Abstract
Downregulation of brain-derived neurotrophic factor (BDNF) gene expression with corresponding increased methylation at specific promoters has been associated with stressful experiences in early life and may explain later adulthood psychopathology. We measured the percentage of methylation at BDNF CpG exons I and IV as well as plasma BDNF protein levels in 115 subjects with borderline personality disorder (BPD) and 52 controls. BPD subjects then underwent a 4-week course of intensive dialectical behavior therapy (I-DBT). BDNF methylation status and protein levels were re-assessed at the end of treatment. BPD subjects had significantly higher methylation status in both CpG regions than controls. In addition, the higher the number of childhood trauma, the higher was the methylation status. In BPD subjects, BDNF methylation significantly increased after I-DBT. Nonresponders accounted for the majority of this increase, whereas responders showed a decrease in methylation status over time. Accordingly, the changes in methylation status over time were significantly associated with changes in depression scores, hopelessness scores and impulsivity. No association was found between protein levels and BDNF methylation status. We here found a relationship between child maltreatment and higher DNA methylation of BDNF. These results moreover support the idea that these epigenetic marks may be changed through psychotherapeutic approaches and that these changes underline changes in cognitive functions.
Keywords: BDNF, borderline personality disorder, psychotherapy, DBT, epigenetic
Introduction
Borderline personality disorder (BPD) is a disorder characterized by marked impulsivity, lack of emotional control, disturbed interpersonal relationships and frequent self-injurious and suicidal behaviors. Not surprisingly, it is associated with high socioeconomic burden and high morbidity and mortality. One of the etiological factors believed to be responsible for the development of BPD is childhood maltreatment.1 It is hypothesized that early-life adverse events may favor the occurrence of core dimensions of this personality disorder through sustained epigenetic modifications of key developmental or stress-related genes such as the one coding for the glucocorticoid receptor (NR3C1).2 One of the proteins that have recently been implicated in BPD is brain-derived neurotrophic factor (BDNF).3, 4, 5 Because of its involvement in neurodevelopment, BDNF may indeed be seen as a natural candidate for a biological correlate of early-life stress. The altered levels of this protein found in BPD subjects5 may thus be the consequence of epigenetic modification resulting from child maltreatment. Higher histone and DNA methylation of the BDNF gene and consecutive downregulation of BDNF mRNA and decreased levels of BDNF have been demonstrated in animal models of maltreatment.6, 7 Tsankova et al.8 showed that chronic defeat stress in mice induced downregulation of the expression of BDNF promoter/exon IV and was associated with increases in histone H3 lysine 27 methylation (H3K27) at the corresponding promoter. Although posttranslational modifications of histones have been shown to be an important correlate of environmental epigenetic modifications, DNA methylation status at CpG sites within the promoter/exon IV has also been extensively studied and found to be an important correlate of the impact of early developmental stress.9, 10, 11 Roth et al.9, 11 found that psychosocial stress in rats increased BDNF DNA methylation at promoter/exon IV, suggesting that there may be a mechanism underlying cognitive deficits found in adult subjects maltreated in their childhood. Although epigenetic modifications of the BDNF gene have never been explored in BPD, increased DNA methylation at specific CpG sites in the BDNF promoter/exon IV and lower BDNF mRNA levels in the Wernike area have been found in suicide victims, a phenotype closely related to BPD.12
Several recent studies in depression have convincingly shown that the epigenetic processes involving BDNF are responsible for the altered levels of BDNF associated with this disorder and that these epigenetic processes can be changed through antidepressant treatment.13, 14 In this perspective, Lopez et al.15 were the first to show that, in humans, 8 weeks of treatment with an antidepressant (citalopram) decreased H3K27 methylation levels at promoter/exon IV of the BDNF gene. This reduction in BDNF H3K27 methylation was not only associated with increased BDNF levels but also with depression response. The same group had already demonstrated that increased expression of BDNF promoter/exon IV and decreased methylation of H3K27 in the prefrontal cortex was associated with a history of antidepressant treatment.16 These studies thus suggest that BDNF methylation, at least in histones, is a dynamic process underlying the cognitive changes observed during treatment. These results clearly need to be extended to CpG DNA methylation as this has been shown to be critical for regulation of BDNF expression and thus for the development of mental health diseases.
Following these observations, this study aims to answer the following questions: is the DNA methylation status of BDNF exons I and IV higher in BPD compared with control subjects? Is this higher DNA BDNF methylation in BPD subjects linked to child maltreatment? And finally can these epigenetic processes be changed through a specific psychotherapeutic approach to subjects with BPD and are they linked to response to treatment?
Patients and methods
A total of 115 outpatients with BPD were admitted to a specialized center proving intensive dialectical behavior therapy (I-DBT) as the main treatment for this disorder.17, 18 Briefly, patients displaying suicidal or para-suicidal behaviors, severe impulse control disorders and anger problems were referred to the specialized center by their physician or other medical services. All participants received psychopharmacological treatment, which was refined by a psychiatrist if necessary before and during follow-up. However, pharmaceutical treatment during I-DBT remained unmodified in most of the subjects (N=89). Only subjects fulfilling DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th Edition) criteria for BPD were accepted for intensive therapy. In this perspective, each participant was interviewed by either a trained psychiatrist or a psychologist before acceptance into treatment using the Screening Interview for Axis II Disorder (SCID-II) BPD part.19 In addition, the French version of the Diagnostic Interview for Genetic Studies (DIGS) was used to assess Axis I disorders.20 At 1 week before the start of I-DBT, each participant completed the Beck Depression Inventory II (BDI-II)21 to assess the current severity of depression, the Beck Hopelessness Scale (BHS)22 to estimate the degree of pessimism and negativity about the future and the Barrat Impulsiveness Scale (BIS-10) to measure the three components of impulsivity: motor (behavior), attentional (cognitive) and non-planning.23 On the last day of I-DBT, participants were asked to complete these questionnaires again. The Childhood Trauma Questionnaire (CTQ), which examines five types of trauma (sexual abuse, physical abuse, physical neglect, emotional abuse and emotional neglect),24 was used to assess childhood traumatic experience. With the exception of the BIS-10, these baseline measurements were previously used in our previous study examining the effect of child maltreatment on NR3C1 methylation status.2
A total of 52 controls completed the same self-report questionnaires and were recruited from the School of Dentistry at the University of Geneva.
The study was approved by the ethics committee of Geneva University Hospital. Informed written consent was obtained from all participants.
Treatment
Participants were referred to I-DBT for 4 weeks of treatment as previously described.17, 25 I-DBT is an adaptation of standard DBT that aims to provide an overview of the traditional DBT behavioral skills (emotion regulation, interpersonal effectiveness, distress tolerance and mindfulness). I-DBT consists of daily group and individual therapy the aim of which is to decrease the behavioral targets that were chosen within a DBT framework, with suicidal behaviors treated as a priority, followed by behaviors that interfere with therapy and then by behaviors that interfere with quality of life. Each participant was followed by a trained DBT therapist (nurse or psychologist).25
DNA extraction
For the BPD subjects, blood samples were systematically collected 1 week before the commencement of the program and on the last day of I-DBT. For control subjects, blood samples were collected just after the interviews. DNA was extracted from peripheral blood leukocytes by using the Nucleon kit (Bioscience Amersham, GE Healthcare, Glattbrugg, Switzerland). After extraction, 2 μg of genomic DNA was bisulfite-modified by using the EpiTect Bisulfite Kit (Qiagen, Germantown, MD, USA) according to the manufacturer's instructions.
Commercial controls of methylation
Methylation status was identified by high-resolution melt assay on a Rotor-Gene 6000 instrument (Corbett Life Science, Chadstone, Victoria, Australia). This technique proved to be accurate, rapid and sensitive.26, 27 Details on the DNA methylation by high-resolution melt analysis are given in the Supplementary Material.
Selection of BDNF regions for methylation analysis and PCR design
We identified by UCSC (University of California, Santa Cruz) genome browser (http://genome.ucsc.edu/index.html?org=Human&db=hg19&hgsid=242691861) a CpG island region located at chr11:27743473–27744564 (CpG count: 81, % GC=60.5 and Obs/Exp=0.83) in the BDNF promoter region, upstream of the ATG start in exon I. PCR design includes 9 CpGs and is located from –1096 to –900 (numbers relate to the translation start site considered as +1 in exon I). We called this CpG island BDNF CpG exon I. The second CpG region (chr11:27723060–27723294), which is not a CpG island by UCSC genome browser criteria (% GC >50, length >200 bp and Obs/Exp >0.6), was positioned in exon IV, upstream of the ATG start in exon VII. The present amplicon encompasses 17 CpGs and is located from –2341 to –2107 (numbers relate to the translation start site considered as +1 in exon VII). We called this CpG region BDNF CpG exon IV (Supplementary Figure S1).
All samples were tested in duplicate. In these assays, the methylation percentage of samples was determined by high-resolution melt profile by comparing them with the scale of commercial controls described in the Supplementary Material.
BDNF protein levels
BDNF protein levels were measured in plasma as previously described.28 Blood obtained from the antecubital vein was collected in a suitable tube containing an anticoagulant solution and centrifuged at 2000 g for 10 min at 4 °C. Plasma was aliquoted and stored at −20 °C until use. BDNF levels were measured with an enzyme-linked immunosorbent assay kit (Promega, Wallisellen, Switzerland) after appropriate dilution with the Block and Sample solution (provided with the kit). A microplate reader (Anthos Labtec Instrument, Chatel St-Denis, Switzerland) set at 450 °C was used to determine plasma BDNF values (intra-assay and interassay variations were <6 and 7%, respectively).
Statistical analyses
Linear regression with adjustment for age and gender was used to assess the effect of disease status (BPD vs controls) and childhood maltreatment status (number of childhood maltreatments as previously described).2
Mean methylation percentage of both BDNF CpG exons I and IV was used as the dependant variable. In a secondary analysis, these two exons were analyzed separately.
Linear mixed models with maximum likelihood estimation where treatment time was a fixed effect and the individual a random effect, as described elsewhere,29, 30 were initially used to analyze the effect of I-DBT on percentage of methylation. Secondarily, these models were used to assess the association between changes in methylation and changes in depression severity, hopelessness and impulsivity respectively. In addition, to define better the link between changes in methylation and treatment response, changes in BDNF methylation during I-DBT were assessed within the following categories according to treatment response: for depression and hopelessness: ⩽25% improvement; >25 to ⩽50% improvement; >50 to ⩽75% improvement and >75% improvement; and for impulsivity: 0% improvement; >0 to ⩽10% improvement; >10 to ⩽20% improvement and >20% improvement.
Finally, to ensure that the observed effect was not better explained by changes in medication during follow-up (26 BPD subjects had a change/adjustment of treatment during follow-up) or by antidepressant treatment (55 BPD subjects were taking antidepressants), these two variables (changes in medication yes/no and taking antidepressant yes/no) were added into the models as covariates. The results of regression models are presented as standardized regression coefficients (β) with 95% confidence intervals that can be interpreted as effect size. The threshold of significance was P=0.05. All analyses were performed using STATA release 10 (StataCorp LP, College Station, TX, USA).
Results
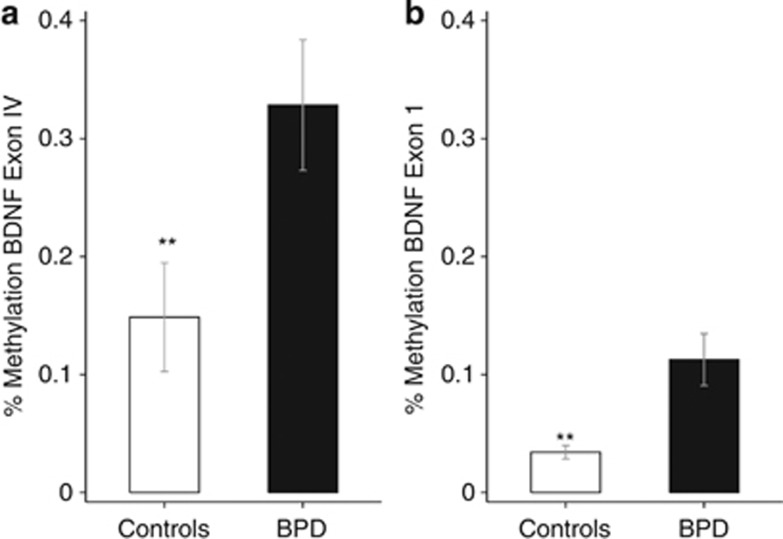
The clinical and demographic characteristics of control and BPD subjects are described in Table 1. After adjustment for age and gender, BPD subjects had significantly higher methylation status in both CpG regions compared with controls (32.84% vs 14.86%, β=0.61, P=0.002, 95% CI 0.22–0.99; and 11.27% vs 3.42%, β=0.66, P=0.001, 95% CI 0.24–0.99 for CpG exon IV and CpG exon I, respectively; Figure 1).
Table 1. Demographic and clinical characteristics of the BPD and control samples.
|
Controls (N=52) |
BPD (N=115) |
t(d.f.) | P-value | |||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | |||
| Age (years) | 40.65 | 12.04 | 30.36 | 9.19 | 6.06 (165) | 8.69 × 10–9 |
| BDI (baseline) | 6.04 | 5.38 | 34.10 | 11.80 | −14.94 (148) | 2.42 × 10–31 |
| Hopelessness (baseline) | 4.03 | 2.5 | 11.30 | 4.82 | −9.39 (149) | 9.33 × 10–17 |
| BIS-10 (baseline) | 42.26 | 11.53 | 69.30 | 17.75 | −9.81 (152) | 6.45 × 10–18 |
| SCID-II BPD part | — | — | 6.52 | 1.75 | ||
| N | % | N | % | X2(d.f.) | P-value | |
| Female | 24 | 46.15 | 108 | 93.91 | 38.03(1) | 6.98 × 10–10 |
| Axis I | ||||||
| Bipolar disorder | 0 | 0 | 22 | 19.13 | ||
| Major depressive disorder | 0 | 0 | 84 | 73.04 | ||
| Schizoaffective disorder | 0 | 0 | 9 | 7.83 | ||
| CTQ | ||||||
| Physical neglect | 6 | 14.29 | 52 | 48.60 | 14.94(1) | 1.11 × 10–4 |
| Physical abuse | 4 | 9.52 | 56 | 52.34 | 22.98(1) | 1.63 × 10–6 |
| Emotional abuse | 12 | 28.57 | 91 | 85.05 | 45.07(1) | 1.89 × 10–11 |
| Emotional neglect | 18 | 42.86 | 90 | 84.11 | 25.73(1) | 3.91 × 10–7 |
| Sexual abuse | 8 | 19.05 | 57 | 53.27 | 14.36(1) | 1.51 × 10–4 |
Abbreviations: BDI, Beck Depression Inventory; BIS-10, Barrat Impulsiveness Scale; BPD, borderline personality disorder; CTQ, Childhood Trauma Questionnaire; SCID-II, Screening Interview for Axis II Disorder.
Figure 1.
Percentage methylation of brain-derived neurotrophic factor (BDNF) CpG exon IV (a) and BDNF CpG exon I (b) regions in controls and borderline personality disorder (BPD) subjects at baseline. **P<0.01. Bars represent s.d.
These results may reflect the association between the number of childhood maltreatments (sum of abuses and neglects) and the total percentage of methylation (mean percentage at both CpG sites). The greater the number of childhood trauma, the higher was the methylation status (β=0.12, P=0.005, 95% CI 0.04–0.21; Figure 2).
Figure 2.
Percentage of methylation (mean of brain-derived neurotrophic factor (BDNF) CpG exon IV and BDNF CpG exon I regions) according to the number of childhood maltreatments. Bars represent s.d.
Effect of I-DBT on BDNF methylation status
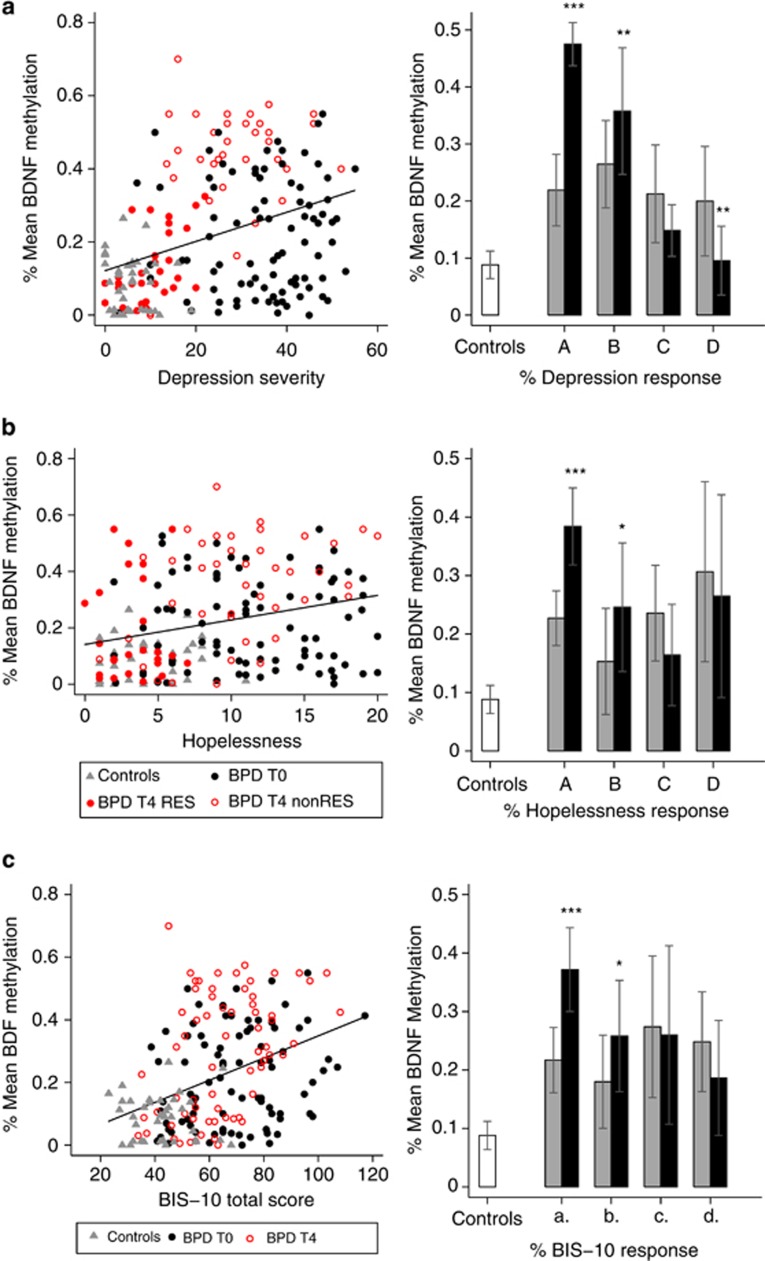
There was a significant positive association between depression severity, hopelessness and impulsivity and BDNF methylation status (β=0.02, P=0.0001, 95% CI 0.01–0.03; β=0.04; P=0.002, 95% CI 0.016–0.07; and β=0.02, P=2.32 × 10−6, 95% CI 0.01–0.025, respectively; Figure 3).
Figure 3.
Percentage of methylation (mean of brain-derived neurotrophic factor (BDNF) CpG exon IV and BDNF CpG exon I regions) according to depression severity (a), hopelessness (b) and impulsivity (c). The right panels in (a–c) indicate treatment response and percentage of methylation according to treatment response: for depression and hopelessness: A, ≤25% improvement; B, >25% to ≤50% improvement; C, >50% to ≤75% improvement; D, >75% improvement; and for impulsivity: a, 0% improvement; b, >0% to ≤10% improvement; c, >10% to ≤20% improvement; d, >20% improvement (gray bars indicate borderline personality disorder (BPD) at baseline and black bars indicate BPD after treatment). Bars represent s.d. *P<0.05; **P<0.01; ***P<0.001. The left panels in (a–c) indicate scatter plots of percentage of methylation and severity of depression, hopelessness and impulsivity. BPD T0, borderline personality disorder subjects at baseline; BPD T4, borderline personality disorder subjects after treatment; non-RES, nonresponders (≤50% improvement); RES, responders (>50% improvement).
There was a significant decrease in depression severity (from 34.10 (s.d.=11.80) to 20.37 (s.d.=12.42), β=−0.94, P=5.68 × 10−35, 95% CI −1.09 to −0.79), hopelessness (from 11.30 (s.d.=4.82) to 7.98 (s.d.=5.04), β=−0.63, P=1.51 × 10−13, 95% CI −0.80 to −0.47) and impulsivity (from 69.30 (s.d.=17.75) to 65.99 (s.d.=17.31), β=−0.16, P=0.006, 95% CI −0.28 to −0.05) over time in BPD subjects following I-DBT.
Surprisingly, BDNF methylation significantly increased over time (β=0.50, P=0.0001, 95% CI 0.25–0.74). Poor responders were mainly responsible for the increase (Table 2 and Figure 3).
Table 2. Percentage of methylation (mean of BDNF CpG exon I and BDNF CpG exon IV regions) before and after I-DBT according to treatment response.
| Mean (baseline) | s.d. | Mean (end) | s.d. | N | β | P-value | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|
| BDI | |||||||||
| ≤25% | 32.77 | 13.67 | 30.63 | 10.64 | 29 | 1.43 | 4.07 × 10–13 | 1.04 | 1.81 |
| >25 to ≤50% | 37.67 | 10.27 | 24.24 | 7.29 | 21 | 0.51 | 0.01 | 0.15 | 0.87 |
| >50 to ≤75% | 35.68 | 7.50 | 13.59 | 4.38 | 22 | −0.36 | 0.06 | −0.74 | 0.02 |
| >75% | 32.27 | 8.99 | 4.73 | 3.17 | 15 | −0.67 | 0.01 | −1.18 | −0.16 |
| Hopelessness | |||||||||
| ≤25% | 11.49 | 4.71 | 7.98 | 5.04 | 40 | 0.87 | 0.00 | 0.48 | 1.27 |
| >25 to ≤50% | 11.05 | 4.84 | 4.42 | 2.87 | 14 | 0.63 | 0.01 | 0.14 | 1.11 |
| >50 to ≤75% | 11.11 | 4.73 | 3.46 | 2.13 | 21 | −0.38 | 0.14 | −0.88 | 0.13 |
| >75% | 10.70 | 4.86 | 1.57 | 0.89 | 9 | −0.36 | 0.20 | −0.92 | 0.19 |
| BIS-10 | |||||||||
| 0 | 64.06 | 17.52 | 71.26 | 16.37 | 36 | 0.85 | 0.0004 | 0.38 | 1.31 |
| >0 to ≤10% | 71.54 | 19.27 | 68.21 | 18.32 | 18 | 0.52 | 0.04 | 0.03 | 1.01 |
| >10 to ≤20% | 74.69 | 18.20 | 64.48 | 15.56 | 13 | −0.32 | 0.19 | −0.81 | 0.16 |
| >20% | 70.07 | 14.01 | 50.94 | 11.36 | 16 | −0.36 | 0.14 | −0.83 | 0.12 |
Abbreviations: BDI, Beck Depression Inventory; BDNF, brain-derived neurotrophic factor; BIS-10, Barrat Impulsiveness Scale; CI, confidence interval; I-DBT, intensive dialectical behavior therapy.
After adjustment for baseline clinical scores, the changes in methylation status over time were significantly associated with changes in depression scores (β=1.05, P=4.60 × 10−11, 95% CI 0.75–1.36), hopelessness scores (β=0.64, P=0.001, 95% CI 0.27–1.01) and impulsivity (β=0.51, P=0.0002, 95% CI 0.24–0.77). Adding antidepressant treatment (yes or no) and changes in medication during follow-up (yes or no) as covariates in the model did not modify the observed associations.
The results were similar when BDNF CpG exons IV and I were analyzed separately.
BDNF protein levels
At baseline, BPD subjects had significantly higher BDNF protein levels than controls (Supplementary Figure S2; β=1.13, P=2.51 × 10−6, 95% CI 0.69–1.58).
There was a significant decrease in BDNF protein levels over time in BPD subjects (β=−0.50, P=0.008, 95% CI −0.87 to −0.13), which was inversely associated with treatment response (β=−0.02, P=0.013, 95% CI −0.04 to −0.01 for depression; and β=−0.049, P=0.020, 95% CI −0.09 to −0.01 for hopelessness). Poor responders (⩽50% in BDI) showed a nonsignificant decrease in BDNF protein levels (β=−0.58, P=0.062, 95% CI −1.18 to 0.03), whereas responders (>50% in BDI) had a nonsignificant increase in protein levels (β=0.44, P=0.78, 95% CI 0.05–0.95). However, these changes were not significantly associated with changes in BDNF methylation status (β=−0.57, P=0.387, 95% CI −1.88 to 0.73). Furthermore, no association was found between protein levels and BDNF methylation status in the whole sample (controls and BPD; β=0.35, P=0.634, 95% CI −1.10 to 1.79).
Discussion
The present study supports the idea that DNA methylation is a dynamic process that underlines cognitive fluctuations in humans. Recently, Lopez et al.15 showed in a convincing study that changes in BDNF H3K27 methylation were associated with antidepressant response. Although it might be thought that these changes are restricted to antidepressant treatment and to histones, we found in this case that a psychotherapeutic approach can have the same impact on DNA CpG islands. Thus, our results underscore the fact that methylation changes in CpGs are associated with treatment response independently of the method used to treat patients. Our results showed that nonresponders showed an increase in BDNF methylation during treatment, whereas responders showed a decrease in BDNF methylation status. Subjects with the best response achieved the level of BDNF methylation found in control subjects. It is worth noting in the light of our findings that D'Addario et al.31 found higher DNA methylation in BDNF exon I promoter of bipolar disorder subjects during pharmacological treatment with mood stabilizers plus antidepressants compared with those exclusively on mood-stabilizing agents, suggesting that antidepressants may increase DNA methylation. We propose that this occurs when subjects are nonresponders to treatment.
The second issue is that BDNF methylation at CpG exons I and IV was significantly higher in BPD patients than in controls, an association that may be the consequence of adverse events occurring early in life. These results are consistent with previous findings showing that BPD subjects exhibited higher methylation status in several candidate genes including NR3C1, HTR2A, MAOA, MAOB and COMT.2, 32 They are also concordant with findings showing higher methylation of BDNF CpG exon IV in suicide victims, a phenotype closely related to BPD.12 Finally, the current data corroborate the increasing number of studies in animals and humans showing increased DNA and histone methylation of BDNF as well as of several other candidate genes in subjects who have endured early-life events such as childhood maltreatment.8, 9, 11, 33, 34, 35 Overall, these studies and ours strongly support the idea that maltreatment is associated with the broad epigenetic signature of genes crucially involved in brain function and development.
We also found a significant higher level of BDNF protein in patients than in controls. This is a striking result as most studies in depression to date have found lower BDNF levels in patients than in controls.36 BPD subjects are usually treated for years with antidepressants and other psychotropic medications. This chronic treatment may have biased the level of BDNF measurements. Indeed, although it is generally accepted that depressed patients have decreased serum BDNF levels, treatment with antidepressants is also widely known to promote an increase in these levels.37 To our knowledge, only one study has examined BDNF proteins levels and found lower levels of this protein in BPD subjects.5 These discrepant results definitely need to be explored in future studies. Another point relating to BDNF protein levels is the fact that, contrary to the results obtained by Lopez et al.15 showing that BDNF H3K27 methylation correlated with BDNF protein levels, we were unable to find any correlation between DNA methylation at CpG exons I and IV and BDNF protein levels. The first obvious explanation is that it may be more difficult to correlate CpG DNA methylation at two specific exons only with changes in protein levels in peripheral blood. Methylation at histones may be a more suitable candidate for this. BDNF shows a complex gene architecture described extensively in several previous papers38 with different splice variants of BDNF mRNA differing by the 5' extremity, each regulated by specific promoter regions.39 These different BDNF mRNA splice variants underline the tissue- and time-specific regulation of BDNF expression.40 In addition to this complex control at the promoter level, BDNF expression is also regulated at the posttranscriptional level during cleavage of pro-BDNF into mature BDNF by means of several mechanisms.41 This complexity may thus explain the problems experienced in linking BDNF protein levels to CpG methylation. We decided to focus on the promoter of BDNF CpG exon I, as it has been described as the brain-specific inducible promoter,42 and on CpG exon IV, as it has previously been shown to be sensitive to environmental factors.35 In addition, the methyl-CpG-binding protein 2 (MeCP2), which is known to repress BDNF gene transcription, binds selectively to methylated DNA at the promoter of exon IV,43 and is thus of particular interest for epigenetic regulation. Moreover, the latter promoter region contains a specific binding site for the cyclic AMP-responsive element-binding protein (CREB),38 which is of particular interest in suicidal behavior and consequently for BPD. Moreover, another gene called antiBDNF (or BDNFOS) overlaps with the BDNF gene and is transcribed in reverse orientation.44 Recently, Pruunsild et al.39 showed that BDNF and antiBDNF transcripts form dsRNA duplexes in brain in vivo. These findings reveal that antiBDNF mRNAs seem to have a significant role in regulating BDNF expression in humans. Its regulatory functions could act directly to inhibit BDNF translation into protein.39 Consequently, the discrepancy between BDNF protein levels and BDNF methylation levels could be because of a low level of antiBDNF mRNAs, which leads to an increase in BDNF expression without any correlation with methylation levels of BDNF. Finally, the origin of plasma or serum BDNF is still unknown. It has been shown that blood BDNF is essentially stored in blood platelets, from which it can be released into the plasma through activation or clotting processes.45 As DNA methylation was assessed on lymphocyte DNA in the current study, its effect on BDNF expression (probably a decrease) fails to overcome the massive effect of platelet release.
This study has several limitations that may, in part, explain the striking results showing no correlation between BDNF protein levels and BDNF DNA methylation. One is that we used peripheral blood that may only be a proxy for what is happening in the brain. Secondarily, most of our subjects were under psychotropic treatment, especially antidepressants. Our findings may not actually be attributable to psychotherapy. Nevertheless, our results were unchanged after adjustment for antidepressant status (taking or not), which indicates at least that the observed association is independent of this medication. We may also be dealing with natural fluctuations in methylation over time. A control sample followed up for the same period would be required to exclude this hypothesis definitively. The duration of follow-up (4 weeks of treatment) was relatively small in length. A longer duration would ideally be needed in the future to establish a firm correlation between response to treatment and changes in methylation status. An additional limitation pertains to the specificity of our findings. In other words, are the changes in methylation status observed in our study specific to BDNF? In order to answer this question, we took the opportunity to assess the methylation status of the exon 1F NR3C1 promoter region in 61 of the BPD subjects participating in our previous report for which we had available DNA at baseline and on the last day of I-DBT.2 Analyzing these data, we observed that there was absolutely no changes in the NR3C1 methylation status between the two measures (mean methylation status at baseline and at the end of I-DBT=0.134 (s.d.=0.02) and 0.134 (s.d.=0.02), respectively; P=0.758). This result strongly suggests that our current findings are specific to BDNF. Finally, other environmental factors that were not measured in this study may have modified DNA methylation during follow-up.
In conclusion, these results provide further support for the impact of environmental factors on BDNF epigenetic processes. First, they provide further evidence of the relationship between child maltreatment, higher DNA methylation of BDNF and the development of adulthood psychopathology. Therefore, it may be possible to use BDNF methylation status as a biological marker of this pathway. Second, they support the idea that these epigenetic marks are susceptible to change through targeted therapeutic approaches and may underlie the amelioration in cognitive function. Thus, evaluation of BDNF methylation levels may have relevance in predicting response to treatment. This hypothesis clearly needs to be extended in future studies to determine whether this is truly the case.
Acknowledgments
We thank Dominique Mouthon and Monique Vessaz for data management and DNA extraction and for technical support. We also thank Gérald Bouillault, Jean-Jaques Kunckler, Brigitte Blanchon, Venus Kaby, and Karen Dieben for the data collection. This work was supported by AXA Research Fund ‘Vulnerability to risky behaviors as anomalies in neuro-developmental trajectories: an individualized approach' granted to Alain Malafosse.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
Supplementary Material
References
- Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. 2011;377:74–84. doi: 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- Perroud N, Paoloni-Giacobino A, Prada P, Olié E, Salzmann A, Nicastro R, et al. Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: a link with the severity and type of trauma. Transl Psychiatry. 2011;1:e59. doi: 10.1038/tp.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner S, Baskaya O, Dahmen N, Lieb K, Tadic A. Modulatory role of the brain-derived neurotrophic factor Val66Met polymorphism on the effects of serious life events on impulsive aggression in borderline personality disorder. Genes Brain Behav. 2010;9:97–102. doi: 10.1111/j.1601-183X.2009.00539.x. [DOI] [PubMed] [Google Scholar]
- Tadic A, Elsasser A, Victor A, von Cube R, Baskaya O, Wagner S, et al. Association analysis of serotonin receptor 1B (HTR1B) and brain-derived neurotrophic factor gene polymorphisms in Borderline personality disorder. J Neural Transm. 2009;116:1185–1188. doi: 10.1007/s00702-009-0264-3. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Yuan P, Diaz GA, Guerreri S, Dorantes C, Mayson S, et al. Platelet protein kinase C and brain-derived neurotrophic factor levels in borderline personality disorder patients. Psychiatry Res. 2012;199:92–97. doi: 10.1016/j.psychres.2012.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzinga BM, Molendijk ML, Oude Voshaar RC, Bus BA, Prickaerts J, Spinhoven P, et al. The impact of childhood abuse and recent stress on serum brain-derived neurotrophic factor and the moderating role of BDNF Val66Met. Psychopharmacology (Berl) 2011;214:319–328. doi: 10.1007/s00213-010-1961-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlovsky N, Matar MA, Kaplan Z, Kotler M, Zohar J, Cohen H. Long-term down-regulation of BDNF mRNA in rat hippocampal CA1 subregion correlates with PTSD-like behavioural stress response. Int J Neuropsychopharmacol. 2007;10:741–758. doi: 10.1017/S1461145707007560. [DOI] [PubMed] [Google Scholar]
- Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9:519–525. doi: 10.1038/nn1659. [DOI] [PubMed] [Google Scholar]
- Roth TL, Zoladz PR, Sweatt JD, Diamond DM. Epigenetic modification of hippocampal Bdnf DNA in adult rats in an animal model of post-traumatic stress disorder. J Psychiatr Res. 2011;45:919–926. doi: 10.1016/j.jpsychires.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubin FD, Roth TL, Sweatt JD. Epigenetic regulation of BDNF gene transcription in the consolidation of fear memory. J Neurosci. 2008;28:10576–10586. doi: 10.1523/JNEUROSCI.1786-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth TL, Lubin FD, Funk AJ, Sweatt JD. Lasting epigenetic influence of early-life adversity on the BDNF gene. Biol Psychiatry. 2009;65:760–769. doi: 10.1016/j.biopsych.2008.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller S, Sarchiapone M, Zarrilli F, Videtic A, Ferraro A, Carli V, et al. Increased BDNF promoter methylation in the Wernicke area of suicide subjects. Arch Gen Psychiatry. 2010;67:258–267. doi: 10.1001/archgenpsychiatry.2010.9. [DOI] [PubMed] [Google Scholar]
- Sen S, Duman R, Sanacora G. Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biol Psychiatry. 2008;64:527–532. doi: 10.1016/j.biopsych.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molendijk ML, Bus BA, Spinhoven P, Penninx BW, Kenis G, Prickaerts J, et al. Serum levels of brain-derived neurotrophic factor in major depressive disorder: state-trait issues, clinical features and pharmacological treatment. Mol Psychiatry. 2011;16:1088–1095. doi: 10.1038/mp.2010.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez JP, Mamdani F, Labonte B, Beaulieu MM, Yang JP, Berlim MT, et al. Epigenetic regulation of BDNF expression according to antidepressant response Mol Psychiatryadvance online publication, 1 May 2012; doi: 10.1038/mp.2012.38 [DOI] [PMC free article] [PubMed]
- Chen ES, Ernst C, Turecki G. The epigenetic effects of antidepressant treatment on human prefrontal cortex BDNF expression. Int J Neuropsychopharmacol. 2011;14:427–429. doi: 10.1017/S1461145710001422. [DOI] [PubMed] [Google Scholar]
- Perroud N, Uher R, Dieben K, Nicastro R, Huguelet P. Predictors of response and drop-out during intensive dialectical behavior therapy. J Pers Disord. 2010;24:634–650. doi: 10.1521/pedi.2010.24.5.634. [DOI] [PubMed] [Google Scholar]
- Perroud N, Nicastro R, Jermann F, Huguelet P. Mindfulness skills in borderline personality disorder patients during dialectical behavior therapy: preliminary results. Int J Psychiatry Clin Pract. 2012;16:189–196. doi: 10.3109/13651501.2012.674531. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer R, Williams JBW, Smith Benjamin L. Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) American Psychiatric Association: Washington DC; 1994. [Google Scholar]
- Preisig M, Fenton BT, Matthey ML, Berney A, Ferrero F. Diagnostic interview for genetic studies (DIGS): inter-rater and test-retest reliability of the French version. Eur Arch Psychiatry Clin Neurosci. 1999;249:174–179. doi: 10.1007/s004060050084. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Bayle FJ, Bourdel MC, Caci H, Gorwood P, Chignon JM, Ades J, et al. [Factor analysis of French translation of the Barratt impulsivity scale (BIS-10)] Can J Psychiatry. 2000;45:156–165. doi: 10.1177/070674370004500206. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire. A Retrospective Self-Report. The Psychological Corporation: San Antonio, USA; 1998. [Google Scholar]
- McQuillan A, Nicastro R, Guenot F, Girard M, Lissner C, Ferrero F. Intensive dialectical behavior therapy for outpatients with borderline personality disorder who are in crisis. Psychiatr Serv. 2005;56:193–197. doi: 10.1176/appi.ps.56.2.193. [DOI] [PubMed] [Google Scholar]
- Wojdacz TK, Dobrovic A, Algar EM. Rapid detection of methylation change at H19 in human imprinting disorders using methylation-sensitive high-resolution melting. Hum Mutat. 2008;29:1255–1260. doi: 10.1002/humu.20779. [DOI] [PubMed] [Google Scholar]
- Wojdacz TK, Dobrovic A, Hansen LL. Methylation-sensitive high-resolution melting. Nat Protoc. 2008;3:1903–1908. doi: 10.1038/nprot.2008.191. [DOI] [PubMed] [Google Scholar]
- Karege F, Bondolfi G, Gervasoni N, Schwald M, Aubry JM, Bertschy G. Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry. 2005;57:1068–1072. doi: 10.1016/j.biopsych.2005.01.008. [DOI] [PubMed] [Google Scholar]
- Uher R, Maier W, Hauser J, Marusic A, Schmael C, Mors O, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry. 2009;194:251–258. doi: 10.1192/bjp.bp.108.057554. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. Stata Press: College Station, TX; 2005. [Google Scholar]
- D'Addario C, Dell'Osso B, Palazzo MC, Benatti B, Lietti L, Cattaneo E, et al. Selective DNA methylation of BDNF promoter in bipolar disorder: differences among patients with BDI and BDII. Neuropsychopharmacology. 2012;37:1647–1655. doi: 10.1038/npp.2012.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dammann G, Teschler S, Haag T, Altmuller F, Tuczek F, Dammann RH. Increased DNA methylation of neuropsychiatric genes occurs in borderline personality disorder. Epigenetics. 2011;6:1454–1462. doi: 10.4161/epi.6.12.18363. [DOI] [PubMed] [Google Scholar]
- McGowan PO, Suderman M, Sasaki A, Huang TC, Hallett M, Meaney MJ, et al. Broad epigenetic signature of maternal care in the brain of adult rats. PLoS One. 2011;6:e14739. doi: 10.1371/journal.pone.0014739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan PO, Szyf M. The epigenetics of social adversity in early life: implications for mental health outcomes. Neurobiol Dis. 2010;39:66–72. doi: 10.1016/j.nbd.2009.12.026. [DOI] [PubMed] [Google Scholar]
- Fuchikami M, Yamamoto S, Morinobu S, Takei S, Yamawaki S. Epigenetic regulation of BDNF gene in response to stress. Psychiatry Investig. 2010;7:251–256. doi: 10.4306/pi.2010.7.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karege F, Perret G, Bondolfi G, Schwald M, Bertschy G, Aubry JM. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002;109:143–148. doi: 10.1016/s0165-1781(02)00005-7. [DOI] [PubMed] [Google Scholar]
- Shimizu E, Hashimoto K, Okamura N, Koike K, Komatsu N, Kumakiri C, et al. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry. 2003;54:70–75. doi: 10.1016/s0006-3223(03)00181-1. [DOI] [PubMed] [Google Scholar]
- Boulle F, van den Hove DL, Jakob SB, Rutten BP, Hamon M, van Os J, et al. Epigenetic regulation of the BDNF gene: implications for psychiatric disorders. Mol Psychiatry. 2012;17:584–596. doi: 10.1038/mp.2011.107. [DOI] [PubMed] [Google Scholar]
- Pruunsild P, Kazantseva A, Aid T, Palm K, Timmusk T. Dissecting the human BDNF locus: bidirectional transcription, complex splicing, and multiple promoters. Genomics. 2007;90:397–406. doi: 10.1016/j.ygeno.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An JJ, Gharami K, Liao GY, Woo NH, Lau AG, Vanevski F, et al. Distinct role of long 3' UTR BDNF mRNA in spine morphology and synaptic plasticity in hippocampal neurons. Cell. 2008;134:175–187. doi: 10.1016/j.cell.2008.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker PA. Whither proBDNF. Nat Neurosci. 2009;12:105–106. doi: 10.1038/nn0209-105. [DOI] [PubMed] [Google Scholar]
- Timmusk T, Palm K, Metsis M, Reintam T, Paalme V, Saarma M, et al. Multiple promoters direct tissue-specific expression of the rat BDNF gene. Neuron. 1993;10:475–489. doi: 10.1016/0896-6273(93)90335-o. [DOI] [PubMed] [Google Scholar]
- Im HI, Hollander JA, Bali P, Kenny PJ. MeCP2 controls BDNF expression and cocaine intake through homeostatic interactions with microRNA-212. Nat Neurosci. 2010;13:1120–1127. doi: 10.1038/nn.2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu QR, Walther D, Drgon T, Polesskaya O, Lesnick TG, Strain KJ, et al. Human brain derived neurotrophic factor (BDNF) genes, splicing patterns, and assessments of associations with substance abuse and Parkinson's Disease. Am J Med Genet B Neuropsychiatr Genet. 2005;134B:93–103. doi: 10.1002/ajmg.b.30109. [DOI] [PubMed] [Google Scholar]
- Fujimura H, Altar CA, Chen R, Nakamura T, Nakahashi T, Kambayashi J, et al. Brain-derived neurotrophic factor is stored in human platelets and released by agonist stimulation. Thromb Haemost. 2002;87:728–734. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.