Abstract
If pain is not treated quickly and effectively in children, it can cause long-term physical and psychological sequelae. Therefore, it is important for all health care providers to understand the importance of effective pain control in children. This article is divided into 2 parts: Part 1 reviews the pharmacotherapy of pain management in children and Part 2 will review the problems relating to the use of codeine in children, and the rationale for recommending morphine as the opioid of choice in the treatment of moderate to severe pain. There has been growing concern about codeine's lack of efficacy and increased safety concerns in its use in children. Due to the variability of codeine metabolism and unpredictable effects on efficacy and safety, The Hospital for Sick Children in Toronto, Ontario, no longer includes codeine or codeine-containing products on the regular hospital formulary and now recommends oral morphine as the agent of choice for the treatment of moderate to severe pain in children. A knowledge translation (KT) strategy was developed and implemented by the hospital's Pain Task Force to support this practice change.
Introduction
Pain is defined by the International Association for the Study of Pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1 Acute pain is one of the most common adverse stimuli experienced by children, occurring as a result of injury, illness and medical procedures.2 If a child's pain is not treated quickly and effectively, it can have long-term physical and psychological sequelae.3 Long-term consequences may include anticipatory anxiety during future procedures, a lowering of the pain threshold and sensitization to future pain, reduced effectiveness of analgesics and increased analgesic requirements subsequently.4 Taddio et al.5 demonstrated that infants who were circumcised without any form of anesthetic or analgesia had a much lower pain threshold when pain was assessed months later. Hence, it is essential for all health care providers to understand the importance of effectively managing a child's pain quickly to minimize potential long-term consequences.
KNOWLEDGE INTO PRACTICE.
It is important for pharmacists to understand some of the misconceptions that prevent children from receiving adequate pain control, as well as some of the nonpharmacological and pharmacological strategies used to treat pain in children.
While codeine is one of the most common oral opioid analogs used in the treatment of mild to moderate pain in both adults and children, there is growing concern about the safety of its use in children.
MISE EN PRATIQUE DES CONNAISSANCES.
Il est important pour les pharmaciens de comprendre certaines des idées fausses qui nuisent à la gestion de la douleur chez les enfants, ainsi que certaines des stratégies non pharmacologiques et pharmacologiques utilisées pour traiter la douleur chez les enfants.
Bien que la codéine soit un des analogues opioïdes oraux les plus communs pour le traitement de douleurs modérées ou graves chez les adultes et les enfants, on se préoccupe de plus en plus de l'innocuité de son utilisation chez les enfants.
Until a short time ago, there were many misconceptions that prevented children from receiving adequate pain control. Some of these misconceptions include beliefs that infants do not feel pain,6 that children suffer less pain than adults7 or that children can become addicted to opioids more easily than adults.3 In addition, pain assessment is challenging in pediatrics, as infants and young children are not able to adequately verbalize pain. As a result, children have been under-treated for pain compared to adults.8 Recent advances in the research of pain in children have made significant contribution to the understanding of pain perception in children. We now know that the anatomical, physiological and biochemical mechanics needed for pain perception are present early in intrauterine life.3 In fact, preterm infants can perceive pain in a way comparable to older children.9
Well-managed pain is associated with faster recoveries, fewer complications and decreased health care resources.10 Yet optimal pain management practices have not been realized for hospitalized children despite the growth in pediatric pain research and the plethora of evidence-based pain management standards and guidelines recommended by local, national and international professional organizations such as the American Academy of Pediatrics, the Canadian Pediatric Society, the Joint Commission on Accreditation of Healthcare Organizations and the Canadian Pain Society.
The purpose of this article is to review pharmacotherapy in the management of pain in children (Part 1), with specific reference to the problems with codeine, the rationale behind why our organization now recommends morphine as the opioid of choice in the treatment of moderate to severe pain and how this practice change was supported by a knowledge translation (KT) strategy (Part 2). Part 2 of this article will appear in the next issue of CPJ.
Assessment of pain in children
Pain assessment is an important part of pain management. To adequately assess a child's response to treatment, it is necessary to have ongoing assessment of the child's pain.2 Because pain is a subjective experience, individual self-reporting is the preferred method for assessing pain. However, for children who cannot communicate this information due to age or developmental status, observational and behavourial assessment tools are acceptable alternatives when valid self-report is not available.2 Depending on the age of the child and his/her ability to communicate the information to the health care provider, there are many reliable, valid and clinically sensitive assessment tools available for use.2 At The Hospital for Sick Children (SickKids) in Toronto, Ontario, several different assessment tools are used, depending on the child's age and developmental status (see Appendix 1 for an algorithm of pain assessment and management of the child). For young infants, there are 2 pain assessment tools commonly used at SickKids.11 One scale is the Premature Infant Pain Profile (PIPP), which consists of 3 behavioural (facial actions: brow bulge, eye squeeze and nasolabial furrow) and 2 physiological (heart rate and oxygen saturation) indicators, and 2 contextual (gestational age and behavioural state) variables that modify pain.12 PIPP was developed 13 years ago and continues to be a reliable and valid measure of acute pain in infants.12 The other scale is the Face, Legs, Activity, Cry and Consolability (FLACC) scale, which incorporates 5 pain behaviours that make up the scale's name: facial expression, leg movement, activity, cry and consolability.13,14 Each behaviour is scored from 0 to 2, with the highest possible cumulative score being 10 (most pain).13,14 For school-aged children and adolescents (4–12 years of age), several tools can be used to report pain.15 In younger children, developmental capabilities may hinder the use of purely numeric scales and therefore pictorialbased pain scales such as the Faces Pain Scale- Revised is used.11,15 The child is asked to select 1 of 6 neutral faces that accurately reflect their pain, which is scored from 0 to 10.16 Older children (>8 years of age) who are able to understand abstract concepts can use the visual analog scale (VAS) and 0 to 10 Numeric Rating Scale (NRS).11,15 The VAS uses either a vertical or horizontal premeasured line (100 mm) to estimate pain.15 The ends of the lines represent the 2 extremes of pain (“no pain” to “worst pain”).15 It may include a numerical representation along the line.15 The child makes a mark on the line to indicate his/her level of pain. The pain score is calculated by measuring the distance from the left end point of the scale to the child's mark.15 The NRS does not include any lines, but is administered as a script asking the child to rate his/her pain from 0 to 10, with 0 being no pain and 10 being the worst pain.11
Nonpharmacological strategies for pain management
Nonpharmacological measures can be used as an adjunct therapy in the management of pain in both adults and children. Nonpharmacological strategies such as physical and psychological comfort measures are useful in conjunction with pharmacological options to help lower levels of anxiety, distress and pain.2,11 Some physical comfort measures include the use of massage or heat and/or cold compresses, applying pressure or vibration and repositioning.11 Psychological comfort measures include use of imagery, distraction and relaxation techniques.2,11
Pharmacotherapy in the management of pain
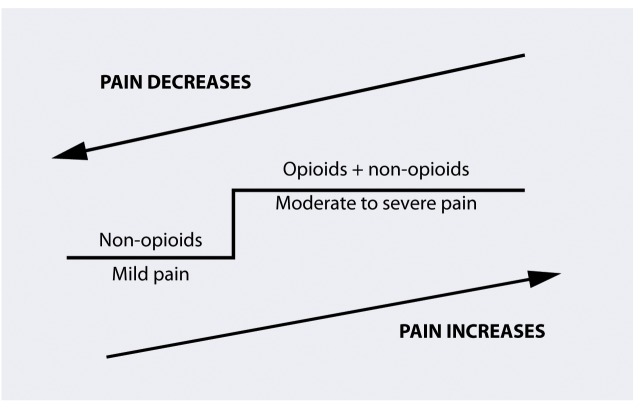
Over the past 2 decades, pain assessment and management in children has improved, due to the development of age-appropriate pain assessment tools and a better understanding of the role of analgesics in children.10,17 The most common analgesic agents used in the management of pain in both adults and children are opioids and non-opioids. Non-opioids and opioids are used in a “step-wise” approach depending on the severity of pain. The World Health Organization (WHO) has developed a tool to guide clinicians in selecting the appropriate analgesic agent (Figure 1). The WHO analgesic ladder18 was originally devised for the management of cancer pain in adults, but it can be easily adapted to managing any type of pain, including in children.
FIGURE 1.
Adaptation of the WHO Analgesic Ladder18
Non-opioid agents such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are the most common drugs used for the treatment of mild pain in both adults and children. However, compared to opioids, non-opioids have a relatively low analgesic potency and a ceiling effect may be observed.19 Therefore, non-opioids are frequently combined with an opioid to provide balanced multimodal analgesia to treat moderate to severe pain.17 When non-opioids are used in combination with opioids, they can exert an “opioid-sparing” effect by reducing the dose of opioid needed by up to 30%.19 With this combination, the patient may experience fewer adverse effects than with either analgesic alone.17
For the treatment of moderate to severe pain in both adults and children, opioids remain the agent of choice. Opioids work primarily in the central nervous system through the mu receptors.3 Over the years, many opioid analogs have been developed, including codeine, morphine, hydromorphone and oxycodone. Codeine is one of the most common oral opioid analogs used in the treatment of mild to moderate pain in both adults and children. Codeine can be given as a single agent or in combination with a non-opioid such as acetaminophen. Codeine is also available in many dosage forms, including oral liquids, which make the administration of codeine easier in children. However, there is growing concern about the safety of codeine use in children. There have been several case reports in the literature of morphine intoxication in children due to the use of codeine. Part 2 of this article will review codeine's questionable efficacy, as well as safety concerns about the use of codeine in children and the rationale for The Hospital for Sick Children in Toronto to recommend oral morphine as the opioid of choice in the treatment of moderate to severe pain.
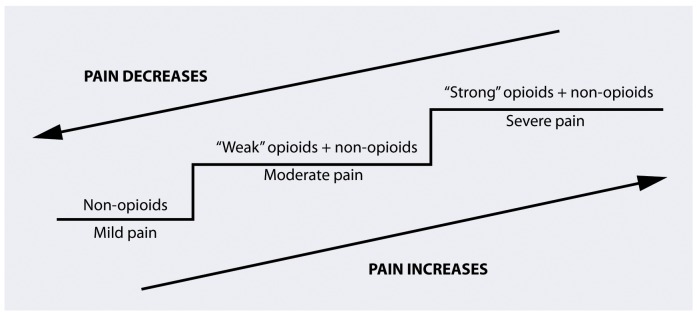
FIGURE 2.
Modified version of the WHO Analgesic Ladder used at The Hospital for Sick Children
References
- 1.International Association for the Study of Pain. Subcommittee on taxonomy. Pain terms: a list with definitions and notes on usage. Pain. 1979;6:249–52. [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108:793–7. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 3.Cunliffe M, Roberts SA. Pain management in children. Curr Anaesth Crit Care. 2004;15:272–83. [Google Scholar]
- 4.Taddio A, Chambers CT, Halperin SA, et al. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31(Suppl 2):S152–67. doi: 10.1016/j.clinthera.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 5.Taddio A, Goldbach M, Ipp M, et al. Effect of neonatal circumcision on pain responses during vaccination in boys. Lancet. 1995;345:291–2. doi: 10.1016/s0140-6736(95)90278-3. [DOI] [PubMed] [Google Scholar]
- 6.Purcell-Jones, Dorman F, Summer E. Paediatric anaesthetists' perceptions of neonatal and infant pain. Pain. 1988;33:181–7. doi: 10.1016/0304-3959(88)90089-9. [DOI] [PubMed] [Google Scholar]
- 7.Mather L, Mackie J. The incidence of postoperative pain in children. Pain. 1983;15:271–82. doi: 10.1016/0304-3959(83)90062-3. [DOI] [PubMed] [Google Scholar]
- 8.Beyer JE, DeGood DE, Ashley LC, et al. Patterns of postoperative analgesic use with adults and children following cardiac surgery. Pain. 1983;17:71–81. doi: 10.1016/0304-3959(83)90129-X. [DOI] [PubMed] [Google Scholar]
- 9.Anand KJ, Sippell WG, Aynsley-Green A. Randomized trial of fentanyl anaesthetic in preterm neonates undergoing surgery: effects on the stress response. Lancet. 1987;1:243–8. doi: 10.1016/s0140-6736(87)90065-1. [DOI] [PubMed] [Google Scholar]
- 10.Dufault MA, Sullivan M. A collaborative research utilization approach to evaluate the effects of pain management standards on patient outcomes. J Prof Nurs. 2000;16:240–50. doi: 10.1053/jpnu.2000.4593. [DOI] [PubMed] [Google Scholar]
- 11.Campbell F, Palozzi L, Jeavons M, et al. Pain management. In: Brown S, Daneman D, Dodds A, editors. Policies & procedure database. Clinical practice guideline. Toronto (ON): The Hospital for Sick Children; 2008. et al., editors. [Google Scholar]
- 12.Stevens B, Johnston C, Taddio A, et al. The premature infant pain profile: evaluation 13 years after development. Clin J Pain. 2010;26:813–30. doi: 10.1097/AJP.0b013e3181ed1070. [DOI] [PubMed] [Google Scholar]
- 13.Merkel SI, Shayevitz JR, Voepel-Lewis T, et al. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23:293–7. [PubMed] [Google Scholar]
- 14.Manworren RC, Hynan LS. Clinical validation of FLACC: preverbal patient pain scale. Pediatr Nurs. 2003;29:140–6. [PubMed] [Google Scholar]
- 15.Drendel AL, Kelly BT, Ali S. Pain assessment for children: overcoming challenges and optimizing care. Pediatr Emerg Care. 2011;27:773–81. doi: 10.1097/PEC.0b013e31822877f7. [DOI] [PubMed] [Google Scholar]
- 16.Hicks C, von Baeyer C, Spafford P, et al. The Faces Pain Scale – Revised: toward a common metric in pediatric pain measurement. Pain. 2001;93:173–83. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 17.Matthews ML. Management of postoperative pain in children. US Pharm. 2008;33:HS10–5. [Google Scholar]
- 18.World Health Organization. Cancer Pain Relief. Geneva: WHO; 1986. pp. 18–19. [Google Scholar]
- 19.Morton NS. Management of postoperative pain in children. Arch Dis Child Educ Pract Ed. 2007;92:ep14–9. doi: 10.1136/adc.2004.070888. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.