Abstract
Background:
The regenerating gene Iα (REG Iα) is involved in gastric carcinogenesis as an antiapoptotic factor. Therefore, we investigated whether REG Iα confers resistance to chemotherapeutic drugs in gastric cancer (GC) cells and whether REG Iα expression is useful for predicting the response to chemotherapy and outcome in patients with GC.
Methods:
A total of 70 patients with unresectable stage IV GC received first-line chemotherapy with S-1 and cisplatin (S-1/CDDP). The expression of REG Iα was evaluated immunohistochemically using biopsy samples obtained before chemotherapy, and its relationship to clinicopathological parameters was analysed statistically. The effects of REG Iα gene induction on resistance to 5-FU or CDDP treatment were examined by cell survival assay and flow cytometry.
Results:
Of the 70 patients with unresectable stage IV GC, 19 (27%) were positive for REG Iα expression. The expression of REG Iα was independently predictive of poorer progression-free and overall survival in such patients (hazard ratio (HR) 2.46; P=0.002 and HR 1.89; P=0.037, respectively). The gene induction of REG Iα conferred resistance to cell death induced by 5-FU or CDDP in GC cells.
Conclusion:
In patients with stage IV GC, REG Iα, which confers resistance to chemotherapeutic drugs in GC cells, is a potential biomarker for predicting resistance to S-1/CDDP treatment.
Keywords: REG, biomarker, chemotherapy, prognosis, apoptosis, gastric cancer
Gastric cancer (GC) is a major cause of cancer-related death worldwide (Kamangar et al, 2006; Ferlay et al, 2010), and the outcome of patients with unresectable GC is very poor (Chau et al, 2004; Lee et al, 2007). Recently, advances in chemotherapy have considerably improved the prognosis of patients with unresectable GC, and subsequently the combination of S-1 (comprising a prodrug of 5-fluorouracil, 5-chloro-2,4-dihydropyrimidine, and potassium oxonate) with cisplatin (S-1/CDDP) has been accepted as a first-line therapy for such patients in Japan (Boku, 2008; Koizumi et al, 2008; Ohtsu, 2008). However, the response to chemotherapy is known to differ widely among such patients, and in fact GC patients who show a poor response to first-line chemotherapy are considered to have a dismal prognosis (Matsubara et al, 2008; Choi et al, 2011; Park et al, 2011). In this connection, reliable biomarkers that are able to predict the response to chemotherapy are urgently needed to improve the efficiency of chemotherapy for patients with unresectable GC.
The regenerating gene (Reg) was originally isolated from rat regenerating pancreatic islet cells (Terazono et al, 1988), and thereafter Reg was shown to have a trophic effect on gastric epithelial cells (Fukui et al, 1998). Recently, its human homologue, REG Iα, was identified by microarray analysis as a gene distinctly overexpressed in GC tissues (Takaishi and Wang, 2007), and indeed several studies have indicated that REG Iα is overexpressed in a subset of GC patients (Yonemura et al, 2003; Fukui et al, 2004; Yamagishi et al, 2009). Moreover, we have previously clarified that REG Iα functions as an antiapoptotic factor in the development of GC (Sekikawa et al, 2005, 2008). These findings suggest that REG Iα plays a pivotal role in gastric carcinogenesis, and thus it is tempting to speculate that an antiapoptotic effect of REG Iα may be associated with a poor response to chemotherapy in patients with GC. Therefore, in the present study we examined whether REG Iα is involved in acquisition of resistance to chemotherapeutic drugs in GC cells. Moreover, we aimed to clarify whether REG Iα expression in biopsy samples before treatment could be a useful biomarker for predicting the response to chemotherapy and outcome in patients with unresectable GC.
Materials and methods
Patients, procedures, and tissue samples
A total of 70 patients who were diagnosed as having unresectable GC at Osaka Red Cross Hospital between 2007 and 2011 were enroled. Patients were eligible if they were diagnosed as having stage IV GC by oesophagogastroduodenoscopy (EGDS) and abdominopelvic computed tomography (CT), and moreover had histologically confirmed adenocarcinoma. Patients with recurrent gastric cancer or other malignancies and those who had received previous chemotherapy or radiotherapy were excluded. Patients with an Eastern Cooperative Oncology Group (ECOG) performance status of 3 or 4 and those without adequate organ function were also excluded. Stage classification was done in accordance with the criteria of the Japanese Gastric Cancer Association (Japanese Gastric Cancer Association, 1998).
All patients received first-line chemotherapy with S-1/CDDP for unresectable GC, as reported previously (Koizumi et al, 2008). Briefly, S-1 was given orally twice for the first 3 weeks of a 5-week cycle. The dose of S-1 administered each time was determined according to each patient's body surface area as follows: <1.25 m2, 40 mg; 1.25–1.50 m2, 50 mg; and >1.5 m2, 60 mg. Intravenous infusion of CDDP (60 mg m−2) was administrated on day 8 of each cycle. Treatment was repeated until one of the following occurred: progressive disease, unacceptable toxic side effect, and withdrawal of the patient's consent. If the S-1/CDDP chemotherapy failed, second-line chemotherapy was recommended for all patients if they had adequate organ function and performance status. Of the 70 patients, 49 (70.0%) received second-line chemotherapy; 27 patients (55.1%) were treated with irrinotecan-based regimens and 22 (44.9%) were treated with taxane-based regimens. The patients who exchanged to second-line treatment without progressive disease because of adverse reactions were censored. To evaluate tumour responses to S-1/CDDP chemotherapy, tumours were measured after every two courses of chemotherapy using CT or MRI imaging. Tumour responses were classified according to the Response Evaluation Criteria for Solid Tumours (RECIST) (Therasse et al, 2000). The patients who had no measurable lesions were excluded. Progression-free survival (PFS) was defined as the time from the first day of chemotherapy to the date of onset of progressive disease during treatment with S-1/CDDP or death from any cause. Overall survival (OS) was defined as time from the first day of chemotherapy to the date of death because of any cause.
The biopsy samples from GC tissues were obtained by EGDS before chemotherapy and examined for the study. The tissue samples were fixed in 10% formalin and embedded in paraffin. Multiple haematoxylin–eosin-stained sections of all 70 lesions were examined. The tissue sections were also subjected to immunostaining. The following factors were determined for all patients and lesions: age, gender, performance status, tumour location, macroscopic type, Lauren's histological classification, location of metastasis, number of metastatic organs, serum albumin, alkaline phosphatase, CEA, and CA19-9. The clinicopathological features of the patients are summarised in Table 1.
Table 1. Univariate analyses of progression-free and overall survival in patients with unresectable stage IV gastric cancer treated with S-1/CDDP.
| Characteristics | Number of patients | Median PFS | P-value | Median OS | P-value |
|---|---|---|---|---|---|
|
Age (years, range; 38–78) | |||||
| <60 | 16 (22.9%) | 4.0 | 0.667 | 10.0 | 0.112 |
| ⩾60 |
54 (77.1%) |
5.8 |
|
12.8 |
|
|
Gender | |||||
| Male | 48 (68.6%) | 5.5 | 0.340 | 12.4 | 0.580 |
| Female |
22 (31.4%) |
5.4 |
|
10.3 |
|
|
Performance status | |||||
| 0 | 53 (75.7%) | 5.5 | 0.261 | 14.5 | 0.284 |
| 1–2 |
17 (24.3%) |
5.4 |
|
10.4 |
|
|
Location | |||||
| Fundus | 50 (71.4%) | 4.7 | 0.986 | 10.6 | 0.145 |
| Antrum |
20 (28.6%) |
6.0 |
|
14.6 |
|
|
Macroscopic type | |||||
| Scirrhous | 13 (18.6%) | 3.8 | 0.058 | 10.0 | 0.028 |
| Nonscirrhous |
57 (81.4%) |
5.8 |
|
12.4 |
|
|
Lauren's classification | |||||
| Intestinal | 34 (48.6%) | 5.4 | 0.919 | 13.0 | 0.197 |
| Diffuse |
36 (51.4%) |
5.4 |
|
10.0 |
|
|
Liver metastasis | |||||
| Yes | 31 (44.3%) | 4.8 | 0.136 | 10.2 | 0.176 |
| No |
39 (55.7%) |
6.0 |
|
13.0 |
|
|
Peritoneal dissemination | |||||
| Yes | 31 (44.3%) | 5.4 | 0.956 | 12.4 | 0.427 |
| No |
39 (55.7%) |
5.5 |
|
10.6 |
|
|
Other metastasis | |||||
| Yes | 17 (24.3%) | 4.9 | 0.198 | 10.3 | 0.239 |
| No |
53 (75.7%) |
5.7 |
|
12.4 |
|
|
Number of metastatic organs | |||||
| One | 18 (25.7%) | 6.3 | 0.320 | 12.8 | 0.234 |
| More than two |
52 (74.3%) |
4.8 |
|
11.1 |
|
|
Albumin (mg dl−1, range; 2.2–4.6) | |||||
| <3.5 | 28 (40.0%) | 4.1 | 0.210 | 10.2 | 0.202 |
| ⩾3.5 |
42 (60.0%) |
6.2 |
|
12.4 |
|
|
ALP (IU l−1, range; 96–3696) | |||||
| <339 | 54 (77.2%) | 5.5 | 0.828 | 12.4 | 0.968 |
| ⩾339 |
16 (22.8%) |
6.0 |
|
11.5 |
|
|
CEA (mg dl−1, range; 1–8040) | |||||
| <5.0 | 35 (50.0%) | 5.8 | 0.690 | 13.0 | 0.572 |
| ⩾5.0 |
35 (50.0%) |
4.9 |
|
11.1 |
|
|
CA19-9 (mg dl−1, range; 1–182 500) | |||||
| <37 | 40 (57.4%) | 4.8 | 0.622 | 12.8 | 0.317 |
| ⩾37 | 30 (42.6%) | 5.7 | 10.2 | ||
Abbreviations: ALP=alkaline phosphatase; CA=carbohydrate antigen; CEA=carcinoembryonic antigen; OS=overall survival; PFS=progression-free survival; S-1/CDDP=S-1 and cisplatin.
This study was carried out with the approval of the Osaka Red Cross Hospital Ethical Committee, and informed consent was obtained from all patients.
Immunohistochemical staining
Immunohistochemical staining for REG Iα was performed with a LSAB-2 kit (DAKO, Kyoto, Japan) as described previously (Yamagishi et al, 2009), using anti-human REG Iα antibody (dilution 1 : 1000). The monoclonal antibody for human REG Iα was generated against human REG Iα corresponding to positions 23–166 of the deduced human REG Iα (Watanabe et al, 1990). The specificity of the antibody was proven by not only western blot analysis (Watanabe et al, 1990) but also immunohistochemistry (Satomura et al, 1993). Finally, the sections were incubated in 3,3′-diaminobenzide tetrahydrochloride with 0.05% H2O2 for 3 min and then counterstained with Mayer's haematoxylin. The percentage of cancer cells stained with anti-human REG Iα antibody was evaluated. A specimen was considered positive when >10% of cancer cells were stained. When <10% of cancer cells were stained, immunostaining was considered negative. When multiple biopsy samples were obtained from the lesion, the patient was considered as positive if at least one sample is positive.
Transfection and expression of the human REG Iα cDNA in gastric cancer cell line
A human gastric cancer cell line AGS was maintained routinely in Ham's F12 medium (Invitrogen, Grand Island, NY, USA) with 10% fetal bovine serum (Sigma Chemical Co., St Louis, MO, USA) in a humidified incubator at 37 °C with an atmosphere of 5% CO2.
The full-length human REG Iα cDNA was inserted in the pIRES2-EGFP vector (Clontech, Palo Alto, CA, USA). The construct was named pIRES2-hREG Iα, and the pIRES2-EGFP vector without an insert was used as control. The AGS cells, stably transfected with pIRES2-hREG Iα (AGS-REG Iα) or pIRES2-EGFP (AGS-EGFP) vectors, were prepared as previously described (Sekikawa et al, 2005).
Cell survival assay
5-Fluorouracil (5-FU; Wako Pure Chemical Industries, Ltd, Osaka, Japan) and CDDP (Wako) were dissolved in dimethylsulphoxide and then diluted in culture medium for experiments. The AGS-REG Iα cells or AGS-EGFP cells (2 × 104) were plated in 12-well microplates (IWAKI, Funabashi, Japan). The cells were then treated with 5-FU (0.2–20 mℳ) or CDDP (1–100 μℳ) in serum-free medium for 30 h. Thereafter, both floating and attached cells were collected, and the number of surviving cells was evaluated by Trypan blue exclusion.
Cell death assay
The AGS-REG Iα cells or AGS-EGFP cells (2.5 × 105) were plated in 6 cm dishes (IWAKI). The cells were treated with 5-FU or CDDP for 24 h and collected as described above. After washing with PBS, the cells were incubated with propidium iodide in binding buffer in accordance with the manufacturer's protocol. Stained cells were analysed on a FACScalibur flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA), and the data obtained were analysed using CELL-QUEST software (Becton Dickinson).
Statistical analysis
Statview 5.0J statistical software (Abacus Concepts Inc., Berkeley, CA, USA) was used for all analyses. Cumulative survival rate was evaluated by the Kaplan–Meier method and analysed by the log-rank test. The χ2 analyses were performed to investigate the relationship between REG Iα expression and clinicopathological features, and Fisher's exact analyses were also used, as necessary. Univariate and multivariate Cox regression analyses were used to examine whether REG Iα expression was an independent predictor of PFS or OS. All values were expressed as the mean±s.e.m. The data for cell survival and death were analysed using unpaired two-tailed t-test. The P-values of <0.05 were considered to indicate statistical significance.
Results
Outcome of first-line treatment with S-1/CDDP in patients with stage IV unresectable GC
A total of 348 cycles (median of 5.0 cycles for each patient (range 1–17)) of S-1/CDDP treatment were administered. Median follow-up period was 12.4 (mean 12.8; range 2–42) months. No treatment-related deaths were identified during the study. Among the 70 patients treated with S-1/CDDP, 2 (2.9%) showed a complete response and 23 (33%) showed a partial response, giving an overall response rate of 36%. The median PFS and OS for the patients overall were 5.4 months (95% CI, 4.8–6.2) and 12.3 months (95% CI, 11.1–13.5), respectively (Supplementary Figure 1). Regarding the relationship between outcome and response to S-1/CDDP treatment, the median OS was significantly longer in responders (18.3 months, 95% CI, 16.1–20.5) than in nonresponders (9.3 months, 95% CI, 7.9–10.8, P=0.0002). These outcomes were consistent with previous reports describing S-1/CDDP treatment in patients with unresectable GC (Koizumi et al, 2008).
Relationship between PFS or OS and clinicopathological features
In patients with scirrhous-type GC, PFS tended to be shorter (P=0.058, Table 1) and OS was significantly shorter (P=0.028, Table 1) than those in patients with nonscirrhous-type GC. None of the other parameters, including age, gender, performance status, Lauren's classification, liver metastasis, peritoneal dissemination, number of metastatic organs, serum albumin, ALP, CEA, or CA19-9, had a significant relationship to PFS or OS (Table 1).
Relationship between REG Iα expression and clinicopathological features in patients with unresectable GC
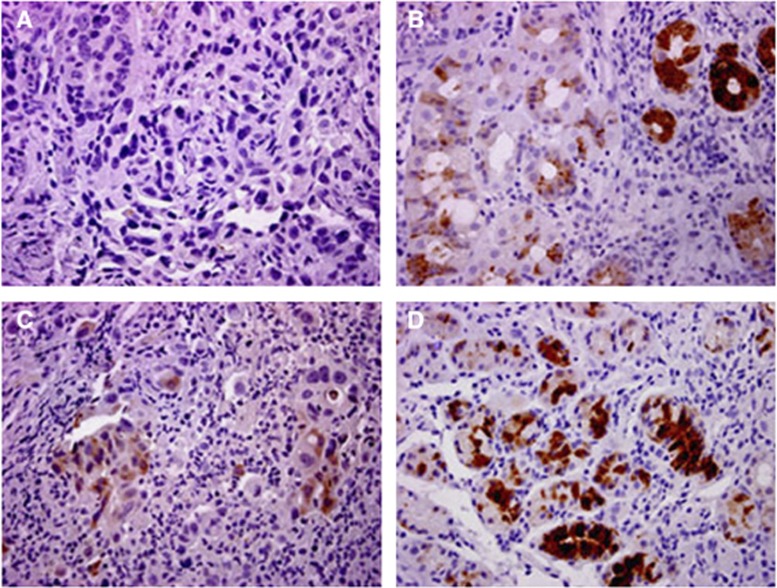
The expression of REG Iα was evaluated immunohistochemically in biopsy samples from patients with unresectable GC before chemotherapy. Among the 70 patients examined, 19 (27%) were positive for REG Iα expression (Figure 1). Regarding the clinicopathological features in patients with stage IV GC, REG Iα expression showed no relationship to any of the clinicopathological features investigated (Supplementary Table 1).
Figure 1.
Immunostaining of REG Iα in biopsy samples obtained from gastric cancer tissues. The biopsy samples were obtained before chemotherapy (A, B, and D) and after disease progression (C). (A) The REG Iα-negative gastric cancer (diffuse type). (B) The REG Iα-positive gastric cancer (intestinal type). (C) The REG Iα-positive gastric cancer (diffuse type). This sample was obtained from the same patient as that in (A) when he developed disease progression after S-1/CDDP treatment. (D) The REG Iα-positive signet-ring cell carcinoma (diffuse type).
REG Iα expression is predictive of response to S-1/CDDP treatment
We examined the relationship between REG Iα expression in pretreatment biopsy samples and the subsequent response to S-1/CDDP treatment. Among the 19 patients with REG Iα-positive unresectable GC, only 1 (5%) showed partial response to S-1/CDDP treatment, whereas the remaining 18 patients showed stable or progressive disease. In contrast, among the 51 REG Iα-negative patients, 2 had a complete response and 22 had a partial response; that is, 47% of REG Iα-negative patients responded to S-1/CDDP treatment. The difference in response to S-1/CDDP treatment between the REG Iα-positive and REG Iα-negative groups was significant (P=0.0084; Table 2).
Table 2. Association of REG Iα expression with response to S-1/CDDP treatment.
| |
REG Iα
expression |
|
|
|---|---|---|---|
| Negative | Positive | P-value | |
| CR |
2 |
0 |
|
| PR |
22 |
1 |
0.0084 |
| SD |
13 |
6 |
|
| PD | 14 | 12 | |
Abbreviations: CR=complete response; PD=progressive disease; PR=partial response; REG Iα=regenerating gene Iα; SD=stable disease; S-1/CDDP=S-1 and cisplatin.
Moreover, we investigated whether the expression of REG Iα changed in patients with unresectable GC after disease progression. Among the 10 patients whose GC had been negative for REG Iα before S-1/CDDP treatment, 8 became positive for REG Iα after disease progression (Figure 1).
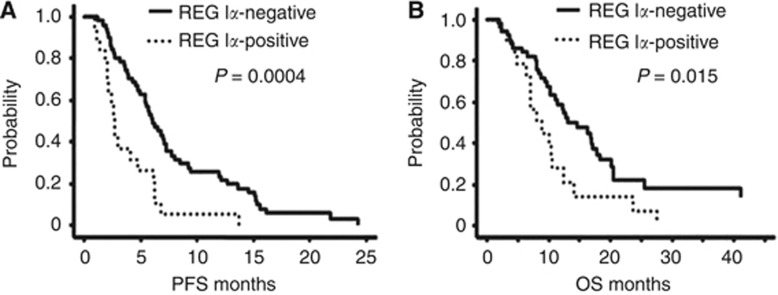
REG Iα expression is prognostic for patients with unresectable GC treated with S-1/CDDP
To evaluate the prognostic significance of REG Iα expression in patients treated with S-1/CDDP, we constructed Kaplan–Meier curves (Figure 2). The patients with REG Iα-positive GC had a significantly worse PFS than those without (P=0.0004, Figure 2A). In addition, the patients positive for REG Iα had a significantly worse OS than those who were negative (P=0.015, Figure 2B).
Figure 2.
(A) Progression-free survival (PFS) and (B) overall survival (OS) according to REG Iα expression in patients with unresectable stage IV GC who received first-line treatment with S-1/CDDP. Kaplan–Meier curves were constructed and pairwise differences were analysed by log-rank test.
To confirm whether GC patients are possible to be subdivided, we classified GC patients into four groups according to REG index in biopsy samples as follows: group 0 (0%, n=37), group I (1–9%, n=14), group II (10–49%, n=12), and group III (50–100%, n=7). The PFS and OS were not significantly different between group 0 and group I but those were significantly worse in group II than in group I (P=0.015 and 0.024, respectively). On the other hand, PFS and OS were not significantly different between group II and group III, although these were significantly worse in group II/III than in group I (P=0.0005 and 0.0261, respectively).
We next examined whether REG Iα expression is an independent factor predictive of PFS and OS. Univariate analysis indicated that macroscopic type as well as REG Iα expression was predictive of PFS in patients with unresectable GC after S-1/CDDP treatment (P=0.058 and 0.0004, respectively). Furthermore, multivariate analysis revealed that REG Iα expression was an independent factor predictive of PFS in these patients (P=0.002, Table 3).
Table 3. Univariate and multivariate analyses of progression-free and overall survival in patients with unresectable stage IV gastric cancer treated with S-1/CDDP.
| PFS | OS | |||||
|---|---|---|---|---|---|---|
|
Univariate |
Multivariate |
Univariate |
Multivariate |
|||
| P-value | 95% CI | P-value | P-value | 95% CI | P-value | |
|
Macroscopic type | ||||||
| Nonscirrhous | 1 | 1 | ||||
| Scirrhous |
0.058 |
1.52 (0.81–2.87) |
0.195 |
0.028 |
1.81 (0.94–3.47) |
0.075 |
|
REG Iα expression | ||||||
| Negative | 1 | 1 | ||||
| Positive | 0.0004 | 2.46 (1.37–4.35) | 0.002 | 0.015 | 1.89 (1.04–3.44) | 0.037 |
Abbreviations: CI=confidence interval; OS=overall survival; PFS=progression-free survival; REG Iα=regenerating gene Iα; S-1/CDDP=S-1 and cisplatin.
With regard to OS in the patients investigated, univariate analysis showed that macroscopic type and REG Iα expression were predictive factors. Similarly for PFS, multivariate analysis revealed that REG Iα expression was an independent factor predictive of OS in patients with unresectable GC after S-1/CDDP treatment (P=0.037, Table 3).
Although we performed multivariate analysis by adding two more categories (liver metastasis and other metastasis) in multivariate analysis for PFS, REG Iα expression remained to be an independent factor predictive of PFS in patients with GC after S-1/CDDP treatment (P=0.0075). On the other hand, we added two more categories (age and location) in multivariate analysis for OS. The expression of REG Iα was also an independent factor predictive of OS in these patients (P=0.047).
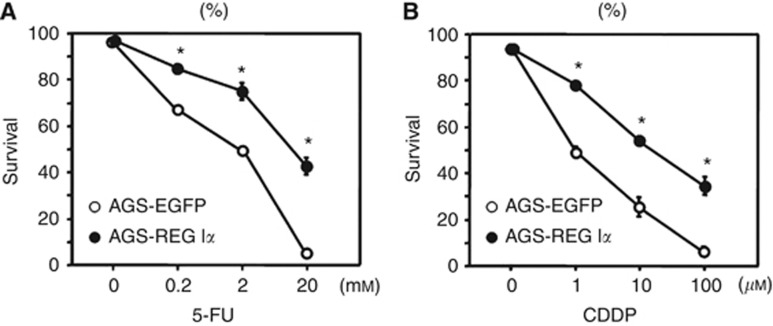
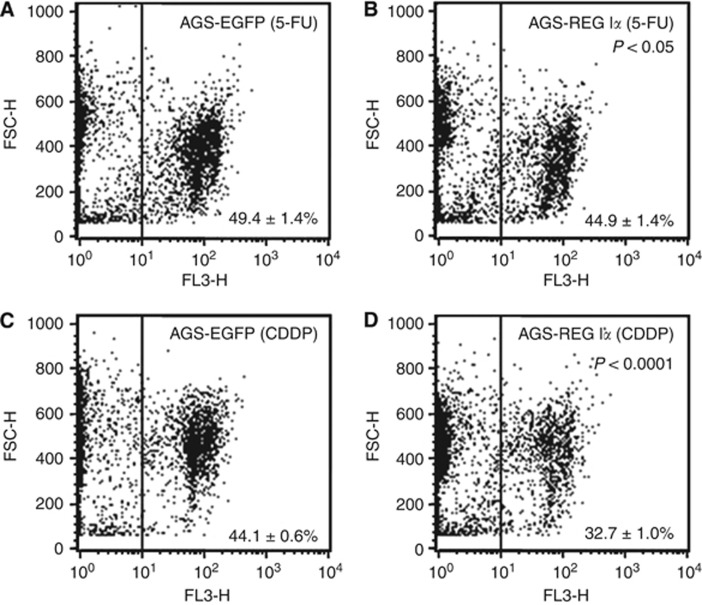
Effects of REG Iα gene induction on resistance to anticancer drugs in GC cells
We next examined the effect of REG Iα gene induction in GC cells treated with 5-FU or CDDP in terms of cell survival. The survival rate of gastric cancer cells decreased in a dose-dependent manner when they were treated with 5-FU or CDDP (Figure 3). Thus, the survival rate was significantly higher in the AGS-REG Iα group than in the AGS-EGFP group when cells were treated with 5-FU at concentrations of 0.2–20 mℳ (P<0.001, Figure 3A). Similarly, the survival rate was significantly higher in the AGS-REG Iα group when treated with CDDP at concentrations of 1–100 μℳ (P<0.001, Figure 3B). Conversely, FACS analyses revealed that the number of propidium iodide-positive cells was significantly smaller in the AGS-REG Iα group than in the AGS-EGFP group when cells were treated with 5-FU (P<0.05, Figure 4A and B) or CDDP (P<0.0001, Figure 4C and D), suggesting that induction of the REG Iα gene played a role in conferring resistance to anticancer drug-induced cell death.
Figure 3.
Effects of REG Iα gene induction on resistance to anticancer drugs in gastric cancer cells. Human gastric cancer AGS cells stably transfected with pIRES2-hREG Iα (AGS-REG Iα) or pIRES2-EGFP (AGS-EGFP; control) plasmid were treated with 5-FU (A, 0.2–20 mℳ) or CDDP (B, 1–100 μℳ) for 30 h. The percentage of viable cells was then evaluated, as described in Materials and Methods. All results are expressed as the means±s.e.m. of four samples. *P<0.001 vs AGS-EGFP at the same dose point.
Figure 4.
Effects of REG Iα gene induction on cell death induced by anticancer drugs in gastric cancer cells. The AGS-REG Iα or AGS-EGFP cells were treated with 5-FU (A and B, 20 mℳ) or CDDP (C and D, 100 μℳ) for 24 h. The cells were then stained using propidium iodide and analysed by flow cytometry to evaluate the percentage of dead cells, as described in Materials and Methods. All results are expressed as the means±s.e.m. of four samples.
Discussion
Recent studies have suggested that the tumour response to first-line chemotherapy is strongly correlated with PFS and/or OS in patients with unresectable GC (Ichikawa and Sasaki, 2006; Kodera et al, 2011). Supporting those data, the present study showed that not only PFS but also OS was significantly longer in responders to S-1/CDDP treatment than in nonresponders. Thus, the outcome in patients with unresectable GC is markedly dependent on the response to first-line chemotherapy. In this context, it is very important to identify biomarkers that can be used to predict the responses of such patients to first-line chemotherapy. Therefore, in the present study we investigated the expression of REG Iα in biopsy samples before chemotherapy and subsequently showed that REG Iα expression is a useful biomarker for predicting not only the response to S-1/CDDP treatment but also PFS and OS in patients with unresectable GC. Previously, we and others have suggested that REG Iα expression might be applicable as a marker for prediction of OS in GC patients; however, those studies included patients with various stages of GC receiving a variety of treatments (Dhar et al, 2004; Yamagishi et al, 2009). On the other hand, the patients investigated here were homogeneous in terms of both stage and the type of first-line chemotherapy. Although this investigation was designed as historical cohort study, it is tempting to conclude that REG Iα expression has potential promise as a biomarker for predicting the response to S-1/CDDP treatment and subsequent PFS and OS in patients with unresectable GC. Furthermore, it is noteworthy that REG Iα expression was examined in biopsy samples before chemotherapy. Numerous molecules have been reported as prognostic markers in GC patients, and supportive evidence has been obtained using mainly surgically resected samples. Although surgical specimens are more suitable than biopsy samples for examining the expression of target molecules, it would be clearly more desirable to examine the presence of predictive biomarkers in samples that can be easily obtained before treatment, such as biopsied tissues. In this context, as demonstrated in the present study, REG Iα may be a valuable biomarker for practical assessment of patients with unresectable GC. On the other hand, several studies have suggested that GC patients in high PS score (PS⩾2) show worse prognosis compared with ones in low PS score (PS<2) when they were treated with chemotherapy (Chau et al, 2004; Lee et al, 2007). In the present study, we divided the patients into PS0 and PS1–2 groups, because the number of PS2 patients was small (n=8). This may be rationale that we found no relation between prognosis and PS status.
During the follow-up periods, we had a chance to obtain biopsy samples from patients who showed resistance to S-1/CDDP treatment and apparent progression of their disease. Interestingly, we found that some REG Iα-negative patients became positive when the first-line chemotherapy failed, implying that GC may begin to express REG Iα during acquisition of resistance to chemotherapy. On the other hand, as GC lesions are not homogeneous in terms of REG Iα expression, we cannot exclude the possibility that initial biopsy samples had been accidentally obtained from REG Iα-negative parts of the lesions. However, like the REG IV gene, it is likely that repeated exposure to cytotoxic chemotherapeutic reagents had induced the expression of the antiapoptotic REG Iα gene (Violette et al, 2003). Although our preliminary data need to be reconfirmed in further experiments using a cell-biological approach, REG Iα appears to have potential utility as a marker for predicting susceptibility to chemotherapy in patients with unresectable GC.
How, then, does REG Iα confer resistance to chemotherapy in GC cells? Previous studies have indicated that activation of the antiapoptotic pathway, overexpression of multidrug transporter proteins, and activation of enzymes capable of metabolising chemotherapeutic drugs are involved in resistance of chemotherapy (Longley et al, 2003; Tsuruo et al, 2003; Matsubara et al, 2008; Zhang et al, 2011). We have previously shown that REG Iα exerts its antiapoptotic effect by activating Akt signalling and its downstream Bad phosphorylation and Bcl-xL expression (Sekikawa et al, 2005, 2008), suggesting that REG Iα confers resistance to chemotherapy by activating the antiapoptotic pathway in GC cells. In the present in vitro studies, we examined the effect of REG Iα gene induction on resistance to 5-FU and CDDP in GC cells. Subsequently, REG Iα-overexpressing GC cells showed significant resistance to those chemotherapeutic agents in comparison with control GC cells, although the difference between the two groups was not as great as we had expected. Conversely, this finding may be reasonable if REG Iα plays a role as only one of several antiapoptotic molecules, and does not activate multidrug transporter proteins or chemotherapeutic drug-metabolising enzymes. Clearly, however, further studies will be needed to clarify the mechanism by which REG Iα confers resistance to chemotherapy in GC cells.
In summary, we have shown that REG Iα is a potential marker for predicting not only resistance to S-1/CDDP treatment but also the outcome in patients with stage IV GC. Moreover, our in vitro studies have demonstrated that REG Iα gene induction confers resistance to the treatment with 5-FU or CDDP in GC cells. In the context of potential clinical application, these data suggest that REG Iα could be a target of anticancer therapy, and that its expression would be a useful marker for allocation of individualised chemotherapy.
Acknowledgments
This work was supported in part by grants-in-aid for Scientific Research 23590929 from the Ministry of Education, Culture, Sports, Science and Technology, Japan. We are grateful to Dr Hiroshi Okamoto from Tohoku University Graduate School of Medicine, Sendai, Japan, for providing the anti-REG Iα antibody.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Boku N. Chemotherapy for metastatic gastric cancer in Japan. Int J Oncol. 2008;13:483–487. doi: 10.1007/s10147-008-0847-2. [DOI] [PubMed] [Google Scholar]
- Chau I, Norman AR, Cunningham D, Waters JS, Oates J, Ross PJ. Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer-pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol. 2004;22:2395–2403. doi: 10.1200/JCO.2004.08.154. [DOI] [PubMed] [Google Scholar]
- Choi IS, Lee HS, Lee KW, Kim H, Kim KH, Kim YJ, Kim JH, Kim WH, Lee JS. Biomarker analysis in patients with advanced gastric cancer treated with S-1 plus cisplatin chemotherapy: orotate phosphoribosyltransferase expression is associated with treatment outcomes. Med Oncol. 2011;28:991–998. doi: 10.1007/s12032-010-9590-4. [DOI] [PubMed] [Google Scholar]
- Dhar DK, Udagawa J, Ishihara S, Otani H, Kinoshita Y, Takasawa S, Okamoto H, Kubota H, Fujii T, Tachibana M, Nagasue N. Expression of regenerating gene I in gastric cancer adenocarcinomas. Cancer. 2004;100:1130–1136. doi: 10.1002/cncr.20097. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Fukui H, Fujii S, Takeda J, Kayahara T, Sekikawa A, Nanakin A, Suzuki K, Hisatsune H, Seno H, Sawada M, Fujimori T, Chiba T. Expression of Reg Iα protein in human gastric cancers. Digestion. 2004;69:177–184. doi: 10.1159/000078762. [DOI] [PubMed] [Google Scholar]
- Fukui H, Kinoshita Y, Maekawa T, Okada A, Waki S, Hassan S, Okamoto H, Chiba T. Regenerating gene protein may mediate gastric mucosal proliferation induced by hypergastrinemia in rats. Gastroenterology. 1998;115:1483–1493. doi: 10.1016/s0016-5085(98)70027-7. [DOI] [PubMed] [Google Scholar]
- Ichikawa W, Sasaki Y. Correlation between tumor response to first-line chemotherapy and prognosis in advanced gastric cancer patients. Ann Oncol. 2006;17:1665–1672. doi: 10.1093/annonc/mdl174. [DOI] [PubMed] [Google Scholar]
- Japanese Gastric Cancer Association Japanese classification of gastric carcinoma, 2nd English edn. Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24:2137–2150. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- Kodera Y, Ito Y, Ohashi N, Nakayama G, Koike M, Fujiwara M, Nakao A. Impact of clinical response to first-line chemotherapy on gastric cancer patients treated with second-line and third-line chemotherapy. Hepatogastroenterology. 2011;58:1041–1045. [PubMed] [Google Scholar]
- Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Miyashita K, Nishizaki T, Kobayashi O, Takiyama W, Toh Y, Nagaie T, Takagi S, Yamamura Y, Yanaoka K, Orita H, Takeuchi M. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–221. doi: 10.1016/S1470-2045(08)70035-4. [DOI] [PubMed] [Google Scholar]
- Lee J, Lim T, Uhm JE, Park KW, Park SH, Lee SC, Park JO, Park YS, Lim HY, Sohn TS, Noh JH, Heo JS, Park CK, Kim S, Kang WK. Prognostic model to predict survival following first-line chemotherapy in patients with metastatic gastric adenocarcinoma. Ann Oncol. 2007;18:886–891. doi: 10.1093/annonc/mdl501. [DOI] [PubMed] [Google Scholar]
- Longley DB, Harkin DP, Johnston PG. 5-Fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3:330–338. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- Matsubara J, Nishina T, Yamada Y, Moriwaki T, Shimoda T, Kajiwara T, Nakajima TE, Kato K, Hamaguchi T, Shimada Y, Okayama Y, Oka T, Shirao K. Impacts of excision repair cross-complementing gene 1 (ERCC1), dihydropyrimidine dehydrogenase, and epidermal growth factor receptor on the outcomes of patients with advanced gastric cancer. Br J Cancer. 2008;98:832–839. doi: 10.1038/sj.bjc.6604211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsu A. Chemotherapy for metastatic gastric cancer: past, present, and future. J Gastroenterol. 2008;43:256–264. doi: 10.1007/s00535-008-2177-6. [DOI] [PubMed] [Google Scholar]
- Park SR, Kong SY, Nam BH, Choi IJ, Kim CG, Lee JY, Cho SJ, Kim YW, Ryu KW, Lee JH, Rhee J, Park YI, Kim NK. CYP2A6 and ERCC1 polymorphisms correlate with efficacy of S-1 plus cisplatin in metastatic gastric cancer patients. Br J Cancer. 2011;104:1126–1134. doi: 10.1038/bjc.2011.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satomura Y, Sawabu N, Ohta H, Watanabe H, Yamakawa O, Motoo Y, Okai T, Toya D, Makino H, Okamoto H. The immunohistochemical evaluation of PSP/reg-protein in normal and diseased human pancreatic tissues. Int J Pancreatol. 1993;13:59–67. doi: 10.1007/BF02795200. [DOI] [PubMed] [Google Scholar]
- Sekikawa A, Fukui H, Fujii S, Ichikawa K, Tomita S, Imura J, Chiba T, Fujimori T. REG Iα protein mediates an anti-apoptotic effect of STAT3 signaling in gastric cancer cells. Carcinogenesis. 2008;29:76–83. doi: 10.1093/carcin/bgm250. [DOI] [PubMed] [Google Scholar]
- Sekikawa A, Fukui H, Fujii S, Takeda J, Nanakin A, Hisatsune H, Seno H, Takasawa S, Okamoto H, Fujimori T, Chiba T. REG Iα protein may function as a trophic and/or anti-apoptotic factor in the development of gastric cancer. Gastroenterology. 2005;128:642–653. doi: 10.1053/j.gastro.2004.12.045. [DOI] [PubMed] [Google Scholar]
- Takaishi S, Wang TC. Gene expression profiling in a mouse model of Helicobacter-induced gastric cancer. Cancer Sci. 2007;98:284–293. doi: 10.1111/j.1349-7006.2007.00392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terazono K, Yamamoto H, Takasawa S, Shiga K, Yonemura Y, Tochino Y, Okamoto H. A novel gene activated in regenerating islets. J Biol Chem. 1988;263:2111–2114. [PubMed] [Google Scholar]
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- Tsuruo T, Naito M, Tomida A, Fujita N, Mashima T, Sakamoto H, Haga N. Molecular targeting therapy of cancer: drug resistance, apoptosis and survival signal. Cancer Sci. 2003;94:15–21. doi: 10.1111/j.1349-7006.2003.tb01345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Violette S, Festor E, Pandrea-Vasile I, Mitchell V, Adida C, Dussaulx E, Lacorte JM, Chambaz J, Lacasa M, Lesuffleur T. REG IV, a new member of the regenerating gene family, is overexpressed in colorectal carcinomas. Int J Cancer. 2003;103:185–193. doi: 10.1002/ijc.10788. [DOI] [PubMed] [Google Scholar]
- Watanabe T, Yonekura H, Terazono K, Yamamoto H, Okamoto H. Complete nucleotide sequence of human reg gene and its expression in normal and tumoral tissues. J Biol Chem. 1990;265:7432–7439. [PubMed] [Google Scholar]
- Yamagishi H, Fukui H, Sekikawa A, Kono T, Fujii S, Ichikawa K, Tomita S, Imura J, Hiraishi H, Chiba T, Fujimori T. Expression profile of REG family proteins REG Iα and REG IV in advanced gastric cancer: comparison with mucin phenotype and prognostic markers. Mod Pathol. 2009;22:906–913. doi: 10.1038/modpathol.2009.41. [DOI] [PubMed] [Google Scholar]
- Yonemura Y, Sakurai S, Yamamoto H, Endou Y, Kawamura T, Bandou E, Elnemr A, Sugiyama K, Sasaki T, Akiyama T, Takasawa S, Okamoto H. REG gene expression is associated with the infiltrating growth of gastric cancer. Cancer. 2003;98:1394–1400. doi: 10.1002/cncr.11658. [DOI] [PubMed] [Google Scholar]
- Zhang J, Roberts TM, Shivdasani RA. Targeting PI3K signaling as a therapeutic approach for colorectal cancer. Gastroenterology. 2011;141:50–61. doi: 10.1053/j.gastro.2011.05.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.