuous infusion of [6,6-2H2]glucose (priming dose: 22 μmol/kg; infusion rate: 0.22 μmol·kg−1·min−1) was administered through the femoral vein catheter and continued for 9 h. After 3 h of isotope tracer infusion (basal period), animals were randomized to receive either the HCLF or the LCHF test meal, which was always completely consumed within 20 min. Approximately 1 wk later, the mixed-meal metabolic study was repeated using the alternate meal.
Blood samples during the mixed-meal metabolic studies were obtained through the tether catheter lines, which had a dead space volume of 1.5 ml. Thirty seconds before each blood sample was taken, the dead space was cleared by withdrawing blood into a 3-ml syringe containing heparinized saline. This sample was reinfused into the animal after the study blood sample was obtained. The draw time for the study blood sample was ∼30 s. A blood sample (containing 1.0–2.5 ml) was obtained from the femoral artery before the beginning of the isotope infusion to and from the femoral artery and portal vein every 10 min during the last 20 min of the basal period, every 15 min for the first hour after the meal, and every 20 min during the 2nd through 6th hours after the meal to determine plasma glucose, insulin, and C-peptide concentrations and [6,6-2H2]- and [U-13C]glucose tracer/tracee ratio (TTR). A total of 87 ml of blood, 44 ml from the artery and 43 ml from the portal vein, was withdrawn from each animal during each study.
Portal vein blood flow was recorded continuously during the mixed-meal metabolic studies. Once in position and activated, the ultrasound circuitry directed alternate emissions of ultrasonic plane waves from the upstream and downstream transducers. The upstream beam completely traversed the vessel, was reflected by the reflector piece on the other side, and traversed the vessel again and was detected by the downstream transducer. The time required for the beam to reach the upstream transducer to the downstream transducer was recorded by the flow meter. Immediately, another ultrasonic beam was released from the downstream transducer, reflected, and detected by the upstream transducer. This transit time was proportional to the volume flow that intersected the beam. The flow rate was calculated as the difference between the upstream and the downstream transit times and was converted to a DC voltage directly proportional to blood flow by the flow meter. This approach enabled direct assessments of volumetric flow that were unaffected by changes in vessel diameter and probe misalignment. The portal vein blood flow signal was digitized continuously by the Ponemah software throughout the entire 9 h of the mixed-meal metabolic study; values were averaged over 10-min intervals.
Analyses of blood samples.
Plasma glucose concentration was determined by using the glucose oxidase method (Autokit Glucose; Wako Diagnostic, Richmond, VA) with an automated glucose analyzer. Plasma C-peptide and insulin concentrations were measured by using human enzyme-linked immunosorbent assays (Millipore, Billerica, MA). These assays are used to measure baboons' C-peptide and insulin concentrations because of the homology between human and baboon amino acid sequences for these molecules. Cholesterol, triglycerides, and liver enzymes were analyzed according to standardized methodology on an automated analyzer (Cobas Mira; Roche Diagnostic Systems, Nutley, NJ) (23).
Plasma glucagon concentrations were measured by using an enzyme-linked immunosorbent assays (R & D Systems, Minneapolis, MN). Free fatty acid (FFA) concentrations were measured by colorimetric assay (Wako Diagnostic). Plasma glucose TTR was determined by using electron impact ionization gas chromatography-mass spectrometry (MSD 5973 system with capillary column; Hewlett-Packard, Palo Alto, CA) as we have described previously (30).
Calculations.
Plasma glucose, insulin, and glucagon areas under the curve (AUC), C-peptide, insulin secretion rate (ISR), incremental AUC (iAUC) over baseline levels were calculated by using the trapezoid method (45) over the 6 h (3 h for glucagon) after meal consumption. ISRs were derived by using stochastic deconvolution of the peripheral C-peptide concentrations, as described previously (40, 41, 46). The assumed C-peptide clearance kinetics parameters (46) were based on that of a middle aged (35 yr) man with normal glycemic control, using each individual animal's body surface area. Total, endogenous, and ingested (meal) glucose rates of appearance (Ra) were calculated by using arterial glucose concentrations and enrichments as reported previously (21) based on Steele's equation for non-steady-state conditions (42). Before applying Steele's equation, plasma glucose concentration and TTR data were smoothed to stabilize the calculation of the derivative of enrichment (21). Oral glucose Ra was determined in a similar manner using portal vein concentrations and enrichments, and hepatic glucose extraction was calculated by subtracting arterial oral glucose Ra from portal vein oral glucose Ra.
Statistical analyses.
All data were tested for normality according to Shapiro-Wilk. Student's paired t-test was used to evaluate differences in AUC for glucose, insulin, C-peptide, and glucagon between HCLF and LCHF meals and/or between arterial and portal venous blood. A one-tailed t-test was used based on the assumption that the HCLF would elicit a greater increase in glucose and insulin concentrations than the LCHF meal. Repeated measures of variance with two within-subject factors (meal test and time or artery/portal vein and time) were used to compare differences in plasma FFA, glucose kinetics, and portal vein blood flow between HCLF and LCHF diet conditions. A P value of ≤0.05 was considered statistically significant. All data are presented as means ± SD, unless otherwise indicated.
RESULTS
Metabolic characteristics and body composition.
Total body fat mass was 4–5% of total body mass, which represents a normal amount of fat mass for these animals (Table 1). Glucose, total cholesterol, triglycerides, and liver enzymes were all in the normal range (Table 1).
Table 1.
Individual characteristics of the 5 animals
| Animal | 1 | 2 | 3 | 4 | 5 | Average |
|---|---|---|---|---|---|---|
| Body weight, kg | 28.1 | 29.5 | 28.9 | 28.8 | 27.5 | 28.6 ± 0.8 |
| Fat mass, kg | 1.1 | 1.3 | 1.4 | 1.1 | 1.3 | 1.3 ± 0.1 |
| Fat mass, %body weight | 3.9 | 4.3 | 5.0 | 4.0 | 4.7 | 4.4 ± 0.5 |
| Fat-free mass, kg | 25.6 | 26.5 | 25.8 | 26.24 | 25.0 | 24.9 ± 0.6 |
| Glucose, mmol/l | 5.3 | 4.3 | 4.4 | 5.0 | 4.8 | 4.8 ± 0.4 |
| Triglycerides, mmol/l | 0.5 | 0.7 | 0.7 | 0.3 | 0.3 | 0.5 ± 0.2 |
| Total cholesterol, mmol/l | 2.2 | 3.0 | 2.4 | 2.9 | 2.6 | 2.6 ± 0.3 |
| HDL cholesterol, mmol/l | 1.7 | 1.9 | 1.7 | 1.0 | 1.0 | 1.4 ± 0.4 |
| Alanine transaminase, U/l | 30 | 28 | 28 | 20 | 32 | 28 ± 5 |
| Aspartate aminotransferase, U/l | 41 | 16 | 22 | 22 | 21 | 24 ± 10 |
Average values are means ± SD.
Substrate and hormonal response to the meal.
The total AUCs of glucose and insulin were higher in both the femoral artery and the portal vein after ingestion of the HCLF compared with the LCHF meal (Fig. 1). The C-peptide and ISR in response to meal ingestion (measured as the iAUC over baseline) were higher in both the femoral artery and the portal vein after ingestion of the HCLF than the LCHF meal (Fig. 1). Glucagon AUC in both femoral artery and portal vein were greater after the LCHF than after the HCLF meal (P < 0.05) (Fig. 2). There was a significant diet-by-time interaction for the plasma FFA time course, suggesting a more prolonged suppression of adipose tissue lipolytic activity after the HCLF meal than after LCHF meal (P < 0.05; Fig. 3).
Fig. 1.

Plasma glucose, insulin, C-peptide, and insulin secretion rate (ISR), total area under the curve (AUC), or change from baseline [incremental AUC (iAUC)] in artery (top) and portal vein (bottom) for 6 h after a high-carbohydrate/low-fat (HCLF) or low-carbohydrate/high-fat (LCHF) meal. Data are presented individually for each animal (each line represents 1 animal) and as means ± SE of the whole group (cross-like bars). *Value different from LCHF meal value, P < 0.05.
Fig. 2.
Plasma glucagon AUC for 180 min in artery (left) and portal vein (right) after ingestion of either a HCLF or LCHF meal. Data are presented individually for each animal (each line represents 1 animal) and as means ± SE of the whole group (cross-like bars). *Value different from HCLF meal value, P < 0.05.
Fig. 3.
Time course of plasma free fatty acid concentrations in the systemic circulation (top) and portal vein (bottom) after ingestion of a HCLF or a LCHF meal. *Value different from HCLF meal value, P < 0.05. Data are presented as means ± SE.
Glucose kinetics in response to the meal.
There was a significant diet-by-time interaction for the Ra of ingested glucose into the systemic circulation and into the portal vein, endogenous glucose Ra, and total (both ingested and endogenous) glucose Ra (all P < 0.001), indicating that the HCLF and the LCHF meals had a different effect on these kinetic outcome measurements (Fig. 4). Compared with the LCHF meal, the Ra of ingested glucose into the systemic circulation and into the portal vein was significantly greater within 10 min after the HCLF meal consumption was initiated and remained higher throughout the entire study (P < 0.05; Fig. 4). Based on the difference in glucose appearance in the portal venous and arterial circulation, we calculated that hepatic extraction of glucose was 20 ± 5% after the HCLF meal and 7 ± 3% after the LCHF meal (P < 0.05). Ingestion of the HCLF meal decreased endogenous glucose Ra by ∼40% for several hours after meal ingestion (P < 0.05; Fig. 4), whereas the LCHF meal did not affect endogenous glucose production (Fig. 4). Total glucose Ra into the systemic circulation, which is comprised of both ingested and endogenously produced glucose, was higher after the ingestion of the HCLF than the LCHF meal (P < 0.05; Fig. 4).
Fig. 4.

The rate of appearance (Ra) of ingested glucose into the systemic circulation (top left) and into the portal vein (bottom left), total glucose Ra into the systemic circulation (top right), and endogenous glucose Ra (bottom right) after ingestion of either a HCLF or a LCHF meal. *Value different from HCLF meal value, P < 0.05; ‡P < 0.06.
The relative contribution (calculated as the average of the individual time points over 6 h after the meals) of endogenous gluccose production (EGP) to total glucose Ra into plasma was 42 ± 18% after ingestion of the HCLF meal and 83 ± 10% after ingestion of the LCHF meal (P < 0.001); conversely, the contribution of ingested glucose to total glucose Ra was 58 ± 18% after the HCLF meal and 17 ± 10% after ingestion of the LCHF meal (P < 0.001).
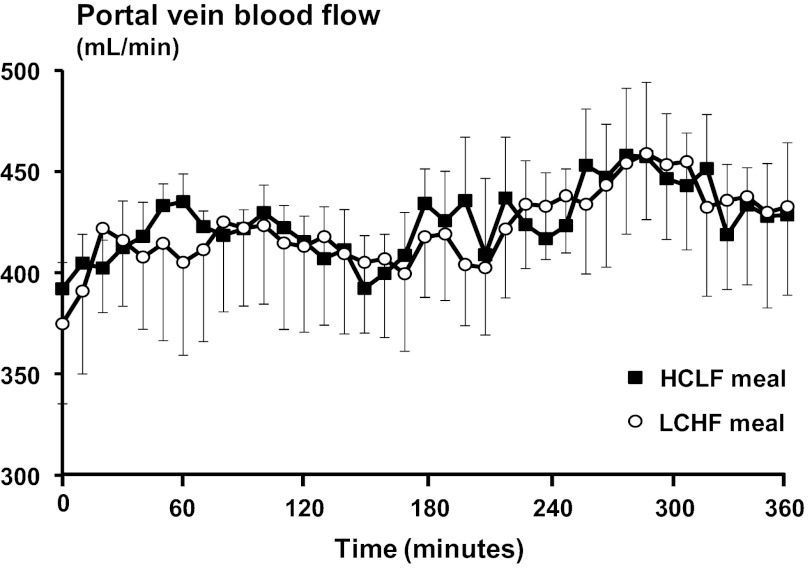
Portal vein blood flow.
Portal vein blood flow increased after both HCLF and LCHF meal ingestion (P < 0.001), but there was no difference between the HCLF and the LCHF meals (interaction between time and diet P = 0.968) (Fig. 5).
Fig. 5.
Portal vein blood flow before and for 6 h after a HCLF or a LCHF meal. Time point 0 is the average of the measurements carried out for 30 min before the meals were given. Portal vein blood flow increased (P < 0.001) after HCLF and LCHF meals in a similar fashion (no interaction between time and type of meal was observed). Values are presented as means ± SE.
DISCUSSION
In the present study, we established, for the first time, a model of chronic portal vein catheterization in awake nonhuman primates, which we used to evaluate the dynamic response to LCHF and HCLF meal ingestion. In this model, portal vein sampling and blood flow measurement provide a comprehensive in vivo metabolic assessment of meal ingestion. Stable isotopically labeled glucose tracers were administered orally and intravenously, and both systemic arterial and portal vein blood samples were obtained to evaluate ingested and endogenous glucose metabolism and the β-cell and α-cell responses to feeding. Our data demonstrate that a LCHF meal causes minimal changes in the Ra of glucose in both portal and systemic circulations, does not affect the rate of EGP, and causes minimal stimulation of C-peptide and insulin secretion and less suppression of plasma glucagon. In addition, we found that plasma glucose concentration is maintained primarily by the delivery of ingested glucose into the systemic circulation after a HCLF meal is consumed, whereas plasma glucose concentration is maintained primarily by EGP after a LCHF meal. These observations demonstrate that LCHF diets cause minimal perturbations in glucose homeostasis and pancreatic β-cell and α-cell activities and help explain why low-glycemic diets have therapeutic effects on glycemic control (28, 47) and reduce the risk of developing type 2 diabetes (39).
Decreasing the glycemic load of meals by reducing the amount or composition of dietary carbohydrates has beneficial therapeutic effects on overall glycemic control and plasma glucose concentration. In subjects with type 2 diabetes, a low-glycemic index diet decreases fasting plasma glucose concentration, decreases 2-h glucose concentration during an oral glucose tolerance test, and improves glycemic control, as assessed by plasma Hb A1c concentration (28, 47). A low-glycemic index diet also has beneficial effects in overweight and obese nondiabetic subjects by lowering postprandial glucose and insulin concentrations (13, 32). Even in healthy normal-weight subjects, reducing the carbohydrate load leads to a reduction in mean plasma glucose concentration over 24 h (5, 26). In contrast, a high-carbohydrate diet, particularly one that contains high-glycemic index foods, is associated with an increased risk of developing type 2 diabetes (39). We found that the HCLF meal had a prolonged suppressive effect on plasma FFA concentration, which lasted for 5 h after the meal. The increase in plasma insulin and greater reduction in plasma FFA availability after meal ingestion were likely responsible for the greater suppression of EGP observed after the HCLF than after the LCHF meal (25, 35). Although this effect on lipolysis and EGP has acute benefits on glucose control, chronic consumption of a high-carbohydrate diet can have adverse effects on overall glucose and lipid metabolism by stimulating de novo lipogenesis and the accumulation of intrahepatic triglyceride (36), increasing plasma triglyceride concentration (20, 31), and decreasing insulin sensitivity (17). The results from our study suggest that a LCHF diet can have beneficial effects in both preventing and treating diabetes by reducing meal-induced plasma glucose excursions and requiring minimal β-cell action and insulin response to meal ingestion. The variability in the response to ingesting the same meal observed in our homogeneous baboon model suggests that much larger numbers of subjects will be needed when studies evaluating the metabolic response to food intake in people are conducted.
Most glucose ingested during a meal is delivered into the systemic circulation and taken up by peripheral tissues, whereas only a portion of ingested glucose is metabolized by the liver during its first pass from the portal vein. We found that ∼20% of ingested glucose was extracted by the liver after a HCLF meal was ingested in our baboon model, which is the middle of the range reported in studies that assessed fractional hepatic glucose extraction after ingestion of an oral glucose load in human subjects (14, 24, 29, 37). Therefore, our results, which were derived from direct measurement of portal vein glucose concentration and glucose tracer/tracee ratios, support the estimates made from previous studies conducted in people, which used indirect assessments to determine hepatic fractional extraction.
Portal vein blood flow is involved in regulating glucose metabolism because it provides ∼80% of the blood delivered to the liver (22). The uptake and metabolism of glucose by the liver after food intake is affected by the rate of glucose and hormone delivery, which in turn depends on portal vein blood flow during a meal (11). Portal venous blood flow increases by 20 to 80% 30 min after a meal, depending on the type of meal (liquid vs. solid), and remains elevated for 2 h after meal consumption (10, 12, 16, 44). The main determinant of the postprandial increase in portal vein flow is the gastrointestinal hyperemic response that follows food digestion and absorption, which leads to a marked increase in blood outflow from extrahepatic splanchnic tissues to the portal system (38). We found that both LCHF and HCLF meals caused similar increases in portal vein blood flow. This observation in our awake baboon model is consistent with data from studies conducted in an anesthetized dog model, which found that the increase in portal vein blood flow was similar after intrajejunal infusion of either fat or carbohydrate (8). In contrast, Hoost et al. (27) found that portal vein flow in healthy people was slightly greater after a high-fat meal compared with a high-carbohydrate meal. The reasons for the differences in their results and the other studies are not clear but could be related to the use of Doppler ultrasonography through the abdominal wall to assess portal vein blood flow in the study conducted in people, rather than the direct assessment of portal vein blood flow, by using an intraportal flow probe in our study.
In summary, we developed a model of chronic portal vein catheterization in awake baboons to evaluate the integrated metabolic response to meal ingestion. Our data demonstrate that in adult male baboons a LCHF meal elicited a less robust insulin secretory response compared with a HCLF meal and support the importance of further studies to assess the potential for therapeutic benefit of a low-carbohydrate diet on glycemic control and prevention of type 2 diabetes.
GRANTS
This work was supported by National Institutes of Health (NIH) Grants UL1-RR-024992 (Clinical Translational Science Award) and DK-56341 (Nutrition and Obesity Research Center) and a grant from the Atkins Foundation Philanthropic Trust. The investigation was conducted in facilities constructed with support from the Research Facilities Improvement Program under grant no. C06-RR (nos. 014578, 013556, 015456, and 017515) from the National Center for Research Resources, NIH, and with support from NIH grants PO1-HL-028972, P51-RR-013986, and P51-OD-013986.
DISCLOSURES
Washington University School of Medicine has received an endowment from the Atkins Foundation Philanthropic Trust for the Atkins Center of Excellence in Obesity Medicine.
AUTHOR CONTRIBUTIONS
E.F., P.B.H., F.M., R.A.B., A.G.C., R.E.S., B.W.P., and S.K. contributed to the conception and design of research; E.F., P.B.H., V.S.V., A.G.C., and R.E.S. performed the experiments; E.F., P.B.H., F.M., R.E.S., A.G., J.D.H., D.O., B.W.P., and S.K. analyzed the data; E.F., P.B.H., F.M., R.A.B., V.S.V., A.G.C., R.E.S., A.G., J.D.H., D.O., B.W.P., and S.K. interpreted the results of experiments; E.F. and F.M. prepared the figures; E.F. drafted the manuscript; E.F., P.B.H., F.M., V.S.V., A.G.C., R.E.S., A.G., J.D.H., D.O., B.W.P., and S.K. edited and revised the manuscript; E.F., P.B.H., F.M., R.A.B., V.S.V., A.G.C., R.E.S., A.G., D.O., B.W.P., and S.K. approved the final version of the manuscript.
ACKNOWLEDGMENTS
We thank Norma Anderson, Freida Custodio, Magdelena Forey, Jennifer Shew, and Adewole Okunade for their technical assistance, Phillip Williams for developing the surgical procedure for implantation of the portal vein catheters, Dr. Patrice Frost for assistance during the surgical procedures, and the veterinarian technicians and the staff at the Texas Biomedical Research Institute (Texas Biomed) for their excellent care of the animals.
REFERENCES
- 1.No authors listed. Position of the American Dietetic Association: weight management. J Am Diet Assoc 97: 71–74, 1997 [DOI] [PubMed] [Google Scholar]
- 2.No authors listed. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. National Institutes of Health. Obes Res 6, Suppl 2: 51S–209S, 1998 [PubMed] [Google Scholar]
- 3.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 27, Suppl 1: S5–S10, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Austin GL, Ogden LG, Hill JO. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971–2006. Am J Clin Nutr 93: 836–843, 2011 [DOI] [PubMed] [Google Scholar]
- 5.Brynes AE, Adamson J, Dornhorst A, Frost GS. The beneficial effect of a diet with low glycaemic index on 24 h glucose profiles in healthy young people as assessed by continuous glucose monitoring. Br J Nutr 93: 179–182, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Burcelin R, Dolci W, Thorens B. Glucose sensing by the hepatoportal sensor is GLUT2-dependent: in vivo analysis in GLUT2-null mice. Diabetes 49: 1643–1648, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Burcelin R, Dolci W, Thorens B. Portal glucose infusion in the mouse induces hypoglycemia: evidence that the hepatoportal glucose sensor stimulates glucose utilization. Diabetes 49: 1635–1642, 2000 [DOI] [PubMed] [Google Scholar]
- 8.Chou CC, Kvietys P, Post J, Sit SP. Constituents of chyme responsible for postprandial intestinal hyperemia. Am J Physiol Heart Circ Physiol 235: H677–H682, 1978 [DOI] [PubMed] [Google Scholar]
- 9.Coelho AM, Jr, Carey KD. A social tethering system for nonhuman primates used in laboratory research. Lab Anim Sci 40: 388–394, 1990 [PubMed] [Google Scholar]
- 10.Cooper AM, Braatvedt GD, Qamar MI, Brown H, Thomas DM, Halliwell M, Read AE, Corrall RJ. Fasting and post-prandial splanchnic blood flow is reduced by a somatostatin analogue (octreotide) in man. Clin Sci (Lond) 81: 169–175, 1991 [DOI] [PubMed] [Google Scholar]
- 11.Dardevet D, Moore MC, Remond D, Everett-Grueter CA, Cherrington AD. Regulation of hepatic metabolism by enteral delivery of nutrients. Nutr Res Rev 19: 161–173, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Dauzat M, Lafortune M, Patriquin H, Pomier-Layrargues G. Meal induced changes in hepatic and splanchnic circulation: a noninvasive Doppler study in normal humans. Eur J Appl Physiol Occup Physiol 68: 373–380, 1994 [DOI] [PubMed] [Google Scholar]
- 13.de Rougemont A, Normand S, Nazare JA, Skilton MR, Sothier M, Vinoy S, Laville M. Beneficial effects of a 5-week low-glycaemic index regimen on weight control and cardiovascular risk factors in overweight non-diabetic subjects. Br J Nutr 98: 1288–1298, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Ferrannini E, Bjorkman O, Reichard GA, Jr, Pilo A, Olsson M, Wahren J, DeFronzo RA. The disposal of an oral glucose load in healthy subjects. A quantitative study. Diabetes 34: 580–588, 1985 [DOI] [PubMed] [Google Scholar]
- 15.Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary PO, Rader DJ, Edman JS, Klein S. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 348: 2082–2090, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Gaiani S, Bolondi L, Li Bassi S, Santi V, Zironi G, Barbara L. Effect of meal on portal hemodynamics in healthy humans and in patients with chronic liver disease. Hepatology 9: 815–819, 1989 [DOI] [PubMed] [Google Scholar]
- 17.Garg A, Bantle JP, Henry RR, Coulston AM, Griver KA, Raatz SK, Brinkley L, Chen YD, Grundy SM, Huet BA, Reaven GM. Effects of varying carbohydrate content of diet in patients with non-insulin-dependent diabetes mellitus. JAMA 271: 1421–1428, 1994 [DOI] [PubMed] [Google Scholar]
- 18.Garg A, Bonanome A, Grundy SM, Zhang ZJ, Unger RH. Comparison of a high-carbohydrate diet with a high-monounsaturated-fat diet in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 319: 829–834, 1988 [DOI] [PubMed] [Google Scholar]
- 19.Garg A, Grundy SM, Koffler M. Effect of high carbohydrate intake on hyperglycemia, islet function, and plasma lipoproteins in NIDDM. Diabetes Care 15: 1572–1580, 1992 [DOI] [PubMed] [Google Scholar]
- 20.Garg A, Grundy SM, Unger RH. Comparison of effects of high and low carbohydrate diets on plasma lipoproteins and insulin sensitivity in patients with mild NIDDM. Diabetes 41: 1278–1285, 1992 [PubMed] [Google Scholar]
- 21.Gastaldelli A, Casolaro A, Pettiti M, Nannipieri M, Ciociaro D, Frascerra S, Buzzigoli E, Baldi S, Mari A, Ferrannini E. Effect of pioglitazone on the metabolic and hormonal response to a mixed meal in type II diabetes. Clin Pharmacol Ther 81: 205–212, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Greenway CV, Stark RD. Hepatic vascular bed. Physiol Rev 51: 23–65, 1971 [DOI] [PubMed] [Google Scholar]
- 23.Hainsey BM, Hubbard GB, Leland MM, Brasky KM. Clinical parameters of the normal baboons (Papio species) and chimpanzees (Pan troglodytes). Lab Anim Sci 43: 236–243, 1993 [PubMed] [Google Scholar]
- 24.Hall SE, Bolton TM, Hetenyi G., Jr The effect of bran on glucose kinetics and plasma insulin in non-insulin-dependent diabetes mellitus. Diabetes Care 3: 520–525, 1980 [DOI] [PubMed] [Google Scholar]
- 25.Hawkins M, Tonelli J, Kishore P, Stein D, Ragucci E, Gitig A, Reddy K. Contribution of elevated free fatty acid levels to the lack of glucose effectiveness in type 2 diabetes. Diabetes 52: 2748–2758, 2003 [DOI] [PubMed] [Google Scholar]
- 26.Henry CJ, Lightowler HJ, Tydeman EA, Skeath R. Use of low-glycaemic index bread to reduce 24-h blood glucose: implications for dietary advice to non-diabetic and diabetic subjects. Int J Food Sci Nutr 57: 273–278, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Hoost U, Kelbaek H, Rasmusen H, Court-Payen M, Christensen NJ, Pedersen-Bjergaard U, Lorenzen T. Haemodynamic effects of eating: the role of meal composition. Clin Sci (Lond) 90: 269–276, 1996 [DOI] [PubMed] [Google Scholar]
- 28.Jenkins DJ, Kendall CW, McKeown-Eyssen G, Josse RG, Silverberg J, Booth GL, Vidgen E, Josse AR, Nguyen TH, Corrigan S, Banach MS, Ares S, Mitchell S, Emam A, Augustin LS, Parker TL, Leiter LA. Effect of a low-glycemic index or a high-cereal fiber diet on type 2 diabetes: a randomized trial. JAMA 300: 2742–2753, 2008 [DOI] [PubMed] [Google Scholar]
- 29.Kalant N, Kuyumjian J, Luna F, Nastase C. Hepatic glucose extraction in normal and diabetic man. Metabolism 36: 513–520, 1987 [DOI] [PubMed] [Google Scholar]
- 30.Klein S, Mittendorfer B, Eagon JC, Patterson B, Grant L, Feirt N, Seki E, Brenner D, Korenblat K, McCrea J. Gastric bypass surgery improves metabolic and hepatic abnormalities associated with nonalcoholic fatty liver disease. Gastroenterology 130: 1564–1572, 2006 [DOI] [PubMed] [Google Scholar]
- 31.Krauss RM, Blanche PJ, Rawlings RS, Fernstrom HS, Williams PT. Separate effects of reduced carbohydrate intake and weight loss on atherogenic dyslipidemia. Am J Clin Nutr 83: 1025–1031; quiz 1205, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Krog-Mikkelsen I, Sloth B, Dimitrov D, Tetens I, Björck I, Flint A, Holst JJ, Astrup A, Elmståhl H, Raben A. A low glycemic index diet does not affect postprandial energy metabolism but decreases postprandial insulinemia and increases fullness ratings in healthy women. J Nutr 141: 1679–1684, 2011 [DOI] [PubMed] [Google Scholar]
- 33.McGuinness OP, Fugiwara T, Murrell S, Bracy D, Neal D, O'Connor D, Cherrington AD. Impact of chronic stress hormone infusion on hepatic carbohydrate metabolism in the conscious dog. Am J Physiol Endocrinol Metab 265: E314–E322, 1993 [DOI] [PubMed] [Google Scholar]
- 34.Moore MC, Cardin S, Edgerton DS, Farmer B, Neal DW, Lautz M, Cherrington AD. Unlike mice, dogs exhibit effective glucoregulation during low-dose portal and peripheral glucose infusion. Am J Physiol Endocrinol Metab 286: E226–E233, 2004 [DOI] [PubMed] [Google Scholar]
- 35.Moore MC, Satake S, Lautz M, Soleimanpour SA, Neal DW, Smith M, Cherrington AD. Nonesterified fatty acids and hepatic glucose metabolism in the conscious dog. Diabetes 53: 32–40, 2004 [DOI] [PubMed] [Google Scholar]
- 36.Postic C, Dentin R, Denechaud PD, Girard J. ChREBP, a transcriptional regulator of glucose and lipid metabolism. Annu Rev Nutr 27: 179–192, 2007 [DOI] [PubMed] [Google Scholar]
- 37.Radziuk J, McDonald TJ, Rubenstein D, Dupre J. Initial splanchnic extraction of ingested glucose in normal man. Metabolism 27: 657–669, 1978 [DOI] [PubMed] [Google Scholar]
- 38.Richardson PD, Withrington PG. Liver blood flow. I. Intrinsic and nervous control of liver blood flow. Gastroenterology 81: 159–173, 1981 [PubMed] [Google Scholar]
- 39.Sluijs I, van der Schouw YT, van der A DL, Spijkerman AM, Hu FB, Grobbee DE, Beulens JW. Carbohydrate quantity and quality and risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition-Netherlands (EPIC-NL) study. Am J Clin Nutr 92: 905–911, 2010 [DOI] [PubMed] [Google Scholar]
- 40.Sparacino G, Cobelli C. A stochastic deconvolution method to reconstruct insulin secretion rate after a glucose stimulus. IEEE Trans Biomed Eng 43: 512–529, 1996 [DOI] [PubMed] [Google Scholar]
- 41.Sparacino G, Pillonetto G, Capello M, De Nicolao G, Cobelli C. WINSTODEC: a stochastic deconvolution interactive program for physiological and pharmacokinetic systems. Comput Methods Programs Biomed 67: 67–77, 2002 [DOI] [PubMed] [Google Scholar]
- 42.Steele R. Influences of glucose loading and of injected insulin on hepatic glucose output. Ann NY Acad Sci 82: 420–430, 1959 [DOI] [PubMed] [Google Scholar]
- 43.Steil GM, Rebrin K, Mittelman SD, Bergman RN. Role of portal insulin delivery in the disappearance of intravenous glucose and assessment of insulin sensitivity. Diabetes 47: 714–720, 1998 [DOI] [PubMed] [Google Scholar]
- 44.Szinnai C, Mottet C, Gutzwiller JP, Drewe J, Beglinger C, Sieber CC. Role of gender upon basal and postprandial systemic and splanchnic haemodynamics in humans. Scand J Gastroenterol 36: 540–544, 2001 [DOI] [PubMed] [Google Scholar]
- 45.Tai MM. A mathematical model for the determination of total area under glucose tolerance and other metabolic curves. Diabetes Care 17: 152–154, 1994 [DOI] [PubMed] [Google Scholar]
- 46.Van Cauter E, Mestrez F, Sturis J, Polonsky KS. Estimation of insulin secretion rates from C-peptide levels. Comparison of individual and standard kinetic parameters for C-peptide clearance. Diabetes 41: 368–377, 1992 [DOI] [PubMed] [Google Scholar]
- 47.Wolever TM, Gibbs AL, Mehling C, Chiasson JL, Connelly PW, Josse RG, Leiter LA, Maheux P, Rabasa-Lhoret R, Rodger NW, Ryan EA. The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: no effect on glycated hemoglobin but reduction in C-reactive protein. Am J Clin Nutr 87: 114–125, 2008 [DOI] [PubMed] [Google Scholar]
- 48.Wuesten O, Balz CH, Bretzel RG, Kloer HU, Hardt PD. Effects of oral fat load on insulin output and glucose tolerance in healthy control subjects and obese patients without diabetes. Diabetes Care 28: 360–365, 2005 [DOI] [PubMed] [Google Scholar]
- 49.Zheng D, Ionut V, Mooradian V, Stefanovski D, Bergman RN. Portal glucose infusion-glucose clamp measures hepatic influence on postprandial systemic glucose appearance as well as whole body glucose disposal. Am J Physiol Endocrinol Metab 298: E346–E353, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]