Abstract
Atherosclerosis is an inflammatory disease, and several inflammatory biomarkers, such as C-reactive protein, have been used to predict the risk of coronary heart disease. High white blood cell count is a strong and independent predictor of coronary risk in patients of both sexes, with and without coronary heart disease. A high number of white blood cells and their subtypes (for example, neutrophils, monocytes, lymphocytes, and eosinophils) are associated with the presence of coronary heart disease, peripheral arterial disease, and stroke. The coronary heart disease risk ratios associated with a high white blood cell count are comparable to those of other inflammatory markers, including C-reactive protein. In addition, other components of the complete blood count, such as hematocrit and the erythrocyte sedimentation rate, also are associated with coronary heart disease, and the combination of the complete blood count with the white blood cell count can improve our ability to predict coronary heart disease risk. These tests are inexpensive, widely available, and easy to order and interpret. They merit further research.
Key words: Atherosclerosis, biological markers/blood, complete blood count, coronary artery disease, coronary heart disease, inflammation, leukocyte count, white blood cell count
Coronary heart disease (CHD) is the leading cause of death in the United States, and it is estimated that the prevalence of cardiovascular disease will increase by approximately 10% over the next 20 years.1,2 During the past 2 decades, extensive research has established that atherosclerosis is an inflammatory disease,3 a finding that has offered new possibilities for predicting CHD risk. The presence of many types of inflammatory biomarkers, most notably high-sensitivity C-reactive protein (CRP), have been found to be consistent predictors of CHD events.4 Although an increasing number of novel inflammatory biomarkers are being studied in this context, many offer little improvement in the current risk-prediction models.5 Whereas measurement of CRP and lipoprotein-associated phospholipase A2 (Lp-PLA2) have shown promise as predictors of CHD events,5 most of the other newly introduced inflammatory risk markers are expensive to test, are not readily available, lack standardization, and have not been confirmed by multiple prospective studies.
We have previously shown that a growing body of evidence supports the usefulness of the white blood cell (WBC) count as a predictor of future coronary events.6 Herein, we review the most recent data on the use of the WBC count and other components of the complete blood count (CBC) to predict CHD risk. An elevated WBC is a well-recognized indicator of inflammation.6 The total number of WBCs and each subtype (for example, neutrophils, monocytes, lymphocytes, and eosinophils) have been implicated as predictors of CHD.6 Nearly all of the cellular elements in the blood, including WBCs, red blood cells (RBCs), and platelets, are involved in the underlying pathogenesis of atherosclerosis.3,6 These markers not only play a role in the development of CHD in asymptomatic patients, but they predict recurrent events and death in patients who already have CHD.7,8 In addition to the cellular components, an elevated erythrocyte sedimentation rate (ESR) has been shown to be a weak prognostic factor in CHD patients.9–11
Total White Blood Cell Count and Coronary Heart Disease
The relationship between white blood cell count and CHD was first suggested more than 80 years ago.12 Results from multiple studies of patients with and without CHD at baseline have indicated that the WBC count can be used to predict the incidence of coronary events.13–25
A high WBC count also has been shown to be predictive of future cardiovascular events in individuals who were disease free at baseline (Fig. 1 14–25).6 Multiple studies have shown that a high WBC count is associated with increased mortality rates in patients who present with unstable angina pectoris,26,27 acute coronary syndromes (ACS),28 and acute myocardial infarction (MI),29–32 and in patients who undergo percutaneous coronary interventions (PCIs)33 or coronary artery bypass grafting (CABG) (Fig. 2 8,29,32,34–40).34–36,41 Moreover, elevated total WBC and neutrophil and monocyte counts are associated with cerebral ischemia and stroke.42–45 In 2004, Grau and colleagues38 showed that, in patients who had had an ischemic stroke or MI or who had peripheral arterial disease (PAD), there was a relationship between high WBC counts and the recurrence of vascular events.
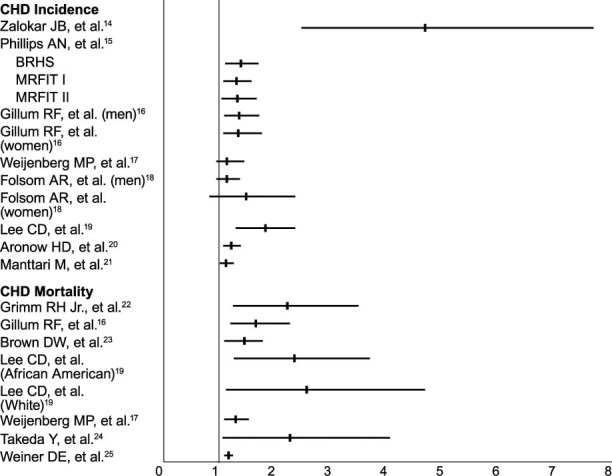
Fig. 1 The 95% confidence interval and point estimate for coronary heart disease (CHD) incidence and CHD mortality in patients free of CHD. The solid vertical line denotes a relative risk of 1 (no effect); horizontal lines represent 95% confidence interval; and tick marks show point estimates for relative risk.
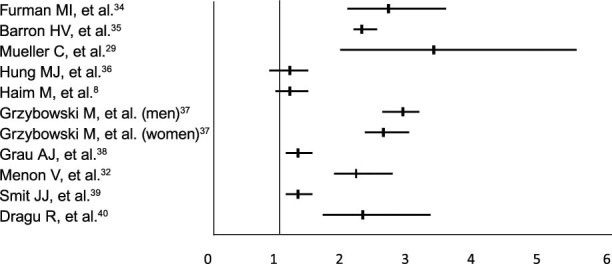
Fig. 2 The 95% confidence interval and point estimate for coronary heart disease death in patients with acute coronary syndromes, as determined on the basis of total white blood cell count.
An increase in quartiles of WBC count from baseline over 24 hours after an MI episode has been correlated with an increase in all-cause death after an MI,46 and a recent subanalysis of the Ongoing Tirofiban In Myocardial Infarction Evaluation (On-TIME) trial showed that an increase in WBC count (defined as WBC count after 6 or 24 hours minus the WBC count on admission) was a significant predictor of death after PCI.39 In an analysis of 900 patients in the Stent Primary Angioplasty in Myocardial Infarction (Stent PAMI) trial, investigators found that an elevated WBC count upon hospital admission (highest tertile, ≥12) had a strong independent association with reinfarction at 1 year.47 Moreover, in a subanalysis using data from the Atherosclerotic Risk in Communities (ARIC) and Cardiovascular Health Study that compared patients with and without stages 3 to 4 chronic kidney disease, investigators found that elevated inflammatory markers, including the WBC count, were associated with an increase in adverse cardiac events and death.25 They also found that, although the risk is additive, the synergy between inflammation and chronic kidney disease was not statistically significant.25 Finally, results from a meta-analysis of 5,337 CHD patients from 7 large studies showed that a high WBC count was associated with a risk ratio of 1.4 (95% CI, 1.3–1.5) for CHD.48 This risk ratio is comparable to those seen with other novel inflammatory markers associated with atherosclerosis, including CRP.49
Therefore, the relationship between white blood cell count and CHD is strong, consistent, dose-dependent, independent, biologically plausible, and coherent with the current paradigm of the inflammatory origin of atherosclerosis. The association between WBC count and CHD has been consistently observed in different populations with varying degrees of baseline risk—in asymptomatic individuals and symptomatic patients. The association between the WBC count and CHD appears to be independent of other traditional coronary risk factors, including smoking. Although smoking is associated with leukocytosis, studies have shown that the predictive value of a high WBC count for CHD is independent of whether patients are smokers.6
Differential White Blood Cell Count and Coronary Heart Disease
Elevated levels of almost all subtypes of WBCs, including eosinophils,50,51 monocytes,52–54 neutrophils,38,55–60 and lymphocytes (an inverse relationship),52,61–63 have been associated with increased risk of CHD (Fig. 3 16,38,40,52,55,57,64).6 In a large, disease-free patient cohort from the Adult Health Study (AHS) of Hiroshima and Nagasaki, results showed a relationship between the total WBC count, including the eosinophil, neutrophil, and monocyte counts, and the incidence of CHD.50 Results from the Paris Prospective Study II showed an increased risk of CHD in patients with high monocyte counts.52 In the Caerphilly and Speedwell studies, increased coronary risk was associated with high neutrophil, eosinophil, lymphocyte, monocyte, or basophil counts.55 A prospective study40 of 1,037 patients who experienced an acute MI showed that elevated total WBC, monocyte, and neutrophil counts and low lymphocyte counts were independent predictors of all-cause death. The investigators in that study found that adding the neutrophil count to models of total WBC, monocyte, and lymphocyte counts improved the models' predictive ability.40 Furthermore, Papa and colleagues65 found that higher neutrophil-lymphocyte counts in patients with angiographically documented coronary artery disease (CAD) increased the risk of cardiac death within a 36-month follow-up period.
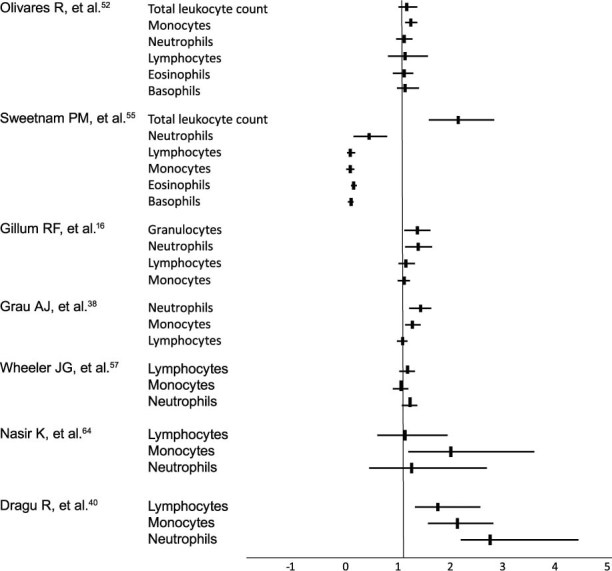
Fig. 3 The 95% confidence interval and point estimate for coronary heart disease incidence and mortality rate in disease-free persons and in patients with acute coronary syndromes, as determined on the basis of white blood cell subtypes.
In a large cross-sectional study of middle-aged, asymptomatic participants in the 1999–2002 National Health and Nutrition Examination Survey (NHANES), elevated monocyte and neutrophil counts, along with elevated CRP and fibrinogen levels, were associated with the presence of subclinical PAD.64 In another study of patients with PAD, only an elevated neutrophil count was predictive of an increased risk of major adverse cardiovascular events or death within the study's 20-month follow-up period.66 However, a study using intravascular ultrasonography showed a direct relationship between the monocyte count and an increase in the volume of atherosclerotic plaque in the arteries of patients who have had an acute MI.67 In addition, a higher prevalence of monocytosis has been reported in patients with angiographically documented CAD.54 When the relationship between peripheral monocyte count and coronary vasospasm was examined in 180 patients with chest pain, an elevated monocyte count was strongly associated with coronary vasospasm.68 A more recent (2008) prospective, observational study in asymptomatic adults showed that, of all the WBC subtypes, the monocyte count had the strongest independent relationship with CHD risk, as estimated by the Framingham and SCORE calculations.69 Moreover, several studies have shown that the WBC70,71 and, more specifically, the monocyte count are independent predictors of subclinical carotid plaque deposition and carotid intima medial thickening.71,72
In a genetic analysis of the inflammatory role of eosinophils, Gudbjartsson and colleagues73 undertook a genome-wide association scan of the blood of more than 9,000 Icelanders to determine the sequence variants affecting eosinophil counts and to evaluate the association with inflammatory disorders. The analysis revealed that a single nucleotide polymorphism at 12q24, in SH2B3, had a significant association (P < 0.002) with MI in their scan data set and was consistent with 6 replication sets of European ancestry, with an odds ratio of 1.13 (95% CI, 1.08–1.18).73 Further studies are needed to evaluate the consistency of the relationship of WBC subtypes and cardiovascular risk. It should be noted that most of the above-mentioned studies have excluded subjects with hematologic disorders, such as chronic lymphocytic leukemia or aplastic disorders, and the relationship between WBCs and CHD requires separate investigation in those situations.
White Blood Cell Count versus High-Sensitivity C-Reactive Protein as Coronary Heart Disease Risk Markers
High-sensitivity C-reactive protein is increasingly used for coronary risk prediction in clinical settings. With the knowledge that neither CRP nor the WBC count is the “perfect” screening tool, it is noteworthy that the WBC count is comparable in efficacy to CRP for predicting CHD risk (Fig. 4 74–80). Both tests are nonspecific markers of systemic inflammation and have comparable power for predicting coronary events. Meta-analyses by Danesh and colleagues48,49 found that the WBC had an odds ratio of 1.4 (95% CI, 1.3–1.5) and the CRP had an odds ratio of 1.45 (95% CI, 1.2–1.6).
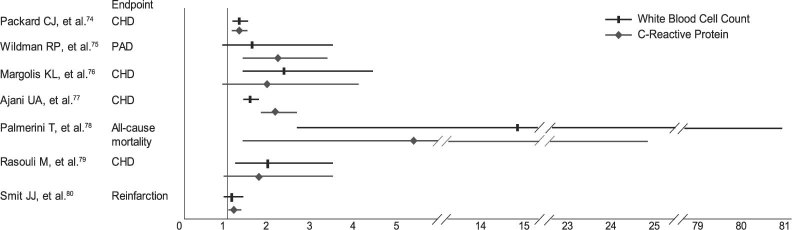
Fig. 4 The 95% confidence interval and point estimate for coronary heart disease (CHD) event risk based on white blood cell count versus C-reactive protein.
PAD = peripheral arterial disease
Unfortunately, there are few head-to-head comparisons of WBC count with CRP for CHD risk prediction (Fig. 4). In a subset of the West of Scotland Coronary Prevention Study, univariate analysis showed that both the WBC count and the CRP were risk predictors of coronary events, with respective risk ratios of 1.15 (95% CI, 1.02–1.31) and 1.21 (95% CI, 1.06–1.31).74 However, multivariate analysis showed that only Lp-Pla2 had significant predictive ability for the risk of a coronary event, with a risk ratio of 1.18 (95% CI, 1.05–1.33).74 In a study of the relationship between inflammation and PAD that used data from the 1999–2002 NHANES, the multivariate adjusted odds ratio of PAD was increased for the highest quartiles of both WBC count (OR, 1.67; 95% CI, 0.84–3.31) and CRP (OR, 2.14; 95% CI, 1.41–3.25), compared with the lowest quartiles.75 These relations remained significant across different subgroups that were used to evaluate the influence of sex, obesity, and diabetes mellitus.75
In a fully adjusted model from the Women's Health Initiative Observational Study,76 a comparison of WBC counts in the first and 4th quartiles showed that women in the 4th quartile were at higher risk for CHD events: the odds ratio was 2.36 (95% CI, 1.33–4.19), which was higher than the odds ratio of 1.95 (95% CI, 0.95–4.01) for women with elevated CRP levels. In that study, elevated WBC counts and CRP levels synergistically predicted CHD risk, with an odds ratio of 6.8 (95% CI, 2.7–16.9).76 Another study, from the Centers for Disease Control and Prevention (CDC), evaluated 8,355 participants in the 1999–2002 NHANES for lifestyle and emerging risk factors that could contribute to participants' Framingham risk score. Results of the study showed that an elevated WBC count (>7 ×109/L, the population median) was associated with an odds ratio of 1.49 (95% CI, 1.32–1.67) of the highest 10-year CHD risk—as was an elevated CRP level, with an odds ratio of 2.10 (95% CI, 1.74–2.53).77 In addition, in a study of outcomes after patients underwent stent placement for unprotected left main coronary artery stenosis, Palmerini and colleagues78 found that WBC counts and CRP levels were comparable in predicting outcomes at 9 months.78
Conversely, in a study of 270 patients with angiographically documented CAD, results showed that increases in the total WBC count and the neutrophil and eosinophil counts all were significantly associated not only with the presence of CAD but also with its severity, as determined by the number and extent of lesions, whereas levels of CRP and the ESR were not.79 Similarly, in a study of patients undergoing diagnostic coronary angiography, the WBC count was independently associated with angiographically documented CAD and multivessel disease, whereas CRP values, tissue inhibitor of metalloproteinases-1 (TIMP-1), and the ESR were not.81
However, in a subanalysis of the On-TIME trial that evaluated early versus late administration of tirofiban during primary PCI for ST-elevation myocardial infarction (STEMI), results showed that the baseline CRP value was a significant predictor of re-infarction and 1-year death, with an odds ratio of 1.03 (95% CI, 1.01–1.05; P = 0.012), whereas the baseline WBC count was not significantly associated with worse outcomes, with an odds ratio of 1.09 (95% CI, 0.96–1.23; P = 0.202).80 Kruk and colleagues82 also evaluated patients with STEMI who underwent primary PCI and found that elevated WBC counts and CRP values were independent predictors of in-hospital death.82
In a study of patients who presented at the emergency department with chest pain suggestive of ACS, both the WBC counts and the CRP values were associated with a diagnosis of ACS upon hospital discharge; however, multivariate analysis showed that only the WBC count was actually associated with the presence of ACS, with an odds ratio of 20.9 (95% CI, 3.7–19.5).83 In a prospective cohort study of 128 patients with angina pectoris,84 investigators found that WBC counts and CRP levels were significantly higher in patients with unstable angina pectoris than in patients with stable angina (P < 0.0001) and that the circulating level of CRP was strongly associated with the clinical setting of unstable angina, with an odds ratio of 1.56 (95% CI, 1.23–2.0).
Consequently, it appears that both tests are useful in different populations and among men and women and that these tests have comparable weaknesses and strengths in predicting coronary risk. However, the test for WBC count is less expensive and more widely available than is the test for CRP. Obviously, a high WBC count, like other markers of risk such as high cholesterol level and CRP, is not synonymous with the presence of CHD and is one of multiple risk markers used to predict the risk of CHD. Similarly, many subjects with cardiovascular disease have normal WBC counts.
Effect of Statins on White Blood Cell Count
Statins are known to reduce cardiovascular events and related inflammatory markers,85 but they also reduce the WBC count. In a study of 1,246 patients with angiographically documented CAD, the use of statins was associated not only with lower WBC counts, but also with reduced levels of CRP, fibrinogen, and von Willebrand factor.86 Lower WBC counts and lower values of other inflammatory markers have also been seen in CHD patients who take statins, even in the absence of changes in total cholesterol, low-density-lipoprotein cholesterol (LDL-C), high-density-lipoprotein cholesterol (HDL-C), and triglyceride levels.87 In the National Registry of Myocardial Infarction (NRMI)-4 study, the WBC count was an independent predictor of in-hospital death from acute MI and was lower in patients who were taking statins or aspirin.37 Statin use is also associated with a decrease in the neutrophil count in patients with existing peripheral vascular disease.88
In a 6-month prospective study of patients with stable CAD, pravastatin significantly lowered the WBC count (8.9% vs baseline; P < 0.01), and multivariate regression analysis showed that the change in WBC count was an independent predictor of coronary plaque regression (14% reduction vs baseline; P < 0.0001).89 In the Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) study,90 in patients with stable CAD, the baseline WBC count was associated with greater CHD death in patients who were randomly assigned to receive a placebo, but not in patients given pravastatin. The number of coronary deaths and other cardiac outcomes that were prevented in the statin arm of the study increased, as did baseline WBC quartiles. The WBC count was a stronger predictor of treatment benefit than was the ratio of total cholesterol to HDL-C. Moreover, after statin treatment, the WBC count decreased at 1-year follow-up and remained stable thereafter.90
Beyond Leukocytes: Use of the Complete Blood Count to Predict Coronary Heart Disease Risk
Other components of the CBC, such as the RBC and platelet counts and hemoglobin and hematocrit values, also are associated with CHD and can be used in combination with the WBC count to predict coronary risk. Few studies, however, have examined the usefulness of combining multiple CBC elements to predict CHD risk. According to one such study by Ronnow and colleagues,91 a simple CBC-derived risk score comprising the hematocrit and WBC and platelet counts could be used to predict death in a meaningful way; but an expanded CBC-derived risk score comprising the hematocrit, mean corpuscular volume (MCV), red cell distribution width (RDW), mean corpuscular hemoglobin concentration, and platelet and WBC counts provided substantially greater predictive value. Predictive ability was further improved by adjustment for age, sex, and other traditional risk factors.91 In another study, the same group showed that in patients with angiographically documented CAD, the total WBC count was an independent predictor of death or MI.62 In these patients, good predictive power was provided by high neutrophil or low lymphocyte counts, but the greatest risk prediction was achieved by using the neutrophil-to-lymphocyte ratio.62
Gibson and colleagues92 found that, in patients undergoing CABG, the preoperative WBC count was not a predictor of death during their 3.6 years of follow-up, but that the neutrophil-lymphocyte count was a significant predictor of both cardiovascular and all-cause death, especially in the highest quartile (hazard ratio, 2.09; 95% CI, 1.54–2.84).92 In an extension of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), Spencer and colleagues93 screened 383 patients with hypertension to determine whether there was a relationship between hematologic factors and global measures of cardiovascular risk. They found that elevated WBC counts and increased levels of fibrinogen and von Willebrand factor significantly correlated with a higher Framingham 10-year CHD risk score and were independent predictors of Framingham CHD risk.93 A lower hematocrit significantly correlated with both the Pocock and Framingham 5-year cardiovascular risk scores.93
Anderson and colleagues94 evaluated the predictive ability of the CBC in a prospective cohort of 29,526 patients undergoing coronary angiography and found that the CBC score had discriminatory predictive ability for all-cause death at 30 days, with an area under the curve of 0.75. The age- and sex-adjusted CBC model had an area under the curve of 0.78. In addition, the CBC score showed strong predictive ability at 30 days and at 1, 5, and 10 years when a scalar risk score incorporating age and sex was used (linear trend, P < 0.001).94
Red Blood Cell Count and Coronary Heart Disease Risk
Several factors related to RBCs are associated with CHD, including hemoglobin levels and the hematocrit, RDW, and ESR95; however, there are not enough data to suggest an association between the RBC count and cardiovascular disease. Although polycythemia vera is associated with an increased risk of macrovascular events,96 elevated RBC counts within the upper limits of normal have been reported to have only weak or no association with cardiovascular risk.97
Hematocrit and Coronary Heart Disease Risk
Several studies have shown a relationship between the hematocrit and incident cardiovascular events in patients who have had an MI,98,99 in those with PAD,100 and in asymptomatic individuals.101–109 However, results of some studies have not shown a significant relationship between hematocrit and CHD risk.103,110,111 In fact, while most studies of different patient populations do show an association between increased hematocrit and increased risk of CHD, the observed risk ratios are generally low, and, therefore, the clinical usefulness of hematocrit alone is unclear.
A meta-analysis of 19 prospective studies of hematocrit and CHD risk showed a pooled odds ratio of 1.16 (95% CI, 1.05–1.29) in disease-free subjects, and a risk ratio of 1.81 (95% CI, 1.19–2.76) in patients with vascular disease.95 The same meta-analysis also dealt with the value of viscosity and the ESR for CHD risk prediction. The investigators reported a risk ratio of 1.57 (95% CI, 1.34–1.85) for the top tertile of plasma viscosity in population-based studies, and a risk ratio of 2.6 (95% CI, 1.64–4.12) for patients with vascular disease.95 Results of a more recent study show that the hematocrit-to-blood viscosity (Hct-BV) ratio had significant negative correlation with the frequency of hospital admission and that a lower Hct-BV ratio was associated with a greater likelihood of cardiac death in CHD patients.112
Uncertainty remains in regard to the effectiveness of blood transfusion in correcting a low hematocrit in ACS patients.113 Although an observational study by Wu and colleagues114 suggests that blood transfusion can improve short-term survival in patients who are anemic at presentation, Hebert and colleagues115 found no such benefit, while others116–118 actually report a harmful effect. A retrospective cohort study (2006) suggests that higher mortality rates in women after CABG are due in part to the more common occurrence of blood transfusions in women, leading to immunomodulation and an increased risk of infection and death after bypass surgery.119 Results from a pooled study of ACS patients from 3 large international trials showed an increased mortality rate after blood transfusion in patients who developed moderate-to-severe bleeding, anemia, or both, during hospitalization.113 In another analysis involving a subset of 44,242 patients, investigators found an inverse relationship between in-hospital death and nadir hematocrit in non-STEMI patients.120 They also found that transfusions were related to significantly increased in-hospital death in the highest hematocrit quartile (Hct >30).120 Therefore, it appears that well-designed, randomized, controlled trials of transfusion strategies are needed to provide clear guidelines with regard to blood transfusion in ACS patients. Until then, a cautious approach is warranted in the use of blood transfusion in these patients.
The RDW, a numerical measure of the variability of the size of circulating erythrocytes, is significantly associated with an increased risk of all-cause death, and specifically with death secondary to cardiovascular disease in cross-sectional studies of the population of the United States.121,122 In addition, the RDW is an independent predictor of death in patients who have had previous MIs123 or stroke124 and in men referred for coronary angiography.125
Erythrocyte Sedimentation Rate and Coronary Heart Disease Risk
Although the ESR varies among elderly patients, it has a positive correlation with several CHD risk factors, including age, sex, smoking, systolic blood pressure, total cholesterol levels, heart rate, body mass index, diabetes, alcohol consumption, and fibrinogen, hemoglobin, and albumin levels.126–129 After multivariate adjustment, the ESR is an independent and strong short- and long-term predictor of CHD death.128 In young subjects, a moderate but persistent elevation in the ESR has been associated with an increased risk of incident MI.130 Other conditions associated with a persistently elevated ESR include chronic infectious states, renal failure, rheumatoid arthritis, and chronic bronchitis.131 In the Stockholm Prospective Study, there was a positive and independent relationship between the ESR and fatal MI in asymptomatic men and women,132 but in NHANES I, the ESR was a risk factor for fatal MI only in men.10 In the Reykjavik Study, the ESR was an independent long-term predictor of CHD and death due to stroke in both men and women.9 Another study found that the ESR was related to the extent of coronary atherosclerosis on angiography and was a predictor of cardiac death in men with ischemic heart disease.129 Finally, a meta-analysis of 4 population-based studies showed that an ESR in the top third tertile yielded a risk ratio of 1.33 (95% CI, 1.15–1.54), compared with an ESR in the bottom tertile.95
Platelets and Coronary Heart Disease Risk
High platelet counts—such as those seen with hematologic neoplasms—are clearly associated with an increased risk of thrombosis; however, the effect of increased platelet numbers that are still within physiologic ranges remains unclear. A limited number of studies have shown that high platelet counts and a rapid platelet-aggregation response are associated with increased long-term coronary death.133 Conversely, a low platelet count in the presence of an increased mean platelet volume after ischemic cerebral infarction is also associated with increased mortality rate.134 In a cross-sectional study of patients undergoing coronary angiography, the mean platelet volume was higher in MI patients than in control patients, and stable angina pectoris correlated with the extent of CHD.135
Other studies suggest that platelet counts and aggregation that are within physiologic range are not related to CHD events.136 Khandekar and colleagues137 found a significant increase in platelet volume indices, mean platelet volume, and platelet distribution width in patients with unstable angina or acute MI, compared with stable CHD patients and healthy matched control patients.137
It appears that the role of platelets in the pathogenesis of CHD is due mainly to their functional properties and their interaction with plasma and tissue factors; only a small proportion of their effect—if any—is related to their absolute number. The small number of related positive studies may be the result of a publication bias toward the withholding of negative findings.
Potential Mechanisms
The effect of leukocytosis on CHD can be explained by multiple mechanisms; however, the inflammatory basis of atherosclerosis remains the cornerstone of this relation. Atherosclerotic lesions are inflammatory in nature, occur predominantly in large- and medium-sized arteries, and develop early in life.3 Leukocytosis can be considered a marker of inflammatory changes in atherosclerotic lesions, because leukocytes play a key role in the initiation and progression of the disease. In terms of ACS pathophysiology, leukocytes themselves are directly responsible for myocardial injury. Leukocytes release cytokines, bringing about further macrophage recruitment and the proliferation of smooth muscle cells within the vascular wall. In addition, protease secretion leads to endothelial damage of the coronary vessels, exposing thrombogenic collagen and predisposing the vessels to thrombus formation. Phagocytes release myeloperoxidase, which generates reactive oxygen species that are involved in the generation and progression of atherosclerosis and that contribute to the development of plaque instability in acute MI.31
A 2007 study has linked high WBC counts to the presence of vulnerable plaque.138 The investigators used optical coherence tomography to visualize lesions in patients undergoing coronary catheterization. An elevated baseline WBC count correlated with the macrophage density of the visualized plaque (r = 0.483; P = 0.001), and it was shown that patients with thin-cap fibroatheromas had higher WBC counts than did those without thin-cap fibroatheromas (11 vs 7.9; P = 0.007).138 Other studies139–148 have shown that leukocytes also play an important role in the pathogenesis of myocardial injury through multiple mechanisms, such as vessel-plugging, decreased perfusion, and abnormal WBC aggregation.
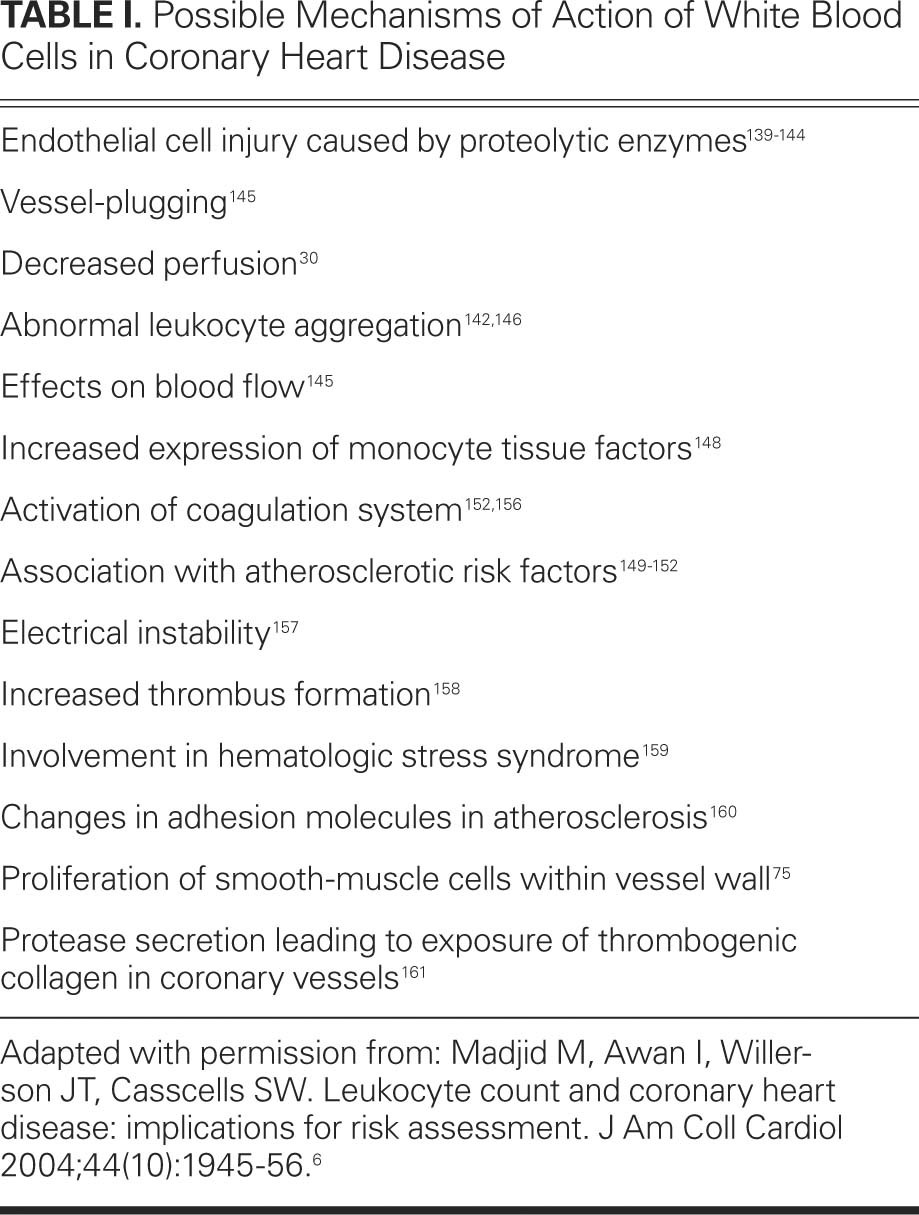
Elevated WBC counts are associated with several coronary risk factors, including smoking, elevated serum triglyceride and cholesterol levels, clotting factors, body mass index, obesity, and diastolic blood pressure.149–152 Leukocytosis also is associated with several disorders that characterize the metabolic syndrome153,154 and with micro- and macrovascular complications in patients with diabetes.155 The different mechanisms by which leukocytosis might affect CHD are listed in Table I.30,75,139–146,148–152,156–161
TABLE I. Possible Mechanisms of Action of White Blood Cells in Coronary Heart Disease
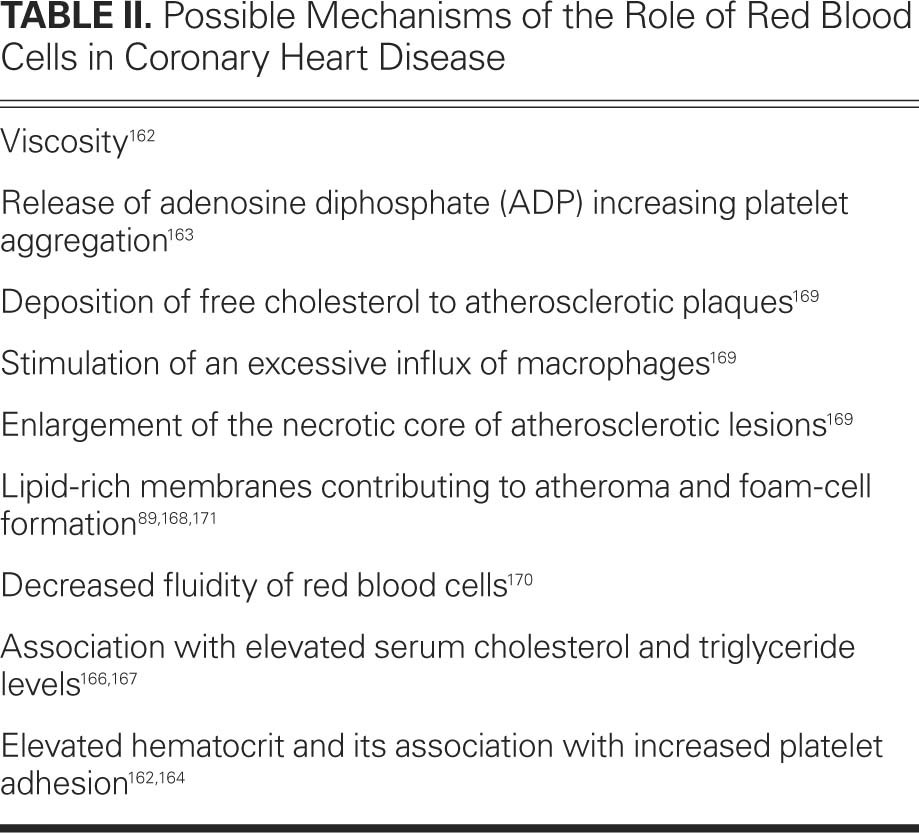
Elevated RBC counts and hematocrit are associated with rheologic effects, such as increased viscosity, which is a risk factor for coronary events.162 The adenosine diphosphate released from the RBCs enhances platelet aggregation,163 and the elevated hematocrit is associated with a concomitant increase in platelet adhesion.162,164 Aggregation of RBCs is significantly higher in men with proven vascular disease.165 In addition, RBC indices are associated with a number of CHD risk factors. For example, increased hemoglobin levels are associated with elevated serum cholesterol and triglyceride levels,166,167 and it is believed that the lipid-rich membranes of RBCs contribute to atheroma formation in the coronary arteries.168 In an elaborate set of studies in patients who died suddenly of cardiac causes, Kolodgie and colleagues169 found that an accumulation of erythrocytic membranes within an atherosclerotic plaque increases the risk of plaque destabilization by contributing to the deposition of free cholesterol. A prospective study using data from the Nurses' Health Study showed that a higher total trans-fatty acid content in the erythrocytes is associated with a significantly increased risk of CHD, with the highest quartile of trans-fatty acid content in erythrocytes having a relative risk of 2.7 (95% CI, 1.5–5; P < 0.01 for trend), compared with the lowest quartile.170 Accordingly, Tziakas and colleagues171 showed that the cholesterol content of erythrocytic membranes was significantly higher in patients with ACS than in patients with stable angina. It is thought that the altered membranes might decrease the fluidity of the RBCs. The different mechanisms by which RBCs might affect CHD are summarized in Table II.89,162–164,166–171
TABLE II. Possible Mechanisms of the Role of Red Blood Cells in Coronary Heart Disease
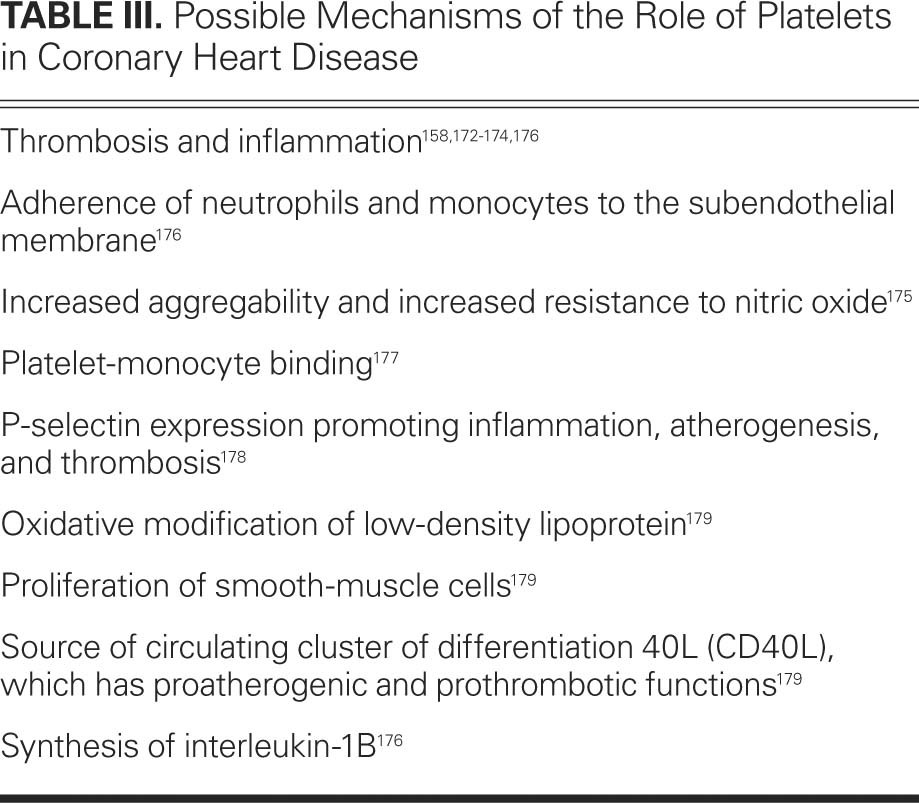
Inflammation and thrombosis are closely related.172 Platelets have clear roles in thrombosis and contribute to inflammation.158,173,174 Under stress, activated platelets help neutrophils adhere to the subendothelial matrix. Chirkov and colleagues175 have shown that there is increased platelet aggregability and resistance to nitric oxide in patients with stable angina pectoris and ACS, compared with patients without CHD (P < 0.01). Platelets also synthesize interleukin-1 beta (IL-1β), an important mediator of platelet-induced activation of the endothelial cells, which, in turn, induce chemokines that up-regulate the molecules that promote endothelial adhesion of neutrophils and monocytes.176 This increased total platelet-monocyte binding has been shown in ACS patients.177 In addition, patients with a larger territorial burden of atherosclerotic disease have shown greater P-selection expression, which promotes inflammation, atherogenesis, and thrombosis.178 Activated platelets also have been implicated in the oxidative modification of LDL-C that can contribute to proliferation of smooth-muscle cells. Platelets are the source of 90% of the circulating CD40L, which has proatherogenic and prothrombotic functions and is a predictor of incident MI, stroke, and cardiovascular death.179 The different mechanisms by which platelets might affect CHD are summarized in Table III.158,172–179
TABLE III. Possible Mechanisms of the Role of Platelets in Coronary Heart Disease
Conclusions
Elevated WBC counts, along with other components of the CBC, are associated with CHD morbidity and death. The tests are inexpensive and widely available and warrant further use for the purpose of coronary risk evaluation in the clinical and research settings. Comparative studies are needed of the WBC count and the CBC versus more novel inflammatory markers (such as CRP) for predicting cardiovascular disease risk. In addition to the absolute number of leukocytes and other blood cells, several indices of their activity, such as expression of different leukocytic proinflammatory genes, should also be tested in this context. Such analyses should take into account the intra-individual variability of WBC counts and subtypes, and also the known racial variances in WBC counts.
The WBC count should be further tested as a surrogate marker of outcomes for evaluating the effect of statins and similar pharmacologic interventions. Results of a 2008 study showed that statins can prevent vascular events in patients with high baseline CRP and moderate levels of LDL-C.180 Future studies and subgroup analyses are needed to determine whether patients with high WBC counts and moderate-to-low LDL-C levels (with either high or low CRP levels) are a new target population that could benefit from statin therapy. Elevated baseline WBC counts or no reduction in WBC counts (or related cell subtypes) during therapy might identify different response patterns and a need for more aggressive or combined therapy. Results from such trials could be used to develop clinical guidelines and to promote the use of these tests in the most appropriate manner.
Footnotes
Address for reprints: Mohammad Madjid, MD, MS, Texas Heart Institute, MC 2-255, 6770 Bertner Ave., Houston, TX 77030
E-mail: mmadjid@gmail.com
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee [published errata appear in Circulation 2011;124 (16):e424, Circulation 2010;122(1):e11, and Circulation 2009;119(3):e182]. Circulation 2009;119(3):e21–181. [DOI] [PubMed]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123(8):933–44. [DOI] [PubMed]
- 3.Libby P. Inflammation in atherosclerosis. Nature 2002;420 (6917):868–74. [DOI] [PubMed]
- 4.Madjid M, Casscells SW, Willerson JT. Biomarkers of inflammation as surrogate markers in detection of vulnerable plaques and vulnerable patients In: Willerson JT, Cohn JN, Wellens HJJ, Holmes DR Jr, editors. Cardiovascular medicine. 3rd ed. London: Springer-Verlag London Limited; 2007. p. 641–51.
- 5.Folsom AR, Chambless LE, Ballantyne CM, Coresh J, Heiss G, Wu KK, et al. An assessment of incremental coronary risk prediction using C-reactive protein and other novel risk markers: the atherosclerosis risk in communities study. Arch Intern Med 2006;166(13):1368–73. [DOI] [PubMed]
- 6.Madjid M, Awan I, Willerson JT, Casscells SW. Leukocyte count and coronary heart disease: implications for risk assessment. J Am Coll Cardiol 2004;44(10):1945–56. [DOI] [PubMed]
- 7.Koren-Morag N, Tanne D, Goldbourt U. White blood cell count and the incidence of ischemic stroke in coronary heart disease patients. Am J Med 2005;118(9):1004–9. [DOI] [PubMed]
- 8.Haim M, Boyko V, Goldbourt U, Battler A, Behar S. Predictive value of elevated white blood cell count in patients with preexisting coronary heart disease: the Bezafibrate Infarction Prevention Study. Arch Intern Med 2004;164(4):433–9. [DOI] [PubMed]
- 9.Andresdottir MB, Sigfusson N, Sigvaldason H, Gudnason V. Erythrocyte sedimentation rate, an independent predictor of coronary heart disease in men and women: The Reykjavik Study. Am J Epidemiol 2003;158(9):844–51. [DOI] [PubMed]
- 10.Gillum RF, Mussolino ME, Makuc DM. Erythrocyte sedimentation rate and coronary heart disease: the NHANES I Epidemiologic Follow-up Study. J Clin Epidemiol 1995;48 (3):353–61. [DOI] [PubMed]
- 11.Bholasingh R, Cornel JH, Kamp O, van Straalen JP, Sanders GT, Dijksman L, et al. The prognostic value of markers of inflammation in patients with troponin T-negative chest pain before discharge from the emergency department. Am J Med 2003;115(7):521–8. [DOI] [PubMed]
- 12.Keefer CS, Resnik WH. Angina pectoris. A syndrome caused by anoxemia of the myocardium. Arch Intern Med 1928;41 (6):769–807.
- 13.Rana JS, Boekholdt SM, Ridker PM, Jukema JW, Luben R, Bingham SA, et al. Differential leucocyte count and the risk of future coronary artery disease in healthy men and women: the EPIC-Norfolk Prospective Population Study. J Intern Med 2007;262(6):678–89. [DOI] [PubMed]
- 14.Zalokar JB, Richard JL, Claude JR. Leukocyte count, smoking, and myocardial infarction. N Engl J Med 1981;304(8): 465–8. [DOI] [PubMed]
- 15.Phillips AN, Neaton JD, Cook DG, Grimm RH, Shaper AG. Leukocyte count and risk of major coronary heart disease events. Am J Epidemiol 1992;136(1):59–70. [DOI] [PubMed]
- 16.Gillum RF, Mussolino ME, Madans JH. Counts of neutrophils, lymphocytes, and monocytes, cause-specific mortality and coronary heart disease: the NHANES-I epidemiologic follow-up study. Ann Epidemiol 2005;15(4):266–71. [DOI] [PubMed]
- 17.Weijenberg MP, Feskens EJ, Kromhout D. White blood cell count and the risk of coronary heart disease and all-cause mortality in elderly men. Arterioscler Thromb Vasc Biol 1996;16 (4):499–503. [DOI] [PubMed]
- 18.Folsom AR, Wu KK, Rosamond WD, Sharrett AR, Chambless LE. Prospective study of hemostatic factors and incidence of coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 1997;96(4):1102–8. [DOI] [PubMed]
- 19.Lee CD, Folsom AR, Nieto FJ, Chambless LE, Shahar E, Wolfe DA. White blood cell count and incidence of coronary heart disease and ischemic stroke and mortality from cardiovascular disease in African-American and White men and women: atherosclerosis risk in communities study. Am J Epidemiol 2001;154(8):758–64. [DOI] [PubMed]
- 20.Aronow HD, Quinn MJ, Gurm HS, Lauer MS, Brennan DM, Topol EJ, Lincoff AM. Preprocedure inflammatory state predicts periprocedural myocardial infarction after elective percutaneous coronary intervention: an EPIC substudy [abstract 1051–190]. J Am Coll Cardiol 2003;41(6 Suppl 1): 17A.
- 21.Manttari M, Manninen V, Koskinen P, Huttunen JK, Oksanen E, Tenkanen L, et al. Leukocytes as a coronary risk factor in a dyslipidemic male population. Am Heart J 1992;123(4 Pt 1):873–7. [DOI] [PubMed]
- 22.Grimm RH Jr, Neaton JD, Ludwig W. Prognostic importance of the white blood cell count for coronary, cancer, and all-cause mortality. JAMA 1985;254(14):1932–7. [PubMed]
- 23.Brown DW, Giles WH, Croft JB. White blood cell count: an independent predictor of coronary heart disease mortality among a national cohort. J Clin Epidemiol 2001;54(3):316–22. [DOI] [PubMed]
- 24.Takeda Y, Suzuki S, Fukutomi T, Kondo H, Sugiura M, Suzumura H, et al. Elevated white blood cell count as a risk factor of coronary artery disease: inconsistency between forms of the disease. Jpn Heart J 2003;44(2):201–11. [DOI] [PubMed]
- 25.Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS, Sarnak MJ. Inflammation and cardiovascular events in individuals with and without chronic kidney disease. Kidney Int 2008;73(12):1406–12. [DOI] [PMC free article] [PubMed]
- 26.Zouridakis EG, Garcia-Moll X, Kaski JC. Usefulness of the blood lymphocyte count in predicting recurrent instability and death in patients with unstable angina pectoris. Am J Cardiol 2000;86(4):449–51. [DOI] [PubMed]
- 27.Cannon CP, McCabe CH, Wilcox RG, Bentley JH, Braunwald E. Association of white blood cell count with increased mortality in acute myocardial infarction and unstable angina pectoris. OPUS-TIMI 16 Investigators. Am J Cardiol 2001; 87(5):636–9, A10. [DOI] [PubMed]
- 28.Sabatine MS, Morrow DA, Cannon CP, Murphy SA, Demopoulos LA, DiBattiste PM, et al. Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombolysis in Myocardial Infarction 18 trial) substudy. J Am Coll Cardiol 2002;40(10):1761–8. [DOI] [PubMed]
- 29.Mueller C, Neumann FJ, Perruchoud AP, Buettner HJ. White blood cell count and long term mortality after non-ST elevation acute coronary syndrome treated with very early revascularisation. Heart 2003;89(4):389–92. [DOI] [PMC free article] [PubMed]
- 30.Barron HV, Cannon CP, Murphy SA, Braunwald E, Gibson CM. Association between white blood cell count, epicardial blood flow, myocardial perfusion, and clinical outcomes in the setting of acute myocardial infarction: a thrombolysis in myocardial infarction 10 substudy. Circulation 2000;102(19): 2329–34. [DOI] [PubMed]
- 31.Cheng ML, Chen CM, Gu PW, Ho HY, Chiu DT. Elevated levels of myeloperoxidase, white blood cell count and 3-chlorotyrosine in Taiwanese patients with acute myocardial infarction. Clin Biochem 2008;41(7–8):554–60. [DOI] [PubMed]
- 32.Menon V, Lessard D, Yarzebski J, Furman MI, Gore JM, Goldberg RJ. Leukocytosis and adverse hospital outcomes after acute myocardial infarction. Am J Cardiol 2003;92(4): 368–72. [DOI] [PubMed]
- 33.Blum A. White blood cell count and the coronary anatomy in acute coronary events. Am J Cardiol 2005;95(1):159–60. [DOI] [PubMed]
- 34.Furman MI, Becker RC, Yarzebski J, Savegeau J, Gore JM, Goldberg RJ. Effect of elevated leukocyte count on in-hospital mortality following acute myocardial infarction. Am J Cardiol 1996;78(8):945–8. [DOI] [PubMed]
- 35.Barron HV, Harr SD, Radford MJ, Wang Y, Krumholz HM. The association between white blood cell count and acute myocardial infarction mortality in patients > or = 65 years of age: findings from the cooperative cardiovascular project. J Am Coll Cardiol 2001;38(6):1654–61. [DOI] [PubMed]
- 36.Hung MJ, Cherng WJ. Comparison of white blood cell counts in acute myocardial infarction patients with significant versus insignificant coronary artery disease. Am J Cardiol 2003;91(11):1339–42. [DOI] [PubMed]
- 37.Grzybowski M, Welch RD, Parsons L, Ndumele CE, Chen E, Zalenski R, Barron HV. The association between white blood cell count and acute myocardial infarction in-hospital mortality: findings from the National Registry of Myocardial Infarction. Acad Emerg Med 2004;11(10):1049–60. [DOI] [PubMed]
- 38.Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T, Hacke W. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke 2004;35(5):1147–52. [DOI] [PubMed]
- 39.Smit JJ, Ottervanger JP, Kolkman JJ, Slingerland RJ, Suryapranata H, Hoorntje JC, et al. Change of white blood cell count more prognostic important than baseline values after primary percutaneous coronary intervention for ST elevation myocardial infarction. Thromb Res 2008;122(2):185–9. [DOI] [PubMed]
- 40.Dragu R, Khoury S, Zuckerman R, Suleiman M, Mutlak D, Agmon Y, et al. Predictive value of white blood cell subtypes for long-term outcome following myocardial infarction. Atherosclerosis 2008;196(1):405–12. [DOI] [PubMed]
- 41.Dacey LJ, DeSimone J, Braxton JH, Leavitt BJ, Lahey SJ, Klemperer JD, et al. Preoperative white blood cell count and mortality and morbidity after coronary artery bypass grafting. Ann Thorac Surg 2003;76(3):760–4. [DOI] [PubMed]
- 42.Kochanek PM, Hallenbeck JM. Polymorphonuclear leukocytes and monocytes/macrophages in the pathogenesis of cerebral ischemia and stroke. Stroke 1992;23(9):1367–79. [DOI] [PubMed]
- 43.Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke 2003;34(10):2518–32. [DOI] [PubMed]
- 44.Beamer NB, Coull BM, Clark WM, Briley DP, Wynn M, Sexton G. Persistent inflammatory response in stroke survivors. Neurology 1998;50(6):1722–8. [DOI] [PubMed]
- 45.Tohgi H, Konno S, Takahashi S, Koizumi D, Kondo R, Takahashi H. Activated coagulation/fibrinolysis system and platelet function in acute thrombotic stroke patients with increased C-reactive protein levels. Thromb Res 2000;100(5):373–9. [DOI] [PubMed]
- 46.Patel MR, Mahaffey KW, Armstrong PW, Weaver WD, Tasissa G, Hochman JS, et al. Prognostic usefulness of white blood cell count and temperature in acute myocardial infarction (from the CARDINAL Trial). Am J Cardiol 2005;95(5): 614–8. [DOI] [PubMed]
- 47.Pellizzon GG, Dixon SR, Stone GW, Cox DA, Mattos L, Boura JA, et al. Relation of admission white blood cell count to long-term outcomes after primary coronary angioplasty for acute myocardial infarction (The Stent PAMI Trial). Am J Cardiol 2003;91(6):729–31. [DOI] [PubMed]
- 48.Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 1998;279(18):1477–82. [DOI] [PubMed]
- 49.Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med 2004;350(14):1387–97. [DOI] [PubMed]
- 50.Prentice RL, Szatrowski TP, Fujikura T, Kato H, Mason MW, Hamilton HH. Leukocyte counts and coronary heart disease in a Japanese cohort. Am J Epidemiol 1982;116(3):496–509. [DOI] [PubMed]
- 51.Umemoto S, Suzuki N, Fujii K, Fujii A, Fujii T, Iwami T, et al. Eosinophil counts and plasma fibrinogen in patients with vasospastic angina pectoris. Am J Cardiol 2000;85(6):715–9. [DOI] [PubMed]
- 52.Olivares R, Ducimetiere P, Claude JR. Monocyte count: a risk factor for coronary heart disease? Am J Epidemiol 1993;137 (1):49–53. [DOI] [PubMed]
- 53.Yun KH, Oh SK, Park EM, Kim HJ, Shin SH, Lee EM, et al. An increased monocyte count predicts coronary artery spasm in patients with resting chest pain and insignificant coronary artery stenosis. Korean J Intern Med 2006;21(2):97–102. [DOI] [PMC free article] [PubMed]
- 54.Afiune Neto A, Mansur Ade P, Avakian SD, Gomes EP, Ramires JA. Monocytosis is an independent risk marker for coronary artery disease [in Portuguese]. Arq Bras Cardiol 2006;86(3):240–4. [DOI] [PubMed]
- 55.Sweetnam PM, Thomas HF, Yarnell JW, Baker IA, Elwood PC. Total and differential leukocyte counts as predictors of ischemic heart disease: the Caerphilly and Speedwell studies. Am J Epidemiol 1997;145(5):416–21. [DOI] [PubMed]
- 56.Avanzas P, Arroyo-Espliguero R, Cosin-Sales J, Aldama G, Pizzi C, Quiles J, Kaski JC. Markers of inflammation and multiple complex stenoses (pancoronary plaque vulnerability) in patients with non-ST segment elevation acute coronary syndromes. Heart 2004;90(8):847–52. [DOI] [PMC free article] [PubMed]
- 57.Wheeler JG, Mussolino ME, Gillum RF, Danesh J. Associations between differential leucocyte count and incident coronary heart disease: 1764 incident cases from seven prospective studies of 30,374 individuals. Eur Heart J 2004;25(15):1287–92. [DOI] [PubMed]
- 58.Avanzas P, Quiles J, Lopez de Sa E, Sanchez A, Rubio R, Garcia E, Lopez-Sendon JL. Neutrophil count and infarct size in patients with acute myocardial infarction. Int J Cardiol 2004; 97(1):155–6. [DOI] [PubMed]
- 59.Kawaguchi H, Mori T, Kawano T, Kono S, Sasaki J, Arakawa K. Band neutrophil count and the presence and severity of coronary atherosclerosis. Am Heart J 1996;132(1 Pt 1):9–12. [DOI] [PubMed]
- 60.Biasucci LM, D'Onofrio G, Liuzzo G, Zini G, Monaco C, Caligiuri G, et al. Intracellular neutrophil myeloperoxidase is reduced in unstable angina and acute myocardial infarction, but its reduction is not related to ischemia. J Am Coll Cardiol 1996;27(3):611–6. [DOI] [PubMed]
- 61.Ommen SR, Gibbons RJ, Hodge DO, Thomson SP. Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease. Am J Cardiol 1997;79(6):812–4. [DOI] [PubMed]
- 62.Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol 2005;45(10): 1638–43. [DOI] [PubMed]
- 63.Sakatani T, Hadase M, Kawasaki T, Kamitani T, Kawasaki S, Sugihara H. Usefulness of the percentage of plasma lymphocytes as a prognostic marker in patients with congestive heart failure. Jpn Heart J 2004;45(2):275–84. [DOI] [PubMed]
- 64.Nasir K, Guallar E, Navas-Acien A, Criqui MH, Lima JA. Relationship of monocyte count and peripheral arterial disease: results from the National Health and Nutrition Examination Survey 1999–2002. Arterioscler Thromb Vasc Biol 2005;25(9):1966–71. [DOI] [PubMed]
- 65.Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F. Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta 2008;395(1–2):27–31. [DOI] [PubMed]
- 66.Haumer M, Amighi J, Exner M, Mlekusch W, Sabeti S, Schlager O, et al. Association of neutrophils and future cardiovascular events in patients with peripheral artery disease. J Vasc Surg 2005;41(4):610–7. [DOI] [PubMed]
- 67.Nozawa N, Hibi K, Endo M, Sugano T, Ebina T, Kosuge M, et al. Association between circulating monocytes and coronary plaque progression in patients with acute myocardial infarction. Circ J 2010;74(7):1384–91. [DOI] [PubMed]
- 68.Hung MJ, Kuo LT, Cheng CW, Chang CP, Cherng WJ. Comparison of peripheral monocyte counts in patients with and without coronary spasm and without fixed coronary narrowing. Am J Cardiol 2004;93(5):620–4. [DOI] [PubMed]
- 69.Waterhouse DF, Cahill RA, Sheehan F, McCreery C. Prediction of calculated future cardiovascular disease by monocyte count in an asymptomatic population. Vasc Health Risk Manag 2008;4(1):177–87. [DOI] [PMC free article] [PubMed]
- 70.Loimaala A, Rontu R, Vuori I, Mercuri M, Lehtimaki T, Nenonen A, Bond MG. Blood leukocyte count is a risk factor for intima-media thickening and subclinical carotid atherosclerosis in middle-aged men. Atherosclerosis 2006;188(2):363–9. [DOI] [PubMed]
- 71.Huang ZS, Jeng JS, Wang CH, Yip PK, Wu TH, Lee TK. Correlations between peripheral differential leukocyte counts and carotid atherosclerosis in non-smokers. Atherosclerosis 2001;158(2):431–6. [DOI] [PubMed]
- 72.Chapman CM, Beilby JP, McQuillan BM, Thompson PL, Hung J. Monocyte count, but not C-reactive protein or interleukin-6, is an independent risk marker for subclinical carotid atherosclerosis. Stroke 2004;35(7):1619–24. [DOI] [PubMed]
- 73.Gudbjartsson DF, Bjornsdottir US, Halapi E, Helgadottir A, Sulem P, Jonsdottir GM, et al. Sequence variants affecting eosinophil numbers associate with asthma and myocardial infarction. Nat Genet 2009;41(3):342–7. [DOI] [PubMed]
- 74.Packard CJ, O'Reilly DS, Caslake MJ, McMahon AD, Ford I, Cooney J, et al. Lipoprotein-associated phospholipase A2 as an independent predictor of coronary heart disease. West of Scotland Coronary Prevention Study Group. N Engl J Med 2000;343(16):1148–55. [DOI] [PubMed]
- 75.Wildman RP, Muntner P, Chen J, Sutton-Tyrrell K, He J. Relation of inflammation to peripheral arterial disease in the national health and nutrition examination survey, 1999–2002. Am J Cardiol 2005;96(11):1579–83. [DOI] [PubMed]
- 76.Margolis KL, Manson JE, Greenland P, Rodabough RJ, Bray PF, Safford M, et al. Leukocyte count as a predictor of cardiovascular events and mortality in postmenopausal women: the Women's Health Initiative Observational Study. Arch Intern Med 2005;165(5):500–8. [DOI] [PubMed]
- 77.Ajani UA, Ford ES, McGuire LC. Distribution of lifestyle and emerging risk factors by 10-year risk for coronary heart disease. Eur J Cardiovasc Prev Rehabil 2006;13(5):745–52. [DOI] [PubMed]
- 78.Palmerini T, Marzocchi A, Marrozzini C, Ortolani P, Saia F, Bacchi-Reggiani L, et al. Preprocedural levels of C-reactive protein and leukocyte counts predict 9-month mortality after coronary angioplasty for the treatment of unprotected left main coronary artery stenosis. Circulation 2005;112(15): 2332–8. [DOI] [PubMed]
- 79.Rasouli M, Kiasari AM, Bagheri B. Total and differential leukocytes counts, but not hsCRP, ESR, and five fractioned serum proteins have significant potency to predict stable coronary artery disease. Clin Chim Acta 2007;377(1–2):127–32. [DOI] [PubMed]
- 80.Smit JJ, Ottervanger JP, Slingerland RJ, Kolkman JJ, Suryapranata H, Hoorntje JC, et al. Comparison of usefulness of C-reactive protein versus white blood cell count to predict outcome after primary percutaneous coronary intervention for ST elevation myocardial infarction. Am J Cardiol 2008;101(4):446–51. [DOI] [PubMed]
- 81.Cavusoglu E, Chopra V, Gupta A, Ruwende C, Yanamadala S, Eng C, et al. Usefulness of the white blood cell count as a predictor of angiographic findings in an unselected population referred for coronary angiography. Am J Cardiol 2006;98 (9):1189–93. [DOI] [PubMed]
- 82.Kruk M, Przyluski J, Kalinczuk L, Pregowski J, Deptuch T, Kadziela J, et al. Association of non-specific inflammatory activation with early mortality in patients with ST-elevation acute coronary syndrome treated with primary angioplasty. Circ J 2008;72(2):205–11. [DOI] [PubMed]
- 83.Roy D, Quiles J, Avanzas P, Arroyo-Espliguero R, Sinha M, Kaski JC. A comparative study of markers of inflammation for the assessment of cardiovascular risk in patients presenting to the emergency department with acute chest pain suggestive of acute coronary syndrome. Int J Cardiol 2006;109(3):317–21. [DOI] [PubMed]
- 84.Yip HK, Wu CJ, Hang CL, Chang HW, Yang CH, Hsieh YK, et al. Levels and values of inflammatory markers in patients with angina pectoris. Int Heart J 2005;46(4):571–81. [DOI] [PubMed]
- 85.Willerson JT, Ridker PM. Inflammation as a cardiovascular risk factor. Circulation 2004;109(21 Suppl 1):II2–10. [DOI] [PubMed]
- 86.Bickel C, Rupprecht HJ, Blankenberg S, Espiniola-Klein C, Schlitt A, Rippin G, et al. Relation of markers of inflammation (C-reactive protein, fibrinogen, von Willebrand factor, and leukocyte count) and statin therapy to long-term mortality in patients with angiographically proven coronary artery disease. Am J Cardiol 2002;89(8):901–8. [DOI] [PubMed]
- 87.Bickel C, Rupprecht HJ, Blankenberg S, Espinola-Klein C, Rippin G, Hafner G, et al. Influence of HMG-CoA reductase inhibitors on markers of coagulation, systemic inflammation and soluble cell adhesion. Int J Cardiol 2002;82(1):25–31. [DOI] [PubMed]
- 88.Schillinger M, Exner M, Mlekusch W, Amighi J, Sabeti S, Muellner M, et al. Statin therapy improves cardiovascular outcome of patients with peripheral artery disease. Eur Heart J 2004;25(9):742–8. [DOI] [PubMed]
- 89.Tani S, Nagao K, Anazawa T, Kawamata H, Iida K, Matsumoto M, et al. Association of circulating leukocyte count with coronary atherosclerosis regression after pravastatin treatment. Atherosclerosis 2008;198(2):360–5. [DOI] [PubMed]
- 90.Stewart RA, White HD, Kirby AC, Heritier SR, Simes RJ, Nestel PJ, et al. White blood cell count predicts reduction in coronary heart disease mortality with pravastatin. Circulation 2005;111(14):1756–62. [DOI] [PubMed]
- 91.Ronnow BS, Muhlestein JB, Carlquist JF, Renlund DG, Lappe DL, Thomas H, et al. A complete blood count-derived risk score greatly improves predictive ability for mortality [abstract 854–7]. J Am Coll Cardiol 2005;45(3 Suppl A):435A.
- 92.Gibson PH, Croal BL, Cuthbertson BH, Small GR, Ifezulike AI, Gibson G, et al. Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting. Am Heart J 2007;154(5):995–1002. [DOI] [PubMed]
- 93.Spencer CG, Felmeden DC, Blann AD, Lip GY. Haemorheological, platelet and endothelial indices in relation to global measures of cardiovascular risk in hypertensive patients: a substudy of the Anglo-Scandinavian Cardiac Outcomes Trial. J Intern Med 2007;261(1):82–90. [DOI] [PubMed]
- 94.Anderson JL, Ronnow BS, Horne BD, Carlquist JF, May HT, Bair TL, et al. Usefulness of a complete blood count-derived risk score to predict incident mortality in patients with suspected cardiovascular disease. Am J Cardiol 2007;99(2):169–74. [DOI] [PubMed]
- 95.Danesh J, Collins R, Peto R, Lowe GD. Haematocrit, viscosity, erythrocyte sedimentation rate: meta-analyses of prospective studies of coronary heart disease. Eur Heart J 2000;21(7): 515–20. [DOI] [PubMed]
- 96.Michiels JJ. Erythromelalgia and vascular complications in polycythemia vera. Semin Thromb Hemost 1997;23(5):441–54. [DOI] [PubMed]
- 97.Puddu PE, Lanti M, Menotti A, Mancini M, Zanchetti A, Cirillo M, et al. Red blood cell count in short-term prediction of cardiovascular disease incidence in the Gubbio population study. Acta Cardiol 2002;57(3):177–85. [DOI] [PubMed]
- 98.Schlant RC, Forman S, Stamler J, Canner PL. The natural history of coronary heart disease: prognostic factors after recovery from myocardial infarction in 2789 men. The 5-year findings of the coronary drug project. Circulation 1982;66 (2):401–14. [DOI] [PubMed]
- 99.Lowe GD, Machado SG, Krol WF, Barton BA, Forbes CD. White blood cell count and haematocrit as predictors of coronary recurrence after myocardial infarction. Thromb Haemost 1985;54(3):700–3. [PubMed]
- 100.Smith FB, Rumley A, Lee AJ, Leng GC, Fowkes FG, Lowe GD. Haemostatic factors and prediction of ischaemic heart disease and stroke in claudicants. Br J Haematol 1998;100(4): 758–63. [DOI] [PubMed]
- 101.Cullen KJ, Stenhouse NS, Wearne KL. Raised haemoglobin and risk of cardiovascular disease. Lancet 1981;2(8258):1288–9. [DOI] [PubMed]
- 102.Sorlie PD, Garcia-Palmieri MR, Costas R Jr, Havlik RJ. Hematocrit and risk of coronary heart disease: the Puerto Rico Health Program. Am Heart J 1981;101(4):456–61. [DOI] [PubMed]
- 103.Carter C, McGee D, Reed D, Yano K, Stemmermann G. Hematocrit and the risk of coronary heart disease: the Honolulu Heart Program. Am Heart J 1983;105(4):674–9. [DOI] [PubMed]
- 104.Schatzkin A, Cupples LA, Heeren T, Morelock S, Kannel WB. Sudden death in the Framingham Heart Study. Differences in incidence and risk factors by sex and coronary disease status. Am J Epidemiol 1984;120(6):888–99. [DOI] [PubMed]
- 105.Kannel WB, Anderson K, Wilson PW. White blood cell count and cardiovascular disease. Insights from the Framingham Study. JAMA 1992;267(9):1253–6. [PubMed]
- 106.Erikssen G, Thaulow E, Sandvik L, Stormorken H, Erikssen J. Haematocrit: a predictor of cardiovascular mortality? J Intern Med 1993;234(5):493–9. [DOI] [PubMed]
- 107.Gagnon DR, Zhang TJ, Brand FN, Kannel WB. Hematocrit and the risk of cardiovascular disease–the Framingham study: a 34-year follow-up. Am Heart J 1994;127(3):674–82. [DOI] [PubMed]
- 108.Wannamethee G, Shaper AG, Whincup PH. Ischaemic heart disease: association with haematocrit in the British Regional Heart Study. J Epidemiol Community Health 1994;48(2): 112–8. [DOI] [PMC free article] [PubMed]
- 109.Brown DW, Giles WH, Croft JB. Hematocrit and the risk of coronary heart disease mortality. Am Heart J 2001;142(4): 657–63. [DOI] [PubMed]
- 110.Abu-Zeid HA, Chapman JM. Hemoglobin level and ischemic heart disease: relationship to known risk factors. Prev Med 1977;6(1):120–9. [DOI] [PubMed]
- 111.Lowe GD, Lee AJ, Rumley A, Price JF, Fowkes FG. Blood viscosity and risk of cardiovascular events: the Edinburgh Artery Study. Br J Haematol 1997;96(1):168–73. [DOI] [PubMed]
- 112.Kenyeres P, Juricskay I, Tarsoly P, Kesmarky G, Muhl D, Toth K, Bogar L. Low hematocrit per blood viscosity ratio as a mortality risk factor in coronary heart disease. Clin Hemorheol Microcirc 2008;38(1):51–6. [PubMed]
- 113.Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004;292(13):1555–62. [DOI] [PubMed]
- 114.Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med 2001;345(17):1230–6. [DOI] [PubMed]
- 115.Hebert PC, Yetisir E, Martin C, Blajchman MA, Wells G, Marshall J, et al. Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases? Crit Care Med 2001;29(2):227–34. [DOI] [PubMed]
- 116.Fortune JB, Feustel PJ, Saifi J, Stratton HH, Newell JC, Shah DM. Influence of hematocrit on cardiopulmonary function after acute hemorrhage. J Trauma 1987;27(3):243–9. [DOI] [PubMed]
- 117.Johnson RG, Thurer RL, Kruskall MS, Sirois C, Gervino EV, Critchlow J, Weintraub RM. Comparison of two transfusion strategies after elective operations for myocardial revascularization. J Thorac Cardiovasc Surg 1992;104(2):307–14. [PubMed]
- 118.Bush RL, Pevec WC, Holcroft JW. A prospective, randomized trial limiting perioperative red blood cell transfusions in vascular patients. Am J Surg 1997;174(2):143–8. [DOI] [PubMed]
- 119.Rogers MA, Blumberg N, Saint SK, Kim C, Nallamothu BK, Langa KM. Allogeneic blood transfusions explain increased mortality in women after coronary artery bypass graft surgery. Am Heart J 2006;152(6):1028–34. [DOI] [PubMed]
- 120.Alexander KP, Chen AY, Wang TY, Rao SV, Newby LK, LaPointe NM, et al. Transfusion practice and outcomes in non-ST-segment elevation acute coronary syndromes. Am Heart J 2008;155(6):1047–53. [DOI] [PubMed]
- 121.Perlstein TS, Weuve J, Pfeffer MA, Beckman JA. Red blood cell distribution width and mortality risk in a community-based prospective cohort. Arch Intern Med 2009;169(6):588–94. [DOI] [PMC free article] [PubMed]
- 122.Patel KV, Ferrucci L, Ershler WB, Longo DL, Guralnik JM. Red blood cell distribution width and the risk of death in middle-aged and older adults. Arch Intern Med 2009;169(5):515–23. [DOI] [PMC free article] [PubMed]
- 123.Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation 2008;117(2):163–8. [DOI] [PubMed]
- 124.Ani C, Ovbiagele B. Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci 2009;277(1–2):103–8. [DOI] [PubMed]
- 125.Cavusoglu E, Chopra V, Gupta A, Battala VR, Poludasu S, Eng C, Marmur JD. Relation between red blood cell distribution width (RDW) and all-cause mortality at two years in an unselected population referred for coronary angiography. Int J Cardiol 2010;141(2):141–6. [DOI] [PubMed]
- 126.Nayha S. Normal variation in erythrocyte sedimentation rate in males over 50 years old. Scand J Prim Health Care 1987;5 (1):5–8. [DOI] [PubMed]
- 127.Hanger HC, Sainsbury R, Gilchrist NL, Beard ME. Erythrocyte sedimentation rates in the elderly: a community study. N Z Med J 1991;104(909):134–6. [PubMed]
- 128.Erikssen G, Liestol K, Bjornholt JV, Stormorken H, Thaulow E, Erikssen J. Erythrocyte sedimentation rate: a possible marker of atherosclerosis and a strong predictor of coronary heart disease mortality. Eur Heart J 2000;21(19):1614–20. [DOI] [PubMed]
- 129.Natali A, L'Abbate A, Ferrannini E. Erythrocyte sedimentation rate, coronary atherosclerosis, and cardiac mortality. Eur Heart J 2003;24(7):639–48. [DOI] [PubMed]
- 130.Froom P, Margaliot S, Caine Y, Benbassat J. Significance of erythrocyte sedimentation rate in young adults. Am J Clin Pathol 1984;82(2):198–200. [DOI] [PubMed]
- 131.Kirkeby OJ, Risoe C, Vikland R. Significance of a high erythrocyte sedimentation rate in general practice. Br J Clin Pract 1989;43(7):252–4. [PubMed]
- 132.Carlson LA, Bottiger LE. Risk factors for ischaemic heart disease in men and women. Results of the 19-year follow-up of the Stockholm Prospective Study. Acta Med Scand 1985;218 (2):207–11. [DOI] [PubMed]
- 133.Thaulow E, Erikssen J, Sandvik L, Stormorken H, Cohn PF. Blood platelet count and function are related to total and cardiovascular death in apparently healthy men. Circulation 1991;84(2):613–7. [DOI] [PubMed]
- 134.D'Erasmo E, Aliberti G, Celi FS, Romagnoli E, Vecci E, Mazzuoli GF. Platelet count, mean platelet volume and their relation to prognosis in cerebral infarction. J Intern Med 1990; 227(1):11–4. [DOI] [PubMed]
- 135.Kilicli-Camur N, Demirtunc R, Konuralp C, Eskiser A, Basaran Y. Could mean platelet volume be a predictive marker for acute myocardial infarction? Med Sci Monit 2005;11(8): CR387–92. [PubMed]
- 136.Meade TW, Cooper JA, Miller GJ. Platelet counts and aggregation measures in the incidence of ischaemic heart disease (IHD). Thromb Haemost 1997;78(2):926–9. [PubMed]
- 137.Khandekar MM, Khurana AS, Deshmukh SD, Kakrani AL, Katdare AD, Inamdar AK. Platelet volume indices in patients with coronary artery disease and acute myocardial infarction: an Indian scenario. J Clin Pathol 2006;59(2):146–9. [DOI] [PMC free article] [PubMed]
- 138.Raffel OC, Tearney GJ, Gauthier DD, Halpern EF, Bouma BE, Jang IK. Relationship between a systemic inflammatory marker, plaque inflammation, and plaque characteristics determined by intravascular optical coherence tomography. Arterioscler Thromb Vasc Biol 2007;27(8):1820–7. [DOI] [PMC free article] [PubMed]
- 139.Weissmann G, Smolen JE, Korchak HM. Release of inflammatory mediators from stimulated neutrophils. N Engl J Med 1980;303(1):27–34. [DOI] [PubMed]
- 140.Sacks T, Moldow CF, Craddock PR, Bowers TK, Jacob HS. Oxygen radicals mediate endothelial cell damage by complement-stimulated granulocytes. An in vitro model of immune vascular damage. J Clin Invest 1978;61(5):1161–7. [DOI] [PMC free article] [PubMed]
- 141.Harlan JM, Killen PD, Harker LA, Striker GE, Wright DG. Neutrophil-mediated endothelial injury in vitro mechanisms of cell detachment. J Clin Invest 1981;68(6):1394–403. [DOI] [PMC free article] [PubMed]
- 142.Mehta J, Dinerman J, Mehta P, Saldeen TG, Lawson D, Donnelly WH, Wallin R. Neutrophil function in ischemic heart disease. Circulation 1989;79(3):549–56. [DOI] [PubMed]
- 143.Ludwig PW, Hunninghake DB, Hoidal JR. Increased leucocyte oxidative metabolism in hyperlipoproteinaemia. Lancet 1982;2(8294):348–50. [DOI] [PubMed]
- 144.Ricevuti G, Mazzone A, De Servi S, Specchia G, Fratino P. New trends in coronary artery disease: the role of granulocyte activation. Atherosclerosis 1989;78(2–3):261–5. [DOI] [PubMed]
- 145.Stenqvist O, Bagge U, Nilsson K. The tracheal mucosa microvasculature and microcirculation. Intravital microscopic observations in rabbits and a histologic study in man. Acta Otolaryngol 1979;87(1–2):123–8. [DOI] [PubMed]
- 146.Craddock PR, Hammerschmidt D, White JG, Dalmosso AP, Jacob HS. Complement (C5-a)-induced granulocyte aggregation in vitro. A possible mechanism of complement-mediated leukostasis and leukopenia. J Clin Invest 1977;60(1):260–4. [DOI] [PMC free article] [PubMed]
- 147.Shoenfeld Y, Pinkhas J. Leukopenia and low incidence of myocardial infarction. N Engl J Med 1981;304(26):1606. [DOI] [PubMed]
- 148.Neumann FJ, Ott I, Marx N, Luther T, Kenngott S, Gawaz M, et al. Effect of human recombinant interleukin-6 and interleukin-8 on monocyte procoagulant activity. Arterioscler Thromb Vasc Biol 1997;17(12):3399–405. [DOI] [PubMed]
- 149.Ogawa Y, Imaki M, Yoshida Y, Shibakawa M, Tanada S. An epidemiological study on the association between the total leukocyte and neutrophil counts, and risk factors of ischemic heart disease by smoking status in Japanese factory workers. Appl Human Sci 1998;17(6):239–47. [DOI] [PubMed]
- 150.Nieto FJ, Szklo M, Folsom AR, Rock R, Mercuri M. Leukocyte count correlates in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol 1992;136(5):525–37. [DOI] [PubMed]
- 151.Capuano V, Lamaida N, De Martino M, Mazzotta G. Association between white blood cell count and risk factors of coronary artery disease. G Ital Cardiol 1995;25(9):1145–52. [PubMed]
- 152.Bovill EG, Bild DE, Heiss G, Kuller LH, Lee MH, Rock R, Wahl PW. White blood cell counts in persons aged 65 years or more from the Cardiovascular Health Study. Correlations with baseline clinical and demographic characteristics. Am J Epidemiol 1996;143(11):1107–15. [DOI] [PubMed]
- 153.Nakanishi N, Sato M, Shirai K, Nakajima K, Murakami S, Takatorige T, et al. Associations between white blood cell count and features of the metabolic syndrome in Japanese male office workers. Ind Health 2002;40(3):273–7. [DOI] [PubMed]
- 154.Nilsson G, Hedberg P, Jonason T, Lonnberg I, Tenerz A, Ohrvik J. White blood cell counts associate more strongly to the metabolic syndrome in 75-year-old women than in men: a population based study. Metab Syndr Relat Disord 2007;5(4):359–64. [DOI] [PubMed]
- 155.Tong PC, Lee KF, So WY, Ng MH, Chan WB, Lo MK, et al. White blood cell count is associated with macro- and microvascular complications in Chinese patients with type 2 diabetes. Diabetes Care 2004;27(1):216–22. [DOI] [PubMed]
- 156.Diacovo TG, Roth SJ, Buccola JM, Bainton DF, Springer TA. Neutrophil rolling, arrest, and transmigration across activated, surface-adherent platelets via sequential action of P-selectin and the beta 2-integrin CD11b/CD18. Blood 1996;88(1): 146–57. [PubMed]
- 157.Maisel AS, Gilpin EA, LeWinter M, Henning H, Ross J Jr, Engler R. Initial leukocyte count during acute myocardial infarction independently predicts early ventricular fibrillation [abstract]. Circulation 1985;72(Suppl 3):III-414.
- 158.de Gaetano G, Cerletti C, Evangelista V. Recent advances in platelet-polymorphonuclear leukocyte interaction. Haemostasis 1999;29(1):41–9. [DOI] [PubMed]
- 159.Reizenstein P. The haematological stress syndrome. Br J Haematol 1979;43(3):329–34. [DOI] [PubMed]
- 160.Masuda M, Takahashi H. Adhesion of leukocytes to endothelial cells in atherosclerosis [in Japanese]. Rinsho Byori 1998; 46(11):1149–55. [PubMed]
- 161.Turner SJ, Ketch TR, Gandhi SK, Sane DC. Routine hematologic clinical tests as prognostic markers in patients with acute coronary syndromes. Am Heart J 2008;155(5):806–16. [DOI] [PubMed]
- 162.Turitto VT, Weiss HJ. Red blood cells: their dual role in thrombus formation. Science 1980;207(4430):541–3. [DOI] [PubMed]
- 163.Lowe GD, Forbes CD. Platelet aggregation, haematocrit, and fibrinogen. Lancet 1985;1(8425):395–6. [DOI] [PubMed]
- 164.Hellem AJ, Borchgrevink CF, Ames SB. The role of red cells in haemostasis: the relation between haematocrit, bleeding time and platelet adhesiveness. Br J Haematol 1961;7:42–50. [DOI] [PubMed]
- 165.Berliner S, Rogowski O, Aharonov S, Mardi T, Tolshinsky T, Rozenblat M, et al. Erythrocyte adhesiveness/aggregation: a novel biomarker for the detection of low-grade internal inflammation in individuals with atherothrombotic risk factors and proven vascular disease. Am Heart J 2005;149(2):260–7. [DOI] [PubMed]
- 166.Elwood PC, Sweetnam P, Welsby E, Mahler R, Moore F. Association between circulating haemoglobin level, serum-cholesterol, and blood-pressure. Lancet 1970;1(7647):589–90. [DOI] [PubMed]
- 167.Bottiger LE, Carlson LA. Relation between serum cholesterol and triglyceride concentration and haemoglobin values in non-anaemic healthy persons. Br Med J 1972;3(5829):731–3. [DOI] [PMC free article] [PubMed]
- 168.Pasterkamp G, Virmani R. The erythrocyte: a new player in atheromatous core formation. Heart 2002;88(2):115–6. [DOI] [PMC free article] [PubMed]
- 169.Kolodgie FD, Gold HK, Burke AP, Fowler DR, Kruth HS, Weber DK, et al. Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med 2003;349(24):2316–25. [DOI] [PubMed]
- 170.Sun Q, Ma J, Campos H, Hankinson SE, Manson JE, Stampfer MJ, et al. A prospective study of trans fatty acids in erythrocytes and risk of coronary heart disease. Circulation 2007; 115(14):1858–65. [DOI] [PubMed]
- 171.Tziakas DN, Kaski JC, Chalikias GK, Romero C, Fredericks S, Tentes IK, et al. Total cholesterol content of erythrocyte membranes is increased in patients with acute coronary syndrome: a new marker of clinical instability? J Am Coll Cardiol 2007;49(21):2081–9. [DOI] [PubMed]
- 172.Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation 2001;103(13):1718–20. [DOI] [PubMed]
- 173.de Gaetano G, Evangelista V, Cerletti C. Should cardiologists forget about platelets and take an interest in blood leukocytes? Ital Heart J 2000;1(7):453–6. [PubMed]
- 174.Tousoulis D, Davies G, Stefanadis C, Toutouzas P, Ambrose JA. Inflammatory and thrombotic mechanisms in coronary atherosclerosis. Heart 2003;89(9):993–7. [DOI] [PMC free article] [PubMed]
- 175.Chirkov YY, Holmes AS, Willoughby SR, Stewart S, Wuttke RD, Sage PR, Horowitz JD. Stable angina and acute coronary syndromes are associated with nitric oxide resistance in platelets. J Am Coll Cardiol 2001;37(7):1851–7. [DOI] [PubMed]
- 176.Davi G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med 2007;357(24):2482–94. [DOI] [PubMed]
- 177.Sarma J, Laan CA, Alam S, Jha A, Fox KA, Dransfield I. Increased platelet binding to circulating monocytes in acute coronary syndromes. Circulation 2002;105(18):2166–71. [DOI] [PubMed]
- 178.Keating FK, Whitaker DA, Kabbani SS, Ricci MA, Sobel BE, Schneider DJ. Relation of augmented platelet reactivity to the magnitude of distribution of atherosclerosis. Am J Cardiol 2004;94(6):725–8. [DOI] [PubMed]
- 179.Schonbeck U, Varo N, Libby P, Buring J, Ridker PM. Soluble CD40L and cardiovascular risk in women. Circulation 2001;104(19):2266–8. [DOI] [PubMed]
- 180.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359(21):2195–207. [DOI] [PubMed]


