Abstract
Bipolar disorder is a severe mental illness characterized by recurrent manic and depressive episodes. In bipolar disorder, family and twin studies suggest contributions from genetic and environmental factors; however, the detailed molecular pathogenesis is yet unknown. Thus, identification of biomarkers may contribute to the clinical diagnosis of bipolar disorder. Monozygotic twins discordant for bipolar disorder are relatively rare but have been reported. Here we performed a comparative proteomic analysis of whole cell lysate derived from lymphoblastoid cells of monozygotic twins discordant for bipolar disorder by using two-dimensional differential in-gel electrophoresis (2D-DIGE). We found approximately 200 protein spots to be significantly differentially expressed between the patient and the co-twin (t test, p<0.05). Some of the proteins were subsequently identified by liquid chromatography tandem mass spectrometry and included proteins involved in cell death and glycolysis. To examine whether these proteins could serve as biomarkers of bipolar disorder, we performed Western blot analysis using case–control samples. Expression of phosphoglycerate mutase 1 (PGAM1), which is involved in glycolysis, was significantly up-regulated in patients with bipolar disorder (t test, p<0.05). Although PGAM1 cannot be regarded as a qualified biomarker of bipolar disorder from this preliminary finding, it could be one of the candidates for further study to identify biomarkers of bipolar disorder.
Introduction
Bipolar disorder is a severe mental illness characterized by recurrent manic and depressive episodes. It affects approximately 1% of the general population. In bipolar disorder, contributions of genetic and environmental factors have been indicated by family and twin studies [1]. Patients with this disease have a high relapse rate, and lifelong treatment with mood stabilizers such as lithium is often needed [2]. Past studies of bipolar disorder have focused on monoamines and intracellular signal transduction pathways as related to the effects of psychotropic drugs [3], [4], but recent studies focus more on neuroplasticity or resilience based on reports of neuroprotective effects of mood stabilizers [5]. Recent genome-wide association studies identified new candidate genes, such as CACNA1C [6], [7], but the effects are relatively small.
Bipolar disorder is often misdiagnosed as depression or schizophrenia, and delayed diagnosis and treatment worsen the course of illness [8]. Thus, early diagnosis is important to prevent deterioration; however, no biomarkers for bipolar disorder are available yet. Identification of biomarkers would be indispensable for early diagnosis.
Much research on biomarkers in psychiatric diseases has been published [9], [10]. Though several candidate biomarkers were identified from postmortem brains, these studies are undermined by many confounding factors, including cause of death, postmortem interval, and brain pH [11]. Postmortem interval affects degradation of mRNAs and protein levels [12], [13], [14], [15] and significantly influences phosphorylation of signaling proteins [16]. In particular, the influence of medication cannot be ignored because a number of proteins are affected by mood stabilizers, antipsychotics, or antidepressant medication [17], [18], [19]. Additionally, large interindividual variations hamper the identification of biomarkers.
Biomarker research in other tissues such as serum, plasma, cerebrospinal fluids, saliva, and urine have also been performed [20], [21] but has not led to a diagnostic test.
The concordance rate of bipolar disorder between monozygotic twins is approximately 70% [22], [23]. By comparing monozygotic twins discordant for bipolar disorder, biochemical differences associated with bipolar disorder might be detected without interference from interindividual genetic variation [24].
Although several genome, transcriptome, and epigenome analyses in monozygotic twins discordant for bipolar disorder and other diseases have been reported [24]–[29], proteomic analysis has not been applied to identifying the difference between monozygotic twins discordant for bipolar disorder, possibly due to technical difficulties. Because transcript levels do not completely correlate with protein expression levels [30], [31] and aberrant post-translational modifications can cause disease, proteomic analysis is needed to supplement transcriptome and epigenome analyses.
In the present study, we performed proteomic analysis of lymphoblastoid cells derived from monozygotic twins discordant for bipolar disorder.
Materials and Methods
Subjects
For 2D-DIGE, we used lymphoblastoid cells derived from a pair of 42-year-old male monozygotic twins discordant for bipolar disorder. We initially examined their monozygosity by genotyping microsatellite repeat markers [25] and later confirmed it by single nucleotide polymorphism array [29].
For a case–control study of differentially expressed proteins using Western blot analyses, we used lymphoblastoid cells derived from eight unrelated patients with bipolar I disorder (BPI) (four men and four women, 35.6±9.0 years old [mean ± SD], Japanese) and eight unrelated control subjects (six men and two women, 36.9±10.0 years old [mean ± SD], Japanese). Table 1 gives detailed information for each subject used in Western blot analysis. Patients and controls with a history of alcohol or illicit drug abuse were excluded from the study. The patients were treated with various medications. Diagnoses were made by the consensus of two senior psychiatrists using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria. Controls were selected from among students, nurses, office workers, and doctors in participating institutes, their friends, and other volunteers. A senior psychiatrist interviewed control subjects and found that they did not have major mental disorders. Written informed consent was obtained from all subjects. The ethics committees of RIKEN approved the study.
Table 1. Characteristics of the subjects.
| ID | Age | Sex | Diagnosis | Age at onset | Family history of bipolar disorder within first degree relatives | Medication |
| B1 | 40 | F | Bipolar I disorder with psychotic features | 24 | Yes | Li, VPA, CBZ, HP, CP |
| B2 | 23 | F | Bipolar I disorder | 23 | No | Li, VPA, PAR |
| B3 | 46 | F | Bipolar I disorder | 27 | Yes | VPA, THY |
| B4 | 26 | M | Bipolar I disorder, rapid cycling | 24 | Yes | Li |
| B5 | 38 | M | Bipolar I disorder | 35 | No | VPA, OLA |
| B6 | 40 | M | Bipolar I disorder | 25 | No (three had major depression) | Li, VPA |
| B7 | 27 | F | Bipolar I disorder with psychotic features | 24 | No | Li, VPA |
| B8 | 45 | M | Bipolar I disorder | 20 | No | Li |
| C1 | 36 | M | - | No | - | |
| C2 | 29 | M | - | No | - | |
| C3 | 34 | M | - | No | - | |
| C4 | 29 | M | - | No | - | |
| C5 | 27 | F | - | No | - | |
| C6 | 52 | M | - | No | - | |
| C7 | 52 | M | - | No | - | |
| C8 | 33 | F | - | No | - |
Li: lithium carbonate, VPA, sodium valproate, CBZ, carbamazepine, HP, haloperidol, CP, chlorpromazine, PAR, paroxetine, THY, levothyroxine, OLA, olanzapine.
Cell culture and extraction of proteins
Lymphocytes were separated from the peripheral blood and transformed by Epstein-Barr virus using previously described standard techniques [32]. These cells were cultured and kept frozen until experiments. Lymphoblastoid cells were cultured in RPMI 1640 medium (Sigma-Aldrich, St. Louis, MO, USA) containing 10% fetal bovine serum (Sigma-Aldrich), 50 U/mL penicillin, 50 μg/mL streptomycin (GIBCO, Invitrogen/Life Technologies Corporation, Grand Island, NY), and 60 μg/mL tylosin solution (Sigma-Aldrich). Cells were cultured at approximately 1×108 cells. Total proteins were extracted from the lymphoblastoid cells using the Q-proteome mammalian protein preparation kit (Qiagen, QIAGEN, Hilden, Germany). After the supernatant was precipitated with acetone, the pellet was dissolved using the lysis buffer (7 M urea, 2 M thiourea, 4% CHAPS, 10 mM Tris-HCl [pH 8.5]) (GE Healthcare Bio-Sciences, San Francisco, CA, USA).
Two-dimensional difference gel electrophoresis (2D-DIGE) and imaging analyses
Protein concentration was determined by the Bradford method using a protein assay kit (Bio-Rad, Hercules, CA, USA) and the Pierce 660 nm protein assay (Pierce, Rockford, IL, USA). Proteins were set to a final concentration of 5 mg/mL with the lysis buffer and labeled separately with 400 pmol of CyDye (Cy3 or Cy5) (GE Healthcare Bio-Sciences), vortexed, and incubated on ice in the dark for 30 min. A mixed sample composed of equal amount of proteins from the patient and the co-twin was labeled with Cy2 and used as an internal standard. After 30 min, the labeling reaction was stopped with 10 mM lysine. To avoid the possible effect of labeling efficiency, the dyes were swapped for each experiment using three gels. Labeled proteins were subjected to SDS-PAGE analysis, and the gels were scanned with the Typhoon 9400 scanner (GE Healthcare Bio-Sciences) at the wavelengths corresponding to each CyDye, namely 480 nm (Cy2), 532 nm (Cy3), and 633 nm (Cy5). A 50 μg portion of each Cy3-, Cy5-, and Cy2-labeled sample was combined. Nonlinear IPG strips (pH 3–10, 18 cm long; GE Healthcare Bio-Sciences) were rehydrated for 12 h at 50 mA per strip with the sample solution on an IPGphor isoelectric focusing unit (GE Healthcare Bio-Sciences). Three mixed samples were separated by isoelectric focusing on an IPGphor isoelectric focusing unit at 0.5 V⋅h, 0.8 V⋅h, 13.5 kV⋅h, and 21 kV⋅h at 20°C and a maximum current setting of 50 μA per strip. The second dimension was run on 12.5% acrylamide gels in a SE600 (GE Healthcare Bio-Sciences) at 45 mA per gel. To avoid artifacts, three gels of same condition were simultaneously run for each experiment. Gels were scanned directly between low-fluorescence glass plates with the Typhoon 9400 (GE Healthcare Bio-Sciences) scanner at the three wavelengths specific for the CyDyes. The resolution was approximately 100 μm. Determination of protein spot abundance was performed using the DeCyder 2D Ver. 6.0 software (GE Healthcare Bio-Sciences). Spots were automatically detected. Spot editing (separation of two spots) or deleting (artifacts) was performed manually. The three CyDye–labeled forms of each spot were co-detected within each gel. Ratios between sample and internal standard abundances were calculated for each protein spot with the Differential In-gel Analysis (DIA) module. Inter-gel variability was corrected by matching and normalization of the internal standard spot maps by the Biological Variance Analysis (BVA) module of the DeCyder software and incorrectly matched spots were manually eliminated or corrected if possible. During the spot detection, the estimated number of spots was set at 4000. Protein spots that showed a statistically significant intensity in Student's t test were accepted as being differentially expressed between the extracts under comparison among these. Protein spots showing at least 1.25-fold changes (p<0.05) in intensity were selected for next steps.
Protein identification by mass spectrometry and database search
The preparative gels were stained with a SYPRO® ruby (Invitrogen/Life Technologies Corporation) and scanned with the Typhoon 9400. Protein spots that showed differences in relative fluorescence were excised from the gel using the automated spot picker (GE Healthcare Bio-Sciences). The picked gel pieces were destained with 50% CH3CN in a 50 mM NH4HCO3 solution. After removal of the supernatant, cysteine residues were reduced with dithiothreitol and carbamidomethylated with iodoacetamide. In-gel trypsin digestion was performed at 37°C overnight, using sequencing grade modified trypsin (Promega, Southampton, UK) reconstituted in 100 mM NH4HCO3. The trypsinized gel was rinsed three times in extraction buffer (5% trifluoroacetic acid in 50% CH3CN and 50% H2O). The trypsinized peptides solution was dried by speed vacuum, suspended in 2% CH3CN with 0.1% trifluoroacetic acid, and analyzed by LTQ (Fisher Scientific, Waltham, MA) liquid chromatography/linear ion trap mass spectrometry (LC-MS/MS) system. Their corresponding proteins were searched using the program Mascot database-searching software (Matrix Science, London, UK), which accesses protein identification by matching mass spectroscopy data with the protein databases NCBI (http://www.ncbi.nlm.nih.gov) and UniProt (http://www.uniprot.org/uniprot). Identification criteria included a Mascot score >45 (selected based on a corrected p-value <0.05).
Functional grouping of altered proteins
The IPA software (Ingenuity Systems, Redwood City, CA) was used to identify the key biological relationships and functions of differentially expressed proteins and their interaction networks. For pathway analysis, Swiss-Prot and GenBank accession numbers were used to catalogue the identified protein into known interaction pathways based upon the Ingenuity Pathway Knowledge Base (IPKB). IPA classification data were derived from the published literature in a systematic way using a comprehensive ontology of functional annotations and protein–protein interaction data. The most significant interaction networks, biological functions and pathway associated with the differentially expressed proteins were identified. To confirm biological functions and gene ontology annotation between identified proteins, we used bioinformatics resources, PANTHER (http://www.pantherdb.org/) and DAVID (http://david.abcc.ncifcrf.gov/). DAVID program uses a modified Fisher's exact p value (EASE score) to rank gene clusters by statistical overrepresentation of individual genes, based on the co-occurrence/enrichment of the category within the gene list relative to all genes in the same category on the study.
Western blot analyses for validation
Lymphoblastoid cells in a case–control study were individually cultured. Total proteins were individually extracted using Q-proteome Mammalian Protein prep kit (Qiagen), and protein concentrations were determined by the methods mentioned above. Equal concentration (5 μg per lane) of proteins from control and case samples were separated by 12% or 4–15% SDS-polyacrylamide gel electrophoresis and transferred onto Immun-Blot PVDF membranes (Bio-Rad) using a mini Trans-blot Cell (Bio-Rad). After transfer, the blotted membrane were blocked with 4% w/v ECL Advance Blocking Reagent (GE Healthcare Bio-Sciences) in phosphate-buffered saline containing 0.1% Tween20 (PBST) (MP Biomedicals Inc., Santa Ana, CA) at 4°C overnight and incubated with primary antibody in PBST with 4% w/v skim milk for 1 h at room temperature. PSME1, WARS, and PGAM1 were chosen for quantification by Western blot analysis. As an internal control, NM23A was used because there was no significant difference of protein levels of NM23A between patient and the co-twin in 2D-DIGE. Primary antibodies were as follows: rabbit antibody against human PSME1 (Calbiochem, La Jolla, CA), mouse antibody against human WARS (Abnova, Taipei City, Taiwan), goat antibody against human PGAM1 (Novus Biologicals, Littleton, CO), and rabbit monoclonal and polyclonal against human NM23A (Abcam, Cambridge, MA). The blotted membranes were washed in TBST and incubated at room temperature with each secondary antibodies, Alexa Fluor 488–labeled donkey anti-goat IgG antibody (Molecular Probes/Life Technologies Corporation), Cy5-conjugated affiniPure donkey anti rabbit IgG antibody and Cy3-conjugated affiniPure donkey anti mouse IgG antibody (Jackson Immuno Research, West Grove, PA). The membranes were directly scanned with the Molecular Imager FX (Bio-Rad). Protein bands were analyzed to give a quantitative estimation of intensity change using the Quantity One Software (Bio-Rad) adapted to the Molecular Imager FX. To estimate the relative molecular weight of each protein, molecular markers, Dual Color Precision Plus Protein Standards (Bio-Rad) and ECL Plex Fluorescent Rainbow Markers (GE Healthcare Bio-Sciences) were used. Preliminary experiments indicated that amounts of these proteins in the lysates of lymphoblastoid cells were within the linear range of detection.
Results
Detection of spots differentially expressed between monozygotic twins discordant for bipolar disorder by 2D-DIGE
First, we extracted total protein from cultured lymphoblastoid cells derived from a pair of monozygotic twins discordant for bipolar disorder. The total protein for each twin was separately labeled with different CyDyes (Cy3 or Cy5), and dyes were swapped between gels. A mixed sample composed of an equal amount of proteins from the patient and the co-twin was labeled with Cy2 and used as an internal standard. These processes minimized gel-to-gel variation and improved protein spot statistics at the analysis stage. These labeled proteins were mixed and analyzed by 2D-DIGE. To detect robust differences between the patient and the co-twin, we performed 2D-DIGE. To avoid artifacts, four gels of same condition were simultaneously run for each experiment. Three gels were used as analytical gels to detect differentially expressed spots between the patient and the co-twin, and the remaining gel was used as preparative gel for picking out differentially expressed spots. We performed 2D-DIGE and liquid chromatography tandem mass spectrometry (LC-MS/MS) analyses in quadruplicate experiments using protein samples independently extracted from different aliquots of cell culture.
Using 2D-DIGE and DeCyder Ver.6.0 image analysis software, approximately 3200 protein spots were separated (3220±51 [mean ± SD]). The observed spot pattern images in each gel were very similar among quadruplicate experiments. The protein spots were selected if the intensity difference between the affected and nonaffected twin was larger than 1.25-fold (absolute value >1.25 or absolute value <−1.25). Approximately 200 spots (211±115, quadruplicate) were found to be significantly differentially expressed (p<0.05, Student's t test) between the twins per experiment.
Identification of spots by LC-MS/MS
The proteins in preparative gels were stained by SYPRO Ruby after electrophoresis, and the preparative gels were performed matching to analytical gels. The largest 100 spots out of the 200 differentially expressed protein spots were picked from each preparative gel and were considered suitable for subsequent analysis by LC-MS/MS. The spots were chosen sequentially from those with a large absolute value fold change. The 68 spots, averaged for quadruplicate values, were successfully identified as unique proteins through LC-MS/MS and are listed in Table 2. Since Epstein-Barr virus–transformed lymphoblastoid cells were used in this study, all immunoglobulin and B-cell–related proteins were removed from the analysis. Moreover, we also removed keratin and trypsin-related proteins because of the possibility of experimental contamination. Table 2 shows only proteins identified by LC-MS/MS in common with each experiment. Proteins identified twice or more with Mascot search results (ion scores of higher than 45) included PSME1, RPLP0, TPI1, ALDOC, ANXA4, PGAM1, and WARS. Fifty-three proteins had high ion scores and were identified at least twice in four experiments.
Table 2. Proteins differentially expressed in monozygotic twin discordant for BP identifed by LC-MS/MS.
| Exp.1 | Exp.2 | Exp.3 | Exp.4 | |||||||
| Fold change | Fold change | Fold change | Fold change | |||||||
| Gene names | Acc. No. | Protein names | (BP/CT) | p – value | (BP/CT) | p – value | (BP/CT) | p – value | (BP/CT) | p – value |
| PSME1 | Q06323 | Proteasome activator complex subunit 1 | −1.42 | 0.00013 | −1.44 | 0.00018 | −1.3 | 0.0079 | −1.91 | 0.0056 |
| RPLP0 | P05388 | 60S acidic ribosomal protein P0 | −1.34 | 0.00031 | −1.39 | 0.03 | −1.45 | 0.0053 | −1.31 | 0.0059 |
| TPI1 | P00939 | Triosephosphate isomerase | 1.95 | 0.034 | 3.17 | 7.10E-05 | 1.68 | 0.015 | 1.3 | 0.015 |
| ALDOC | P09972 | Fructose-bisphosphate aldolase C | −1.47 | 0.0024 | −1.35 | 0.0013 | −1.26 | 0.0059 | ||
| ANXA4 | P09525 | Annexin A4 | −1.96 | 0.00022 | −1.62 | 0.00011 | −1.35 | 0.00029 | ||
| PGAM1 | P18669 | Phosphoglycerate mutase 1 | 1.9 | 0.0023 | 1.59 | 0.0001 | 2.12 | 0.0035 | ||
| WARS | P23381 | Tryptophanyl-tRNA synthetase, cytoplasmic | 1.6 | 0.00037 | 1.55 | 0.00023 | 1.28 | 0.00062 | ||
| ACADS | P16219 | Short-chain specific acyl-CoA dehydrogenase, mitochondrial | −1.56 | 0.00014 | −1.37 | 0.0006 | ||||
| ALDH2 | P05091 | Aldehyde dehydrogenase, mitochondrial | −1.26 | 0.018 | −1.29 | 0.01 | ||||
| ALDOA | P04075 | Fructose-bisphosphate aldolase A | 1.48 | 0.0023 | 1.29 | 0.0055 | ||||
| ANXA5 | P08758 | Annexin A5 | −1.25 | 0.0046 | −1.29 | 0.007 | ||||
| APOA1BP | Q8NCW5 | Apolipoprotein A-I-binding protein | 2.56 | 1.90E-06 | 2.16 | 0.00023 | ||||
| ATP5A1 | P25705 | ATP synthase subunit alpha, mitochondrial | −1.61 | 0.00048 | −1.33 | 6.70E-06 | ||||
| C19orf10 | Q969H8 | UPF0556 protein C19orf10 | 1.66 | 0.001 | 2.16 | 0.0012 | ||||
| CACYBP | Q9HB71 | Calcyclin-binding protein | −1.99 | 0.00075 | −11.74 | 0.00023 | ||||
| CAPZB | P47756 | F-actin-capping protein subunit beta | −1.56 | 0.00021 | −1.36 | 7.10E-06 | ||||
| CASP3 | P42574 | Caspase-3 | 1.49 | 0.00011 | 1.44 | 0.0054 | ||||
| CMPK1 | P30085 | UMP-CMP kinase | 2.9 | 1.40E-05 | 3.22 | 0.00029 | ||||
| CORO1A | P31146 | Coronin-1A | 1.31 | 0.0013 | 1.36 | 0.0029 | ||||
| DNAJB11 | Q9UBS4 | DnaJ homolog subfamily B member 11 | 1.37 | 0.00032 | 1.41 | 0.0052 | ||||
| ECH1 | Q13011 | Delta(3,5)-Delta(2,4)-dienoyl-CoA isomerase, mitochondrial | 1.91 | 0.0014 | 1.74 | 0.00016 | ||||
| ENO1 | P06733 | Alpha-enolase | −1.62 | 0.049 | −1.58 | 0.012 | ||||
| ETFB | P38117 | Electron transfer flavoprotein subunit beta | 1.27 | 0.019 | 1.36 | 0.00099 | ||||
| GALE | Q14376 | UDP-glucose 4-epimerase | −1.35 | 0.0051 | −1.33 | 0.044 | ||||
| GAPDH | P04406 | Glyceraldehyde-3-phosphate dehydrogenase | −1.38 | 0.0038 | −1.33 | 0.044 | ||||
| HIST2H4B | P62805 | Histone H4 | 2.07 | 0.0038 | 1.95 | 0.0014 | ||||
| HNRNPM | P52272 | Heterogeneous nuclear ribonucleoprotein M | 1.46 | 0.0033 | 1.4 | 0.0023 | ||||
| HSPA5 | P11021 | 78 kDa glucose-regulated protein | 3.18 | 0.00012 | 3.02 | 5.50E-06 | ||||
| HSPB1 | P04792 | Heat shock protein beta-1 | 1.58 | 0.0001 | 1.46 | 0.0071 | ||||
| LDHA | P00338 | L-lactate dehydrogenase A chain | 1.26 | 0.035 | 5.6 | 0.0042 | ||||
| LGALS3 | P17931 | Galectin-3 | −1.78 | 0.00033 | −1.99 | 0.00075 | ||||
| NANS | Q9NR45 | Sialic acid synthase | 1.46 | 0.0012 | 1.62 | 1.60E-05 | ||||
| NDUFS3 | O75489 | NADH dehydrogenase [ubiquinone] iron-sulfur protein 3, mitochondrial | 1.58 | 0.0001 | 1.46 | 0.0071 | ||||
| NPM1 | P06748 | Nucleophosmin | −1.53 | 0.00074 | −1.42 | 0.0042 | ||||
| OTUB1 | Q96FW1 | Ubiquitin thioesterase OTUB1 | 1.52 | 6.00E-05 | 1.47 | 0.0043 | ||||
| P4HB | P07237 | Protein disulfide-isomerase | 1.47 | 0.00017 | 1.69 | 0.0029 | ||||
| PACAP | Q8WU39 | Plasma cell-induced resident endoplasmic reticulum protein | 2 | 0.011 | 2.01 | 0.0077 | ||||
| PCBP1 | Q15365 | Poly(rC)-binding protein 1 | −1.47 | 0.0024 | −1.35 | 0.0013 | ||||
| PDIA3 | P30101 | Protein disulfide-isomerase A3 | 1.98 | 8.60E-06 | 2.09 | 0.0017 | ||||
| PDIA6 | Q15084 | Protein disulfide-isomerase A6 | 1.58 | 0.00042 | 1.75 | 1.20E-05 | ||||
| PHGDH | O43175 | D-3-phosphoglycerate dehydrogenase | 2.05 | 0.003 | 3.13 | 0.0001 | ||||
| PITHD1 | Q9GZP4 | PITH domain-containing protein 1 | 2.15 | 0.012 | 2.13 | 0.011 | ||||
| PKM2 | P14618 | Pyruvate kinase isozymes M1/M2 | 1.36 | 0.0029 | 1.36 | 0.045 | ||||
| PNPO | Q9NVS9 | Pyridoxine-5′-phosphate oxidase | −1.74 | 0.0085 | −1.41 | 0.001 | ||||
| POLR2E | P19388 | DNA-directed RNA polymerases I, II, and III subunit RPABC1 | 1.65 | 0.00025 | 2.12 | 0.00013 | ||||
| PRDX2 | P32119 | Peroxiredoxin-2 | 2.9 | 1.40E-05 | 3.22 | 0.00029 | ||||
| PSMB1 | P20618 | Proteasome subunit beta type-1 | −1.77 | 0.0093 | −1.29 | 0.00032 | ||||
| SARS | P49591 | Seryl-tRNA synthetase, cytoplasmic | 1.31 | 0.0013 | 1.36 | 0.0029 | ||||
| SERPINB1 | P30740 | Leukocyte elastase inhibitor | 1.37 | 0.00032 | 1.41 | 0.0052 | ||||
| SSR4 | P51571 | Translocon-associated protein subunit delta | 1.67 | 0.0059 | 1.77 | 0.00018 | ||||
| STMN1 | P16949 | Stathmin | −2.02 | 6.90E-05 | −1.53 | 3.70E-05 | ||||
| UCHL1 | P09936 | Ubiquitin carboxyl-terminal hydrolase isozyme L1 | 2.5 | 1.90E-05 | 2.16 | 0.00023 | ||||
| VDAC1 | P21796 | Voltage-dependent anion-selective channel protein 1 | 1.43 | 0.0013 | 2.29 | 0.00023 | ||||
Functional grouping of altered proteins
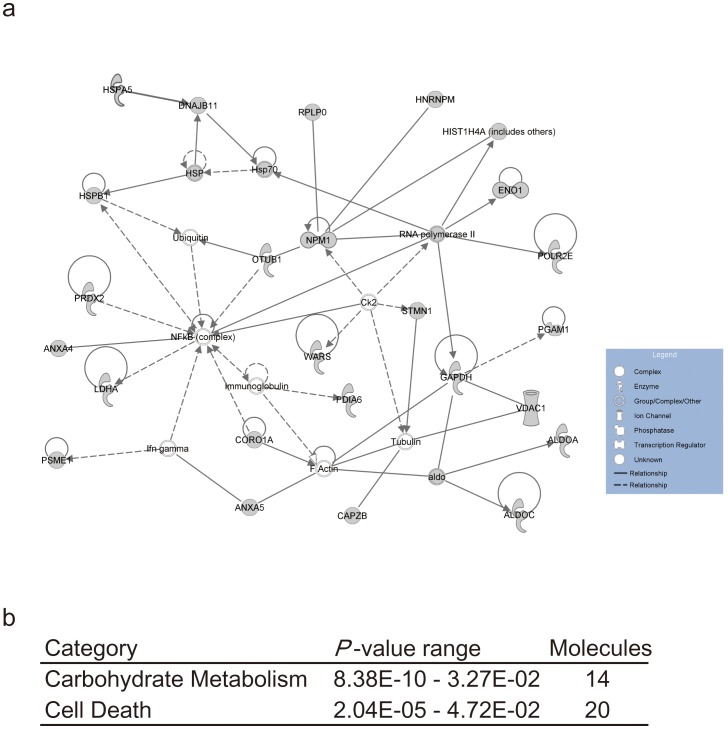
To explore the biological function (protein-interaction network) of the 53 differentially expressed proteins, we performed protein classification using the Ingenuity Pathway Knowledge Base software. A data set containing the gene symbols by The HUGO Gene Nomenclature Committee was uploaded into the application. Each protein identifier was converted to its gene identification and mapped to its corresponding gene object in the Ingenuity Pathway Knowledge Base. These genes were overlaid onto a global molecular network developed from information contained in the Ingenuity pathways analysis (IPA) knowledge base, which is based entirely on findings reported in the literature. Networks of these focus genes were algorithmically generated based on their connectivity. One of the 53 proteins was omitted because it was not included in the database, and the remaining 52 proteins were mapped onto mainly three networks. The largest network, having the highest score, is associated with carbohydrate metabolism, neurological disease, and skeletal and muscular disorders (Fig. 1A). This network includes ALDOA, ALDOC, ANXA4, ANXA5, CAPZB, CORO1A, DNAJB11, ENO1, GAPDH, HIST1H4A (includes others), HNRNPM, HSPB1, LDHA, NPM1, OTUB1, PDIA6, PGAM1, POLR2E, PRDX2, PSME1, RNA polymerase II, RPLP0, STMN1, VDAC1, and WARS. Next, the 53 proteins were classified according to biological function and canonical pathway. The categories pertained to carbohydrate metabolism (8.38E-10–3.27E-02, 14 molecules) and cell death (2.04E-05–4.72E-02, 20 molecules) (Fig. 1B). Pathway analysis and gene ontology classification using PANTHER and DAVID were conducted on the same protein IDs. These analyses also showed pathways and categories associated with glycolysis and anti-apoptosis. Taken together, most proteins identified in the present study were related to glycolysis and neurological diseases.
Figure 1. Gene networks showing interrelationships between differentially expressed genes in the twin with bipolar disorder.
Case–control study by Western blot analysis
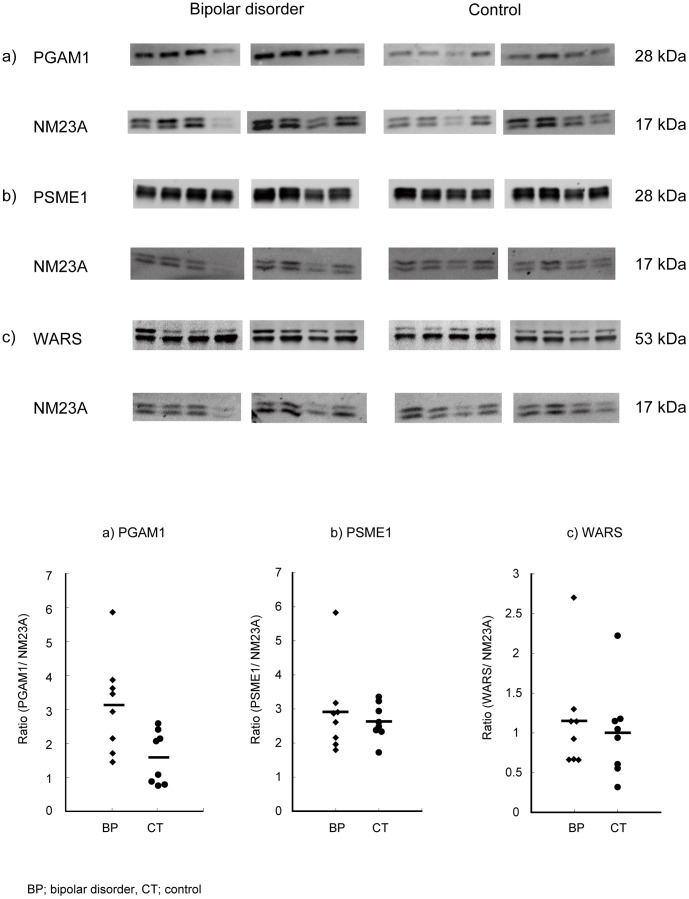
We postulated that the differentially expressed proteins might be candidate biomarkers for bipolar disorder. To validate the findings from the proteomic profiling study and to examine the possibility of biomarkers for bipolar disorder, Western blot analyses were performed using a case–control sample set consisting of eight subjects with bipolar disorder and eight healthy control subjects. To compare the protein levels across individuals, protein concentration was measured by the Bradford method, and equal amounts of proteins were loaded onto the gels. Commercially available antibodies for the candidate 7 proteins (PSME1, RPLP0, TPI1, ALDOC, ANXA4, PGAM1, and WARS) were searched for, and among available antibodies, those against PSME1, WARS, and PGAM1 showed good performance, and thus they were chosen for quantification by Western blot analysis. The levels of PGAM1, PSME1, and WARS were quantitatively investigated by Western blot analysis using NM23A as a standard (Fig. 2). Expression of PGAM1 was recognized by the presence of a single band at around 28 kDa and its protein expression was increased by 197% in bipolar disorder compared with controls (p<0.05). However, the levels of the other proteins were similar between bipolar disorder and controls in this case–control sample set (Fig. 2).
Figure 2. Protein expression validation by Western blot analysis with an internal standard, NM23A.
Proteins from each of the eight pairs of samples were separated by SDS-PAGE and transferred to PVDF membranes. Proteins were immunodetected using the respective primary antibodies and fluorescent secondary antibodies. Signals were captured with FX and signal intensity and shown by the. a) PGAM1, b) PSME1, c) WARS. Scatter plots show the ratio of each protein to an internal standard protein, NM23A, measured by densitometric scanning of the band intensities. The p values were calculated using a t test in all proteins. Number of the subjects is 8 for bipolar disorder and 8 for controls, respectively. The absolute band intensity for the PGAM1 was also significantly higher in patients with bipolar disorder (0.93+/−0.23 [mean +/− standard deviation] [arbitrary unit]) than control subjects (0.39+/−0.18, p<0.0005).
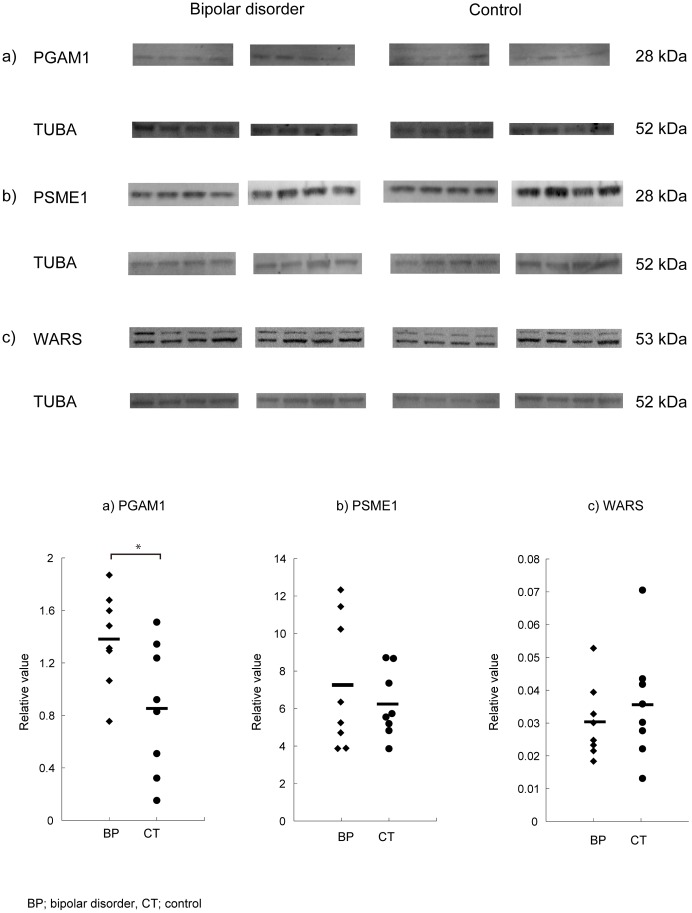
The absolute band intensity for the PGAM1 was also significantly higher in patients with bipolar disorder (0.93±0.23 [mean ± standard deviation] [arbitrary unit]) than control subjects (0.39±0.18, p<0.0005). In addition, we also performed an independent experiment using the other, more popular house-keeping protein, tubulin alpha (TUBA), as an internal standard. This analysis also showed higher PGAM1 levels in patients with bipolar disorder than controls (p<0.05) (Figure 3).
Figure 3. Verification of the alternation of PGAM1 using the other internal protein, tubulin alpha (TUBA).
The methods are similar to the Figure 2, except that tubulin alpha (TUBA) was used for the internal standard. a) PGAM1, b) PSME1, c) WARS. Scatter plots show the ratio of each protein to an internal standard protein, TUBA, measured by densitometric scanning of the band intensities. The PGAM1/TUBA ratio was significantly higher in patients with bipolar disorder compared with controls (p<0.05). Number of the subjects is 8 for bipolar disorder and 8 for controls, respectively.
Discussion
In this study, we identified 53 proteins that were differentially expressed between a pair of monozygotic twins discordant for bipolar disorder; 34 were up-regulated and 19 were down-regulated. The differentially expressed proteins included those previously implicated in psychiatric disorders, such as ALDOC, ENO1, and PRDX2 [10], [33]. Differences for ALDOC, ANXA4, PGAM1, PSME1, RPLP0, TPI1, and WARS between twins were regarded as robust because they were identified in three of four experiments with high scores.
To evaluate whether identified proteins might be biomarkers for bipolar disorder, we performed a case–control study for several proteins by Western blot analysis using available antibodies. An increased level of PGAM1 was observed in samples from patients with bipolar disorder. PGAM1 is an enzyme of the glycolytic pathway that catalyzes the conversion of 3-phosphoglycerate to 2-phosphoglycerate [34]. This enzyme also promotes glycolysis and ATP production via the TCA cycle and the electron transport system. Although previous studies using postmortem brains of patients with bipolar disorder and schizophrenia suggested altered protein expression of glycolysis enzymes, including PGAM1 [10], [35], the results were controversial. The differentially expressed proteins between bipolar disorder and healthy control including PGAM1, might be a clue to understand the biological basis of bipolar disorder.
To examine whether the 53 identified proteins were related to each other and constituted a global molecular network, pathway, or category, we applied IPA to our data. The results showed that the networks having a high score belonged to cell death, energy production, and glucose metabolism categories. The cell death category included the following proteins: NPM1, P4HB, LGALS3, CASP3, PDIA3, ATP5A1, GAPDH, ANXA4, HSPA5, RPLP0, UCHL1, STMN1, ENO1, ANXA5, MZB1, PSMB1, ALDOA, VDAC1, LDHA, HSPB1, and PRDX2 (Fig. 1). These results are consistent with previous studies. Benes et al. [36] showed increased expression of pro-apoptotic gene transcripts in postmortem brains of bipolar disorder patients. Furthermore, Herbeth et al. [21] indicated altered cell death and inflammation-related proteins in peripheral blood mononuclear cells and serum from patients with euthymic bipolar disorder. Brain imaging studies demonstrated reductions in the mean gray matter volume of brains from patients with bipolar disorder [37]. Previous studies reported a decreased density of nonpyramidal neurons in layer II of the anterior cingulate and a lower number of glial cells in layer III with bipolar disorder [38]. Meta-analyses of volumetric magnetic resonance imaging studies showed reduced volume of gray matter in the anterior cingulate and bilateral insula [39], [40]. Neuropathological studies of bipolar disorder showed decreases of each brain field and neuronal cells. Because mood stabilizers and antidepressants, which are used for treatment of bipolar disorder, have neuroprotective actions [5], [41], [42], it has been suggested that cells derived from patients with bipolar disorder are more vulnerable to factors related to cell death than those from controls. Patients with unipolar or bipolar depression exhibit decreased brain-derived neurotrophic factor levels [43]. Moreover, mood stabilizers have neuroprotective effects by increasing bcl-2 levels [42], [44], [45]. These findings suggest cellular vulnerability has a role in the pathology of bipolar disorder. Dysregulation of the apoptotic process found in the monozygotic twins discordant for bipolar disorder might be relevant to this hypothesis.
We examined the relationship of the identified proteins with canonical pathways and found that the proteins were related to the glycolysis pathway. The proteins included PKM2, ALDH2, ENO1, PGAM1, GAPDH, ALDOA, LDHA, and ALDOC. Glycolysis, or anaerobic respiration, is a fundamental metabolic process that produces energy for all cells. In order to maintain its functions, the brain needs an enormous amount of energy compared with other tissues. ALDOC is a brain-specific glycolysis enzyme that catalyzes the reversible aldol cleavage of fructose-1,6-biphosphate and fructose-1-phosphate to dihydroxyacetone phosphate and either glyceraldehyde-3-phosphate or glyceraldehyde [46]. In the present study, we found a decrease of the ALDOC protein level in the affected twin. However, previous reports showed that protein expression level of ALDOC was increased in the frontal cortex of patients, including those with mood disorder [35], [47]. This discrepancy might reflect differences between tissues. Moreover, we found differential expression of many essential enzymes of glycolysis such as TPI1, ALDOA, and PGAM1. A previous report using positron emission tomography showed that familial bipolar depressive patients had decreased blood flow in the cerebrum and a decreased rate of glucose metabolism in the ventral anterior cingulate cortex [37]. As indicated by an alteration in energy metabolism, compromised metabolic function has been reported in bipolar disorder [48], [49]. In these studies, alteration of mitochondrial proteins was reported. Mitochondria are involved in processes including the TCA cycle, glycolysis and gluconeogenesis, lipogenesis, and malate-asparate shuttle [50]. Thus, changes in these proteins may lead to major alterations in the energy pathways, thus affecting ATP production. Recently, many reports have suggested that mitochondrial dysfunction is involved in bipolar disorder and other psychiatric disorders [51], [52], [53]. Mitochondria are also involved in other essential processes such as apoptosis, oxidative stress, and calcium regulation [50]. Thus, a decrease in energy production due to mitochondrial dysfunction in the brains of patients with bipolar disorder may be compensated for by an increase in energy production by glycolysis. It is possible that mitochondrial dysfunction affects neuronal cell death. Further study is needed to know whether these alterations in glycolysis-related proteins are a cause or consequence of the disease process.
This is the first study to our knowledge to apply proteomics for the analysis of monozygotic twins discordant for bipolar disorder, and it has major limitations. First of all, we analyzed only a single pair of monozygotic twins. Thus, results cannot be applied to bipolar disorder in general. Another limitation is the tissue examined; that is, lymphoblastoid cells. Although brain samples may be optimal to identify molecules directly related to bipolar disorder, brain samples of twins are difficult to access. In addition, accessible tissues such as body fluid and peripheral cells such as serum, plasma, cerebrospinal fluids, saliva, urine, and peripheral blood cells should be used for biomarkers. In this study, we used lymphoblastoid cells and avoided a possible effect of medication by culturing the cells in drug-free media. However, a possibility that the effect of medication at the collection of blood last even after culturing the cells in drug-free media for a month cannot be totally ruled out. The other major limitation is the small number of case–control samples.
In summary, we performed a proteomic analysis of lymphoblastoid cells in a pair of monozygotic twins discordant for bipolar disorder. The identified proteins were mainly categorized as those involved in cell death and glycolysis. In a case–control study, protein expression of PGAM1, which is related to glycolysis, was significantly higher in patients than in healthy controls. The present findings suggest future new targets that may be relevant to the pathology of bipolar disorder. The present results need to be tested in a larger, independent sample set to reach a valid conclusion.
Funding Statement
This study was supported by grant-in-aid from Japanese Ministry of Health, Labour and Welfare, and a grant from Japanese Ministry of Education, Culture, Sports, Science and Technology to AK and TK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gershon ES, Cloninger CR (1994) Genetic approaches to mental disorders. Washington, DC: American Psychiatric Press.
- 2.Goodwin FK, Jomison KR (1990) Manic-depressive illness. New York: Oxford University Press.
- 3. Bunney WE Jr, Davis JM (1965) Norepinephrine in depressive reactions. A review. Arch Gen Psychiatry 13: 483–494. [DOI] [PubMed] [Google Scholar]
- 4.Meltzer H (1989) Serotonergic dysfunction in depression. Br J Psychiatry Suppl: 25–31. [PubMed]
- 5. Chuang DM, Chen RW, Chalecka-Franaszek E, Ren M, Hashimoto R, et al. (2002) Neuroprotective effects of lithium in cultured cells and animal models of diseases. Bipolar Disord 4: 129–136. [DOI] [PubMed] [Google Scholar]
- 6. Sklar P, Smoller JW, Fan J, Ferreira MA, Perlis RH, et al. (2008) Whole-genome association study of bipolar disorder. Mol Psychiatry 13: 558–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ferreira MA, O'Donovan MC, Meng YA, Jones IR, Ruderfer DM, et al. (2008) Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet 40: 1056–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Altamura AC, Dell'Osso B, Berlin HA, Buoli M, Bassetti R, et al. (2010) Duration of untreated illness and suicide in bipolar disorder: a naturalistic study. Eur Arch Psychiatry Clin Neurosci 260: 385–391. [DOI] [PubMed] [Google Scholar]
- 9. Schwarz E, Bahn S (2008) The utility of biomarker discovery approaches for the detection of disease mechanisms in psychiatric disorders. Br J Pharmacol 153 Suppl 1S133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. English JA, Pennington K, Dunn MJ, Cotter DR (2011) The neuroproteomics of schizophrenia. Biol Psychiatry 69: 163–172. [DOI] [PubMed] [Google Scholar]
- 11. Iwamoto K, Bundo M, Kato T (2005) Altered expression of mitochondria-related genes in postmortem brains of patients with bipolar disorder or schizophrenia, as revealed by large-scale DNA microarray analysis. Hum Mol Genet 14: 241–253. [DOI] [PubMed] [Google Scholar]
- 12. Fountoulakis M, Hardmeier R, Hoger H, Lubec G (2001) Postmortem changes in the level of brain proteins. Exp Neurol 167: 86–94. [DOI] [PubMed] [Google Scholar]
- 13. Franzen B, Yang Y, Sunnemark D, Wickman M, Ottervald J, et al. (2003) Dihydropyrimidinase related protein-2 as a biomarker for temperature and time dependent post mortem changes in the mouse brain proteome. Proteomics 3: 1920–1929. [DOI] [PubMed] [Google Scholar]
- 14. Li JZ, Vawter MP, Walsh DM, Tomita H, Evans SJ, et al. (2004) Systematic changes in gene expression in postmortem human brains associated with tissue pH and terminal medical conditions. Hum Mol Genet 13: 609–616. [DOI] [PubMed] [Google Scholar]
- 15.Vawter MP, Tomita H, Meng F, Bolstad B, Li J, et al.. (2006) Mitochondrial-related gene expression changes are sensitive to agonal-pH state: implications for brain disorders. Mol Psychiatry 11: 615, 663–679. [DOI] [PMC free article] [PubMed]
- 16. Li J, Gould TD, Yuan P, Manji HK, Chen G (2003) Post-mortem interval effects on the phosphorylation of signaling proteins. Neuropsychopharmacology 28: 1017–1025. [DOI] [PubMed] [Google Scholar]
- 17. Hollander BA, Bennett GS (1991) Lithium chloride alters cytoskeletal organization in growing, but not mature, cultured chick sensory neurons. J Neurosci Res 28: 332–342. [DOI] [PubMed] [Google Scholar]
- 18. Cannell GR, Bailey MJ, Dickinson RG (2002) Inhibition of tubulin assembly and covalent binding to microtubular protein by valproic acid glucuronide in vitro. Life Sci 71: 2633–2643. [DOI] [PubMed] [Google Scholar]
- 19. Corena-McLeod Mdel P, Oliveros A, Charlesworth C, Madden B, Liang YQ, et al. (2008) Paliperidone as a mood stabilizer: a pre-frontal cortex synaptoneurosomal proteomics comparison with lithium and valproic acid after chronic treatment reveals similarities in protein expression. Brain Res 1233: 8–19. [DOI] [PubMed] [Google Scholar]
- 20. Sussulini A, Dihazi H, Banzato CE, Arruda MA, Stuhmer W, et al. (2011) Apolipoprotein A-I as a candidate serum marker for the response to lithium treatment in bipolar disorder. Proteomics 11: 261–269. [DOI] [PubMed] [Google Scholar]
- 21. Herberth M, Koethe D, Levin Y, Schwarz E, Krzyszton ND, et al. (2011) Peripheral profiling analysis for bipolar disorder reveals markers associated with reduced cell survival. Proteomics 11: 94–105. [DOI] [PubMed] [Google Scholar]
- 22. Allen MG (1976) Twin studies of affective illness. Arch Gen Psychiatry 33: 1476–1478. [DOI] [PubMed] [Google Scholar]
- 23. Bertelsen A, Harvald B, Hauge M (1977) A Danish twin study of manic-depressive disorders. Br J Psychiatry 130: 330–351. [DOI] [PubMed] [Google Scholar]
- 24. Kato T, Iwamoto K, Kakiuchi C, Kuratomi G, Okazaki Y (2005) Genetic or epigenetic difference causing discordance between monozygotic twins as a clue to molecular basis of mental disorders. Mol Psychiatry 10: 622–630. [DOI] [PubMed] [Google Scholar]
- 25. Kakiuchi C, Iwamoto K, Ishiwata M, Bundo M, Kasahara T, et al. (2003) Impaired feedback regulation of XBP1 as a genetic risk factor for bipolar disorder. Nat Genet 35: 171–175. [DOI] [PubMed] [Google Scholar]
- 26. Hu VW, Frank BC, Heine S, Lee NH, Quackenbush J (2006) Gene expression profiling of lymphoblastoid cell lines from monozygotic twins discordant in severity of autism reveals differential regulation of neurologically relevant genes. BMC Genomics 7: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Matigian N, Windus L, Smith H, Filippich C, Pantelis C, et al. (2007) Expression profiling in monozygotic twins discordant for bipolar disorder reveals dysregulation of the WNT signalling pathway. Mol Psychiatry 12: 815–825. [DOI] [PubMed] [Google Scholar]
- 28. Kuratomi G, Iwamoto K, Bundo M, Kusumi I, Kato N, et al. (2008) Aberrant DNA methylation associated with bipolar disorder identified from discordant monozygotic twins. Mol Psychiatry 13: 429–441. [DOI] [PubMed] [Google Scholar]
- 29. Sugawara H, Iwamoto K, Bundo M, Ueda J, Miyauchi T, et al. (2011) Hypermethylation of serotonin transporter gene in bipolar disorder detected by epigenome analysis of discordant monozygotic twins. Translational Psychiatry 1: e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gygi SP, Rochon Y, Franza BR, Aebersold R (1999) Correlation between protein and mRNA abundance in yeast. Mol Cell Biol 19: 1720–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Greenbaum D, Colangelo C, Williams K, Gerstein M (2003) Comparing protein abundance and mRNA expression levels on a genomic scale. Genome Biol 4: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kato T, Ishiwata M, Mori K, Washizuka S, Tajima O, et al. (2003) Mechanisms of altered Ca2+ signalling in transformed lymphoblastoid cells from patients with bipolar disorder. Int J Neuropsychopharmacol 6: 379–389. [DOI] [PubMed] [Google Scholar]
- 33. Vercauteren FG, Bergeron JJ, Vandesande F, Arckens L, Quirion R (2004) Proteomic approaches in brain research and neuropharmacology. Eur J Pharmacol 500: 385–398. [DOI] [PubMed] [Google Scholar]
- 34. Campbell JW, Watson HC, Hodgson GI (1974) Structure of yeast phosphoglycerate mutase. Nature 250: 301–303. [DOI] [PubMed] [Google Scholar]
- 35. Novikova SI, He F, Cutrufello NJ, Lidow MS (2006) Identification of protein biomarkers for schizophrenia and bipolar disorder in the postmortem prefrontal cortex using SELDI-TOF-MS ProteinChip profiling combined with MALDI-TOF-PSD-MS analysis. Neurobiol Dis 23: 61–76. [DOI] [PubMed] [Google Scholar]
- 36. Benes FM, Matzilevich D, Burke RE, Walsh J (2006) The expression of proapoptosis genes is increased in bipolar disorder, but not in schizophrenia. Mol Psychiatry 11: 241–251. [DOI] [PubMed] [Google Scholar]
- 37. Drevets WC, Price JL, Simpson JR Jr, Todd RD, Reich T, et al. (1997) Subgenual prefrontal cortex abnormalities in mood disorders. Nature 386: 824–827. [DOI] [PubMed] [Google Scholar]
- 38. Benes FM, Vincent SL, Todtenkopf M (2001) The density of pyramidal and nonpyramidal neurons in anterior cingulate cortex of schizophrenic and bipolar subjects. Biol Psychiatry 50: 395–406. [DOI] [PubMed] [Google Scholar]
- 39. Ellison-Wright I, Bullmore E (2010) Anatomy of bipolar disorder and schizophrenia: a meta-analysis. Schizophr Res 117: 1–12. [DOI] [PubMed] [Google Scholar]
- 40. Bora E, Fornito A, Yucel M, Pantelis C (2010) Voxelwise meta-analysis of gray matter abnormalities in bipolar disorder. Biol Psychiatry 67: 1097–1105. [DOI] [PubMed] [Google Scholar]
- 41. Manji HK, Moore GJ, Chen G (2000) Clinical and preclinical evidence for the neurotrophic effects of mood stabilizers: implications for the pathophysiology and treatment of manic-depressive illness. Biol Psychiatry 48: 740–754. [DOI] [PubMed] [Google Scholar]
- 42. Manji HK, Moore GJ, Rajkowska G, Chen G (2000) Neuroplasticity and cellular resilience in mood disorders. Mol Psychiatry 5: 578–593. [DOI] [PubMed] [Google Scholar]
- 43. Kapczinski F, Frey BN, Kauer-Sant'Anna M, Grassi-Oliveira R (2008) Brain-derived neurotrophic factor and neuroplasticity in bipolar disorder. Expert Rev Neurother 8: 1101–1113. [DOI] [PubMed] [Google Scholar]
- 44. Yuan PX, Huang LD, Jiang YM, Gutkind JS, Manji HK, et al. (2001) The mood stabilizer valproic acid activates mitogen-activated protein kinases and promotes neurite growth. J Biol Chem 276: 31674–31683. [DOI] [PubMed] [Google Scholar]
- 45. Manji HK, Chen G (2002) PKC, MAP kinases and the bcl-2 family of proteins as long-term targets for mood stabilizers. Mol Psychiatry 7 Suppl 1S46–56. [DOI] [PubMed] [Google Scholar]
- 46. Villar-Palasi C, Larner J (1970) Glycogen metabolism and glycolytic enzymes. Annu Rev Biochem 39: 639–672. [DOI] [PubMed] [Google Scholar]
- 47. Johnston-Wilson NL, Sims CD, Hofmann JP, Anderson L, Shore AD, et al. (2000) Disease-specific alterations in frontal cortex brain proteins in schizophrenia, bipolar disorder, and major depressive disorder. The Stanley Neuropathology Consortium. Mol Psychiatry 5: 142–149. [DOI] [PubMed] [Google Scholar]
- 48. Pennington K, Beasley CL, Dicker P, Fagan A, English J, et al. (2008) Prominent synaptic and metabolic abnormalities revealed by proteomic analysis of the dorsolateral prefrontal cortex in schizophrenia and bipolar disorder. Mol Psychiatry 13: 1102–1117. [DOI] [PubMed] [Google Scholar]
- 49. English JA, Dicker P, Focking M, Dunn MJ, Cotter DR (2009) 2-D DIGE analysis implicates cytoskeletal abnormalities in psychiatric disease. Proteomics 9: 3368–3382. [DOI] [PubMed] [Google Scholar]
- 50.Scheffler IE (1999) Mitochondria: Wiley-Liss.
- 51. Kato T, Kato N (2000) Mitochondrial dysfunction in bipolar disorder. Bipolar Disord 2: 180–190. [DOI] [PubMed] [Google Scholar]
- 52. Clay HB, Sillivan S, Konradi C (2011) Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int J Dev Neurosci 29: 311–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Manji H, Kato T, Di Prospero NA, Ness S, Beal MF, et al. (2012) Impaired mitochondrial function in psychiatric disorders. Nat Rev Neurosci 13: 293–307. [DOI] [PubMed] [Google Scholar]