Abstract
Psychotic-like experiences (PLEs) have been observed worldwide in both adults and children outside the context of a clinical disorder. In the current study, we investigate the prevalence and patterns of PLEs among children and adolescents in Kenya. Among 1,971 students from primary and secondary schools around Nairobi (aged 8–19), 22.1 % reported a lifetime history of a psychotic experience, and 16.3 % reported this unrelated to sleep or drugs. Psychotic experiences were more common in males compared to females. LCA resulted in a three-class model comprised of a normative class (83.3 %), a predominately hallucinatory class (Type 1 psychosis: 9.6 %), and a pan-psychotic class (Type 2 psychosis: 7.2 %). These results indicate that PLEs are prevalent in children and adolescents, and the distributions of symptom clusters are similar to that found in adulthood. The relationship of specific PLEs to the future development of psychotic disorder, functional impairment or distress will require further study.
Keywords: Psychosis, Children, Adolescents, Kenya, Africa, LCA
Introduction
In recent years, there has been a great amount of research regarding the prevalence and meaning of psychotic-like experiences (PLEs). While such occurrences are present in the general population outside the context of psychopathology [1–4], the presence of PLEs is associated with increased risk of later psychotic disorder development and may represent a potential etiological focus useful for further study of pathology [5–7]. PLEs have been thought to likely exist along a continuum in the general population, from normative experience to multiple PLEs or diagnosable psychotic disorders [8–10].
Non-clinical PLEs have been described in children and adolescents with varying prevalence rates. Studies in different countries have showed sample estimations in children and adolescents between 38 and 66 % for endorsement of any PLE [5, 11–14]. Epidemiological studies have also suggested endorsement of PLEs at higher rates in children compared to older populations [15–18]. Higher reports of psychotic experiences suggests that there is some overre-porting of symptoms in younger individuals, possibly due to misattribution of an experience or misunderstanding of screen questions. However, older adults may also have a higher severity threshold for endorsing having experienced specific psychosis screen items, or may have forgotten more distant experiences. The significance of PLEs in children is not entirely clear. Presence of hallucinatory experiences, even in the absence of other indications of illness, have been linked to increased subsequent psychopathology [19]. Other data have shown that increasing PLEs during childhood and adolescence may be predictive of later development of psychotic illness by early adulthood, or that certain PLEs (such as perceptual abnormalities or persecutory ideation) during youth may be more specific for psychotic disorder development [14, 20]. While a relationship between childhood PLEs and adult psychotic illness has been suggested in past research, the fact that PLEs are often found to be more prevalent in children than adults suggests some may be normative in development [21].
PLEs have been associated with increased interpersonal violence [22], emotional distress and symptoms of depressive illness [23, 24], and increased use of illicit substances [25]. In general populations, increasing PLE load has also been associated with linear decline in health status in several countries throughout the world [26]. For these reasons, in addition to their relationship to later psychotic illness development, PLEs—particularly in children and adolescent populations—represent an important research focus for potential early risk identification efforts.
In our recent study of college-aged students in Kenya [27], we found that 19.2 % of students had experienced at least one psychotic phenomenon while not dreaming or under the influence of alcohol or drugs. Latent class analysis (LCA) of symptoms indicated a three-class model, which included a hallucinatory class (termed “Type 1” PLE), a class comprising of multiple perceptual and delusionary experiences (“Type 2” PLE), and a normative class. This distribution of symptoms was similar to that found in latent class analyses evaluating general adult populations in New Zealand and the United States [28, 29]. In the current study, we investigate PLEs in Kenyan children and adolescents (students), and explore whether the prevalence and patterns of symptoms are comparable to adult students studied in the same demographic area [27]. In examining this younger cohort, we hypothesized that reports of PLEs would be lower than in the older individuals previously studied, with a gender bias toward males having more psychotic phenomena. Furthermore, we predicted that LCA would show a similar symptom distribution pattern in our participants and those found in adult studies, with a predominantly hallucinatory type (“Type 1”) and a pan-psychotic type (“Type 2”) of PLE.
Methods
Participants
Participants consisted of students from four public primary schools (grades 5–8; Manguo Primary, Kasarani, Drive-In, and Ngecha) and three public secondary schools (grades 9–12; Manguo Secondary, Gichuru, and Ruaraka) in Kenya, with reported age ranges from 8 to 19. The Manguo, Ngecha and Gichuru schools were located in rural areas, in the Kiambu West district in central Kenya. The other schools were urban, located in Nairobi city. The study was described to prospective participants while in class, and the students were given the option to decline or to participate and assured of anonymity. A research assistant distributed questionnaires and was available for assistance if needed. Of the 2,385 students given the questionnaire, 1,971 provided usable data. Written and signed consent was obtained from all participants or guardians. Ethical clearance for the study was received from Kenyatta National Hospital and the University of Nairobi Ethical Review Board.
Assessments
Participants completed the psychosis portion of the English version of the composite international diagnostic interview (CIDI)—a self-report questionnaire, that examined six different domains of past psychotic experience: (1) visual hallucinations, (2) auditory hallucinations, (3) thought insertion and broadcasting, (4) belief that one’s mind was being controlled by an outside force (mind control), (5) referential thinking, and (6) persecutory ideation. Past studies of the psychosis module of the CIDI have demonstrated that the level of agreement is high between CIDI questionnaire items and clinician diagnosis when the latter is driven by clinicians asking diagnostic questions of symptoms as compared to clinician observation of the subject [30]; as our current study was designed to evaluate PLEs as experienced by the participants themselves, this particular validity of the CIDI was found to be advantageous. For each domain, participants were asked to report whether or not they had ever experienced the phenomenon and if so, if it had occurred outside of dreaming, being half-asleep, or under the influence of alcohol or drugs.
Statistical Analysis
General statistical analyses were done using SPSS 11.0.1 (SPSS Inc., Chicago, IL, USA). Comparisons between groups were made using Pearson’s Chi-square (χ2) test or the Fischer‘s exact test (2-tailed for all tests). Logistic regressions were used to calculate odds ratios that described the strength of association between gender and PLEs. Obtained data were also analyzed using LCA to attempt to empirically define groups in the data based on presence or absence of particular PLEs [31]. The Latent Gold 4.5 statistical program (Statistical Innovations, Belmont, MA, USA) was used for this purpose; an identical analytical approach was used in our previous study of college students in Kenya [27]. LCA was applied to a 1,903 × 6 data matrix in an iterative manner. The rows corresponded to 1,903 of 1,971 surveyed Kenyan students who indicated their gender on the questionnaire. We included gender as a covariate in the analysis to allow for the possibility of gender- related differences in symptoms. A total of 1,169 participants completed all six of the symptom endorsement items on the screen. For purposes of LCA, items with a response of “don’t know” or no response were treated as an absence of symptoms. In determining the optimal number of classes for the final solution, we looked at the cluster configurations that yielded a significant decrease in the Bayesian information criterion (BIC) [32] values from the preceding lower class solution; smaller BIC values are preferred over larger ones as the former represent overall model improvement [33, 34]. Individual subjects were then assigned class membership based on the likelihood of their particular response profile, and LCA class differences in demographic variables were explored.
Results
Demographic Information and Participation Characteristics
Demographic information of the 1,971 participants is provided in Table 1. Only 320 (16.2 %) participants reported their age. The mean (SD) age of the students was 12.98 years (SD = 1.8), and the median was 12.95 years. The reported ages of participants were 8–19 years. Grade data was available for 1,835 (93.1 %) participants. The mean “grade of study” in our sample was 7.6, and the median was 7. The grades of study ranged from 5th grade to 12th grade.
Table 1.
Demographic profiles of surveyed Kenyan primary and secondary school students (N = 1,971)
| Demographic variable | Value |
|---|---|
| Gender | |
| Female | 965 (49,0) |
| Male | 938 (47.6) |
| Not provided | 68 (3.4) |
| Age (years)a | |
| Mean (total) | 13.0 (1.8) |
| Female | 12.7 (1.7) |
| Male | 13.3 (1.8) |
| Median (total) | 13.0 |
| Grade of studyb | |
| Mean (total) | 7.6 (1.9) |
| Female | 7.5 (1.8) |
| Male | 7.6 (2.0) |
| Median (total) | 7 |
Values are given as number of participants (percentages)
320 participants completed question on age
1,835 participants completed question on grade of study
Prevalence and Presentation of Psychotic Experiences
Among the students surveyed, prevalence of psychotic experiences is reported in Table 2. Among those who completed the entire psychosis questionnaire, 265 (22.1 %) reported having experienced a psychotic symptom in the past; and 195 (16.3 %) reported at least one psychotic phenomenon that occurred while not half-asleep, dreaming, or under the influence of drugs or alcohol. The prevalence across genders was 18.8 % for males and 14.2 % for females; the most commonly reported symptom was visual hallucinations (9.7 %) while the least common was persecutory ideation (7.1 %).
Table 2.
Prevalence of psychotic experiences of surveyed Kenyan primary and secondary school students
| Psychotic experience | |
|---|---|
| Any psychotic experiencea | |
| Total | 265 (22.1) |
| Not sleep/drug related | 195 (16.3) |
| Male | 106 (18.8) |
| Female | 86 (14.2) |
| Visual hallucinations | |
| Total | 287 (15.3) |
| Not sleep/drug related | 183 (9.7) |
| Male | 103 (11.5) |
| Female | 73 (7.9) |
| Auditory hallucinations | |
| Total | 212 (12.2) |
| Not sleep/drug related | 152 (8.8) |
| Male | 83 (10.1) |
| Female | 63 (7.3) |
| Thought broadcasting/insertion | |
| Total | 161 (10.4) |
| Not sleep/drug related | 141 (9.1) |
| Male | 84 (11.4) |
| Female | 56 (7.3) |
| Mind control | |
| Total | 192 (12.9) |
| Not sleep/drug related | 138 (9.2) |
| Male | 82 (11.4) |
| Female | 54 (7.3) |
| Referential thinking | |
| Total | 194 (13.2) |
| Not sleep/drug related | 136 (9.3) |
| Male | 78 (11.2) |
| Female | 54 (7.4) |
| Persecutory ideation | |
| Total | 146 (10.1) |
| Not sleep/drug related | 103 (7.3) |
| Male | 62 (9.1) |
| Female | 39 (5.4) |
Prevalence estimates derived using total numbers of students completing specific item on the questionnaire
Refers to prevalence of having any of the six psychotic experiences asked. Prevalence estimates were based on students completing all six psychotic experience items (N = 1,199)
Mental Health Treatment
Five males and nine females reported lifetime history of seeking professional help for psychotic symptoms—this translated to 8.8 and 23.1 % of symptomatic males and females respectively who answered this question. Of these individuals reporting help seeking, past psychiatric hospitalization were reported by three males (6.8 %) and five (15.2 %) females.
Gender Effects
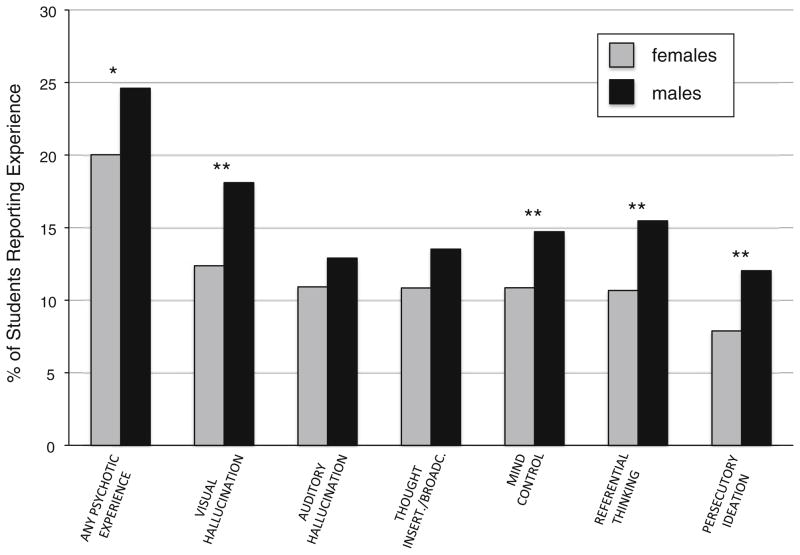
Figure 1 shows the percentage of male and female students who reported psychotic experiences. PLEs were more prevalent in males than females, however statistically significant differences were only noted for “visual hallucination” (m: 18.1 %, f: 12.4 %; p = 0.0007), “mind control” (m: 14.7 %; f: 10.9 %; p = 0.03), “referential thinking” (m: 15.5 %, f: 10.7 %; p = 0.008), and “perse-cutory ideation” (m: 12.0 %, f: 7.9 %; p = 0.01). There was a trend level effect of gender (p = 0.09) on having had any psychotic experience.
Fig. 1.
Gender differences in PLE prevalence. The graph shows the percentage of students that reported any PLE (1st bars), and specific PLEs, for each gender. Comparisons were done using Chi-square analysis. *p < 0.10; **p < 0.05. Gray females; Black males
Latent Class Analysis
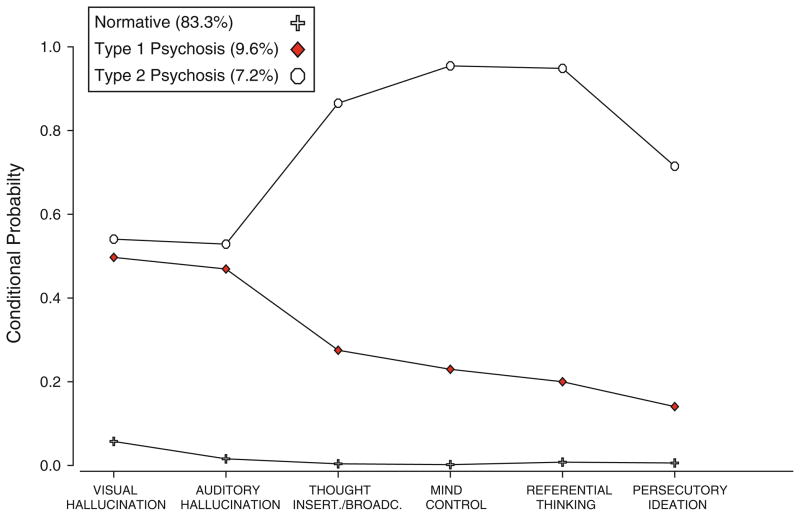
The LCA was done generating up to seven-class solutions. Obtained BIC values included: 1-class: 7,645; 2-class: 5,542; 3-class: 5,467; 4-class: 5,466; 5-class: 5,484; 6-class: 5,521; and 7-class: 5,568. A three-class solution was selected as optimal, as the corresponding BIC value represented a significant decrease from that obtained from a two-class solution. Further increase in the number of classes did not significantly decrease the BIC value any further. Figure 2 shows the results obtained from a three-class LCA model. The obtained classes included: (1) a largely normative class (83.3 % of participants), (2) a class with hallucinatory experiences occurring at higher probability than other experiences (9.6 %), and (3) a class with all psychotic experiences occurring with high probability (7.2 %). Symptom distributions of hallucinatory and pan-psychotic classes were similar to that previously reported in Kenyan adults as “Type 1” and “Type 2” PLE, respectively Ndetei et al. [27].
Fig. 2.
Classes of psychotic experiences in Kenyan children and adolescents. Latent class analysis (LCA) was used to classify students based on their reports on the presence of absence of PLEs. Gender was included as a covariate in the analysis. Only students who stated their gender were used in the LCA (N = 1,903). The graph shows the three classes derived from LCA (i.e. “normative”, “Type 1 psychosis” and “Type 2 psychosis”), and the probability of having specific PLEs in each class
The gender distribution was significantly different across the derived classes (χ2 = 11.4, p = 0.003), with relatively more males than females in the psychotic classes. The normative class comprised of 754 (47.6 %) males and 831 (52.4 %) females; the “Type 1” psychosis class comprised of 107 (58.8 %) males and 75 (41.2 %) females; and the “Type 2” psychosis class comprised of 77 (56.6 %) males and 59 (43.4 %) females.
As data on age was available for only a minority of participants, “grade of study” The mean (SD) grade of study of individuals in the normative LCA class was 7.7 (1.9); for those in the “Type 1” psychosis class was 7.3 (2.0); and for those in the “Type 2” psychosis class was 6.7 (1.7). Analysis of variance (ANOVA) of LCA classes resulted in significant effects for grade of study (F = 17.3; p < 0.0001).
Discussion
In this data, we found that a lifetime history of PLE is prevalent (22.1 %) in Kenyan students between the ages of 8 and 19. Prevalence rates found in our study were lower than those reported in other studies of children and adolescents, which were between 38 and 66 % [5, 11, 13, 14]. Comparisons of PLE rates across studies is however complicated by differences in the survey questions or the number of questions, which can influence prevalence estimates [5, 27]. To our knowledge the 6-item CIDI psychosis screen has not been previously used to exclusively study children and adolescents; however it has been used in older populations [28, 35]. A cross-national study of adults using the CIDI screen reported an overall PLE prevalence of 12.5 % [26]. The rates found in our study are comparable to that previously reported in Kenyan college students (mean age of 21.3 years) using the identical CIDI screen, where PLE prevalence was 23 % [27]. The high degree of similarity in prevalence across these different ages may suggest there are few cases of a first episode PLE beyond adolescence in Kenyan youth, though longitudinal work would be needed to confirm this. The findings could imply that the onset of full-blown psychotic disorder, usually in late adolescence or in the twenties [36], is often preceded by PLEs several years earlier. However, PLE prevalence in college students may underestimate the true population prevalence in that age group; since some of those with existing psychopathology would conceivably not go on to attend college.
Among individual psychotic experiences, the prevalence rates in our sample ranged from 10.1 % (persecutory ideation) to 15.3 % (visual hallucinations). Perceptual abnormalities have also been reported as the most common PLE in child, adolescent and adult community surveys [5, 11, 28, 37–39]; while other authors have found delusionary experiences, particularly persecutory ideation as the most prevalent [14, 29, 40–43]. Compared to our previous survey of Kenyan college students, this study’s younger cohorts had a higher prevalence of delusionary experiences and a slightly lower prevalence of perceptual experiences. Thus, while overall PLE prevalence rates were similar, the specific PLEs reported appear to change with age in this population. This is consistent with previous reports of more delusional phenomena in younger compared to older youth [24, 44]. Relatively high rates of delusionary experiences in our current study suggest that some delusional experiences may be normative in children and adolescents. Our findings of increased PLE in males compared to females are consistent with an earlier onset of psychotic disorders in males [45–47]. Male–female discrepancy in PLE prevalence was also evident in our study of older Kenyan youth [27], although these differences were less significant than in the current study.
Results of LCA suggest the existence of two major classes of psychotic experiences in Kenyan children and adolescents, including a “Type 1” psychosis (9.6 % of analyzed sample) comprised primarily of hallucinatory experiences, and “Type 2” psychosis (7.2 %) with high conditional probabilities of multiple psychotic experiences. In our previous analysis of college-aged Kenyan students, LCA also resulted in a three-class solution, including a similar “Type 1” (12.7 %) and “Type 2” (3.5 %) psychosis pattern [27]. In the research literature, two other LCA studies of PLEs have been reported, both in adult populations [28, 29]. Using an identical psychosis screen as in our study, Gale et al. [28] found a three-class solution using in a general population survey (ages 16 and over) in New Zealand. The two psychotic classes found showed symptom distributions similar to that in our study, with a hallucinatory class (6.9 %) and a pan-psychotic class (0.2 %). In a study on American adults aged 15–54 years, Shevlin et al. [29] conducted LCA on items from a 13-item CIDI screen. These authors reported a resulting four class-solution, with a hallucinatory class (6 %), and two pan-psychotic classes with different symptom endorsement probabilities (high—1.8 %, and intermediate—5.9 %). Taken together, these studies indicate that across cultures and ages, predominantly hallucinatory psychotic experiences are more prevalent than those that also include delusions. Across studies, the reason for the disparity in the proportion of individuals in each class is unclear. The sampled populations were different, with other studies surveying older community samples. Cross-national differences in the distribution of reported PLE symptoms have also been found by other authors [26], and may reflect real prevalence differences or those resulting from cultural differences in interpreting survey questions.
There were only limited demographic data available for this study and no information on psychotic diagnosis or functioning. Our data however indicated that compared to the normative group, both Type 1 and Type 2 psychotic students had a higher frequency of males compared to females. Similarly, a predominance of males was reported in Kenyan young adults for both Type 1 and Type 2 psychosis [27]. However, other authors have reported a predominance of females in the hallucinatory group with pan-psychotic groups being gender neutral [29]. Gender differences across studies may result from age differences in the study populations, since studies involving older participants would be expected to have a greater proportion of females with PLEs due to their delayed onset of psychosis development. In our study, Type 2 psychotic individuals also appeared to be on average a year younger than the normal group, with Type 1 psychotic individuals intermediate between the two. While this is a small difference, it may be due to overendorsement of symptoms with younger age. Alternatively, it may indicate that individuals with psychopathology are more common in the lower academic grades, perhaps because of a tendency towards increased drop out rates with advanced educational attainment. Significant age effects were however not noted across LCA classes in adult studies of psychotic experiences [27, 29].
The prognostic significance of the two types of psychosis in children and adolescents is unclear. Previous research in adults suggests that individuals with pan-psychotic (Type 1) psychosis are more significantly impaired and in greater psychological distress than those with hallucinatory (Type 2) psychosis. Specifically, increased lifetime prevalence of anxiety, mood or substance use disorders has been reported in individuals in a pan-psychotic class compared to those in a hallucinatory class [28]. Similarly, Shevlin et al. [29] found that high probability pan-psychotic individuals had significantly higher rates of major depression, bipolar disorder, post-traumatic stress disorder, and substance/alcohol dependence compared to hallucinatory individuals. These authors also found that indices of distress or functionality, such as psychological trauma, having received mental health services, unemployment, or being in the lowest income category were greatest for the pan-psychotic group, although all groups had higher odds ratios compared to normative individuals [29]. Taken together, these findings suggest that the historical pattern of psychotic experiences can determine the overall severity of psychopathology. It provides evidence that Type 1 psychotic (i.e. hallucinatory) adults are less impaired than those with Type 2 psychotic (i.e. pan-psychotic) adults. However, it is uncertain if these conclusions can be extrapolated to children or adolescents. Self-reported psychotic experiences in children and adolescents have been associated with future psychotic disorders and impairment [20, 48]. Hallucinatory experiences in adolescents have also been related to impairment from non-psychotic disorders over time [49]. Future studies will be required to evaluate the association of psychiatric conditions and functionality in children, as well as longitudinal studies to evaluate if Type 2 psychosis may impart a greater risk to developing psychotic disorders or other more severe conditions than Type 1 psychosis. Such studies could aid the development of more targeted preventative interventions in those most at risk.
There are some limitations to our study. While short self-report questionnaires have been shown to have acceptable levels of accuracy and good predictive power in identifying PLEs in adolescents compared to clinical interviews [50], prevalence differences may be due in part to differences in how symptoms are assessed. There were also many students who did not indicate “yes” or “no” for all six items on the questionnaire, thus there may have been errors in our estimation of prevalence rates. For much of our analysis, items without a definite response were treated as negative for that particular experience. However, students’ responses to these items may have been a result of a lack of comprehension of some of these questions or due to paranoia or command hallucinations. In this scenario, it is conceivable that prevalence rates for individual items may have been underestimated. Alternatively, a lack of comprehension of specific questions may also have led to item overendorsement.
In summary, our studies indicate that PLEs occur commonly in Kenyan children and adolescents. Hallucinatory and pan-psychotic patterns of psychotic experiences were noted, which are comparable to those found in cross-national studies in adults. Studies evaluating functionality and distress associated with PLEs, as well as conversion rates to psychotic illness would provide valuable additional insight into the nature of risk in this particular population.
Summary
Studying PLEs in early life are important as they can indicate prodromal symptoms of psychotic disorders such as schizophrenia, and can facilitate early intervention. Previous studies using LCA in Kenyan and other populations have suggested there may be two classes of psychotic experiences, which have been termed “Type 1” (predominantly hallucinatory) and “Type 2” (pan-psychotic). In the current study, we investigated the prevalence and patterns of PLEs among children and adolescents in Kenya. 1,971 students from primary and secondary schools around Nairobi (aged 8–19) provided data from the psychosis screen of the CIDI. LCA was used to determine specific classes of psychotic experiences. We found that among all respondents, 22.1 % reported a lifetime history of a PLE, and 16.3 % reported this unrelated to sleep or drugs. Among PLEs, visual and auditory hallucinatory experiences were reported most frequently. Psychotic experiences were more common in males compared to females. LCA resulted in a three-class model comprised of a normative class (83.3 %), a predominately hallucinatory class (Type 1 psychosis: 9.6 %), and a pan-psychotic class (Type 2 psychosis: 7.2 %). These results indicate that PLEs are prevalent in children and adolescents, and the distributions of symptom clusters are similar to that found in adulthood. The relationship of specific PLEs to the future development of psychotic disorder, functional impairment or distress will require further study.
Footnotes
Conflict of interest The authors do not have any conflicts of interest and declare no financial interest from this study.
Contributor Information
Daniel Mamah, Email: mamahd@psychiatry.wustl.edu, Department of Psychiatry, Washington University School of Medicine, Box 8134, 660 S. Euclid, St. Louis, MO 63110, USA.
Akinkunle Owoso, Department of Psychiatry, Washington University School of Medicine, Box 8134, 660 S. Euclid, St. Louis, MO 63110, USA.
Anne W. Mbwayo, Africa Mental Health Foundation, Nairobi, Kenya
Victoria N. Mutiso, Africa Mental Health Foundation, Nairobi, Kenya
Susan K. Muriungi, Kenya Medical Training College, Nairobi, Kenya
Lincoln I. Khasakhala, Africa Mental Health Foundation, Nairobi, Kenya
Deanna M. Barch, Department of Psychiatry, Washington University School of Medicine, Box 8134, 660 S. Euclid, St. Louis, MO 63110, USA. Department of Psychology, Washington University, St. Louis, MO, USA. Department of Anatomy and Neurobiology, Washington University, St. Louis, MO, USA
David M. Ndetei, Africa Mental Health Foundation, Nairobi, Kenya. Department of Psychiatry, University of Nairobi, Nairobi, Kenya
References
- 1.Eaton WW, Romanoski A, Anthony JC, Nestadt G. Screening for psychosis in the general population with a self-report interview. J Nerv Ment Dis. 1991;179:689–693. doi: 10.1097/00005053-199111000-00007. [DOI] [PubMed] [Google Scholar]
- 2.van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 3.Varghese D, Scott J, McGrath J. Correlates of delusion-like experiences in a non-psychotic community sample. Aust NZJ Psychiatry. 2008;42:505–508. doi: 10.1080/00048670802050595. [DOI] [PubMed] [Google Scholar]
- 4.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- 5.Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. 2011;41:1–6. doi: 10.1017/S0033291710001005. [DOI] [PubMed] [Google Scholar]
- 6.Mittal VA, Dean DJ, Pelletier A, Caligiuri M. Associations between spontaneous movement abnormalities and psychotic-like experiences in the general population. Schizophr Res. 2011;132:194–196. doi: 10.1016/j.schres.2011.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macmanus D, Laurens KR, Walker EF, Brasfield JL, Riaz M, Hodgins S. Movement abnormalities and psychotic-like experiences in childhood: markers of developing schizophrenia? Psychol Med. 2012;42:99–109. doi: 10.1017/S0033291711001085. [DOI] [PubMed] [Google Scholar]
- 8.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–1031. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 9.Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res. 2002;54(1–2):59–65. doi: 10.1016/s0920-9964(01)00352-8. [DOI] [PubMed] [Google Scholar]
- 10.Stip E, Letourneau G. Psychotic symptoms as a continuum between normality and pathology. Can J Psychiatry. 2009;54:140–151. doi: 10.1177/070674370905400302. [DOI] [PubMed] [Google Scholar]
- 11.Fonseca-Pedrero E, Santarén-Rosell M, Lemos-Giráldez S, Paino M, Sierra-Baigrie S, Muñiz J. Psychotic-like experiences in the adolescent general population. Actas Esp Psiquiatr. 2011;39:155–162. [PubMed] [Google Scholar]
- 12.Laurens KR, Hodgins S, Maughan B, Murray RM, Rutter ML, Taylor EA. Community screening for psychotic-like experiences and other putative antecedents of schizophrenia in children aged 9–12 years. Schizophr Res. 2007;90:130–146. doi: 10.1016/j.schres.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Laurens KR, Hobbs MJ, Sunderland M, Green MJ, Mould GL. Psychotic-like experiences in a community sample of 8000 children aged 9 to 11 years: an item response theory analysis. Psychol Med. 2012;42(7):1495–1506. doi: 10.1017/S0033291711002108. [DOI] [PubMed] [Google Scholar]
- 14.Yung AR, Nelson B, Baker K, Buckby JA, Baksheev G, Cosgrave EM. Psychotic-like experiences in a community sample of adolescents: implications for the continuum model of psychosis and prediction of schizophrenia. Aust NZJ Psychiatry. 2009;43:118–128. doi: 10.1080/00048670802607188. [DOI] [PubMed] [Google Scholar]
- 15.McGee R, Williams S, Poulton R. Hallucinations in non-psychotic children. J Am Acad Child Adolesc Psychiatry. 2000;39:12–13. doi: 10.1097/00004583-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Yoshizumi T, Murase S, Honjo S, Kaneko H, Murakami T. Hallucinatory experiences in a community sample of Japanese children. J Am Acad Child Adolesc Psychiatry. 2004;43:1030–1036. doi: 10.1097/01.chi.0000126937.44875.6b. [DOI] [PubMed] [Google Scholar]
- 17.Rössler W, Riecher-Rössler A, Angst J, Murray R, Gamma A, Eich D, van Os J, Gross VA. Psychotic experiences in the general population: a twenty-year prospective community study. Schizophr Res. 2007;92:1–14. doi: 10.1016/j.schres.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edelsohn GA, Rabinovich H, Portnoy R. Hallucinations in nonpsychotic children: findings from a psychiatric emergency service. Ann NY Acad Sci. 2003;1008:261–264. doi: 10.1196/annals.1301.028. [DOI] [PubMed] [Google Scholar]
- 20.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 21.Jardri R, Delion P, Goëb J-L. Hallucinations in children and adolescents: diagnostic and treatment strategies. Presse Med. 2010;39:420–430. doi: 10.1016/j.lpm.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Kinoshita Y, Shimodera S, Nishida A, Kinoshita K, Watanabe N, Oshima N, Akechi T, Sasaki T, Inoue S, Furukawa TA, Okazaki Y. Psychotic-like experiences are associated with violent behavior in adolescents. Schizophr Res. 2011;126:245–251. doi: 10.1016/j.schres.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 23.Yung AR, Buckby JA, Cosgrave EM, Killackey EJ, Baker K, Cotton SM, McGorry PD. Association between psychotic experiences and depression in a clinical sample over 6 months. Schizophr Res. 2007;91:246–253. doi: 10.1016/j.schres.2006.11.026. [DOI] [PubMed] [Google Scholar]
- 24.Armando M, Nelson B, Yung AR, Ross M, Birchwood M, Girardi P, Fiori Nastro P. Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr Res. 2010;119:258–265. doi: 10.1016/j.schres.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Mackie CJ, Castellanos-Ryan N, Conrod PJ. Developmental trajectories of psychotic-like experiences across adolescence: impact of victimization and substance use. Psychol Med. 2011;41:47–58. doi: 10.1017/S0033291710000449. [DOI] [PubMed] [Google Scholar]
- 26.Nuevo R, Chatterji S, Verdes E, Naidoo N, Arango C, Ayuso-Mateos JL. The continuum of psychotic symptoms in the general population: a cross-national study. Schizophr Bull. 2012;38(3):475–485. doi: 10.1093/schbul/sbq099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ndetei DM, Muriungi SK, Owoso A, Mutiso VN, Mbwayo AW, Khasakhala LI, Barch DM, Mamah D. Prevalence and characteristics of psychotic-like experiences in Kenyan youth. Psychiatry Res. 2012;196(2–3):235–242. doi: 10.1016/j.psychres.2011.12.053. [DOI] [PubMed] [Google Scholar]
- 28.Gale CK, Wells JE, McGee MA, Browne MAO. A latent class analysis of psychosis-like experiences in the New Zealand Mental Health Survey. Acta Psychiatr Scand. 2011;124:205–213. doi: 10.1111/j.1600-0447.2011.01707.x. [DOI] [PubMed] [Google Scholar]
- 29.Shevlin M, Murphy J, Dorahy MJ, Adamson G. The distribution of positive psychosis-like symptoms in the population: a latent class analysis of the National Comorbidity Survey. Schizophr Res. 2007;89:101–109. doi: 10.1016/j.schres.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr Res. 1998;32:361–368. doi: 10.1016/s0022-3956(98)00021-1. [DOI] [PubMed] [Google Scholar]
- 31.McCutcheon AL. Latent class analysis. Sage Publications, Inc; Newbury Park: 1987. [Google Scholar]
- 32.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 33.Hagenaars JA, McCutcheon AL. Applied latent class analysis. Cambridge University Press; Cambridge: 2002. [Google Scholar]
- 34.Magidson J, Vermunt JK. Latent class models. In: Kaplan D, editor. The SAGE handbook of quantitative methodology for the social sciences. Sage Publications Inc; Thousand Oaks, CA: 2004. [Google Scholar]
- 35.Ochoa S, Haro JM, Torres JV, Pinto-Meza A, Palacín C, Bernal M, Brugha T, Prat B, Usall J, Alonso J, Autonell J. What is the relative importance of self reported psychotic symptoms in epidemiological studies? Results from the ESEMeD–Catalonia Study. Schizophr Res. 2008;102:261–269. doi: 10.1016/j.schres.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 36.Häfner H, Maurer K, Löffler W, Van der Heiden W, Munk-Jørgensen P, Hambrecht M, Riecher-Røssler A. The ABC Schizophrenia Study: a preliminary overview of the results. Soc Psychiatry Psychiatr Epidemiol. 1998;33:380–386. doi: 10.1007/s001270050069. [DOI] [PubMed] [Google Scholar]
- 37.Gureje O, Olowosegun O, Adebayo K, Stein DJ. The prevalence and profile of non-affective psychosis in the Nigerian Survey of Mental Health and Wellbeing. World Psychiatry. 2010;9:50–55. doi: 10.1002/j.2051-5545.2010.tb00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leiderman EA. Psychotic-like experiences in the general population of Buenos Aires city. Schizophr Res. 2011;130:291–292. doi: 10.1016/j.schres.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 39.Mojtabai R. Psychotic-like experiences and interpersonal violence in the general population. Soc Psychiatry Psychiatr Epidemiol. 2006;41:183–190. doi: 10.1007/s00127-005-0020-4. [DOI] [PubMed] [Google Scholar]
- 40.Barragan M, Laurens KR, Navarro JB, Obiols JE. Psychotic-like experiences and depressive symptoms in a community sample of adolescents. Eur Psychiatry. 2011;26:396–401. doi: 10.1016/j.eurpsy.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 41.Morgan C, Fisher H, Hutchinson G, Kirkbride J, Craig TK, Morgan K, Dazzan P, Boydell J, Doody GA, Jones PB, Murray RM, Leff J, Fearon P. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta Psychiatr Scand. 2009;119:226–235. doi: 10.1111/j.1600-0447.2008.01301.x. [DOI] [PubMed] [Google Scholar]
- 42.Alptekin K, Ulas H, Akdede BB, Tümüklü M, Akvardar Y. Prevalence and risk factors of psychotic symptoms: in the city of Izmir, Turkey. Soc Psychiatry Psychiatr Epidemiol. 2009;44:905–910. doi: 10.1007/s00127-009-0012-x. [DOI] [PubMed] [Google Scholar]
- 43.Jenkins R, Mbatia J, Singleton N, White B. Prevalence of psychotic symptoms and their risk factors in urban Tanzania. Int J Environ Res Public Health. 2010;7:2514–2525. doi: 10.3390/ijerph7062514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scott J, Welham J, Martin G, Bor W, Najman J, O’Callaghan M, Williams G, Aird R, McGrath J. Demographic correlates of psychotic-like experiences in young Australian adults. Acta Psychiatr Scand. 2008;118:230–237. doi: 10.1111/j.1600-0447.2008.01214.x. [DOI] [PubMed] [Google Scholar]
- 45.Hambrecht M, Maurer K, Häfner H, Sartorius N. Transnational stability of gender differences in schizophrenia? An analysis based on the WHO study on determinants of outcome of severe mental disorders. Eur Arch Psychiatry Clin Neurosci. 1992;242:6–12. doi: 10.1007/BF02190336. [DOI] [PubMed] [Google Scholar]
- 46.Gureje O. Gender and schizophrenia: age at onset and sociodemographic attributes. Acta Psychiatr Scand. 1991;83:402–405. doi: 10.1111/j.1600-0447.1991.tb05564.x. [DOI] [PubMed] [Google Scholar]
- 47.Loranger AW. Sex difference in age at onset of schizophrenia. Arch Gen Psychiatry. 1984;41:157–161. doi: 10.1001/archpsyc.1984.01790130053007. [DOI] [PubMed] [Google Scholar]
- 48.Welham J, Scott J, Williams G, Najman J, Bor W, O’Callaghan M, McGrath J. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychol Med. 2009;39:625–634. doi: 10.1017/S0033291708003760. [DOI] [PubMed] [Google Scholar]
- 49.Dhossche D, Ferdinand R, Van der Ende J, Hofstra MB, Verhulst F. Diagnostic outcome of self-reported hallucinations in a community sample of adolescents. Psychol Med. 2002;32:619–627. doi: 10.1017/s003329170200555x. [DOI] [PubMed] [Google Scholar]
- 50.Kelleher I, Harley M, Murtagh A, Cannon M. Are screening instruments valid for psychotic-like experiences? A validation study of screening questions for psychotic-like experiences using in-depth clinical interview. Schizophr Bull. 2011;37:362–369. doi: 10.1093/schbul/sbp057. [DOI] [PMC free article] [PubMed] [Google Scholar]