Abstract
Background: Pharmacists' scope of practice has been steadily expanding across Canada to encompass clinical activities. In January 2009, pharmacists in British Columbia (BC) were given the authority to adapt prescriptions for renewals; change in dose, formulation or regimen; and therapeutic substitutions. This study evaluated the labour costs associated with pharmacy adaptation services in BC.
>Methods: Ten high-adapting pharmacies participated in the study. Through workflow observations, we measured the time incurred for adapted and nonadapted prescriptions.
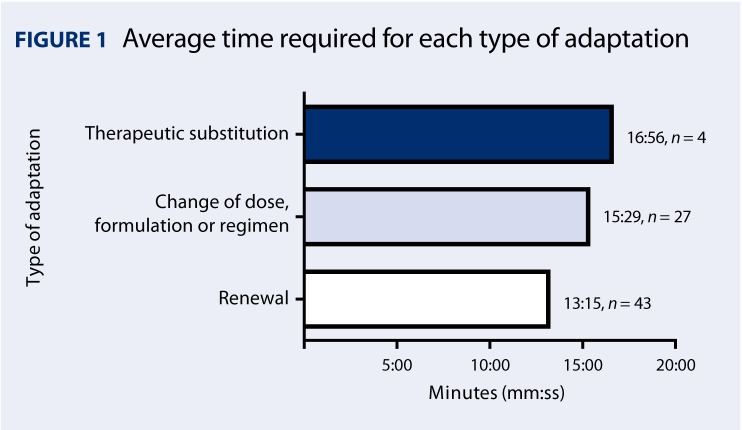
Results: We observed 91 adapted prescriptions and 1081 nonadapted prescriptions. The total average time to provide adapted prescriptions was 6:43 minutes (SD 3:50) longer than to provide nonadapted prescriptions. The total average cost of an adapted prescription was $6.10 greater than a nonadapted prescription. Renewals took the least amount of time to complete, and therapeutic substitutions took the most time to complete.
Discussion: Through workflow observations, it was determined that 10 stages of activity occur when adapting a prescription, with the most time being expended during the documentation and processing phases. Labour costs associated with adapted prescriptions were higher than for nonadapted prescriptions.
Introduction
In January 2009, pharmacists in British Columbia (BC) were given the authority to adapt prescriptions, increasing their opportunities to use their professional expertise and judgment in clinical practice.1 Through this initiative, pharmacists can renew prescriptions for long-term medications; change doses, formulations and regimens; and provide therapeutic substitutions as required to ultimately improve patient health outcomes.1 As compensation for the clinical work associated with the adaptations, pharmacists are paid a fee of $8.60 for a renewal or change and $17.20 for a therapeutic substitution, in addition to their usual dispensing fees.1
KNOWL EDGE INTO PRACTICE.
On average, it took 6:43 minutes longer to complete an adapted prescription relative to a nonadapted prescription.
The average additional cost of pharmacist and technician time required to fill an adapted prescription was $6.10.
The majority of prescription adaptations were renewals, changes to the dose or formulation and therapeutic substitutions. Only rarely were “therapeutic services” provided, despite the higher professional fee.
MIS E EN PRATIQUEDES CONNAISANCES.
L'adaptation d'une ordonnance a nécessité en moyenne 6 : 43 minutes de plus que l'exécution d'une ordonnance sans adaptation.
Le temps devant être consacré par le pharmacien et le technicien pour l'adaptation d'une ordonnance a occasionné un coût supplémentaire moyen de 6,10 $.
Dans la majorité des cas, les adaptations consistent en le renouvellement, en la modification de la dose ou de la préparation ou en le remplacement d'un produit par un autre médicament. La prestation de « services thérapeutiques » ne représente qu'une très faible proportion des cas, malgré les honoraires professionnels plus élevés.
Despite the clinical and drug-related ability of pharmacists to provide additional professional services, barriers to the uptake and provision of new services by pharmacists have been identified. One of the most consistent barriers to pharmacists' uptake of new services has been the lack of remuneration to pay pharmacists for their services.2,3 In addition, system-level barriers include the additional burden on pharmacists' time, limited remuneration models, patient apathy and limited support from physicians and other pharmacists.4 Pharmacist psyche and culture have also been proposed as barriers to practice change.4
Considering that most remuneration models that have been established for clinical pharmacy services have suffered from low uptake and limited sustainability, many considerations must be carefully weighed in the design and implementation of such a model. To ensure that new pharmacy services meet the needs of all stakeholders, including pharmacists, pharmacy owners and managers, physicians, government payers and patients, the impact of services needs to be considered. For the BC program, accurate information pertaining to the costs of providing the additional professional services is required so that the overall cost of providing these services can be estimated. Thus, the objective of this study was to determine the incremental labour costs associated with providing prescription adaptation services among high-adapting community pharmacies in BC.
Methods
Design
In a cross-sectional study, we assessed the labour costs associated with providing both nonadapted and adapted prescriptions from workflow observations in high-adapting community pharmacies, such that the incremental cost of completing an adapted prescription could be determined relative to a nonadapted prescription.
Subjects
The BC Ministry of Health Pharmaceutical Services Division provided a list of the top 100 adapting pharmacies throughout BC, stratified by month and intervention code. From this list, a purposive sample of 20 high-adapting pharmacies was identified that represented a mix of rural and urban practices.
Procedures
In order to determine the time involved by all pharmacy personnel in completing a prescription, prescription workflow was observed in participating high-adapting pharmacies. Using trained research assistants, all of whom had community pharmacy practice experience, workflow was observed for approximately 40 hours in each pharmacy. Each stage of workflow was initially conceptualized by the lead investigators and research assistants. Actual stages from adapted and nonadapted prescriptions were determined by observation. Once the stages were determined, the actual time required to complete each stage in the process of completing both adapted and nonadapted prescriptions (Table 1) was recorded using a stop-watch.
TABLE 1.
Stages for completing nonadapted vs adapted prescriptions and proportion (%) of time spent on each
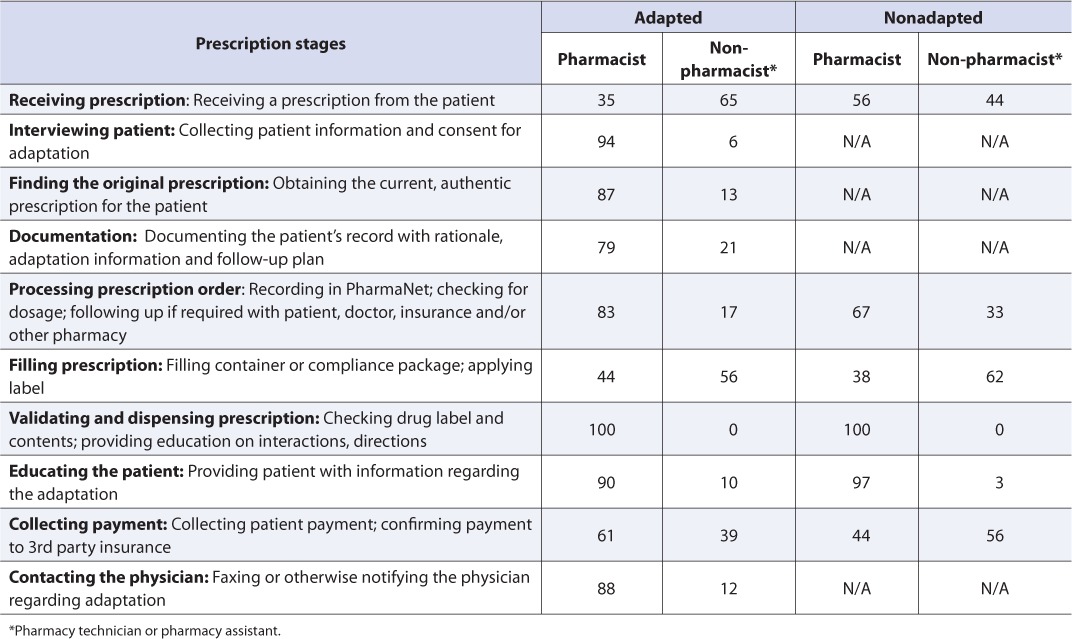
To calculate the labour costs associated with the time required by the pharmacists to complete a prescription, pharmacists' time was multiplied by the average annual pharmacist salary of $87,676 plus 19% benefits for 35.2 hours/week and 48.7 weeks/year, derived from the BC Pharmacy Association 2009 Wage and Benefits Survey.5 To calculate pharmacy technician labour costs associated with providing prescriptions, the average wage of $20.00/hour plus 19% benefits, derived from the 2009 BC Wage and Salary Survey,5 was multiplied by the time expended by the technician.
Analyses
For both adapted and nonadapted prescriptions, the average total time (min:sec) required to complete the 10 stages was assessed and the difference between each applicable stage was estimated. We stratified data by the type of adaptation (renewal; change of dose, formulation or regimen; or therapeutic substitution). For each type of adaptation, we determined the average total time required to complete the 10 stages. We assessed the incremental labour cost by calculating the difference between the average cost of completing an adapted versus a nonadapted prescription.
Results
Twenty high-adapting pharmacies were invited to participate in the workflow observation, and 10 agreed to participate, resulting in a participation rate of 50%. Five urban pharmacies (population greater than 80,000) and 5 rural pharmacies (population less than 25,000) participated in the study. From workflow observations, data on 1018 nonadapted prescriptions and 91 adapted prescriptions were recorded. Adaptations accounted for 8.2% of all prescriptions under workflow observation.
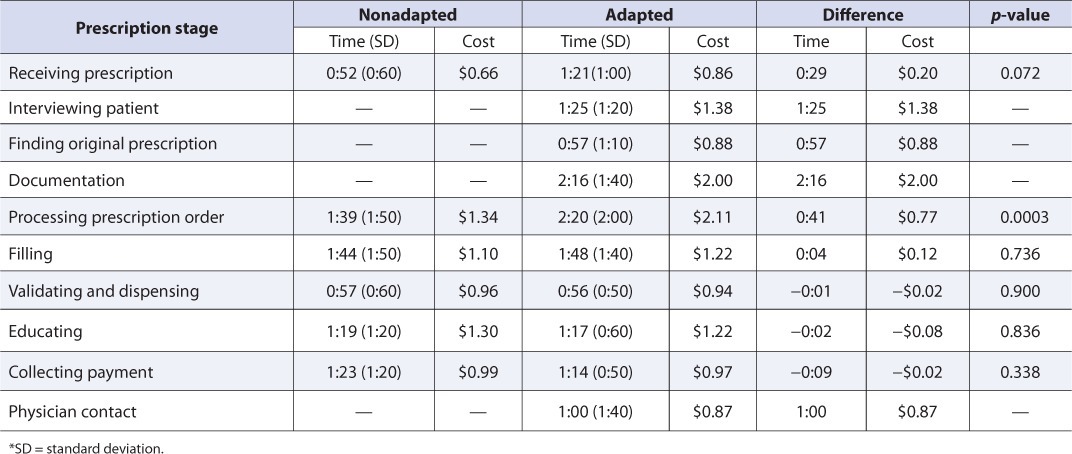
Analysis of workflow for both nonadapted and adapted prescriptions revealed that the average total time to complete the 10 stages involved in adapting a prescription was 14:39 minutes (SD 4:20), while the average total time to complete the 6 stages involved in nonadapted prescriptions was 7:56 minutes (SD 3:10). Pharmacists accounted for 70% and 64% of the total time required to complete an adapted and nonadapted prescription, respectively. These data therefore indicate that the average total time to complete an adapted prescription was 6:43 minutes (SD 3:50) longer than that to complete a nonadapted prescription. Considering pharmacist and pharmacy technician salaries and the time incurred at each prescription stage, the average labour cost to complete an adapted prescription was $12.45 versus $6.35 to complete a nonadapted prescription, translating into an incremental cost of $6.10. The proportion of the total mean labour cost attributable to the pharmacist was 70% and 53% for an adapted and nonadapted prescription, respectively.
By stage, processing an adapted prescription relative to a nonadapted prescription was found to take an average of 41 seconds longer, resulting in an average incremental cost of $0.77 (p = 0.0003). There were no other statistically significant differences across stages that were common to both adapted and nonadapted prescriptions (Table 2).
TABLE 2.
Average time (mm:ss) and cost for each stage of nonadapted vs adapted prescriptions
For adapted prescriptions specifically, the time required to complete the prescription differed by the type of adaptation (Figure 1). On average, providing a prescription renewal required 13:15 minutes (SD 3:34), whereas changing a dose, formulation or regimen required an average total time of 15:29 minutes (SD 4:38). Therapeutic substitutions required the most time (16:56 minutes; SD 6:18); however, this calculation was based on only a few observations (n = 4).
FIGURE 1.
Average time required for each type of adaptation
Discussion
We found that the average total time to complete an adapted prescription in a BC pharmacy was approximately 6:43 minutes longer than the time required to complete a nonadapted prescription. Incorporating this additional time with the average salaries for pharmacists and pharmacy technicians in BC, the total cost of providing an adapted prescription was $12.45 versus $6.35 for a nonadapted prescription, resulting in an incremental cost of $6.10 for a prescription adaptation. This is the first study to quantify both the observed workflow and the additional time and labour costs involved in the provision of professional pharmacy services. In support of our findings, both the costs and workflow observations were consistent with a prior activity-based costing study in BC.6 This study, commissioned by the BC Pharmacy Association, found that the average cost of filling a prescription was $6.62.
Given a cost of $12.45 to adapt a prescription and a fee of $8.60 for renewals and changes, it appears that pharmacies in the province need another $3.85/adaptation to break even. However, pharmacies are still paid a dispensing fee on top of the adaptation fee, which, on average, is about $9.00/prescription (ranging from $4.45 to $10.45). Therefore, there is the potential for added income for providing prescription adaption services to patients in BC. The fee for therapeutic services is much higher ($17.20/adaptation), but few of these adaptations were done during the study.
With prescription adaptation being a relatively new pharmacist-provided clinical service in Canada, there is little information on the effectiveness (i.e., impact on patient outcomes) of this service. Most evaluations have focused on supplementary prescribing in other jurisdictions such as the United Kingdom. In these other programs, barriers to implementing the new services have included workload constraints and lack of resources7,8; however, remuneration was not specifically cited as an issue. Of interest, studies have found that protocol-driven pharmacist prescribing services (such as adaptations) create extra workload for the prescriber and complicate remuneration for prescribing.8–10 Similarly, one of the few studies of the costs associated with supplementary prescribing found that in the UK, the cost (i.e., the value) of a pharmacists' time spent with each supplementary prescribing patient was approximately C$11.00; however, the authors did not evaluate these costs relative to the level of professional remuneration.10 The current study makes a valuable contribution by assessing the labour costs associated with prescription adaptation and will serve to inform the development of a new professional services remuneration agreement.
Limitations
While this study is relatively unique in its approach to program evaluation, there were some limitations. This study used observations over a 5-day period with a relatively low number of prescription adaptations being evaluated (i.e., 8.2% of all observed prescriptions). However, this proportion of adapted prescriptions is significantly greater than the proportion of adapted prescriptions in BC from January to December 2009, during which time only 0.2% of all prescriptions were adapted. In addition, therapeutic substitutions were found to account for a very small number of adapted prescriptions. This study would have benefited from workflow observations of a higher quantity of prescriptions, but due to the low rate of adaptation, a much longer time window for evaluation would have been required.
Labour costs only represent the costs associated with pharmacist and pharmacy technician salaries for providing adapted prescriptions. Capital costs or costs associated with the provision of services are described elsewhere.11 From the supplementary prescribing literature, there is a suggestion that costs associated with logistics such as intensive workloads, lack of resources and outdated computer systems are significant barriers.7,8 Further research will assess capital costs, barriers and facilitators associated with pharmacy adaptation services and physician perspectives on pharmacy adaptation services.
Conclusions
In terms of prescription workflow and labour costs, adapted prescriptions were found to cost more than nonadapted prescriptions. It would not be expected that pharmacy practice and professional activities would differ significantly among different geographic areas in Canada; thus, these results should be generally applicable to other Canadian jurisdictions as they develop remuneration structures. In a review of remuneration strategies, Chan et al.3 recommended that for clinical services a payment schedule should provide adequate remuneration commensurate with the value of service provided. For prescription adaptation, the cited benefits of this service for patients included the following: 1) optimizing drug therapy for improved patient health outcomes; 2) promoting efficiencies in the health care system; 3) expanding opportunities to identify people with significant risk factors; and 4) encouraging collaboration among health care providers.1 Thus, the results of this study may be helpful in developing policies for reimbursement of professional pharmacy services.
References
- 1.College of Pharmacists of British Columbia. Professional practice policy #58: Orientation guide. Medication management (adapting a prescription) Vancouver (BC): College of Pharmacists of British Columbia; 2008. Available: www.bcpharmacists.org/library/D-Legislation_Standards/D-2_Provincial_Legislation/1017-PPP58_OrientationGuide.pdf (accessed October 10, 2009) [Google Scholar]
- 2.Bernsten C, Andersson K, Gariepy Y, et al. A comparative analysis of remuneration models for pharmaceutical professional services. Health Policy. 2010;95(1):1–9. doi: 10.1016/j.healthpol.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Chan P, Grindrod KA, Bougher D, et al. A systematic review of remuneration systems for clinical pharmacy care services. Can Pharm J. 2008;141(2):102–12. [Google Scholar]
- 4.Rosenthal M, Austin Z, Tsuyuki RT. Are pharmacists the ultimate barrier to pharmacy practice change? Can Pharm J. 2010;143(1):37–42. [Google Scholar]
- 5.British Columbia Pharmacy Association. BCPhA 2009 wage and benefits survey. Vancouver (BC): BC Pharmacy Association; 2009. [Google Scholar]
- 6.Canadian Association of Chain Drug Stores. Activity based costing study. Final report: Study findings and analysis. Toronto (ON): Canadian Association of Chain Drug Stores; 2007. Available: http://workbench.cacds.asitechinc.com/lib/db2file.asp?file=142 (accessed October 10, 2009) [Google Scholar]
- 7.Lloyd F, Parsons C, Hughes CM. It's showed me the skills that he has: pharmacists' and mentors' views on supplementary prescribing. Int J Pharm Pract. 2010;18(1):29–36. doi: 10.1211/ijpp.18.01.0006. [DOI] [PubMed] [Google Scholar]
- 8.Tulley MP, Latif S, Cantrill JA, et al. Pharmacists' changing views of their supplementary authority. Pharm World Sci. 2007;29:628–34. doi: 10.1007/s11096-007-9114-2. [DOI] [PubMed] [Google Scholar]
- 9.Emmerton L, Marriott J, Bessell T, et al. Pharmacists and prescribing rights: review of international developments. J Pharm Pharmaceut Sci. 2005;8(2):217–25. [PubMed] [Google Scholar]
- 10.Bissell P, Cooper R, Guillaume L, et al. An evaluation of supplementary prescribing in nursing and pharmacy. Sheffield (UK): University of Sheffield; 2008. Available: www.sheffield.ac.uk/content/1/c6/09/11/83/Supplementary_prescribing.pdf (accessed June 8, 2010) [Google Scholar]
- 11.Grindrod KA, Lynd LD, Joshi P, et al. Pharmacy owner and manager perceptions of pharmacy adaptation services in British Columbia. Can Pharm J. 2011;144:231–5. doi: 10.3821/145.2.cpj78. [DOI] [PMC free article] [PubMed] [Google Scholar]