Abstract
Several epidemiological studies have shown that exercise (EX) and physical activity (PA) can prevent or delay the onset of different mental disorders, and have therapeutic benefits when used as sole or adjunct treatment in mental disorders. This review summarizes studies that used EX interventions in patients with anxiety, affective, eating, and substance use disorders, as well as schizophrenia and dementia/mild cognitive impairment. Despite several decades of clinical evidence with EX interventions, controlled studies are sparse in most disorder groups. Preliminary evidence suggests that PA/EX can induce improvements in physical, subjective and disorder-specific clinical outcomes. Potential mechanisms of action are discussed, as well as implications for psychiatric research and practice.
Keywords: Exercise, Mental disorders, Motor activity
INTRODUCTION
Mental disorders constitute a huge social and economic burden for health care systems worldwide [1], raising the question of effective and lasting treatments. Physical activity (PA) and exercise (EX) continue to gain the attention of practitioners and researchers with regard to prevention and treatment of different psychopathological abnormalities.
Epidemiology/Correlational Studies
In the general population, several epidemiological studies have found significant cross-sectional correlations between mental health and PA levels. In an adult US population, regular PA is associated with a significantly decreased prevalence of current major depression, panic disorder, agoraphobia, social phobia, and specific phobia [2]. A study from Norway confirmed this negative cross-sectional association between depression and leisure-time PA of any intensity (not work-related PA), and pointed out that social factors such as social support, rather than biological markers, play an important role [3]. Recently, a Dutch study replicated this finding, reporting lower rates of any affective, anxiety, or substance use disorder in subjects who exercised at least 1 h/wk, without finding a linear dose-response relationship [4].
Prospectively, the overall incidence of mental disorders and co-morbid mental disorders, as well as the incidence of anxiety, somatoform, and dysthymic disorder, decreases by PA [5]. Furthermore, a four-year prospective study revealed that PA decreases the incidence rates of depressive and anxiety disorders in older adults [6]. Finally, ten Have et al. reported in their epidemiological study that patients engaging in regular PA were more likely to recover from their mental illness at a three-year follow-up [4].
Mechanisms of Action
In psychiatric patients, different mechanisms of action for PA and EX have been discussed: On a neurochemical and physiological level, a number of acute changes occur during and following bouts of EX, and several long-term adaptations are related to regular EX training. For instance, EX has been found to normalize reduced levels of brain-derived neurotrophic factor (BDNF) and therefore has neuroprotective or even neurotrophic effects [7-9]. Animal studies found EX-induced changes in different neurotransmitters such as serotonin and endorphins [10,11], which relate to mood, and positive effects of EX on stress reactivity (e.g., the hypothalamus-pituitary-adrenal axis [12,13]). Finally, anxiolytic effects of EX mediated by atrial natriuretic peptide have been reported [14]. Potential psychological mechanisms of action include learning and extinction, changes in body scheme and health attitudes/behaviors, social reinforcement, experience of mastery, shift of external to more internal locus of control, improved coping strategies, or simple distraction [15,16].
Physical Comorbidity
Patients with mental disorders display a high comorbidity of physical conditions such as respiratory, metabolic, cardio-vascular and neurologic diseases [17,18]. Many of the conditions named above are linked to overweight, smoking, and unhealthy lifestyle [19]; therefore lifestyle interventions based on nutrition and EX are promising approaches for reducing physical comorbidity [20]. Furthermore, psychiatric patients who regularly exercised reported higher health-related quality of life in a cross-sectional study [21].
METHODS
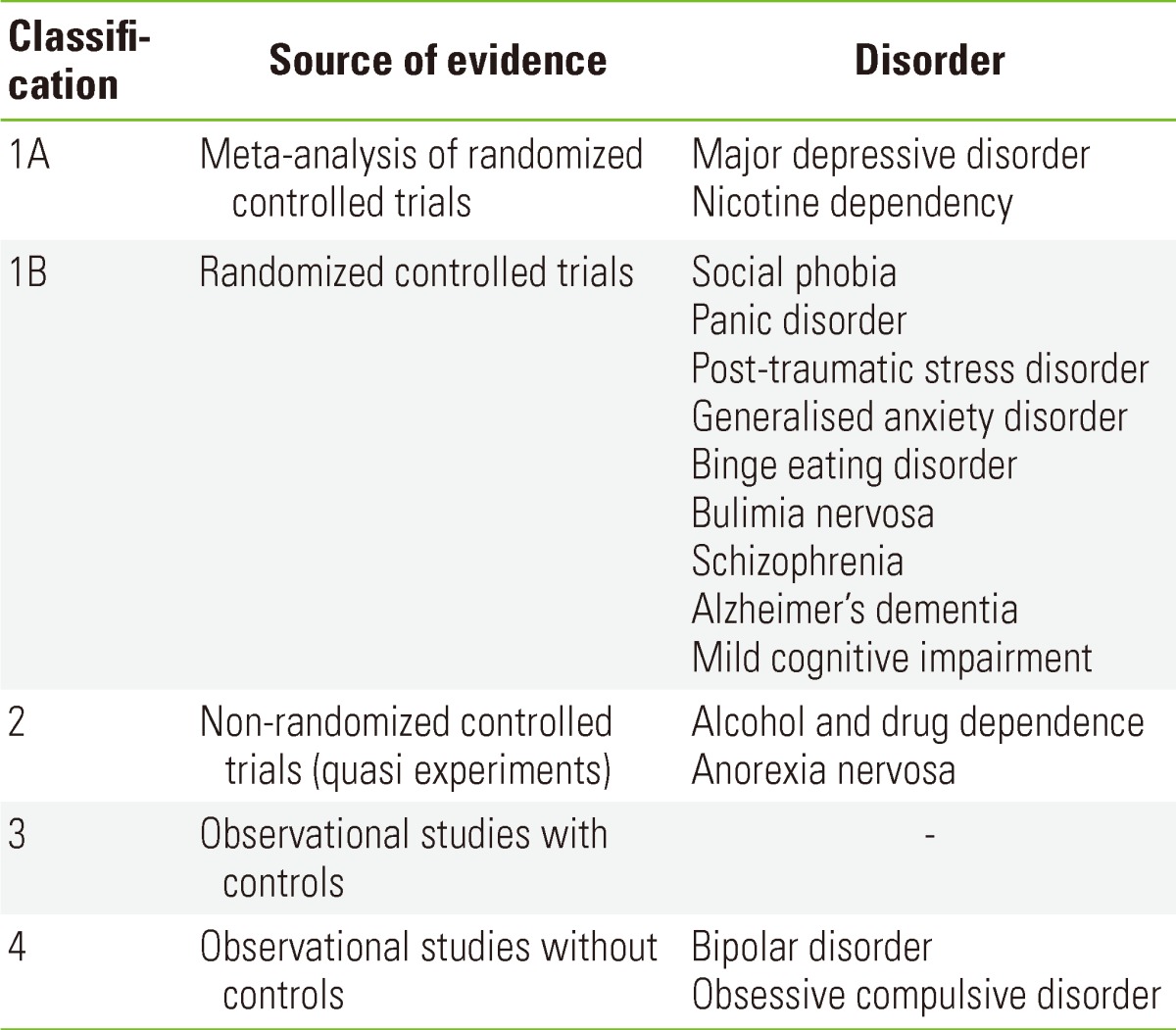
For the present article, the search engines PubMed, Medline, and Web of Science were comprehensively searched for original research articles or reviews in English, German, or French published between 1970 and 2012. The following search terms were used: [exercise OR physical activity] AND [mental disorder OR affective disorder OR depression OR mania OR bipolar disorder OR anxiety OR panic disorder OR agoraphobia OR social phobia OR generalized anxiety disorder OR posttraumatic stress disorder OR obsessive-compulsive disorder OR eating disorder OR anorexia nervosa OR bulimia nervosa OR binge eating disorder OR substance use disorder OR alcohol OR nicotine OR illicit drug OR cannabis OR cocaine OR heroine OR amphetamine OR schizophrenia OR psychosis OR dementia OR mild cognitive impairment OR cognitive decline OR Alzheimer's disease]. The bibliographies of all retrieved articles were searched for additional references. Only intervention studies using EX and PA as a sole or combined treatment and reviews/meta-analyses focusing on intervention studies were included. The level of evidence is heterogeneous amongst different mental disorders (Table 1). In the following sections, evidence for EX/PA interventions is summarized for anxiety disorders, obsessive-compulsive disorder, affective disorders, eating disorders, substance use disorders, schizophrenia/psychosis, and dementia/mild cognitive impairment.
Table 1.
Level of evidence for the therapeutic activity of exercise according to the Agency of Heath Care Policy and Research
RESULTS: EXERCISE INTERVENTIONS IN MENTAL DISORDERS
Anxiety Disorders
In anxiety disorders, one possible mechanism of action is the EX-induced reduction in anxiety sensitivity, a personality trait related to the development and course of anxiety disorders [22]. Subjects with high anxiety sensitivity also report lower levels of PA, higher perceived barriers, and lower benefits of PA, compared to subjects with low anxiety sensitivity [23].
Two meta-analyses concluded that acute and chronic interventions result in decreases in state- and trait anxiety and psycho-physiological correlates of anxiety in different clinical and non-clinical samples [24,25]. Specifically, aerobic and anaerobic EX were found to be similarly effective as cognitive/behavioral therapy, and more effective than most other anxiety-reducing activities [25]. Additionally, a recent study in adults with intellectual disabilities found that an EX intervention decreased trait and state anxiety in this population [26].
Panic disorder
One of the first studies compared a jogging and a walking intervention in patients with panic disorder, finding similar symptom reductions in both groups after eight weeks, and negative correlations between fitness increase and anxiety scores [27]. Comparing endurance training with clomipramine and a placebo revealed that both active treatments were significantly different from the placebo after ten weeks, although the effects of clomipramine occurred significantly faster, and dropout rates were higher in the EX group [28]. Another study [29] that compared paroxetine with a placebo, each combined with either relaxation or running respectively, reported significant effects for paroxetine compared to placebo, but mostly no differences between EX and relaxation. A recently-published randomized controlled trial (RCT) [30] compared EX to standardized cognitive-behavioral therapy (CBT) and found CBT to be superior to EX in reducing panic and agoraphobic symptoms up to 12 months post-treatment. However, significant symptom reduction relative to baseline was seen in the EX group as well.
Three studies focusing on acute EX found a protective effect of EX against the subsequent induction of panic attacks via CO2 [31,32] and CCK-4 [33].
Post-traumatic stress disorder
Evidence is sparse for post-traumatic stress disorder (PTSD). In three pilot studies, positive effects of aerobic EX [34,35] and moderate walking [36] on PTSD symptom severity and associated depressive and anxious symptoms in children [35], adolescents [36], and adults [34] have been reported. However, all of these studies had severe methodological limitations such as very small sample sizes, inclusion of participants without a clinical diagnosis of PTSD, and a lack of control groups.
A RCT focusing on pain in traumatized refugees showed that EX further improved therapy outcomes of biofeedback-based CBT [37]. More RCTs with sufficient sample sizes are needed to determine positive effects and possible risks or adverse events when using EX as adjunct treatment in this clinical population.
Generalized anxiety disorder
In a recent RCT, a six-week program of resistance EX or aerobic EX (two weekly sessions) was applied in sedentary female generalized anxiety disorder patients. Compared to a wait list control, reductions in anxiety-tension and irritability were found in the resistance EX group after six weeks [38], as well as moderately lower worry symptoms in the combined EX groups [39].
Social phobia
Only one study targeted EX interventions for social phobia so far, comparing EX to mindfulness-based stress reduction [40]. Both interventions were associated with diminished social anxiety and depression and increased subjective well-being post-intervention and after three months.
Other anxiety disorders/mixed samples
Two clinical trials [41,42] found that patients suffering from different anxiety disorders achieved higher levels of PA and functional capacity through EX training [42], and that anxiety, depression, and perceived stress declined significantly more strongly in a combined CBT+EX treatment, compared to CBT alone [41]. Patients with social phobia were more likely to benefit from the EX enhancement, compared to patients suffering from other anxiety disorders.
Obsessive Compulsive Disorder
Preliminary evidence for the beneficial effects of EX on obsessive-compulsive and concurrent anxious and depressive symptoms comes from two pilot studies. In patients stably medicated with selective serotonin-reuptake inhibitors, reductions in self-reported obsessive compulsive disorder (OCD) symptoms and depression after six weeks of walking intervention and at one-month follow-up were found, as well as temporarily reduced anxiety scores [43]. Combining behavioral therapy or pharmacotherapy with a 12-week moderate aerobic EX program, the second study reported reduced OCD symptom severity at the end of the treatment, and up to 6 months later [44]. After each 20- to 40-minute training session, patients reported significantly lower anxiety, negative mood, and OCD symptoms relative to the beginning of the session [45]. This effect was particularly dominant at the beginning of the 12-week intervention and diminished as baseline levels decreased.
However, because of a lack of control groups and very small sample sizes, the above-listed results need to be replicated in larger controlled studies.
Affective Disorders
Major depression
A large number of clinical studies have investigated EX-induced decreases in depressive symptoms, negative affect, and sleep disturbances, and these findings have been summarized in several reviews (e.g., [46]). In a recent Cochrane review [47], meta-analyses were conducted of over 30 RCTs that either compared an EX intervention with no treatment (waitlist, placebo, no-treatment), or with any other type of intervention (psychotherapy, pharmacotherapy, alternative therapies), or EX-augmented treatment versus treatment alone. Overall, a moderate clinical effect was found when EX was compared to no-treatment or a control treatment. Contrasting EX interventions to cognitive therapy (six trials) or antidepressants (three trials), no significant differences in the reduction of depressive symptoms were found at the end of treatment, indicating that EX was as effective as these standard treatments. Considering only studies with adequate allocation concealment, intention-to-treat analysis and blinded outcome assessment, only a small effect in favor of EX was found. Follow-up data from seven trials also indicated a small long-term benefit of EX interventions. Mixed and resistance EX showed larger effect sizes (but also larger confidence intervals) than aerobic EX.
In contrast to studies on dementia/mild cognitive impairment (see Mild Cognitive Impairment section), EX failed to improve neurocognitive functions in depressed middle-aged and older adults, when compared to sertraline and a placebo [48]. Some studies, however, reported normalized BDNF levels after acute EX in remitted MDD patients [49].
Bipolar disorder
Bipolar patients experience faster exhaustion during moderate aerobic EX than healthy controls [50]. Two studies investigated the effects of regular aerobic EX training [51,52], indicating that PA interventions (both elective and prescribed) are feasible for bipolar disorder (BD) patients, and decrease stress, depressive, and anxious symptoms [53]. All of the cited studies lacked power and adequate experimental control strategies; therefore, further research will need to determine the potential benefits, but also the limitations and risks of PA in this population (for detailed suggestions see [53]). Using semi-structured interviews, Wright and colleagues carved out subjective benefits, potential harms, and barriers to EX in BD patients, concluding that EX is perceived to be helpful in managing mood fluctuations on the one hand, but on the other hand to inhere a certain risk of intensifying manic symptoms [54].
Other reviews discussed EX-induced changes in neurotransmission in BD [55], EX as a possible treatment for neurocognitive dysfunction in BD [56], and reductions of allostatic load by EX [9].
Eating Disorders
As in BD, the role of PA and EX in eating disorders is ambivalent, displaying positive aspects such as weight loss in patients with binge eating disorder (BED), or prevention of bone mass loss in anorexia nervosa (AN), and negative aspects like excessive PA with compulsive features and deteriorating therapy outcomes [57].
Binge eating disorder
In BED, the promotion of EX is essential, given that most patients tend not to exercise at all [58]. Of the two studies addressing the therapeutic effects of EX in BED, one found moderately reduced weight and depression scores after six months of moderate EX intervention (walking) compared to a control group [59], and the other one reported significantly larger reductions in body mass index (BMI), depression scores, and binge episodes with up to 12 months of combined CBT+EX treatment [60]. Interestingly, the second study revealed positive effects despite sub-optimal EX compliance, with patients' activity levels returning to baseline immediately after the end of treatment. This observation is in line with findings suggesting that the perceived effects of being active may be more relevant than actual fitness gains [61].
Bulimia nervosa
The only study published for bulimia nervosa compared EX to CBT treatment and found that EX was as effective as CBT in reducing the "bulimia" and "body dissatisfaction" subscales of the Eating Disorder Inventory, but surpassed CBT in terms of "drive for thinness" and bulimic behavior up to 18 months after discharge [62].
Anorexia nervosa
Reviewing six studies on the effects of EX in AN, Zunker et al. [63] concluded that EX programs with light to moderate intensity seem to have the potential to reduce obligatory attitudes and beliefs towards EX, reduce emotional stress, protect bone mass, and enhance weight gain. One additional recent study found neither beneficial nor detrimental effects of a 12-week resistance training program in teenage anorectic patients [64]. Since none of the studies did satisfy RCT criteria (lacking randomization [one trial], quasi-experimental design [one trial] or had insufficient sample sizes [four trials]), further research is needed in this patient group.
Substance Use Disorders
Nicotine dependence
For nicotine dependence, there is evidence from a large number of RCTs that EX, combined with CBT and/or nicotine replacement therapy, has a complementary benefit on therapy outcomes in smoking cessation (see [65,66] for reviews). This effect mainly relies on acute relief of cigarette craving, which helps to prevent relapse. In order to successfully support patients, EX programs should begin prior to smoking cessation, have rather high intensities, a minimum duration of about ten weeks, and promote EX as a coping strategy for acute mood-regulation and craving-reduction [65].
Alcohol and drug dependence
In contrast, evidence is much weaker for the efficacy of EX in alcohol and drug rehabilitation (see [66] for a review). Most published studies have not employed adequate control groups, had sample sizes that were too small, non-generalizable populations like homeless veterans, heavy-drinking college students without clinical diagnosis, or mandatorily treated patients, or no intention-to-treat-analyses to correct for the high number of dropouts.
However, there is preliminary evidence for additional benefits of EX in terms of abstinence, concurrent depression, and anxiety symptoms, which is supported by a large number of preclinical studies [67]. Future RTCs with sufficient sample sizes and controlled designs are necessary to confirm or disprove these findings. Besides effects specific for EX, different mechanisms of action (structured social events, general lifestyle modifications, a non-substance use-related social environment) have been discussed in the literature [15] and should be investigated in the context of SUDs.
Schizophrenia/Psychosis
Compared to standard care, stronger (yet non-significant) reductions in body fat, BMI, and positive and negative symptoms were found after 16 weeks of treadmill training in one study [68]. Another study [69] combined 12 weeks of aerobic and strength training, finding significant improvements in the total Mental Health Inventory score in the EX group compared to standard care, which were correlated with increased functional capacity. One additional quasi-experimental study found significant reductions in positive and negative symptoms after ten weeks of moderate aerobic EX compared to standard therapy [70]. A recent study demonstrated that one possible mechanism of action in schizophrenia is EX-induced neuroprotection/neurogenesis [71]. This study not only found EX-induced decreases in positive and negative symptoms, but also increases in hippocampal volumes after three months of aerobic EX [71]. Those increases also were positively correlated with fitness increases [71].
Recently, a couple of studies investigated the effects of yoga on positive and negative symptoms in schizophrenia, and a review of three RCTs [72] concluded that yoga was more effective than EX with regard to symptom reduction. Acutely, 30 minutes of EX or yoga were found to reduce state anxiety and distress [73].
Dementia/Mild Cognitive Impairment
Several prospective studies have found that a high level of PA seems to delay the onset of dementia (see [74] for a review). Since improvements in strength and endurance after training were found in cognitively impaired patients as well as healthy controls [75], PA interventions are generally feasible in this population.
Mild cognitive impairment
Several studies investigated the impact of PA interventions in elderly individuals with mild cognitive impairment (MCI), reporting heterogeneous results. A recent review concluded that EX interventions of all types are beneficial to slow down cognitive decline, and that the best effects can be found with moderate intensity EX (e.g., brisk walking) for at least 30 minutes on five days per week [76]. Interventions with different types of PA and a group setting seem to be particularly helpful in this population. In one study, it became evident that partial improvements in memory and attention occurred only in subjects with greater EX adherence [77].
Alzheimer's disease
For Alzheimer's disease (AD), preliminary evidence suggests that EX interventions may improve communication performance [78], Mini Mental State Examination scores and verbal fluency [79], and disruptive behavior [80]. Four studies [81-84] found that PA slowed down and partially reversed the decline in performance of activities of daily living and progression of the cognitive symptoms related to dementia, in contrast to an older study, which did not find improvements in functional ability [85].
Potential neurophysiological mechanisms and target transmitter systems of EX interventions in cognitive decline and AD are summarized in a recent review [86].
CONCLUSIONS AND FUTURE DIRECTIONS
Although a number of studies have yielded positive results on the effectiveness of EX as an adjunct treatment, evidence is limited for most psychiatric disorders. Generally, studies using equal contact control groups revealed smaller effects than studies comparing PA with no intervention. This leads to the assumption that unspecific effects such as therapeutic contact, social support, and distraction may drive some of the effects of lower intensity EX in particular, which is in line with epidemiological findings [3]. Cost-efficacy cannot be estimated for any group of disorders yet. Future studies should consider risks and adverse effects, as well as the benefits of EX. The precise description of conditions, standardized interventions, validated assessment strategies, adequate randomization and control conditions, and power estimations are essential to obtain meaningful results and to allow for the calculation of effect sizes in meta-analyses.
However, some conclusions can be drawn concerning frame conditions, which can make EX a promising intervention for mental disorders: studies that followed public health recommendations [87] concerning the intensity and duration of their EX intervention were more likely to find significant clinical improvements. Patients' compliance during the EX program and continuation after program termination were found to be more relevant for treatment outcomes than actual fitness gains [61,88]. Social support seems to be crucial for EX adherence and positive effects of EX [3,89], as may be time structure, therapeutic contact, and positive reinforcement [15]. There is evidence that indoor/outdoor activity may have differential effects on mood states [90]. Professional supervision and training management should be provided, especially in the beginning, and PA and EX should be integrated into psychotherapy (e.g., using training and mood diaries). Recent studies indicate that training effects and mood improvements can also be achieved using internet- or telecommunication-based support [91,92]. Caregivers providing EX should be aware of differential acute effects depending on training history and actual fitness: trained subjects usually experience greater improvements in vigor, positive affect, and fatigue, than non-trained subjects (e.g., [24,93]).
Besides physical EX, "mindful EX interventions", such as yoga, draw significant attention as adjunct treatment, for example, in depression and anxiety [94], schizophrenia, eating disorders [95], and smoking cessation [96,97]. Also, martial arts were found to have favorable acute effects in depressed patients [98].
Implications for Future Research
In EX research, blinding of the patients is a general problem: the patients know that EX is supposed to make them feel better, resulting in a potential bias (Rosenthal effect), which points out the need for adequate and credible control interventions. The dose-response relationship remains unclear for most mental disorders (except for MDD and some aspects of anxiety), as well as the most effective type of EX for each disorder group. Costs, efficacy, risks, adverse events, and contraindications of EX interventions need to be specified. Finally, strategies are needed to enhance motivation of patients during the program and after program termination [99].
ACKNOWLEDGEMENTS
This article is based on a presentation of Andreas Ströhle in Taiwan and a recent publication of the authors (Wolff et al. Eur Arch Psychiatry Clin Neurosci 2011;261 Suppl 2:S186-S191.). Work on this article was in part supported by a grant of the German Ministry of Education and Research to Andreas Ströhle (BMBF 01GV0612).
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
References
- 1.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- 3.Harvey SB, Hotopf M, Overland S, Mykletun A. Physical activity and common mental disorders. Br J Psychiatry. 2010;197(5):357–364. doi: 10.1192/bjp.bp.109.075176. [DOI] [PubMed] [Google Scholar]
- 4.Ten Have M, de Graaf R, Monshouwer K. Physical exercise in adults and mental health status findings from the Netherlands mental health survey and incidence study (NEMESIS) J Psychosom Res. 2011;71(5):342–348. doi: 10.1016/j.jpsychores.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Ströhle A, Höfler M, Pfister H, Müller AG, Hoyer J, Wittchen HU, et al. Physical activity and prevalence and incidence of mental disorders in adolescents and young adults. Psychol Med. 2007;37(11):1657–1666. doi: 10.1017/S003329170700089X. [DOI] [PubMed] [Google Scholar]
- 6.Pasco JA, Williams LJ, Jacka FN, Henry MJ, Coulson CE, Brennan SL, et al. Habitual physical activity and the risk for depressive and anxiety disorders among older men and women. Int Psychogeriatr. 2011;23(2):292–298. doi: 10.1017/S1041610210001833. [DOI] [PubMed] [Google Scholar]
- 7.Seifert T, Brassard P, Wissenberg M, Rasmussen P, Nordby P, Stallknecht B, et al. Endurance training enhances BDNF release from the human brain. Am J Physiol Regul Integr Comp Physiol. 2010;298(2):R372–R377. doi: 10.1152/ajpregu.00525.2009. [DOI] [PubMed] [Google Scholar]
- 8.Ströhle A, Stoy M, Graetz B, Scheel M, Wittmann A, Gallinat J, et al. Acute exercise ameliorates reduced brain-derived neurotrophic factor in patients with panic disorder. Psychoneuroendocrinology. 2010;35(3):364–368. doi: 10.1016/j.psyneuen.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 9.Sylvia LG, Ametrano RM, Nierenberg AA. Exercise treatment for bipolar disorder: potential mechanisms of action mediated through increased neurogenesis and decreased allostatic load. Psychother Psychosom. 2010;79(2):87–96. doi: 10.1159/000270916. [DOI] [PubMed] [Google Scholar]
- 10.Fumoto M, Oshima T, Kamiya K, Kikuchi H, Seki Y, Nakatani Y, et al. Ventral prefrontal cortex and serotonergic system activation during pedaling exercise induces negative mood improvement and increased alpha band in EEG. Behav Brain Res. 2010;213(1):1–9. doi: 10.1016/j.bbr.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Meeusen R, Piacentini MF, De Meirleir K. Brain microdialysis in exercise research. Sports Med. 2001;31(14):965–983. doi: 10.2165/00007256-200131140-00002. [DOI] [PubMed] [Google Scholar]
- 12.Rejeski WJ, Thompson A, Brubaker PH, Miller HS. Acute exercise: buffering psychosocial stress responses in women. Health Psychol. 1992;11(6):355–362. doi: 10.1037//0278-6133.11.6.355. [DOI] [PubMed] [Google Scholar]
- 13.Rimmele U, Zellweger BC, Marti B, Seiler R, Mohiyeddini C, Ehlert U, et al. Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men. Psychoneuroendocrinology. 2007;32(6):627–635. doi: 10.1016/j.psyneuen.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Ströhle A, Feller C, Onken M, Godemann F, Heinz A, Dimeo F. The acute antipanic activity of aerobic exercise. Am J Psychiatry. 2005;162(12):2376–2378. doi: 10.1176/appi.ajp.162.12.2376. [DOI] [PubMed] [Google Scholar]
- 15.Read JP, Brown RA. The role of physical exercise in alcoholism treatment and recovery. Prof Psychol Res Pract. 2003;34(1):49–56. [Google Scholar]
- 16.Stathopoulou G, Powers MB, Berry AC, Smits JA, Otto MW. Exercise interventions for mental health: a quantitative and qualitative review. Clin Psychol Sci Pract. 2006;13(2):179–193. [Google Scholar]
- 17.Lin WC, Zhang J, Leung GY, Clark RE. Chronic physical conditions in older adults with mental illness and/or substance use disorders. J Am Geriatr Soc. 2011;59(10):1913–1921. doi: 10.1111/j.1532-5415.2011.03588.x. [DOI] [PubMed] [Google Scholar]
- 18.Scott K, McGee MA, Schaaf D, Baxter J. Mental-physical comorbidity in an ethnically diverse population. Soc Sci Med. 2008;66(5):1165–1173. doi: 10.1016/j.socscimed.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment Health Nurs. 2011;32(9):589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- 20.Chacón F, Mora F, Gervás-Ríos A, Gilaberte I. Efficacy of lifestyle interventions in physical health management of patients with severe mental illness. Ann Gen Psychiatry. 2011;10:22. doi: 10.1186/1744-859X-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmitz N, Kruse J, Kugler J. The association between physical exercises and health-related quality of life in subjects with mental disorders: results from a cross-sectional survey. Prev Med. 2004;39(6):1200–1207. doi: 10.1016/j.ypmed.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 22.Smits JA, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depress Anxiety. 2008;25(8):689–699. doi: 10.1002/da.20411. [DOI] [PubMed] [Google Scholar]
- 23.Sabourin BC, Hilchey CA, Lefaivre MJ, Watt MC, Stewart SH. Why do they exercise less? Barriers to exercise in high-anxiety-sensitive women. Cogn Behav Ther. 2011;40(3):206–215. doi: 10.1080/16506073.2011.573572. [DOI] [PubMed] [Google Scholar]
- 24.Petruzzello SJ, Jones AC, Tate AK. Affective responses to acute exercise: a test of opponent-process theory. J Sports Med Phys Fitness. 1997;37(3):205–212. [PubMed] [Google Scholar]
- 25.Wipfli BM, Rethorst CD, Landers DM. The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. J Sport Exerc Psychol. 2008;30(4):392–410. doi: 10.1123/jsep.30.4.392. [DOI] [PubMed] [Google Scholar]
- 26.Carraro A, Gobbi E. Effects of an exercise programme on anxiety in adults with intellectual disabilities. Res Dev Disabil. 2012;33(4):1221–1226. doi: 10.1016/j.ridd.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 27.Sexton H, Maere A, Dahl NH. Exercise intensity and reduction in neurotic symptoms. A controlled follow-up study. Acta Psychiatr Scand. 1989;80(3):231–235. doi: 10.1111/j.1600-0447.1989.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 28.Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603–609. doi: 10.1176/ajp.155.5.603. [DOI] [PubMed] [Google Scholar]
- 29.Wedekind D, Broocks A, Weiss N, Engel K, Neubert K, Bandelow B. A randomized, controlled trial of aerobic exercise in combination with paroxetine in the treatment of panic disorder. World J Biol Psychiatry. 2010;11(7):904–913. doi: 10.3109/15622975.2010.489620. [DOI] [PubMed] [Google Scholar]
- 30.Hovland A, Nordhus IH, Sjøbø T, Gjestad BA, Birknes B, Martinsen EW, et al. Comparing physical exercise in groups to group cognitive behaviour therapy for the treatment of panic disorder in a randomized controlled trial. Behav Cogn Psychother. 2012 doi: 10.1017/S1352465812000446. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Esquivel G, Dandachi A, Knuts I, Goossens L, Griez E, Schruers K. Effects of acute exercise on CO(2)-induced fear. Depress Anxiety. 2012;29(2):155–158. doi: 10.1002/da.20860. [DOI] [PubMed] [Google Scholar]
- 32.Esquivel G, Díaz-Galvis J, Schruers K, Berlanga C, Lara-Muñoz C, Griez E. Acute exercise reduces the effects of a 35% CO2 challenge in patients with panic disorder. J Affect Disord. 2008;107(1-3):217–220. doi: 10.1016/j.jad.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 33.Ströhle A, Graetz B, Scheel M, Wittmann A, Feller C, Heinz A, et al. The acute antipanic and anxiolytic activity of aerobic exercise in patients with panic disorder and healthy control subjects. J Psychiatr Res. 2009;43(12):1013–1017. doi: 10.1016/j.jpsychires.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Manger TA, Motta RW. The impact of an exercise program on posttraumatic stress disorder, anxiety, and depression. Int J Emerg Ment Health. 2005;7(1):49–57. [PubMed] [Google Scholar]
- 35.Newman CL, Motta RW. The effects of aerobic exercise on childhood PTSD, anxiety, and depression. Int J Emerg Ment Health. 2007;9(2):133–158. [PubMed] [Google Scholar]
- 36.Diaz AB, Motta R. The effects of an aerobic exercise program on posttraumatic stress disorder symptom severity in adolescents. Int J Emerg Ment Health. 2008;10(1):49–59. [PubMed] [Google Scholar]
- 37.Liedl A, Müller J, Morina N, Karl A, Denke C, Knaevelsrud C. Physical activity within a CBT intervention improves coping with pain in traumatized refugees: results of a randomized controlled design. Pain Med. 2011;12(2):234–245. doi: 10.1111/j.1526-4637.2010.01040.x. [DOI] [PubMed] [Google Scholar]
- 38.Herring MP, Jacob ML, Suveg C, O'Connor P. Effects of short-term exercise training on signs and symptoms of generalized anxiety disorder. Ment Health Phys Act. 2011;4(2):71–77. [Google Scholar]
- 39.Herring MP, Jacob ML, Suveg C, Dishman RK, O'Connor PJ. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(1):21–28. doi: 10.1159/000327898. [DOI] [PubMed] [Google Scholar]
- 40.Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. J Clin Psychol. 2012 doi: 10.1002/jclp.21863. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders: a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959–968. doi: 10.1016/j.janxdis.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 42.Oeland AM, Laessoe U, Olesen AV, Munk-Jørgensen P. Impact of exercise on patients with depression and anxiety. Nord J Psychiatry. 2010;64(3):210–217. doi: 10.3109/08039480903511373. [DOI] [PubMed] [Google Scholar]
- 43.Lancer R, Motta R, Lancer D. The effect of aerobic exercise on obsessive-compulsive disorder, anxiety, and depression: a preliminary investigation. Behav Ther. 2007;30(3):53–62. [Google Scholar]
- 44.Brown RA, Abrantes AM, Strong DR, Mancebo MC, Menard J, Rasmussen SA, et al. A pilot study of moderate-intensity aerobic exercise for obsessive compulsive disorder. J Nerv Ment Dis. 2007;195(6):514–520. doi: 10.1097/01.nmd.0000253730.31610.6c. [DOI] [PubMed] [Google Scholar]
- 45.Abrantes AM, Strong DR, Cohn A, Cameron AY, Greenberg BD, Mancebo MC, et al. Acute changes in obsessions and compulsions following moderate-intensity aerobic exercise among patients with obsessive-compulsive disorder. J Anxiety Disord. 2009;23(7):923–927. doi: 10.1016/j.janxdis.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 46.Dinas PC, Koutedakis Y, Flouris AD. Effects of exercise and physical activity on depression. Ir J Med Sci. 2011;180(2):319–325. doi: 10.1007/s11845-010-0633-9. [DOI] [PubMed] [Google Scholar]
- 47.Rimer J, Dwan K, Lawlor DA, Greig CA, McMurdo M, Morley W, et al. Exercise for depression. Cochrane Database Syst Rev. 2012;7:CD004366. doi: 10.1002/14651858.CD004366.pub5. [DOI] [PubMed] [Google Scholar]
- 48.Hoffman BM, Blumenthal JA, Babyak MA, Smith PJ, Rogers SD, Doraiswamy PM, et al. Exercise fails to improve neurocognition in depressed middle-aged and older adults. Med Sci Sports Exerc. 2008;40(7):1344–1352. doi: 10.1249/MSS.0b013e31816b877c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laske C, Banschbach S, Stransky E, Bosch S, Straten G, Machann J, et al. Exercise-induced normalization of decreased BDNF serum concentration in elderly women with remitted major depression. Int J Neuropsychopharmacol. 2010;13(5):595–602. doi: 10.1017/S1461145709991234. [DOI] [PubMed] [Google Scholar]
- 50.Shah A, Alshaher M, Dawn B, Siddiqui T, Longaker RA, Stoddard MF, et al. Exercise tolerance is reduced in bipolar illness. J Affect Disord. 2007;104(1-3):191–195. doi: 10.1016/j.jad.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 51.Edenfield TM. Exercise and mood: exploring the role of exercise in regulating stress reactivity in bipolar disorder [dissertation] Orono: University of Maine; 2007. [Google Scholar]
- 52.Ng F, Dodd S, Berk M. The effects of physical activity in the acute treatment of bipolar disorder: a pilot study. J Affect Disord. 2007;101(1-3):259–262. doi: 10.1016/j.jad.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 53.Wright KA, Everson-Hock ES, Taylor AH. The effects of physical activity on physical and mental health among individuals with bipolar disorder: a systematic review. Ment Health Phys Act. 2009;2(2):86–94. [Google Scholar]
- 54.Wright K, Armstrong T, Taylor A, Dean S. 'It's a double edged sword': a qualitative analysis of the experiences of exercise amongst people with bipolar disorder. J Affect Disord. 2012;136(3):634–642. doi: 10.1016/j.jad.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 55.Alsuwaidan MT, Kucyi A, Law CW, McIntyre RS. Exercise and bipolar disorder: a review of neurobiological mediators. Neuromolecular Med. 2009;11(4):328–336. doi: 10.1007/s12017-009-8079-9. [DOI] [PubMed] [Google Scholar]
- 56.Kucyi A, Alsuwaidan MT, Liauw SS, McIntyre RS. Aerobic physical exercise as a possible treatment for neurocognitive dysfunction in bipolar disorder. Postgrad Med. 2010;122(6):107–116. doi: 10.3810/pgm.2010.11.2228. [DOI] [PubMed] [Google Scholar]
- 57.Bratland-Sanda S, Sundgot-Borgen J, Rø Ø, Rosenvinge JH, Hoffart A, Martinsen EW. Physical activity and exercise dependence during inpatient treatment of longstanding eating disorders: an exploratory study of excessive and non-excessive exercisers. Int J Eat Disord. 2010;43(3):266–273. doi: 10.1002/eat.20769. [DOI] [PubMed] [Google Scholar]
- 58.Hrabosky JI, White MA, Masheb RM, Grilo CM. Physical activity and its correlates in treatment-seeking obese patients with binge eating disorder. Int J Eat Disord. 2007;40(1):72–76. doi: 10.1002/eat.20323. [DOI] [PubMed] [Google Scholar]
- 59.Levine MD, Marcus MD, Moulton P. Exercise in the treatment of binge eating disorder. Int J Eat Disord. 1996;19(2):171–177. doi: 10.1002/(SICI)1098-108X(199603)19:2<171::AID-EAT7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 60.Pendleton VR, Goodrick GK, Poston WS, Reeves RS, Foreyt JP. Exercise augments the effects of cognitive-behavioral therapy in the treatment of binge eating. Int J Eat Disord. 2002;31(2):172–184. doi: 10.1002/eat.10010. [DOI] [PubMed] [Google Scholar]
- 61.Plante TG. Could the perception of fitness account for many of the mental and physical health benefits of exercise? Adv Mind Body Med. 1999;15(4):291–295. doi: 10.1054/ambm.1999.0082. [DOI] [PubMed] [Google Scholar]
- 62.Sundgot-Borgen J, Rosenvinge JH, Bahr R, Schneider LS. The effect of exercise, cognitive therapy, and nutritional counseling in treating bulimia nervosa. Med Sci Sports Exerc. 2002;34(2):190–195. doi: 10.1097/00005768-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 63.Zunker C, Mitchell JE, Wonderlich SA. Exercise interventions for women with anorexia nervosa: a review of the literature. Int J Eat Disord. 2011;44(7):579–584. doi: 10.1002/eat.20862. [DOI] [PubMed] [Google Scholar]
- 64.Del Valle MF, Pérez M, Santana-Sosa E, Fiuza-Luces C, Bustamante-Ara N, Gallardo C, et al. Does resistance training improve the functional capacity and well being of very young anorexic patients? A randomized controlled trial. J Adolesc Health. 2010;46(4):352–358. doi: 10.1016/j.jadohealth.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 65.Ussher MH, Taylor A, Faulkner G. Exercise interventions for smoking cessation. Cochrane Database Syst Rev. 2008;(4):CD002295. doi: 10.1002/14651858.CD002295.pub3. [DOI] [PubMed] [Google Scholar]
- 66.Zschucke E, Heinz A, Ströhle A. Exercise and physical activity in the therapy of substance use disorders. ScientificWorldJournal. 2012;2012:901741. doi: 10.1100/2012/901741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith MA, Lynch WJ. Exercise as a potential treatment for drug abuse: evidence from preclinical studies. Front Psychiatry. 2011;2:82. doi: 10.3389/fpsyt.2011.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Beebe LH, Tian L, Morris N, Goodwin A, Allen SS, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues Ment Health Nurs. 2005;26(6):661–676. doi: 10.1080/01612840590959551. [DOI] [PubMed] [Google Scholar]
- 69.Marzolini S, Jensen B, Melvielle P. Feasibility and effects of a group-based resistance and aerobic exercise program for individuals with schizophrenia: a multidisciplinary approach. Ment Health Phys Act. 2009;2(1):29–36. [Google Scholar]
- 70.Acil AA, Dogan S, Dogan O. The effects of physical exercises to mental state and quality of life in patients with schizophrenia. J Psychiatr Ment Health Nurs. 2008;15(10):808–815. doi: 10.1111/j.1365-2850.2008.01317.x. [DOI] [PubMed] [Google Scholar]
- 71.Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67(2):133–143. doi: 10.1001/archgenpsychiatry.2009.193. [DOI] [PubMed] [Google Scholar]
- 72.Vancampfort D, Vansteelandt K, Scheewe T, Probst M, Knapen J, De Herdt A, et al. Yoga in schizophrenia: a systematic review of randomised controlled trials. Acta Psychiatr Scand. 2012;126(1):12–20. doi: 10.1111/j.1600-0447.2012.01865.x. [DOI] [PubMed] [Google Scholar]
- 73.Vancampfort D, De Hert M, Knapen J, Wampers M, Demunter H, Deckx S, et al. State anxiety, psychological stress and positive well-being responses to yoga and aerobic exercise in people with schizophrenia: a pilot study. Disabil Rehabil. 2011;33(8):684–689. doi: 10.3109/09638288.2010.509458. [DOI] [PubMed] [Google Scholar]
- 74.Hamer M, Chida Y. Physical activity and risk of neurodegenerative disease: a systematic review of prospective evidence. Psychol Med. 2009;39(1):3–11. doi: 10.1017/S0033291708003681. [DOI] [PubMed] [Google Scholar]
- 75.Heyn PC, Johnson KE, Kramer AF. Endurance and strength training outcomes on cognitively impaired and cognitively intact older adults: a meta-analysis. J Nutr Health Aging. 2008;12(6):401–409. doi: 10.1007/BF02982674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Denkinger MD, Nikolaus T, Denkinger C, Lukas A. Physical activity for the prevention of cognitive decline: current evidence from observational and controlled studies. Z Gerontol Geriatr. 2012;45(1):11–16. doi: 10.1007/s00391-011-0262-6. [DOI] [PubMed] [Google Scholar]
- 77.Van Uffelen JG, Chin A Paw MJ, Hopman-Rock M, van Mechelen W. The effect of walking and vitamin B supplementation on quality of life in community-dwelling adults with mild cognitive impairment: a randomized, controlled trial. Qual Life Res. 2007;16(7):1137–1146. doi: 10.1007/s11136-007-9219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Friedman R, Tappen RM. The effect of planned walking on communication in Alzheimer's disease. J Am Geriatr Soc. 1991;39(7):650–654. doi: 10.1111/j.1532-5415.1991.tb03617.x. [DOI] [PubMed] [Google Scholar]
- 79.Van de Winckel A, Feys H, De Weerdt W, Dom R. Cognitive and behavioural effects of music-based exercises in patients with dementia. Clin Rehabil. 2004;18(3):253–260. doi: 10.1191/0269215504cr750oa. [DOI] [PubMed] [Google Scholar]
- 80.Holliman DC, Orgassa UC, Forney JP. Developing an interactive physical activity group in a geriatric psychiatry facility. Act Adapt Aging. 2001;26(1):57–69. [Google Scholar]
- 81.Kemoun G, Thibaud M, Roumagne N, Carette P, Albinet C, Toussaint L, et al. Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord. 2010;29(2):109–114. doi: 10.1159/000272435. [DOI] [PubMed] [Google Scholar]
- 82.Rolland Y, Pillard F, Klapouszczak A, Reynish E, Thomas D, Andrieu S, et al. Exercise program for nursing home residents with Alzheimer's disease: a 1-year randomized, controlled trial. J Am Geriatr Soc. 2007;55(2):158–165. doi: 10.1111/j.1532-5415.2007.01035.x. [DOI] [PubMed] [Google Scholar]
- 83.Santana-Sosa E, Barriopedro MI, López-Mojares LM, Pérez M, Lucia A. Exercise training is beneficial for Alzheimer's patients. Int J Sports Med. 2008;29(10):845–850. doi: 10.1055/s-2008-1038432. [DOI] [PubMed] [Google Scholar]
- 84.Stevens J, Killeen M. A randomised controlled trial testing the impact of exercise on cognitive symptoms and disability of residents with dementia. Contemp Nurse. 2006;21(1):32–40. doi: 10.5172/conu.2006.21.1.32. [DOI] [PubMed] [Google Scholar]
- 85.Francese T, Sorrell J, Butler FR. The effects of regular exercise on muscle strength and functional abilities of late stage Alzheimer's residents. Am J Alzheimers Dis Other Demen. 1997;12(3):122–127. [Google Scholar]
- 86.Foster PP, Rosenblatt KP, Kuljiš RO. Exercise-induced cognitive plasticity, implications for mild cognitive impairment and Alzheimer's disease. Front Neurol. 2011;2:28. doi: 10.3389/fneur.2011.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 88.Murphy TJ, Pagano RR, Marlatt GA. Lifestyle modification with heavy alcohol drinkers: effects of aerobic exercise and meditation. Addict Behav. 1986;11(2):175–186. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- 89.Moore GF, Moore L, Murphy S. Facilitating adherence to physical activity: exercise professionals' experiences of the National Exercise Referral Scheme in Wales: a qualitative study. BMC Public Health. 2011;11:935. doi: 10.1186/1471-2458-11-935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45(5):1761–1772. doi: 10.1021/es102947t. [DOI] [PubMed] [Google Scholar]
- 91.Mailey EL, Wójcicki TR, Motl RW, Hu L, Strauser DR, Collins KD, et al. Internet-delivered physical activity intervention for college students with mental health disorders: a randomized pilot trial. Psychol Health Med. 2010;15(6):646–659. doi: 10.1080/13548506.2010.498894. [DOI] [PubMed] [Google Scholar]
- 92.Sparrow D, Gottlieb DJ, Demolles D, Fielding RA. Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(11):1251–1257. doi: 10.1093/gerona/glr138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hoffman MD, Hoffman DR. Exercisers achieve greater acute exercise-induced mood enhancement than nonexercisers. Arch Phys Med Rehabil. 2008;89(2):358–363. doi: 10.1016/j.apmr.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 94.Saeed SA, Antonacci DJ, Bloch RM. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Physician. 2010;81(8):981–986. [PubMed] [Google Scholar]
- 95.Carei TR, Fyfe-Johnson AL, Breuner CC, Brown MA. Randomized controlled clinical trial of yoga in the treatment of eating disorders. J Adolesc Health. 2010;46(4):346–351. doi: 10.1016/j.jadohealth.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bock BC, Fava JL, Gaskins R, Morrow KM, Williams DM, Jennings E, et al. Yoga as a complementary treatment for smoking cessation in women. J Womens Health (Larchmt) 2012;21(2):240–248. doi: 10.1089/jwh.2011.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Elibero A, Janse Van Rensburg K, Drobes DJ. Acute effects of aerobic exercise and Hatha yoga on craving to smoke. Nicotine Tob Res. 2011;13(11):1140–1148. doi: 10.1093/ntr/ntr163. [DOI] [PubMed] [Google Scholar]
- 98.Bodin T, Martinsen EW. Mood and self-efficacy during acute exercise in clinical depression. A randomized, controlled study. J Sport Exerc Psychol. 2004;26(4):623–633. [Google Scholar]
- 99.Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med. 2011;41(8):641–671. doi: 10.2165/11590680-000000000-00000. [DOI] [PubMed] [Google Scholar]


