Introduction
Diabetes is one of the fastest growing diseases in Canada. It is estimated that 2 million Canadians have type 2 diabetes and that there are more than 60,000 new cases of this disease diagnosed each year. The cost of diabetes in Canada is projected to be up to $9 billion annually.1 One-third of those affected with type 2 diabetes are unaware that they have the disease.1 Managing diabetes is a challenging endeavour for those diagnosed and involves routine monitoring and regular testing in order for patients to maintain reasonable glycemic control. The DICE study in 2005 found that 1 in 2 Canadians with type 2 diabetes do not have their blood sugar under control and that control is worse the longer patients have had diabetes.2 As a measure of glycemic control, the Canadian Diabetes Association (CDA) recommends glycated hemoglobin (HbA1c [%]) levels ≤7.0.3 However, according to one study, only 29% of patients with diabetes actually had an HbA1c test in the previous year, and among those tested, only 43% had an HbA1c less than 7%.4 Additionally, 18% of those tested had an HbA1c of 9.5% or more, meaning that their blood glucose levels were uncontrolled.4
Given the complexity of diabetes control, evidence suggests that diabetes can be best managed through an interdisciplinary team that includes a pharmacist.5 The relative accessibility of the community pharmacist allows patients the opportunity to discuss their health care concerns, typically without the need for a referral or appointment (though making an appointment so that the pharmacist is able to set aside an appropriate amount of time is becoming more common). This unique position allows pharmacists to readily monitor patients and assist them in attaining adequate glucose control.
HbA1c testing is an important outcome measure in patients with diabetes. Unlike a point-in-time blood glucose measure, the HbA1c provides an estimate of glycemic control over a 3-month period. It allows the health care provider to monitor patients with diabetes and estimate how well their disease is controlled and whether they require additional interventions to maintain target levels. The United Kingdom Prospective Diabetes Study (UKPDS) has shown that lower HbA1c levels have been correlated with fewer complications.6 For instance, in epidemiologic analyses, HbA1c levels >7.0% are associated with a significantly increased risk of both microvascular and macrovascular complications, regardless of underlying treatment.3
John Papastergiou Pharmacy Limited operates at 3 locations as Shoppers Drug Mart in Toronto, Ontario. All 3 pharmacies are located in an urban setting with a diverse, multi-ethnic patient population. The Pharmacy team, including pharmacists, pharmacy technicians, interns and pharmacy students from all 3 locations, is working to improve the management of patients with diabetes through the use of HbA1c testing. Historically, the testing of HbA1c required a visit to the physician and was limited to a laboratory blood test. With the introduction of the Bayer A1C Now meters, patients can be tested by their community pharmacist without a laboratory requisition and HbA1c results can be made available within 5 minutes. The HbA1c meter has demonstrated an accuracy of 99% in 3 independent evaluation studies.7 The Pharmacy team decided that the level of accuracy, in combination with the ease and speed of testing, made this new innovation the perfect tool for testing and monitoring their patients with diabetes. The meters provide an efficient and reliable method for HbA1c monitoring. The HbA1c result provides the pharmacist with more information regarding the patient's glycemic control and allows for additional consultation and recommendations in an attempt to improve outcomes.
Clinic days
The Pharmacy team designed special clinic days where patients with diabetes could have their medication, lifestyle and health history assessed. Patients with diabetes were identified when picking up diabetes medications or during a MedsCheck medication review. Patients were then scheduled for HbA1c testing and follow-up at the next planned HbA1c clinic. Upon arrival at the clinic, the patients had a private consultation with a pharmacist. They were then asked to sterilize their skin with an alcohol wipe and to pierce their finger with the lancing device to provide a blood sample for the HbA1c machine. The HbA1c machine works in a similar manner to a glucometer, but requires a couple of additional steps for the testing process. The blood sample is mixed with a reagent and then is inserted into the meter. While the meter calculated the results, the pharmacist took the opportunity to review the patient's medications and lifestyle, and to discuss management including nonpharmacological interventions such as diet and exercise. On average, the patient interactions lasted 20–25 minutes.
The results of the HbA1c test helped direct the patient education provided by the pharmacist. If a patient's HbA1c was found to be less than 7%, the patient was encouraged to maintain any life-style modifications they were making and to continue with the management of their medications to maintain optimal control. If the HbA1c reading was between 7% and 9.5%, patients were cautioned that they needed to improve their glycemic control. Recommendations were made according to the CDA on diet and lifestyle modifications, including exercise. A follow-up with the patient was scheduled. If the HbA1c reading was above 9.5%, patients' lifestyle factors were reviewed and they were strongly encouraged to make changes to their diet and lifestyle according to the CDA recommendations. Medication adherence was also discussed. Patients were encouraged to take a proactive approach to their diabetes management. Interventions included discussing Canada's food guide and suggesting exercise for 30 minutes daily.
In addition to the recommendations on lifestyle given to the patient, the pharmacist offered to fax the physician with the HbA1c result and any suggested changes to therapy. At the end of the appointment, the patients were given a reference copy of their HbA1c reading. They were provided with goals in terms of diabetes management, including future HbA1c targets. Some of the patients preferred to provide their physicians directly with their HbA1c readings, as opposed to having the pharmacy forward a fax. Patients were also offered the opportunity to schedule a follow-up appointment with the pharmacist. The Pharmacy team made an attempt to schedule follow-up HbA1c testing for all patients who attended the clinics 3 months after the initial session with the pharmacist.
Results
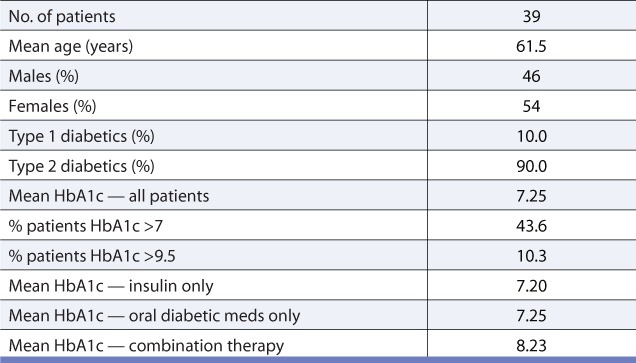
Table 1 summarizes the demographics of the patient population and the results of HbA1c testing. The mean HbA1c was 7.25%, and 43.6% of patients had an HbA1c over 7%, while 10.3% of patients had an HbA1c over 9.5%. No formal feedback was elicited from the patients or their physicians on the value of the HbA1c clinic. However, anecdotally, feedback from both patients and physicians was overwhelmingly positive. Patients valued the opportunity to have a private consultation with a pharmacist. They found the clinic informative and felt it improved their overall understanding of diabetes management.
TABLE 1.
HbA1c results from patients attending clinics
Feedback from the physicians indicated that they appreciated the initiative taken to test patients' HbA1c. Initially, there was a concern about possible unnecessary or duplicate testing if physicians ordered follow-up blood work to verify the pharmacy HbA1c result, but this did not appear to manifest. Physicians identified that they preferred reporting of the HbA1c result and any recommended changes to pharmacotherapy be communicated via fax. This process allowed for the physician to contact the patient and arrange for an appointment if an intervention was necessary.
Discussion
To our knowledge, this is one of the first pilot projects in Canada to examine the use of HbA1c meters in the community pharmacy setting.8 It describes a new model for helping to manage patients with diabetes and outlines strategies for both inter-professional collaboration and follow-up with patients. Based on the experience from the clinic days, communication with the physician or primary care provider was well received.
This pilot project has various limitations. The results of the HbA1c clinics are only able to provide information on initial testing of patients and not the ongoing management of their disease. The impact of the involvement of the pharmacist was assessed only through informal unsolicited satisfaction feedback and could be formally evaluated in future studies. In addition, because of the nature of the clinics, this was a real-time study and not a controlled trial to assess the impact of the pharmacist's interventions. Changes in HbA1c levels over time might help to support the value of this role for the community pharmacist, but would be difficult to directly attribute to the work of the pharmacist alone. Expansion of this pilot program has already begun nationally. A future study involving a greater number of pharmacies and a greater number of patients could help to build on this work.
Conclusion
HbA1c clinics offer an innovative approach for pharmacists to monitor patients with diabetes in the community. In total, 43.6% of patients who attended the clinics presented with an HbA1c level above the recommended target. These results delineate the potential opportunity for pharmacists to play a prominent role in the screening and monitoring of patients in the community. In addition, the clinics provide an effective mechanism for improving patient education, enhancing diabetes management and increasing pharmacist-physician communication. The relative accessibility of community pharmacists places them in a unique position to actively monitor patients with diabetes and other chronic diseases. The wave of technology and innovation, including HbA1c meters, will arm pharmacists with the tools required to meet these needs.
Footnotes
Financial acknowledgements: This project was funded entirely by John Papastergiou Pharmacy Limited. Bayer A1C Now meters were provided at no cost by Bayer Inc.
References
- 1.It's your health — type 2 diabetes (Health Canada, 2005) Available: www.hc-sc.gc.ca/hl-vs/iyh-vsv/diseases-maladies/diabete-eng.php (accessed August 10, 2011) [Google Scholar]
- 2.Harris SB, Ékoé J, Zdanowicz Y, Webster-Bogaert S. Glycemic control and morbidity in the Canadian primary care setting (results of the diabetes in Canada evaluation study) Diabetes Res Clin Pract. 2005;70:90–7. doi: 10.1016/j.diabres.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Available: www.diabetes.ca/files/cpg2008/cpg-2008.pdf (accessed August 10, 2011) [Google Scholar]
- 4.Saaddine JB, Engelgau MM, Beckles GL, et al. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2005;28(suppl 1):S4–36. [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study Group: intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 7.Holmes EW, Erşahin C, Augustine GJ, et al. Analytic bias among certified methods for the measurement of hemoglobin A1C: a cause for concern? Am J Clin Pathol. 2008;129:540–7. doi: 10.1309/U3GPPTCBP1VLL8AW. [DOI] [PubMed] [Google Scholar]
- 8.Al Hamarneh YN, Rosenthal M, Tsuyuki RT. Glycemic control in community-dwelling patients with type 2 diabetes. Can Pharm J. 2012;145:68–9. doi: 10.3821/145.2.cpj68. [DOI] [PMC free article] [PubMed] [Google Scholar]


