Introduction
Nearly 25% of Canadians have either diabetes or prediabetes, with diabetes-associated health care costs reaching $12.2 billion in 2010.1 It has been reported that glycemic control in primary care is poor. Harris and colleagues2 conducted a study across the 10 provinces of Canada to assess the quality of care and treatment of type 2 diabetes patients in primary care settings. They reported that almost half of the patients with type 2 diabetes in primary care settings did not achieve their glycemic target (HbA1c ≤7%).2 Poor glycemic control puts diabetes patients at high risk of suffering from diabetes complications.3 Glycemic control testing plays an essential role not only in diabetes diagnosis,4 but it is also considered the first step in diabetes management.2 There are 3 different ways to measure glycemic control:
Fasting plasma glucose (FPG)
Oral glucose tolerance test (OGTT), in which the blood glucose concentration is measured 2 hours after taking a glucose solution (75 g anhydrous glucose dissolved in water)
Glycated hemoglobin (HbA1c) (the 2008 Canadian Diabetes Association Guidelines recommend diabetes patients to have HbA1c ≤7%)4
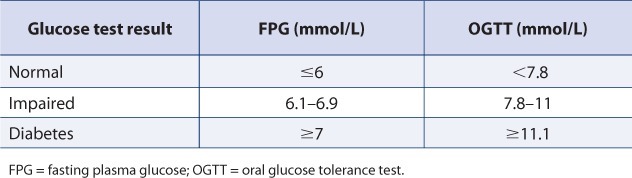
According to the results of FPG or OGTT measurements, individuals can be classified as outlined in Table 1.
TABLE 1.
Glucose test results classification4
Despite proving that they can deliver effective screenings and interventions in chronic diseases5–7 and being located in the heart of the community, there are no published studies to date that focus on community pharmacists identifying the level of glycemic control in the community — an important first step towards improving care. As such, the primary objective of the present study was to determine the level of glycemic control in community-dwelling patients with type 2 diabetes.
Methods
We engaged 10 community pharmacies from across Alberta to participate in the study. Using medication databases, pharmacists systematically identified patients who were receiving oral hypoglycemic agents and/or insulin. Potential participants were invited to measure HbA1c in the pharmacy. Ethics approval was obtained from the Health Research Ethics Board of the University of Alberta.
HbA1c was measured in the pharmacies using DCA Vantage (Siemens, Tarrytown, New York, USA), a point-of-care device. While waiting for the HbA1c result, pharmacists measured the patient's height, weight and waist circumference. After getting the results, pharmacists explained the measurements to the patients and provided them with Canadian Diabetes Association (CDA) educational material outlining diabetes self-care and management (available at www.diabetes.ca). Participants' current diabetes treatment and their willingness to use insulin were also recorded.
In the current study, HbA1c target was defined as ≤7% (the target recommended by CDA Guidelines, 2008).4
Results
A total of 200 adults with type 2 diabetes participated in our study. More than half of the participants were male (56.5%). Average age was 65 years (standard deviation [SD] 11), with 70% over the age of 60. Average body mass index (BMI) was 32 kg/m2 (SD 8) and waist circumference was 111 cm (SD 20), with 12% and 18% having normal BMI or waist circumference, respectively.
The most widely used oral agent (alone or in combination) was metformin (90.5%), followed by sulfonylurea agents (30.5%) and thiazolidinediones (17.5%). Half of the participants (50%) were receiving 2 or more oral agents, while 15.5% were using insulin alone or in combination.
A total of 41.5% of the participants were not at their HbA1c target (HbA1c ≤ 7%), and 60% of those who were not at target were receiving 2 or more medications. About three-quarters (72%) of non-insulin users reported that they would be willing to use insulin if it were prescribed to them.
Discussion
We showed that glycemic control in medically treated, community-dwelling patients with type 2 diabetes is poor. Over half of the patients who were receiving 2 or more diabetes medications were not at the recommended HbA1c target. The community pharmacy setting was a feasible and convenient venue to conduct assessments of glycemic control.
The finding that glycemic control is poor is consistent with the findings of Harris and colleagues,2 who reported that almost half of the patients with type 2 diabetes at primary care settings across Canada did not achieve their glycemic target.
The findings of our study indicate that community pharmacies provide an ideal venue to systematically identify poorly controlled patients with diabetes. Patients see their pharmacists more frequently than they see their physicians.8 Pharmacists can initiate or adjust the patient's treatment (or make recommendations towards this), identify poor adherence and lifestyle problems9 and answer patients' questions. Importantly, there is high-level evidence that pharmacist care improves patient outcomes.10
Those participants who were not at their HbA1c target might also have benefited from adding intermediate or long-acting insulin instead of adding more oral agents. The INSIGHT study demonstrated that adding long-acting insulin to 0, 1 or 2 oral agents will help to achieve lower HbA1c levels.11 The Canadian Diabetes Guidelines also highlighted the benefits of insulin in helping achieving lower HbA1c.4
The fact that participants were invited to measure their HbA1c in the pharmacy could have introduced volunteer bias; however, despite this, almost half of participants did not meet their HbA1c targets. This means that glycemic control in community-dwelling type 2 diabetes patients may be even worse than what was observed.
Conclusion
Glycemic control in treated community-dwelling patients with type 2 diabetes is poor. Community pharmacies represent an excellent venue where poorly controlled patients can be identified. Community pharmacists are highly accessible and indeed, there is good evidence to prove the benefits of their care in diabetes. Furthermore, Alberta pharmacists' recent acquisition of independent prescribing means they are now especially poised to help in the fight against diabetes. (In provinces where they do not have the authority to prescribe, pharmacists can help in the fight against diabetes by making recommendations to alter or change the treatment in order to improve the patient's glycemic control.12) To this end, we have recently begun a trial of pharmacist prescribing of insulin glargine in patients with poorly controlled type 2 diabetes — Pharmacist Intervention for Glycemic Control in the Community (the RxING study).
Acknowledgments
The authors would like to acknowledge the efforts of Candace Necyk, BSc(Pharm) and participation of the following pharmacies and pharmacists in making this study possible: Safeway Pharmacy (Rami Chowaniec, Rita Bowron, Carol Wei, Nicole Bredo, Sheilah Kostecki, Nader Hammoud), Medicine Shoppe (Jasbir Bhui) and Turtle Mountain Pharmacy (Darsey Milford).
Footnotes
Financial acknowledgements: The authors acknowledge the unrestricted investigator-initiated funding provided by Sanofi-aventis Canada and the testing equipment provided by ManthaMed.
References
- 1.Canadian Diabetes Association. 2010. The harsh reality — diabetes is a global pandemic. Available: www.diabetes.ca/diabetes-awareness-month/harsh-reality-of-diabetes/ (accessed May, 2011) [Google Scholar]
- 2.Harris SB, Ekoé JM, Zdanowicz Y, Webster-Bogaert S. Glycemic control and morbidity in the Canadian primary care setting (results of the diabetes in Canada evaluation study) Diabetes Res Clin Pract. 2005;70:90–7. doi: 10.1016/j.diabres.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. Available: www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf (accessed June 2011) [Google Scholar]
- 4.Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32(suppl 1):S1–S201. doi: 10.1016/j.jcjd.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Tsuyuki RT, Johnson JA, Teo KK, et al. A randomized trial of the effect of community pharmacist intervention on cholesterol risk management: the Study of Cardiovascular Risk Intervention by Pharmacists (SCRIP) Arch Intern Med. 2002;162:1149–55. doi: 10.1001/archinte.162.10.1149. [DOI] [PubMed] [Google Scholar]
- 6.McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists – Hypertension (SCRIP-HTN) Arch Intern Med. 2008;168:2355–61. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 7.Martinez Pérez SR, Armando PD, Molina Guerra AC, et al. Relationship between cardiovascular risk factors and high blood pressure by community pharmacists in Spain. Pharm World Sci. 2009;31:406–12. doi: 10.1007/s11096-008-9267-7. [DOI] [PubMed] [Google Scholar]
- 8.Shiu JR, Simpson SH, Johnson JA, et al. Quantifying opportunities to affect diabetes management in the community. Can Pharm J. 2006;139:37–8. [Google Scholar]
- 9.Canadian Pharmacists Association. 2007. CPhA position statement on pharmacist prescribing. Available: www.pharmacists.ca/content/about_cpha/who_we_are/policy_position/pdf/CPhA%20position%20statement%20Pharmacist%20Prescribing%20Final2%20August%2007.pdf (accessed June 2011) [Google Scholar]
- 10.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28:421–36. doi: 10.1592/phco.28.4.421. [DOI] [PubMed] [Google Scholar]
- 11.Gerstein HC, Yale JF, Harris SB, et al. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT study. Diabet Med. 2006;23:736–42. doi: 10.1111/j.1464-5491.2006.01881.x. [DOI] [PubMed] [Google Scholar]
- 12.Law MR, Ma T, Fisher J, et al. Independent pharmacist prescribing in Canada. Can Pharm J. 2012;145:17–23. doi: 10.3821/1913-701X-145.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]


