Abstract
Practitioner-level educational approaches that promote screening and brief intervention (SBI) seldom consider providers’ profession and medical specialization. Strategies that consider these variables may be better equipped to affect change in beliefs and behavior. The aim of this study was to identify beliefs that predict stated likelihood of practicing SBI by specialty and health profession in order to guide the direction of educational strategies. Physicians and nurse practitioners were studied that specialized in family, internal, obstetric gynecology (ObGyn), and pediatric medicine. The results indicated that independent of amount of previous postgraduate alcohol education and knowledge, self-rated competence mediated between specialty and likelihood of practicing SBI. For instance, low self-rated competence for ObGyn was a barrier that suppressed likelihood of practicing SBI. Other findings were that role legitimacy mediated the association between profession and likelihood of SBI, so that lack of role legitimacy was a barrier for physicians but not for nurse practitioners. We suggest that targeted educational strategies for ObGyn and pediatric clinicians may prove more effective than the prevalent one-size-fits all approaches aimed at general adult populations.
Keywords: alcohol screening and brief intervention, physicians, nurse practitioners, attitudinal barriers, education
INTRODUCTION
Attention to educating medical clinicians in screening and brief intervention (SBI) is important because alcohol-related mortality is a significant public health problem accounting for approximately 1 in every 20 deaths in the United States (1). During the course of ongoing care, primary care practitioners have valuable opportunities to recognize and intervene with patients that are drinking in a way that poses harm to themselves or others. Although educators have had success in shaping the beliefs and behaviors of health professionals toward alcohol-related services (2–5), the practice of SBI in primary care settings is far from routine (6–14). El-Guebaly et al. (15) suggest that problems with educational efforts include difficulty with recruitment to CME courses (16,17), little rationale for the selection of interventions aside from available resources, and little attention to differences between specialty groups. One strategy to address these concerns may be to design practitioner-level education to target specific groups of clinicians. Programs that cater to provider’s professional backgrounds and views may be better equipped to affect SBI practices. However, to move beyond one-size-fits all approaches to educating primary care providers, we need more understanding of the beliefs and inclinations toward SBI that different professionals bring to their work.
Past studies suggest that health professionals’ perceptions of themselves and their patients with alcohol problems are influential in determining the rate of screening and brief intervention. These perceptions include but are not limited to confidence in their ability to identify and respond to alcohol problems (18–22), time available for such activities (23–25); ambiguity about such services as part of their responsibility (23, 26–29); lack of organizational support (23, 30); and pessimism about working with patients with alcohol problems (31–34). More recently, Friedmann et al. (34) observed that physicians’ views not only influenced SBI practices, but also did the physicians’ specialization predict these practices. Specifically, they found that internists and psychiatrists were more likely to screen for alcohol-related problems than were family and obstetric gynecology (ObGyn) physicians; and that compared with family physicians, ObGyn physicians were less likely and psychiatrists were more likely to attempt intervention.
Primary health care providers are important in implementing routine screening and brief intervention because they emphasize health promotion and preventive services. Managed care organizations seek primary care practitioners in order to keep patients healthy and thereby constrain the cost of care (35). A priority in managed care is to reduce risk factors, such as risky drinking, to decrease patients’ need for health services. There is broad evidence that screening and brief intervention delivered by physicians or nurse practitioners as part of a primary care visit significantly reduced alcohol consumption by high-risk drinkers (36–42). The nurse practitioner profession originated as a strategy to increase access to primary care in response to a shortage of primary care physicians (43). In the United States the most common specialties in primary care are family, internal, obstetrics, and pediatric medicine. Each specialty has unique opportunities to recognize and act in response to patients’ drinking problems (44). For instance, ObGyn specialists are the primary care providers for many women of all ages (45), and pediatric specialists caring for patients from birth to adulthood have valuable opportunities to intervene early in a patient’s life (46).
The purpose of this study is to examine 1) whether beliefs about screening and brief intervention (SBI) vary by profession (physician, nurse practitioner) and specialty group (family, internal, ObGyn, pediatrics), and 2) whether the beliefs predict stated likelihood of practicing SBI. The beliefs examined are self-rated competency, role legitimacy, satisfaction working with at-risk patients, organizational resources, skepticism about helping problem drinkers, and time concerns. Age, gender, number of patients seen per week, objective knowledge, and postgraduate alcohol education were included in the analysis because of their potential importance for understanding stated likelihood of practicing SBI.
METHOD
Procedure
In 1999, questionnaires were mailed to a random sample of licensed physicians (MDs) and nurse practitioners (NPs) in a Northern California County, whose population is approximately 1,400,000. The names and addresses of state-licensed MDs and NPs were purchased from the California Office of Consumer Affairs. The physician sample was limited to those who practiced through at least one of the region’s several managed care organizations (MCOs). Physicians working with MCOs, but not necessarily exclusively, were chosen because of their high representation in California and because of the array of primary care practitioners employed by these organizations. The sample of NPs saw patients through one of the region’s MCOs and/or one of the city, county, or state government-funded programs (Medi-Cal, Veterans Administration, etc.).
Recruitment materials included an invitation to participate and a return postcard mailed to a random sample of 500 MDs and 300 NPs. Those requesting a questionnaire received either the MD form or the NP form depending on their respective profession. Those not returning the questionnaire within 2 weeks were sent a reminder notice, then telephoned, and, if necessary, sent a follow-up mailing. Because of wrong addresses, 8 questionnaires sent to MDs and 14 sent to NPs never arrived. The response rates for completed questionnaires were therefore 136/492 = 28% for MDs and 168/286 = 59% for NPs. The low response rate compromises our ability to generalize the results, particularly for physicians. This is often the case in studies using survey methods on physicians (12, 21,47). We cannot determine the characteristics of all nonrespondents; however, 83 of them returned postcards indicating no interest or time to complete a questionnaire, and in addition, they responded to a few questions about their clinical practice. This group did not significantly differ from questionnaire recipients in hours of previous training in alcohol problems. Those who requested a questionnaire, however, reported seeing a significantly higher percentage of patients with alcohol-related problems (M = 15.3%, SD = 17.6) than did those who requested not to receive the questionnaire (M = 8.8%, SD = 8.5), F(l, 339) = 7.9, p < 0.005. It is possible that those who did not participate had less favorable attitudes toward problem drinkers, were less aware of alcohol problems in their patients, and had less time to complete the questionnaire. The study did not involve an educational intervention; therefore, we have no reason to suspect nonparticipants were especially unwilling to alter their own practices.
Measures
The self-administered questionnaire contained several items on providers’ beliefs and clinical practices regarding SBI. The questionnaire referred to at-risk drinkers as people whose alcohol use was excessive enough to possibly lead to health problems (e.g., high blood pressure, accidents) or social problems (e.g., difficulties with work). The questionnaire defined screening as asking patients about the amount of alcohol they drink and the symptoms they experience. Brief intervention was defined as stating medical concerns about a patient’s drinking and health-related risks or advising patients to cut back or stop drinking. Other questions pertained to the providers’ clinical practice, demographic characteristics, and knowledge relevant to performing SBI.
Background Variables
Age, number of patients seen per week, and postgraduate alcohol education were treated as continuous variables. Postgraduate education was coded 1 (none), 2 (<4 h), 3 (4–10 h), 4 (11–40 h), and 5 (>40 h). Gender, profession, and primary practice fields were coded as dummy variables (female = 1, nurse practitioner = 1, family medicine = 1, internal medicine = 1, ObGyn = 1, and pediatrics = 1).
Stated Likelihood of SBI Practice
One 3-item scale measured likelihood to practice SBI. The items began, “On average, how likely is it in the next 12 months,” then proceeded, “…that you will ask patients who are current drinkers about their alcohol consumption,” “…that you will state to patients your medical concerns about their drinking patterns or related health risks,” and “…that you will write in patients’ charts your medical concerns about their drinking patterns or related health risks.” Response options ranged from 1 (I do not intend) to 7 (every time). Numeric values for items were summed for a scale ranging from 3 to 21 with Cronbach’s alpha of 0.86.
Knowledge
This was measured by six multiple-choice questions pertaining to the drinking guidelines. For example, one item asked what the U.S. Government Dietary Guideline was for moderate drinking in terms of the upper limit of number of drinks per day for men, a second asked what the guideline was for women, and a third asked about circumstances when a patient should be advised to abstain from alcohol. Correct answers were summed for a scale from 0 to 6 correct answers.
Role Legitimacy Beliefs
This was measured by asking, “How often do you think your physician (nurse practitioner) colleagues screen patients for drinking problems?” and “how often do you think… [they] …state medical concerns about patients’ drinking patterns and related health risks?” Items were scored on a 4-point scale ranging from “rarely/ never” to “always.” Two other items asked, “How do you think your physician (nurse practitioner) colleagues would feel about your screening patients for drinking problems?” and “how do you think… [they] …would feel about your stating medical concerns about patients’ drinking patterns and related health risks?” The format of these items came from a formulation to measure subjective norms toward performing a behavior (48, 49). A 4-point scale applied to each item from “they would not approve” to “most of my colleagues would approve.” These items are included in Table III.
Table III.
Oblimin Rotation Factor Pattern for SBI Variables
| Item | Pattern matrix
|
|||||
|---|---|---|---|---|---|---|
| I (Competence) | II (Lack of role legitimacy) | III (Satisfaction working w/ at-risk) | IV (Organizational resources) | V (Skepticism) | VI (Time & compensation) | |
| I know what questions to aska | 0.78 | |||||
| I’m comfortable asking about drinkinga | 0.74 | |||||
| I don’t know how to identify at-risk drinkers with no obvious signs of excess | 0.65 | |||||
| I know how to effectively help patientsa | 0.71 | |||||
| I am at ease making these statementsa | 0.72 | |||||
| How often do your colleagues screen? | −0.60 | |||||
| How do you think your colleagues would feel about you screening patients? | −0.85 | |||||
| How do you think your colleagues would feel about you briefly intervening? | −0.83 | |||||
| How often do you think your colleagues intervene? | −0.68 | |||||
| It is rewarding to work with at-risk drinkersa | 0.73 | |||||
| There are no professional benefits | 0.46 | |||||
| Problem drinkers are more noncompliant | 0.68 | |||||
| My organization is without an intervention protocol | −0.67 | |||||
| The plans I contract with reimburse for alc counselinga | −0.69 | |||||
| There is no information provided for referring patients | −0.70 | |||||
| I’m not aware of a single problem drinker who cut back | −0.61 | |||||
| Advising patients to seek assistance is the best I can do | −0.61 | |||||
| I’m skeptical of behavioral medicine | −0.46 | |||||
| Given adequate information practitioners can help patients reducea | −0.72 | |||||
| There is not enough time to advise patientsa | 0.61 | |||||
| Patients would not be willing to pay for counseling | 0.60 | |||||
Items were recoded for analysis so that 1 = strongly disagree to 5 = strongly agree.
SBI Practice Beliefs
Seventeen items included in Table III assessed provider beliefs about SBI. Item content came from the alcohol health services research literature on why clinicians fail to conduct SBI. Substantive content also came from focus groups of MDs and NPs that explored the topic of SBI in the primary care setting. The items were scored on a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.”
RESULTS
Sample Characteristics
The mean age for participants was 49 years for MDs and 46 years for NPs. The majority of MDs were male (74%) and 96% of the NPs were female. Physicians were 72% White, 7% African American, 15% Asian, 4% Hispanic, and 2% Other. NPs were 83% White, 7% African American, 4% Asian, 3% Hispanic, and 3% Other. Hours of postgraduate training or continuing medical education on alcohol and alcohol-related problems varied little between professions. Twenty percent of MDs and 27% of NPs reported no education of this type at all. The largest category represented 35% of MDs and 31 % of NPs who reported less than 4 h of training. Participants represented a variety of primary fields of practice as shown in Table I. The category “Other” included a variety of specialties including behavioral medicine, gas-troenterology, cardiology, gerontology, endocrinology, opthamology, and ear, nose, and throat medicine. Respondents were instructed to indicate all primary fields of practice that apply.
Table I.
Primary Practice by Profession (in %)a
| Physicians (n = 136) | Nurse practitioners (n = 168) | |
|---|---|---|
| Family medicine | 13 | 25 |
| Internal medicine | 32 | 16 |
| Obstetrics/gynecology | 7 | 32 |
| Pediatrics | 18 | 12 |
| Surgery | 7 | 1 |
| Emergency medicine | 6 | 3 |
| Anesthesiology | 2 | 0 |
| Neurology | 3 | 1 |
| Radiology | 1 | 0 |
| Psychiatry | 5 | 3 |
| Other | 21 | 38 |
Percentages do not total 100 because participants were instructed to mark all that apply.
Bivariate Analysis
We used independent sample t tests to learn more about the background variables in relation to stated likelihood of performing SBI. The sample was divided into two groups on the basis of each dichotomous variable. Table II compares the mean scores on likelihood of practicing SBI by gender, profession, and the four specialty areas: family, internal, ObGyn, and pediatrics. Females (p < 0.02) and NPs (p < 0.00) on average stated a greater likelihood to perform SBI. In addition, family (p < 0.00) and ObGyn (p < 0.04) practitioners on average indicated a significantly greater likelihood to practice SBI than did those not in these specialties. For those in internal medicine and pediatrics the stated likelihood of performing SBI was statistically no different than those not specializing in these areas.
Table II.
Comparison of Group Means of Respondents’ Stated Likelihood of Practicing SBI
| n | Stated likelihood of practicing SBIa | t Value | Significance (2-tailed) | |
|---|---|---|---|---|
| Gender | −2.41 | 0.02 | ||
| Male | 107 | 14.5 | ||
| Female | 189 | 15.8 | ||
| Profession | −2.97 | 0.00 | ||
| Physician | 136 | 14.5 | ||
| Nurse Practitioners | 161 | 16.0 | ||
| Family | −2.82 | 0.00 | ||
| Yes | 58 | 16.5 | ||
| No | 239 | 15.0 | ||
| Internal | −0.75 | 0.45 | ||
| Yes | 67 | 15.6 | ||
| No | 230 | 15.2 | ||
| Obstetrics | −2.04 | 0.04 | ||
| Yes | 62 | 16.3 | ||
| No | 235 | 15.1 | ||
| Pediatrics | 1.04 | 0.30 | ||
| Yes | 45 | 14.6 | ||
| No | 252 | 15.5 |
Scale ranges from 3 (no intention to perform SBI) to 21 (intend to perform SBI everytime).
Factor Analysis of Belief Items
The 21 role legitimacy and SBI practice belief items were entered into an exploratory factor analysis to determine the underlying structure of items. An Oblimin rotation was used because of potential correlation between factors. Six dimensions were found that accounted for 56% of the total variance. The eigenvalues for the six factors ranged from 3.94 to 1.06. Table III shows the factor pattern matrix of the items. The factors represent competence, lack of role legitimacy, satisfaction working with at-risk drinkers, organizational resources, skepticism, and time/compensation.
Predicting Stated Likelihood of Performing SBI
We used a simultaneous equation path analysis (EQS version 5.7) to examine multivariate relationships among stated likelihood of practicing SBI, feeling competent, lack of role legitimacy, satisfaction working with at-risk drinkers, organizational resources, skepticism, time/compensation beliefs, knowledge, and background variables. Standardized factor scores from the factor analysis represented the six belief variables. Table IV is a correlation matrix of all variables in the path analysis.
Table IV.
Correlation Matrix of Research Variables
| Intent to perform SBI | Fl | F2 | F3 | F4 | F5 | F6 | Know | Age | Female | Nurse | Alcohol education | Patients/ Week | Family | Internal | ObGyn | Pediatrics | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intent to perform SBI | 1.00 | ||||||||||||||||
| Fl | 0.38** | 1.00 | |||||||||||||||
| F2 | −0.36** | −0.17* | 1.00 | ||||||||||||||
| F3 | 0.23** | 0.12 | −0.08 | 1.00 | |||||||||||||
| F4 | −0.10 | −0.12 | 0.09 | −0.12 | 1.00 | ||||||||||||
| F5 | −0.13* | −0.11 | 0.04 | −0.18** | 0.17* | 1.00 | |||||||||||
| F6 | 0.02 | 0.05 | −0.00 | 0.13* | −0.04 | −0.08 | 1.00 | ||||||||||
| Knowledge | 0.07 | 0.15* | −0.10 | 0.15* | −0.14* | −0.07 | −0.03 | 1.00 | |||||||||
| Age | −0.05 | 0.20** | −0.04 | −0.10 | −0.11 | 0.02 | 0.06 | 0.01 | 1.00 | ||||||||
| Female | 0.14* | −0.07 | −0.16* | 0.34** | −0.06 | −0.09 | 0.00 | 0.03 | −0.30** | 1.00 | |||||||
| Nurse | 0.17** | −0.05 | −0.23** | 0.34** | −0.05 | −0.05 | −0.05 | 0.03 | −0.21** | 0.74** | 1.00 | ||||||
| Alcohol education | 0.22** | 0.35** | −0.01 | 0.07 | −0.16* | −0.15* | 0.02 | 0.19** | 0.19** | −0.07 | −0.03 | 1.00 | |||||
| Patients/week | 0.02 | 0.03 | 0.04 | −0.11 | −0.00 | 0.08 | −0.03 | 0.00 | 0.06 | −0.23** | −0.30** | −0.07 | 1.00 | ||||
| Family | 0.13* | 0.15* | −0.06 | 0.04 | 0.11 | −0.06 | −0.04 | 0.03 | 0.05 | 0.10** | 0.16** | −0.04 | 0.16** | 1.00 | |||
| Internal | 0.04 | 0.20** | −0.05 | 0.06 | −0.07 | −0.05 | 0.06 | 0.13 | −0.00 | −0.17** | −0.18** | 0.13* | 0.21** | −0.21** | 1.00 | ||
| ObGyn | 0.11 | −0.15* | −0.13 | 0.11 | 0.01 | 0.05 | −0.07 | 0.05 | −0.06 | 0.26** | 0.30** | −0.07 | −0.09 | −0.11 | −0.26** | 1.00 | |
| Pediatrics | −0.07 | −0.26** | 0.05 | −0.04 | 0.07 | −0.06 | 0.04 | −0.02 | −0.09 | 0.11 | −0.08 | −0.08 | −0.00 | −0.14 | −0.19** | −0.17** | 1.00 |
p = 0.05;
p = 0.01 (2-tailed significance).
The initial model assumed competence, lack of role legitimacy, satisfaction working with at-risk drinkers, organizational resources, skepticism, time/compensation beliefs, knowledge, and background variables all had direct effects on stated likelihood of practicing SBI. It was assumed knowledge, age, gender, profession, alcohol education, number of patients seen per week, and primary field of practice—family, internal, ObGyn, and pediatrics—would have indirect effects on likelihood of practicing SBI mediated through the six-factor belief variables. Further assumed was that these background variables had direct effects on stated likelihood of SBI. All prior variables covaried and the error terms for the six mediational belief variables were allowed to covary. This initial model did not provide a good fit (χ2(16) = 33.03, p < 0.007).
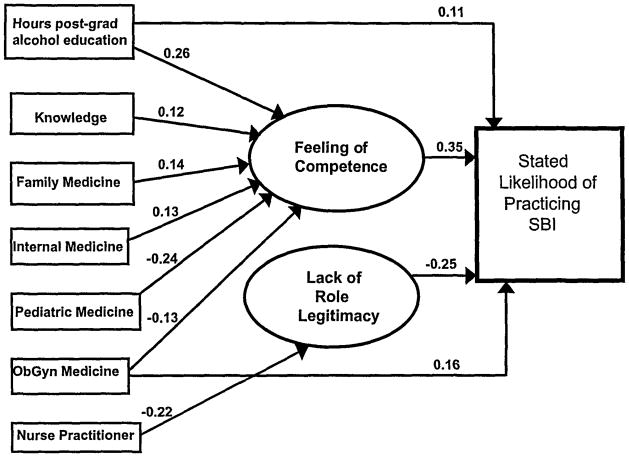
Next, Wald tests served to indicate nonsignificant effects that may be dropped to improve the fit of the model to the data. As a result, the effects of satisfaction working with at-risk drinkers, organizational resources, skepticism, and time/compensation beliefs were dropped from the model. The direct effects of family medicine, internal medicine, ObGyn, and pediatrics on likelihood of SBI were also dropped. The resulting model was a large significant improvement over the initial model (χ2(15) = 32.98, p < 0.001). The final model fit the data (χ2(l) = 0.037, p < 0.843) and had a comparative fit index equal to 1.00. Figure 1 illustrates the path diagram. The findings and interpretations are based on cross-sectional data, and therefore cannot reliably separate cause-and-effect relationships between the variables. We did follow logic of causal order however and specified background variables prior to attitudes; and attitudes prior to intended behaviors (50).
Fig. 1.
Path diagram of variables predicting stated likelihood of practicing SBI.
Direct Effects
Table V shows the significant path coefficients. Feeling competent was related to increased stated likelihood of practicing SBI. Perceived lack of role legitimacy was related to decreased stated likelihood of SBI. Hours of postgraduate alcohol education increased stated likelihood of practicing SBI, and ObGyn practitioners were associated with an increased stated likelihood of practicing SBI.
Table V.
Significant Predictors of Stated Likelihood of Practicing SBI, Feeling of Competence, and Lack of Role Legitimacy for SBI
| Predictor | Standardized coefficient | Unstandardized coefficient | Robust SE | Z | P |
|---|---|---|---|---|---|
| Stated likelihood of SBI practicea | |||||
| Feeling of Competence | 0.35 | 1.53 | 0.30 | 5.13 | <0.001 |
| Lack of role legitimacy | −0.25 | −1.07 | 0.29 | −3.68 | <0.001 |
| Postgraduate alcohol education | 0.11 | 0.29 | 0.16 | 1.83 | <0.05 |
| ObGyn medicine | 0.16 | 1.68 | 0.72 | 2.35 | <0.01 |
| Feeling of competenceb | |||||
| Knowledge | 0.12 | 0.10 | 0.05 | 1.98 | <0.05 |
| Postgraduate alcohol education | 0.26 | 0.18 | 0.06 | 3.16 | <0.001 |
| Family medicine | 0.14 | 0.33 | 0.14 | 2.25 | <0.001 |
| Internal medicine | 0.13 | 0.28 | 0.18 | 2.04 | <0.05 |
| ObGyn medicine | −0.13 | −0.31 | 0.16 | −1.92 | <0.05 |
| Pediatric medicine | −0.24 | −0.66 | 0.21 | −3.17 | <0.001 |
| Lack of role legitimacyc | |||||
| Nurse practitioner | −0.22 | −0.45 | 0.23 | −1.95 | <0.05 |
R2 = 0.30.
R2 = 0.22.
R2= 0.08.
Indirect Effects
Several variables had indirect effects on stated likelihood of practicing SBI mediated through self-rated competence. Hours of postgraduate alcohol education (standardized coefficient = 0.09, Z = 3.34, p < 0.001) and objective knowledge (standardized coefficient = 0.04, Z = 1.85, p < 0.05) mediated by feeling competent was associated with increased stated likelihood to screen and briefly intervene. Specialty groups differentially rated their competency to practice SBI independently of the amount of previous postgraduate alcohol education and knowledge they had received. A specialization in family (standardized coefficient = 0.05, Z = 1.92, p < 0.05) or internal medicine (standardized coefficient = 0.04, Z = 1.70, p < 0.05) mediated by feelings of competence increased stated likelihood of practicing SBI. In contrast, a specialization in pediatrics (standardized coefficient = −0.08, Z = −3.00, p < 0.001) and ObGyn (standardized coefficient = −0.04, Z = 1.77, p < 0.05) mediated by feeling less competent decreased stated likelihood to practice SBI. Finally, NPs were mediated by perceived role legitimacy that was associated with increased stated likelihood of practicing SBI (standardized coefficient = 0.05, Z=1.91, p < 0.05).
DISCUSSION
The aim of this study was to identify beliefs that predict likelihood of practicing SBI by specialty and health profession in order to guide the direction of educational efforts at the practitioner level. On the basis of our sample of physicians and nurse practitioners, the likelihood of practicing SBI varied across specialty group as a function of self-rated competence. For the ObGyn group, low competence was a barrier that suppressed an inclination to practice SBI. For the pediatric group, low self-rated competence was a barrier that decreased stated likelihood of practicing SBI. We found for family and internal medicine practitioners that high competence increased stated likelihood of SBI. The association between confidence and practicing SBI is consistent with past research (22, 34, 51, 52). However, unlike Schorling et al. (22) and Freidmann et al. (34), who examined different specialty groups, we found that clinicians’ self-rated competence intervened in the relationship between specialization and practice of SBI. The past studies may not have observed the intervening role of competence because the analyses used did not examine mediated influences per se (22, 34). Our findings on specialization may be biased because of categorical overlap; however, there was only 1 MD and 17 NPs who indicated practice in two of the primary care areas. The most substantial overlap we observed in family, internal, ObGyn, and pediatric specializations were with the “Other” category. We believe that this extent of dual specialization is common in primary health care settings. The mutual exclusiveness of the specialty categories in the Freidmann et al. study (34) was not mentioned.
Despite what some specialty groups have already learned about alcohol services, they still have competency concerns about applying SBI techniques to their patients. Even when controlling for previous amount of postgraduate alcohol education and objective knowledge, ObGyn specialists were deterred from providing alcohol prevention services by feeling incompetent in using SBI techniques. This is troubling in light of research showing that approximately 20% of women drink some alcohol during pregnancy (53) and even low levels of alcohol use by women who are pregnant can harm the fetus (cited in 54). To build on past educational recommendations to include strategies that increase confidence managing alcohol use disorders (34), the findings here imply that the approaches used to ramp up competence should target specialty groups. We suggest for ObGyn and pediatric specialists that educational approaches move beyond one-size-fits all models to address the specific clinical needs of those specialty practices. By “one-size-fits” all we mean educational materials aimed at general adult populations with a few qualifications made for women, pregnant women, and the elderly. If educators were to cater their SBI materials in terms of the populations these specialties see, then these groups may gain more competencies and be more inclined to apply prevention services. For instance, approaches aimed at ObGyn specialists might want to emphasize the effectiveness of formal screening questionnaires for women (55,56) or how modifications, such as additional questions or lower cutoff scores (54,57), might improve detection. Other examples of useful information would be how varying levels of alcohol consumption are associated with medical risks that are unique to women (58). Information such as this is already present in journal articles and embedded in educational media (45,59–61), but further assembly, packaging, and dissemination of materials to ObGyn audiences may be beneficial.
A targeted approach may also help to engage less involved practitioner groups. For instance, pediatric specialists may see little relevance in attending a CME course on alcohol SBI because the materials seldom pertain to children and adolescents, in conjunction with their parents. Information on prevention and management of substance abuse for youth is available (46, 62–64), but it would be more reasonable to expect pediatric specialists to attend a CME course on SBI if the presentation was devoted to the populations they see. Multifaceted teaching approaches that include information dissemination, case discussion, role play, and presentation by opinion leaders have been shown to be effective in educating clinicians (2, 65, 66). Such approaches could focus on screening and early intervention for the adolescent substance abuser and his or her parents.
On the other hand, the prevalent model of education, which focuses on general adult populations, appears appropriate for building competency among family and internal medical practitioners. As expected, family practitioners’ competency predicted their willingness to practice SBI because health promotion is a clinical priority for them. Internal medicine, however, focuses on diseases and these practitioners need to learn how to identify early stage alcohol abuse (67). Indeed, a subanalysis of an item from the competency scale suggests that the internal medicine clinicians in our sample felt they knew how to “identify at-risk drinkers who have no obvious symptoms of excess consumption” (two-tailed, r = 0.23, p < 0.01). It is plausible although we cannot determine that the internal medicine group learned this competency in early detection of alcohol problems from postgraduate education, and we note that the internal clinicians reported receiving more alcohol education than any of the other specialty groups (two-tailed, r = 0.13, p < 0.05).
In regards to profession, our analysis suggests that perceived role legitimacy is not a barrier to SBI for NPs as it is for MDs. Our result that physicians perceive the provision of alcohol services as separate from their medical role is supported by past work (27). The NPs’ perceived legitimacy for the activities is compatible with their professional culture and clinical orientation of health promotion (68). Furthermore, these findings are consistent with a subanalysis of this sample (not shown) that found NPs reported significantly more frequent questioning of their patients than did MDs in the behavioral lifestyle areas of smoking, exercise, diet, and stress management. Physicians’ perceived lack of role legitimacy from their colleagues suggests that initiatives need to bring higher visibility to the SBI practices of esteemed colleagues, perhaps of members within the respective specialty group (e.g., endorsements, awards, role models). Also, educators should make a priority of responding to skeptics of alcohol-related services and/or behavioral medicine in general, especially if they are opinion leaders, because their views may deter others from practicing preventive services. The vast array of empirical support for the effectiveness of SBI is a crucial component of every type of training to counteract the cynic and to bring a fuller awareness of the potential benefits SBI can have on patients’ health.
As mentioned earlier, the generalizability of the findings is limited by the low response rates. It is possible that alcohol and drug issues were more important to the respondents than to those who did not respond. This may explain why respondents reported they saw more alcohol problems in their patients. In addition, only physicians that worked in a clinical capacity with managed care organizations were included in the study, so the findings cannot address all primary care physicians.
It remains to be seen whether educational strategies informed by group differences have an effect on shaping beliefs and SBI practices. As others have previously reported, practitioner-level education while necessary is not sufficient to the successful implementation of alcohol services in primary care settings (69, 70). Although a discussion of the multilevel and varied approaches to implementing programs is beyond the purview of this report, service delivery systems and policy initiatives may also want to consider group differences among health professionals.
Acknowledgments
This study received support from the National Institute on Alcohol Abuse and Alcoholism (Grant No. R01 AA11713). My thanks to the staff at the Alcohol Research Group, William Colbert, and Norman Turk, who assisted with data management, and thanks also go to John Schafer, who conducted the path analysis. I also thank the scientists at the University of Connecticut Health Center for their collaborative assistance and Constance Wiesner at the Alcohol Research Group for contributing to the original proposal. Finally, thank you to all who participated in the study.
References
- 1.US Department of Health and Human Services. Publication ADM-281-91-0003. Washington, DC: US Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism; 1993. National Institute on Alcohol Abuse and Alcoholism: Eighth special report to the US congress on alcohol and health from the secretary of health and human services. [Google Scholar]
- 2.Saitz R, Sullivan LM, Samet JH. Training community based clinicians in screening and brief intervention for substance abuse problems: Translating evidence into practice. Subst Abuse. 2000;21:21–32. doi: 10.1080/08897070009511415. [DOI] [PubMed] [Google Scholar]
- 3.Adams A, Ockene JK, Wheller EV, Hurley TG. Alcohol counseling: Physicians will do it. J Gen Intern Med. 1998;13:692–698. doi: 10.1046/j.1525-1497.1998.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorman DM, Werner LM, Jacobs LM, Duffy SW. Evaluation of an alcohol education package for non-specialist health care and social workers. Br J Addict. 1990;85:223–233. doi: 10.1111/j.1360-0443.1990.tb03075.x. [DOI] [PubMed] [Google Scholar]
- 5.Rowland N, Maynard AK, Kennedy PF, Wintersgill W, Stone WD. Teaching doctors to take alcohol histories: A limited success story. Med Educ. 1988;22:539–542. doi: 10.1111/j.1365-2923.1988.tb00800.x. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Broadening the Base of Treatment for Alcohol Problems. Washington, DC: National Academy Press; 1990. [PubMed] [Google Scholar]
- 7.Edmunds M, Frank R, Hogan M, McCarty D, Robinson-Beale R, Weisner C, editors. Managing Managed Care: Quality Improvement in Behavioral Health. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 8.Kitchens JM. Does this patient have an alcohol problem? JAMA. 1994;272:1782–1787. [PubMed] [Google Scholar]
- 9.Mezy E. Detecting the problem drinker. Gastrointest Dis Today. 1995;4:19. [Google Scholar]
- 10.Spandorfer JM, Israel Y, Turner BJ. Primary care physicians’ views on screening and management of alcohol abuse inconsistencies with national guidelines. J Fam Pract. 1999;48:899–902. [PubMed] [Google Scholar]
- 11.Center for Substance Abuse Treatment. Primary care physicians: More training needed to diagnose substance abuse. CSAT FAX. 2000;5:1097. [Google Scholar]
- 12.El-Guebaly N, Lockyer JM, Drought J, Parboosingh J, Juschka BB, Weston WA, Campbell W, Chang S. Determining priorities for family physician education in substance abuse by the use of a survey. J Addict Dis. 1995;14:23–31. doi: 10.1300/J069v14n02_03. [DOI] [PubMed] [Google Scholar]
- 13.Ford DE, Klag MJ, Whelton PK, Goldsmith M, Levine ED. Physician knowledge of the CAGE alcohol screening questions and its impact on practice. Alcohol Alcohol. 1994;29:329–336. [PubMed] [Google Scholar]
- 14.Saitz R, Mulvey KP, Plough A, Samet JH. Physician unawareness of serious substance abuse. Am J Alcohol Abuse. 1997;23:343–354. doi: 10.3109/00952999709016881. [DOI] [PubMed] [Google Scholar]
- 15.El-Guebaly N, Toews J, Lockyer J, Armstrong S, Hodgins D. Medical education in substance-related disorders: Components and outcome. Addiction. 2000;95:949–957. doi: 10.1046/j.1360-0443.2000.95694911.x. [DOI] [PubMed] [Google Scholar]
- 16.Lockyer J, El-Guebaly N, Simpson E, Gromoff B, Toews J, Juschka B. Standardized patients as a measure of change in the ability of family physicians to detect and manage alcohol abuse. Acad Med. 1996;71:S1–S3. doi: 10.1097/00001888-199601000-00025. [DOI] [PubMed] [Google Scholar]
- 17.Brown RL. Evaluation of a continuing medical education program for primary care physicians on the management of alcoholism. J Med Educ. 1988;63:482–484. doi: 10.1097/00001888-198806000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Bradley KA. Screening and diagnosis of alcoholism in the primary care setting. West J Med. 1992;156:166–171. [PMC free article] [PubMed] [Google Scholar]
- 19.Fang WL, Applegate SN, Stein RM, Lohr JA. The development of substance-abuse curricular content by five North Carolina schools. Acad Med. 1998;73:1039–1043. doi: 10.1097/00001888-199810000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Center for Substance Abuse Treatment. Less than one-third of primary care physicians routinely screen for substance abuse. CSAT FAX. 2000;5:1096. [Google Scholar]
- 21.Gottlieb NH, Mullen PD, McAlister AL. Patients’ substance abuse and primary care physician: Patterns of practice. Addict Behav. 1987;12:23–32. doi: 10.1016/0306-4603(87)90005-0. [DOI] [PubMed] [Google Scholar]
- 22.Schorling JB, Klas PT, Willems JP, Everett AS. Addressing alcohol use among primary care patients: Differences between family medicine and internal medicine residents. J Gen Intern Med. 1994;9:248–254. doi: 10.1007/BF02599649. [DOI] [PubMed] [Google Scholar]
- 23.McCrady BS, Richter SS, Morgan TJ, Slade J, Pfeifer C. Involving health care workers in screening for alcohol problems. J Addict Dis. 1996;15:45–58. doi: 10.1300/J069v15n03_03. [DOI] [PubMed] [Google Scholar]
- 24.Rowland N, Maynard A, Beveridge A, Kennedy P, Wintersgill W, Stone W. Doctors have no time for alcohol screening. Br J Med. 1987;295:95–96. doi: 10.1136/bmj.295.6590.95-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aborelius E, Thakker KD. Why it is so difficult for general practitioners to discuss alcohol with patients? Fam Pract. 1995;12:419–422. doi: 10.1093/fampra/12.4.419. [DOI] [PubMed] [Google Scholar]
- 26.Ogborne AC, Rush B, Ekdahl A, Fondacaro R. The views of health and social service professionals regarding alcohol problems and their treatment. Int J Addict. 1986;21:1051–1058. doi: 10.3109/10826088609077254. [DOI] [PubMed] [Google Scholar]
- 27.Miller NS, Sheppard MA, Colenda CC, Magen J. Why physicians are unprepared to treat patients who have alcohol- and drug-related disorders. Acad Med. 2001;76:410–418. doi: 10.1097/00001888-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Chappel JN. Attitudes toward the treatment of substance abusers. In: Lowenson J, Ruiz P, Millman R, editors. Comprehensive Textbook of Substance Abuse. Baltimore: Williams & Wilkins; 1992. pp. 983–996. [Google Scholar]
- 29.Westermyer J, Doheny S, Stone B. An assessment of hospital care for the alcoholic patient. Alcohol Clin Exp Res. 1978;2:53–57. doi: 10.1111/j.1530-0277.1978.tb04694.x. [DOI] [PubMed] [Google Scholar]
- 30.Botelho RJ, Richmond R. Secondary prevention of excessive alcohol use: Assessing the prospects of implementation. Fam Pract. 1996;13:182–193. doi: 10.1093/fampra/13.2.182. [DOI] [PubMed] [Google Scholar]
- 31.Drummond DC. Alcohol interventions: Do the best things come in small packages? Addiction. 1997;92:375–379. [PubMed] [Google Scholar]
- 32.O’Connor PG, Schottenfeld RS. Patient with alcohol problems. N Engl J Med. 1998;338:592–602. doi: 10.1056/NEJM199802263380907. [DOI] [PubMed] [Google Scholar]
- 33.Rush B, Bass M, Stewart M, McCracken E, Labreque M, Bondy S. Detecting, preventing, and managing patients’ alcohol problems. Can Fam Physician. 1994;40:1557–1566. [PMC free article] [PubMed] [Google Scholar]
- 34.Freidmann PD, McCullough D, Chin MH, Saitz R. Screening and intervention for alcohol problems: A national survey of primary care physicians and psychiatrists. J Gen Intern Med. 2000;15:84–91. doi: 10.1046/j.1525-1497.2000.03379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deuban CJ. The impact of managed care on labor substitution in the health care workforce. Mich Acad. 1998;30:69–83. [Google Scholar]
- 36.Ockene JK, Adams A, Hurley TG, Wheeler EV, Herbert JR. Brief physician- and nurse practitioner-delivered counseling for high risk drinkers. Arch Int Med. 1999;159:2198–2205. doi: 10.1001/archinte.159.18.2198. [DOI] [PubMed] [Google Scholar]
- 37.Israel Y, Hollander O, Sanchez-Craig M, Booker S, Miller V, Gingrich R, Rankin JG. Screening for problem drinking and counseling by the primary care physician-nurse team. Alcohol Clin Exp Res. 1996;20:1443–1450. doi: 10.1111/j.1530-0277.1996.tb01147.x. [DOI] [PubMed] [Google Scholar]
- 38.Chick J, Lloyd G, Crombie E. Counseling problem drinkers in medical wards: A control study. BMJ. 1985;290:965–967. doi: 10.1136/bmj.290.6473.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kahan M, Wilson L, Becker L. Effectiveness of physician-based interventions with problem drinkers: A review. Can Med Assoc J. 1995;152:851–859. [PMC free article] [PubMed] [Google Scholar]
- 40.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem drinkers: A randomized controlled trial in community based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 41.World Health Organization Study Group. A cross-national trial of brief interventions with heavy drinkers. Am J Public Health. 1996;86:948–955. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–668. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones L. In-patient nurse practitioners. Nurse Pract. 1985;10:48–50. [PubMed] [Google Scholar]
- 44.National Institute on Alcohol Abuse and Alcoholism. The Primary Care Setting Recognition and Care of Patients With Alcohol Problems. Washington, DC: US Government Printing Office; 1994. p. 18. [Google Scholar]
- 45.Thorp JM. The obstetrician/gynecologist. Alcohol Health Res World. 1994;18:117–126. [PMC free article] [PubMed] [Google Scholar]
- 46.Adger H, Werner MJ. The pediatrician. Alcohol Health Res World. 1994;18:121–126. [PMC free article] [PubMed] [Google Scholar]
- 47.Townes PN, Harkley AL. Alcohol screening practices of primary care physician in eastern North Carolina. Alcohol. 1994;11:489–492. doi: 10.1016/0741-8329(94)90073-6. [DOI] [PubMed] [Google Scholar]
- 48.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 49.Ajzen I, Madden TJ. Prediction of goal-directed behavior: Attitudes, intentions and perceived behavioral control. J Exp Soc Psychol. 1986;22:453–474. [Google Scholar]
- 50.Davis JA. The Logic of Causal Order. Newbury Park, CA: Sage; 1985. [Google Scholar]
- 51.Warburg MM, Cleary PD, Rohman M, Barnes HN, Aronson M, Delbanco TL. Residents’ attitudes, knowledge, and behavior regarding diagnosis and treatment of alcoholism. Journal of Medical Education. 1987;62:497–503. doi: 10.1097/00001888-198706000-00007. [DOI] [PubMed] [Google Scholar]
- 52.Geller G, Levine DM, Mamon JA, Moore RD, Bone LR, Stokes EJ. Knowledge, attitudes, and reported practices of medical students and house staff regarding the diagnosis and treatment of alcoholism. JAMA. 1989;261:3115–3120. [PubMed] [Google Scholar]
- 53.Ebrahim SH, Luman ET, Floyd RL, Murphy CC, Bennett EM, Boyle CA. Alcohol consumption by pregnant women in the United States during 1988–1995. Obstet Gynecol. 1998;92:187–192. doi: 10.1016/s0029-7844(98)00205-1. [DOI] [PubMed] [Google Scholar]
- 54.Chang G. Alcohol-screening instruments for pregnant women. Alcohol Health Res World. 2001;25:204–209. [PMC free article] [PubMed] [Google Scholar]
- 55.Stein MD, Cyr MG. Women and substance abuse. In: Samet JH, Stein MD, O’Connor PG, editors. The Medical Clinics of North America. Vol. 81. Philadelphia: Saunders; 1997. pp. 979–998. [DOI] [PubMed] [Google Scholar]
- 56.Dawson NV, Dadheech G, Speroff T, Smith RL, Schubert DSP. The effect of patient gender on the prevalence and recognition of alcoholism on a general medicine inpatient service. J Gen Intern Med. 1992;7:38–45. doi: 10.1007/BF02599100. [DOI] [PubMed] [Google Scholar]
- 57.Cry MG, Moulton AW. The physician’s role in prevention, detection, and treatment of alcohol abuse in women. Psychiatr Ann. 1993;23:454–462. [Google Scholar]
- 58.Bradley KA, Badrinath S, Bush K, Boyd-Wickizer J, Anawalt B. Medical risks for women who drink alcohol. J Gen Intern Med. 1998;13:627–639. doi: 10.1046/j.1525-1497.1998.cr187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.National Institutes of Health. NIH Pub No. 95–3769. Rockville, MD: The Institute; 1995. National Institute on Alcohol Abuse and Alcoholism: The Physicians’ Guide to Helping Patients With Alcohol Problems. [Google Scholar]
- 60.National Institute on Alcohol Abuse and Alcoholism. Alcohol Alert No. 56: Screening for Alcohol Problems—An Update. Rockville, MD: The Institute; 2002. [Google Scholar]
- 61.Russell M. New assessment tools for risk drinking during pregnancy. Alcohol Health Res World. 1994;18:55–61. [PMC free article] [PubMed] [Google Scholar]
- 62.Adger H, Macdonald DI, Wenger S. Core competencies for involvement of health care providers in the care of children and adolescents in families affected by substance abuse. Pediatrics. 1999;103:1083–1084. [PubMed] [Google Scholar]
- 63.Schuydower M, Fuller PG, Heyman RB, Jacobs EA, Pruitt AW, Sutton JM, Tanenbein M. Role of the pediatrician in prevention and management of substance abuse. Pediatrics. 1993;91:1010–1013. [PubMed] [Google Scholar]
- 64.Farrow JA, Deisher RA. A practical guide to the office assessment of substance abuse. Pediatr Ann. 1986;15:675–684. doi: 10.3928/0090-4481-19861001-06. [DOI] [PubMed] [Google Scholar]
- 65.Davis DA, Thomson MA, Oxman AD, Haynes RB. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992;268:1111–1117. [PubMed] [Google Scholar]
- 66.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: A systematic review of 102 trials of interventions to improve professional practice. Can Med Assoc J. 1995;153:1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 67.O’Connor PG. The general internist. Alcohol Health Res World. 1994;18:110–116. [PMC free article] [PubMed] [Google Scholar]
- 68.Standards of Practice. Washington, DC: American Academy of Nurse Practitioners; 1993. [Google Scholar]
- 69.Babor TF, Higgins-Biddle JC. Alcohol screening and brief intervention: Dissemination strategies for medical practice and public health. Addiction. 2000;95:677–686. doi: 10.1046/j.1360-0443.2000.9556773.x. [DOI] [PubMed] [Google Scholar]
- 70.Samet JH, Freidman P, Saitz R. Benefits of linking primary medical care and substance abuse services: Patient, provider, and societal perspectives. Arch of Intern Med. 2001;161:85–91. doi: 10.1001/archinte.161.1.85. [DOI] [PubMed] [Google Scholar]