Abstract
Background
Although there is evidence that hospitals recognized for nursing excellence— Magnet hospitals—are successful in attracting and retaining nurses, it is uncertain whether Magnet recognition is associated with better patient outcomes than non-Magnets, and if so why.
Objectives
To determine whether Magnet hospitals have lower risk-adjusted mortality and failure-to-rescue compared to non-Magnet hospitals, and to determine the most likely explanations.
Method and Study Design
Analysis of linked patient, nurse, and hospital data on 56 Magnet and 508 non-Magnet hospitals. Logistic regression models were used to estimate differences in the odds of mortality and failure-to-rescue for surgical patients treated in Magnet vs. non-Magnet hospitals, and to determine the extent to which differences in outcomes can be explained by nursing after accounting for patient and hospital differences.
Results
Magnet hospitals had significantly better work environments and higher proportions of nurses with bachelor’s degrees and specialty certification. These nursing factors explained much of the Magnet hospital effect on patient outcomes. However, patients treated in Magnet hospitals had 14% lower odds of mortality (OR 0.86, 95% CI 0.76-0.98, p=0.02) and 12% lower odds of failure-to-rescue (OR 0.88, 95% CI 0.77-1.01, p=0.07) while controlling for nursing factors as well as hospital and patient differences.
Conclusions
Magnet hospitals have lower mortality than is fully accounted for by measured characteristics of nursing. Magnet recognition likely both identifies existing quality and stimulates further positive organizational behavior that improves patient outcomes.
Keywords: nursing, Magnet hospitals, quality of health care, organizational culture
Nurses are key players in the effective functioning of complex hospital organizations and their ability to provide good patient care is influenced by the context in which they practice. Hallmarks of successful organizations include flat organizational structure with accessible and informed managers, decentralized decision-making, and the empowerment of front line workers to make decisions.1-2 Managerial strategies that reduce the negative effects of organizational complexity on employee productivity, work quality, and retention have emerged in a variety of industries and settings. The concept of Magnet hospitals—hospitals identified by their reputations for being good places for nurses to work—evolved from observations that hospitals that were successful in attracting and retaining qualified nurses resembled the most highly ranked U.S. corporations.3
In 1994, Medical Care published the first paper on patient outcomes in Magnet hospitals, documenting lower risk-adjusted mortality among Medicare patients in the original Magnet hospitals.4 Magnet hospital designation was formalized with the American Nurses Credentialing Center’s (ANCC) Magnet Recognition Program® in the 1990s.5 The voluntary process was subsequently shown to identify hospitals that were as good as the original “reputational” Magnet hospitals of the 1980s in terms of having excellent work environments and nurse outcomes such as lower levels of burnout and higher job satisfaction.6 With few exceptions,7 studies since have shown that care environments in Magnet recognized hospitals are different from non-Magnet hospitals.8-10 These differences are associated with higher levels of nurse satisfaction, less nurse burnout,11-12 lower patient fall rates,13 and lower mortality among very low birth weight infants.14
The number of Magnet recognized hospitals has grown to nearly 400— about 8% of hospitals nationally. The Magnet Recognition Program® has also achieved status and visibility; Magnet recognition is now an indicator for national hospital ranking and quality benchmarking programs like U.S. News and World Report Best Hospitals rankings and the Leapfrog Group hospital ratings.15-17 During the period of evolution and replication of Magnet hospitals, research emerged documenting associations between hospitals with exemplary nurse practice environments and patient outcomes. Lower risk-adjusted mortality and death following complication among surgical patients have been associated with lower patient-to-nurse ratios,18-20 a more educated nurse workforce,21 more specialty-certified nurses,22 and better nurse work environments.12, 23-24 The Magnet Recognition Program® does not specify nurse staffing levels or educational or specialty certification requirements for bedside nurses. Instead, the program requires evidence-based processes aimed at organizational reform of nurses’ work environment in relation to desired patient outcomes. Hospitals are evaluated for evidence of achieving goals in five areas: transformational leadership; structural empowerment; exemplary professional practice; new knowledge, innovations, and improvements; and empirical outcomes.
Thus, a follow-up to the 1994 paper must go beyond determining whether a mortality advantage can be documented for formally designated Magnet hospitals. Our inquiry must delve into the possible explanations for such an advantage, if found, because there is now a substantial scientific base documenting the association between nursing and patient outcomes. In the 1994 paper, Magnet designation was used as a proxy for good nursing because details of nurse staffing, education, qualifications, and work environments could not be measured with available data. That is no longer the case. A multi-state survey of nurses in California, Pennsylvania, New Jersey, and Florida provides direct measures of key elements of nursing organization and practice across all general, acute care hospitals in these four large states.23 Additionally, Magnet designation is now a formal process involving evidence-based criteria, on-site evaluations, and re-designation every four years with higher standards required the longer the designation is held.25 We use the data from the four states to examine this new environment and to determine whether Magnet hospitals continue to evince organizational characteristics that differentiate them from other hospitals, and if so, the extent to which these characteristics are associated with lower risk-adjusted mortality and failure-to-rescue.
Our hypothesis is that Magnet hospitals should “out-perform” non-Magnet hospitals. Differences in patient outcomes should be associated with the organizational features of nursing that can be measured. However, there may be a Magnet effect above and beyond the effect attributable to the measured nursing features alone.
METHODS
Data Sources and Sample
We analyzed data on adult, general Magnet and non-Magnet hospitals from four states (California, Florida, Pennsylvania and New Jersey) in 2006-2007. The four states were a convenience sample based upon funding availability but these are four of the nation’s largest states, and the characteristics of their hospitals, which account for more than 20% of annual hospitalizations, are roughly similar to hospitals nationally. We identified Magnet hospitals based on ANCC data indicating Magnet recognized hospitals as of 2006 as well as those newly recognized in 2007. The hospitals recently recognized were included because the application review and credentialing process takes at least a year to complete. Our sample included 56 Magnet and 508 non-Magnet general acute hospitals in the four states in 2006-2007.
We have detailed data on nursing factors from virtually all hospitals in the four study states from a unique survey of over 100,000 registered nurses. We sampled registered nurses from state licensure lists and surveyed them by mail.23 The nurses identified their employing hospital, which allowed us to aggregate responses to the hospital level.
All nursing-related measures were drawn from the survey
Nurses provided detailed information about their work environment. This included the features of nursing that have been associated with differences in patient outcomes such as staffing levels, levels of nurse education, and the presence of a work environment conducive to professional nursing practice.18-21, 23, 26
Nurse staffing was measured by aggregating nurses’ reports of the number of patients cared for on the last shift within each hospital. To maintain reliability, analysis was restricted to hospitals with 10 or more nurse respondents.23, 26-28 The staffing measure has been repeatedly shown to be predictive of both nurse and patient outcomes,12, 18, 23, 26 and superior to administrative data, in all likelihood because it includes only inpatient nurses in direct care roles. Respondents reported how many licensed practical nurses (LPNs) were working on their unit on their most recent shift so we could calculate skill mix as the percent of all licensed nurses (registered nurses plus LPNs) who were registered nurses. Education level of a hospital’s nursing workforce was calculated as the percent of direct care registered nurses with a bachelor of science in nursing (BSN) or higher degree.21
The nurse work environment was measured with the Practice Environment Scale of the Nursing Work Index (PES-NWI), an instrument recommended by the National Quality Forum as an organization-level nursing performance measure.29 The PES-NWI includes subscale items related to nurse participation in hospital affairs; nursing foundations for quality care; nurse manager ability, leadership, and support of nurses; staffing and resource adequacy; and collegial nurse–physician relations. Nurses indicated their level of agreement on whether certain features were characteristic of their workplace. Subscale measures were calculated for each hospital by averaging the subscale item values for all the nurses in the hospital. We then created a single practice environment score for each hospital by averaging the aggregated subscales.23 Standard aggregation statistics (ICC(1) = 0.11; ICC(2) = 0.81; omega-squared = 0.11; eta-squared = 0.136) support reliable hospital-level aggregation with a minimum of 10 nurse respondents per hospital.
The nurse survey also allowed us to create hospital level measures of other features of nursing including each hospital’s proportion of specialty-certified nurses, proportion of nurses educated outside of the U.S., proportion of medical–surgical unit nurses, proportion of intensive care unit nurses, proportion of supplemental or agency nurses, nurses’ average age and average years of experience, and proportion of male nurses. These variables were used to determine ways in which Magnet hospitals differed from other hospitals with respect to nursing.
Data on structural characteristics of hospitals, such as size, level of technology, and teaching status, were from the 2006-2007 American Hospital Association (AHA) annual hospital survey. Hospital characteristics associated with differences in patient outcomes30-31 and with organizational innovation32 were included as controls in final models. Teaching intensity was measured as the ratio of physician residents and fellows to hospital beds. High technology hospitals were those that performed open heart surgery, organ transplantation, or both. Hospital size was represented by the number of staffed and licensed beds. Ownership was indicated as non-profit versus for-profit. We included indicators for hospital state and location in a rural, micropolitan, metropolitan, or division core-based statistical area. We used the Herfindahl-Hirschman index (HHI) as a proxy for market competition.
Patient outcomes data were from hospital discharge abstract databases from the four states. We limited our focus to patients ages 21-85 undergoing general, orthopedic, or vascular surgery (see Table, Supplementary Digital Content 1 for Diagnosis Related Groups [DRG] codes defining the sample). Surgical patients are well-represented in most general acute care hospitals and there are established risk-adjustment procedures for administrative data with this population.33-37 Discharges against medical advice were excluded. Measures included 30-day inpatient mortality and failure-to-rescue, defined as deaths among surgical patients who experienced complications.38 The ICD-9-CM codes in the secondary diagnosis and procedure fields of discharge abstracts were reviewed to identify evidence of 39 clinical events indicative of complications (e.g., wound infection, pneumothorax, peritonitis).34 We used Elixhauser’s risk-adjustment approach which identifies 27 comorbidities (excluding fluid and electrolyte disorders and coagulopathy).33-37 Sex, age, and 61 dummy variables based on DRG code indicating the surgery type were also included. Risk-adjustment was enhanced using a 180-day look back to previous hospitalizations. C-statistics for the risk-adjusted mortality and failure-to-rescue models were 0.89 and 0.82, respectively.
Analyses
After descriptive analyses, we used logistic regression models to examine the association between Magnet recognition and patient outcomes, adjusting for differences in patient characteristics and hospital factors other than nursing. Next, we examined the degree to which the effect of Magnet status on outcomes could be explained by nursing factors.
To summarize the organizational nursing characteristics for each hospital, we created a variable using logistic regression to estimate the probability of a hospital being a Magnet hospital based on its nursing characteristics. The model included nursing characteristics more likely to be found in Magnet hospitals8, 10 such as lower patient-to-nurse ratios, better work environments, higher proportions of BSN-prepared nurses, and higher proportions of specialty-certified nurses. We also included variables that might moderate the relationship between these characteristics and Magnet status such as the hospital’s proportion of nurses educated outside of the U.S., proportion of supplemental or agency supplied nurses, proportion of male nurses, and the average age and average years of experience of the hospital nurse workforce (see Table, Supplementary Digital Content 2 for full regression).39-40
Using this composite (propensity) score allowed us to evaluate whether, as presumed in 1994, there was evidence that differences in the organization of nursing accounted for the better patient outcomes seen in Magnet hospitals. We could then determine whether any effect of Magnet recognition over and above the measured characteristics remained. We estimated standard errors and significance using procedures that accounted for clustering of patients within hospitals.41 All analyses were conducted with STATA v.11.
RESULTS
There were differences in hospital characteristics between Magnet and non-Magnet hospitals (Table 1). A larger proportion of Magnet hospitals were large, non-profit, high-technology, teaching hospitals. This is consistent with the 1994 findings.4
TABLE 1.
Study Hospital Characteristics (n=564)
| Mean (SD) or No. (%) | |||
|---|---|---|---|
|
| |||
| Characteristic | Magnet (n=56) |
Non-Magnet (n=508) |
P * |
| Nursing-related characteristic | |||
| Nurse work environment (PES-NWI) | 2.86 (0.18) | 2.66 (0.22) | <0.001 |
| Proportion of nurses holding a BSN or higher | 0.46 (0.12) | 0.39 (0.14) | <0.001 |
| Proportion of specialty-certified nurses | 0.40 (0.14) | 0.36 (0.13) | 0.029 |
| Staffing, patients per nurse | 4.82 (0.73) | 5.03 (1.09) | 0.056 |
| Skill mix (ratio of RNs to total licensed staff) | 0.75 (0.04) | 0.75 (0.08) | 0.746 |
| Supplemental nurse staffing | 0.39 (0.35) | 0.51 (0.54) | 0.025 |
| Proportion of medical-surgical unit nurses | 0.16 (0.07) | 0.17 (0.09) | 0.363 |
| Proportion of intensive care unit nurses | 0.17 (0.06) | 0.17 (0.09) | 0.911 |
| Proportion of US-educated nurses | 0.85 (0.11) | 0.86 (0.15) | 0.780 |
| Years of experience at current hospital | 11.5 (2.9) | 11.4 (2.9) | 0.816 |
| Proportion of female nurses | 0.94 (0.04) | 0.93 (0.05) | 0.099 |
| Composite nursing measure | 0.24 (0.17) | 0.08 (0.10) | <0.001 |
| Hospital characteristic | |||
| State, no. (%) | <0.001 | ||
| New Jersey | 18 (32.1) | 52 (10.2) | |
| Pennsylvania | 11 (19.6) | 123 (24.2) | |
| Florida | 17 (30.4) | 124 (24.4) | |
| California | 10 (17.9) | 209 (41.1) | |
| No. of beds | 398 (195) | 261 (193) | <0.001 |
| Technology status, no. (%) | <0.001 | ||
| High | 39 (69.6) | 212 (41.7) | |
| Low | 17 (30.4) | 296 (58.3) | |
| Teaching status, no. (%) | 0.052 | ||
| Major | 9 (16.1) | 36 (7.1) | |
| Minor | 23 (41.1) | 208 (40.9) | |
| Non-teaching | 24 (42.9) | 264 (52.0) | |
| Non-profit ownership, no. (%) | 56 (100.0) | 406 (79.9) | <0.001 |
t-tests for hospital specific means and chi-square tests for binary variables
Magnet hospitals had significantly better work environments (PES-NWI composite score of 2.86 in Magnet hospitals compared to 2.66 in non-Magnet hospitals [p <0.001]). They also had significantly higher proportions of BSN-educated nurses (0.46 vs. 0.39; p <0.001), higher proportions of specialty-certified nurses (0.40 vs. 0.36; p <0.03), and lower proportions of supplemental nursing staff (0.39 vs. 0.51; p <0.03). Nurse staffing was better in Magnet hospitals compared to non-Magnet hospitals (4.82 vs. 5.03 patients per nurse; p = 0.056). The composite nursing measure, a propensity score indicating the likelihood of an institution being a Magnet hospital conditional on nursing features, differed significantly between Magnet and non-Magnet hospitals (0.24 vs. 0.08 respectively; p <0.001).
Table 2 shows the characteristics of surgical patients and differences in mortality and failure-to-rescue between Magnet and non-Magnet hospitals. Of the surgical patients in Magnet hospitals, 1.5% died within 30 days compared to 1.8% in non-Magnet hospitals (p <0.001). In Magnet hospitals, 3.8% of the surgical patients with complications died (failure-to-rescue) compared to 4.6% in non-Magnet hospitals (p <0.001).
Table 2.
Characteristics of Surgical Patients (n=641,187)
| Magnet Hospitals (N=109,090) |
Non-Magnet Hospitals (N=532,097) |
Relative
Risk * |
P | |
|---|---|---|---|---|
|
|
||||
| Characteristic | % (No.) | % (No.) | ||
| Age (y), mean (SD) | 59.9 (15.9) | 60.1 (16.2) | — | 0.001 |
| Deaths within 30 days of admission | 1.51 (1,645) | 1.79 (9,528) | 0.84 | <0.001 |
| Complications | 34.5 (37,631) | 33.7 (179,650) | 1.02 | <0.001 |
| Failure-to-rescue | 3.83 (1,440) | 4.55 (8,158) | 0.84 | <0.001 |
| Male | 43.2 (47,080) | 43.6 (232,202) | 0.99 | 0.028 |
| Major Diagnostic Categories | ||||
| General surgery | ||||
| Digestive system diseases | 21.8 (23,800) | 21.9 (116,281) | 1.00 | 0.815 |
| Hepatobiliary system diseases | 10.0 (10,928) | 10.8 (57,222) | 0.93 | <0.001 |
| Skin, subcutaneous tissue, and breast diseases | 3.7 (4,034) | 3.4 (18,060) | 1.09 | <0.001 |
| Endocrine, nutritional, and metabolic diseases | 6.3 (6,829) | 5.2 (27,814) | 1.20 | <0.001 |
| Orthopedic surgery | ||||
| Musculoskeletal system diseases | 52.3 (57,056) | 53.3 (283,357) | 0.98 | <0.001 |
| Vascular surgery | ||||
| Circulatory system diseases | 5.9 (6,443) | 5.5 (29,363) | 1.07 | <0.001 |
| Medical history (comorbidities) | ||||
| Hypertension | 48.7 (53,113) | 49.5 (263,512) | 0.98 | <0.001 |
| Chronic pulmonary disease | 13.9 (15,128) | 15.2 (80,736) | 0.91 | <0.001 |
| Diabetes without chronic complications | 14.4 (15,715) | 15.6 (82,930) | 0.92 | <0.001 |
| Metastatic cancer | 3.9 (4,252) | 3.1 (16,532) | 1.25 | <0.001 |
| Congestive heart failure | 4.3 (4,682) | 5.1 (26,907) | 0.85 | <0.001 |
| Liver disease | 2.4 (2,620) | 2.4 (12,679) | 1.01 | 0.712 |
| Obesity | 8.0 (8,712) | 9.5 (50,630) | 0.84 | <0.001 |
| Depression | 7.8 (8,533) | 7.7 (40,915) | 1.02 | 0.151 |
We estimated the relative risk of each binary descriptor to give an indication of the size of differences between the populations served by Magnet and non-Magnet hospitals. The effect size (Cohen’s d) for age was very small (0.008).
Table 3 shows odds ratios for the effect of Magnet status (Model 1), the effect of the composite measure of nursing (Model 2), and the combined effect (Model 3; Magnet status and composite measure of nursing estimated in the same model) on the outcomes (separately) of 30-day inpatient mortality and failure-to-rescue (see Table, Supplementary Digital Content 3 for full regression results). All of the results shown are from models that controlled for patient and hospital characteristics.
Table 3.
Odds Ratios Indicating Effects of Magnet Hospital Recognition and Composite Measure of Nursing on 30-day Mortality and Failure-to-Rescue (n=641,187)
| Patient Outcomes | Model 1 Magnet Only OR (95% CI) |
Model 2 Nursing Only OR (95% CI) |
Model 3 Magnet & Nursing OR (95% CI) |
|---|---|---|---|
| 30-day surgical mortality | |||
| Magnet vs. non-Magnet | 0.80 (0.71-0.89) | 0.86 (0.76-0.98) | |
| Composite nursing measure | 0.50 (0.38-0.67) | 0.62 (0.44-0.87) | |
| Failure-to-rescue | |||
| Magnet vs. non-Magnet | 0.81 (0.72-0.91) | 0.88 (0.77-1.01) | |
| Composite nursing measure | 0.48 (0.37-0.63) | 0.57 (0.41-0.79) |
All estimates represent odds ratios derived from robust logistic regression models that accounted for clustering of observations within hospitals and controlled for patient characteristics (age, sex, diagnosis related group, comorbidities) and hospital controls (technology; teaching status; number of beds; ownership status; Herfindhahl-Hirschman Index; rural, micropolitan, metropolitan, or division core-based statistical area; and indicator for state).
Model 1 shows that the odds of 30-day mortality (OR 0.80, 95% CI 0.71-0.89, p <0.001) and failure-to-rescue (OR 0.81, 95% CI 0.72-0.91, p<0.001) are significantly lower for surgical patients in Magnet hospitals compared to non-Magnet hospitals. In Model 2, the composite measure of nursing, estimated as the likelihood of a hospital being Magnet credentialed as a function of nursing factors, was significantly associated with lower odds of mortality (OR 0.50, 95% CI 0.38-0.67, p<0.001) and failure-to-rescue (OR 0.48, 95% CI 0.37-0.63, p <0.001). This model did not include an indicator of Magnet hospital status.
Model 3 included both the Magnet status indicator and the composite nursing measure. The composite nursing measure was significantly associated with mortality (OR 0.62, 95% CI 0.44-0.87, p=0.005). The effect of Magnet status was also significant (OR 0.86, 95% CI 0.76-0.98, p=0.02) but the magnitude was not as large as Model 1 (a model including the Magnet status indicator only). Similar results were seen for failure-to-rescue with a significant composite nursing measure (OR 0.57, 95% CI 0.41-0.79, p <0.001) and a Magnet effect approaching significance (OR 0.88, 95% CI 0.77-1.01, p=0.07). There was not a significant interaction between Magnet status and the composite score.
DISCUSSION
In 1994, Aiken, Smith, and Lake4 showed that mortality rates were lower in Magnet versus non-Magnet hospitals. Nearly two decades later, we find that surgical patients cared for in Magnet hospitals have significantly lower odds of mortality and failure-to-rescue than those cared for in non-Magnet facilities. Differences in nursing between Magnet and non-Magnet hospitals account in part for this relationship. Nevertheless, even after accounting for organizational aspects of nursing, significant residual differences in patient outcomes were captured by Magnet hospital recognition. Controlling for differences in nursing, hospital, and patient characteristics, surgical patients in Magnet hospitals had 14% lower odds of inpatient death within 30-days and 12% lower odds of failure-to-rescue compared to patients cared for in non-Magnet hospitals.
The original paper suggested that the mortality effect demonstrated in Magnet hospitals derived not just from the mix of credentials and education or number of nurses, but from “the greater status, autonomy, and control afforded nurses in the Magnet hospitals, and their resulting impact on nurses’ behaviors on behalf of patients.”4 Over the years, the preponderance of evidence has borne this out—the organization of nursing care makes a significant difference in patient outcomes.12, 18-21, 23, 26 In this study, we have done what could not be done previously— directly measure the work environment with a variety of indicators, including nurse-survey based measures of the practice environment. Our findings reinforce that better work environments for nurses are the distinguishing factor between Magnet and non-Magnet hospitals and are key to better patient outcomes. The Magnet Recognition Program® is not the only means of improving the work environment, but it may provide a replicable blueprint for doing so.
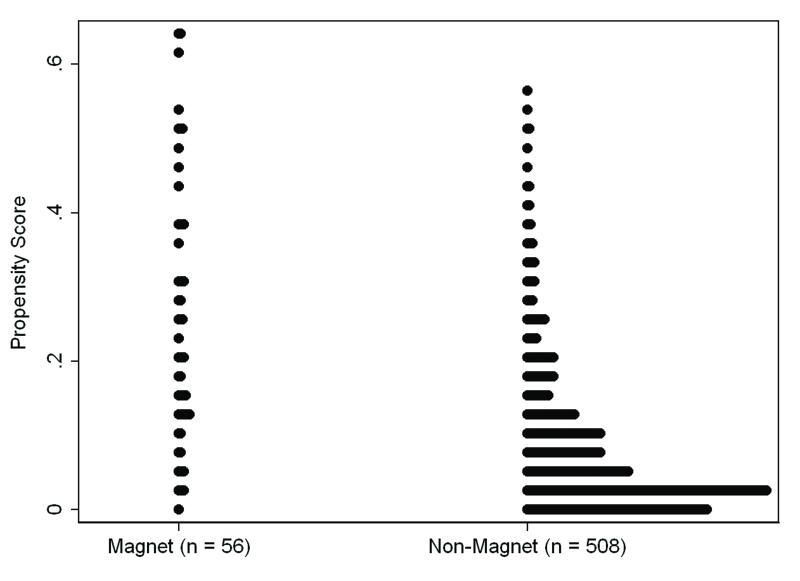
A residual effect of Magnet status suggests that not all of the Magnet effect is explained by the measured nursing characteristics. We found some hospitals not designated as Magnet hospitals shared positive nursing features, while some Magnet hospitals’ organizational nursing strengths were not evident on the surface. Figure 1 shows the distribution of the composite nursing measure for Magnet and non-Magnet hospitals. The vertical axis is the composite nursing score and the horizontal axis shows the number of Magnet and non-Magnet hospitals separately. If our nursing factors were perfect indicators of Magnet status, all of the Magnet hospitals would cluster at the top of the vertical axis and all of the non-Magnet hospitals would cluster at the bottom. The graph suggests that most of the non-Magnet hospitals cluster at the bottom and have relatively low propensity scores, as expected. A relatively higher proportion of Magnet hospitals are distributed in the higher range of the composite nursing score. However, there are some non-Magnet hospitals that look similar to Magnet hospitals in terms of nursing (i.e., they have high composite nursing scores[or propensities]). Likewise, some Magnet hospitals had relatively low composite nursing scores based on the measured nursing characteristics.
FIGURE 1. Comparison of Composite Measure of Nursing (Propensity Scores) for Magnet vs. Non-Magnet Hospitals.
Note: Each dot indicates a hospital
If it were the case that some Magnet hospitals achieved recognition despite having less favorable nursing characteristics than the rest of the Magnet cohort, it is unlikely that Magnet hospitals would be associated with better outcomes. The net effect of the alternative organizational forms (a relatively large number of Magnet hospitals with high composite nursing scores and some with lower composite nursing scores) resulted in our finding that, on average, Magnet hospitals “out-performed” non-Magnet hospitals. These differences were largely captured by the organizational features of nursing that we measured. If we could perfectly measure all the nursing factors associated with Magnet recognition along with any other organizational factors that differentiated Magnet hospitals and lead to better outcomes, we would fully account for the Magnet effect. This was not the case—we found a Magnet effect above and beyond that attributable to the measured organizational characteristics alone.
The residual association between Magnet recognition and outcomes likely signifies a complex organizational condition such as the institution’s commitment to excellence or willingness to undertake organizational innovation.32, 42 These conditions can have positive spillover effects and contribute to a work environment conducive to quality nursing care. The organizational culture change brought about through Magnet recognition requires but also results in leadership and organizational commitment.43-45 Case reports from hospitals that achieved Magnet recognition, those in the process of accreditation, and even those that have applied for Magnet recognition but have failed, support this notion. These institutions report positive organizational change as a benefit of the process.46-48
It is also possible that Magnet recognition is a marker of pre-existing quality, pursued by hospitals that had better outcomes before Magnet recognition. This could come about if hospitals prone to organizational innovation engage in other quality-related programs that account for part of the Magnet advantage over and above the factors we measured. To help us discern whether better outcomes were present in Magnet hospitals before they achieved Magnet status, we conducted a counterfactual analysis excluding the 56 Magnet hospitals but coding the hospitals eventually recognized as Magnets (n=24) in the years following our observation period to 1 and other non-Magnet hospitals to 0. Estimating the same models, we found that better outcomes were not predicted by a hospital’s eventual Magnet status; i.e., better outcomes do not appear to precede Magnet recognition (see Table, Supplementary Digital Content 4). We also found that, among the 24 hospitals that achieved Magnet status after 2007, the composite score declines as the gap between the observation period and eventual Magnet recognition increases (see Table, Supplementary Digital Content 5). This suggests that as hospitals come closer to achieving Magnet recognition, they increasingly look more like other Magnet hospitals in terms of nursing characteristics and less like non-Magnet hospitals. Additional studies with designs that reduce endogeneity bias should continue to be pursued.
Continued progress in measuring the organization of nursing services should provide additional perspective. Process measures would provide insight regarding differences between Magnet and non-Magnet hospitals at the patient-nurse interface. Measuring staffing is imperfect and although our approach has been shown to have better predictive validity than other sources, we assessed whether differences depended on the measure. We calculated the same propensity score except substituted a common staffing measure using AHA annual survey data. The results did not change. California implemented a minimum nurse-to-patient ratio mandate in 2004, however, models that excluded or were limited only to California hospitals were substantively similar. There are papers showing no outcomes advantage for Magnet hospitals. These studies, however, were limited to narrow pediatric populations49 and university-affiliated hospitals;50 if more representative, these studies may have captured the outcomes advantage we saw across the range of Magnet hospitals.
CONCLUSION
The number of Magnet recognized hospitals has increased more than tenfold since the first paper identifying the relationship between Magnet hospitals and patient outcomes. Magnet recognized hospitals continue to demonstrate better outcomes, in this case, lower surgical mortality and failure-to-rescue. Their better outcomes could be attributed in large part, but not entirely, to investments in highly qualified and educated nurses, and practice environments supportive of high quality nursing care. The identification of a Magnet advantage in patient outcomes beyond measureable features of nursing suggests that the process of applying for and retaining Magnet recognition, and the networking opportunities that come with Magnet recognition may promote continuing quality improvement and organizational innovation.
Supplementary Material
SUPPLEMENTAL TABLE 1 Title: Surgical Patient Diagnosis Related Groups
SUPPLEMENTAL TABLE 2. Title: Propensity Score Model Logit Coefficients
Note: Logit coefficients represent the change in the log odds of being a Magnet (versus a non-Magnet) hospital for every one unit change in independent variable
SUPPLEMENTAL TABLE 3. Title: Full regression models
SUPPLEMENTAL TABLE 4 Title: Odds Ratios Indicating Effects of Eventual Magnet Hospital Status (after 2006-07) and Composite Measure of Nursing on 30-day Mortality and Failure-to-Rescue in Non-Magnet Hospitals
SUPPLEMENTAL TABLE 5 Title: Mean Composite Measure of Nursing for Magnet Hospitals, Hospitals that Eventually Became Magnet Hospitals after 2007, and Non-Magnet Hospitals
Acknowledgements
Funding for this study was provided by the Robert Wood Johnson Foundation Nurse Faculty Scholars program (McHugh), National Institute of Nursing Research (R01-NR-004513, P30-NR-005043, T32-NR007104, Aiken), and the American Nurses Foundation (Kelly).
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Matthew D. McHugh, Corresponding Author Robert Wood Johnson Foundation Nurse Faculty Scholar Center for Health Outcomes and Policy Research University of Pennsylvania.
Lesly A. Kelly, College of Nursing and Health Innovation Arizona State University.
Herbert L. Smith, Department of Sociology, Population Studies Center University of Pennsylvania.
Evan S. Wu, Center for Health Outcomes and Policy Research University of Pennsylvania.
Jill M. Vanak, Center for Health Outcomes and Policy Research University of Pennsylvania.
Linda H. Aiken, Center for Health Outcomes and Policy Research University of Pennsylvania.
REFERENCES
- 1.Kramer M, Schmalenberg C. Magnet hospitals: Part I. Institutions of excellence. J Nurs Adm. 1988;18:13–24. [PubMed] [Google Scholar]
- 2.Kramer M, Schmalenberg C. Magnet hospitals: Part II. Institutions of excellence. J Nurs Adm. 1988;18:11–19. [PubMed] [Google Scholar]
- 3.Scott JG, Sochalski J, Aiken L. Review of magnet hospital research: findings and implications for professional nursing practice. J Nurs Adm. 1999;29:9–19. doi: 10.1097/00005110-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Med Care. 1994;32:771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 5.American Nurses Credentialing Center [Accessed May 1, 2012];History of the Magnet Program. 2011 Available at: http://www.nursecredentialing.org/MagnetHistory.aspx.
- 6.Aiken LH, Havens DS, Sloane DM. The Magnet Nursing Services Recognition Program: A comparison of two groups of Magnet hospitals. Am J Nurs. 2000;100:26–35. [PubMed] [Google Scholar]
- 7.Trinkoff AM, Johantgen M, Storr CL, et al. A comparison of working conditions among nurses in magnet and non-magnet hospitals. J Nurs Adm. 2010;40:309–315. doi: 10.1097/NNA.0b013e3181e93719. [DOI] [PubMed] [Google Scholar]
- 8.Kelly L, McHugh M, Aiken L. Nurse outcomes in Magnet® and non-Magnet® hospitals. J Nurs Adm. 2011;41:428–433. doi: 10.1097/NNA.0b013e31822eddbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lacey SR, Cox KS, Lorfing KC, et al. Nursing support, workload, and intent to stay in Magnet, Magnet-aspiring, and non-Magnet hospitals. J Nurs Adm. 2007;37:199. doi: 10.1097/01.NNA.0000266839.61931.b6. [DOI] [PubMed] [Google Scholar]
- 10.Lake ET, Friese CR. Variations in nursing practice environments: relation to staffing and hospital characteristics. Nurs Res. 2006;55:1–9. doi: 10.1097/00006199-200601000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Upenieks VV. The interrelationship of organizational characteristics of magnet hospitals, nursing leadership, and nursing job satisfaction. Health Care Manage. 2003;22:83–98. doi: 10.1097/00126450-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Aiken LH, Clarke SP, Sloane DM, et al. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38:223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lake ET, Shang J, Klaus S, et al. Patient falls: Association with hospital Magnet status and nursing unit staffing. Res Nurs Health. 2010;33:413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lake ET, Staiger D, Horbar J, et al. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307:1709–1716. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McClure ML, Hinshaw AS. Magnet hospitals revisited: Attraction and retention of professional nurses. American Nurses Association; 2002. [Google Scholar]
- 16.Drenkard K. The business case for Magnet. J Nurs Adm. 2010;40:263–271. doi: 10.1097/NNA.0b013e3181df0fd6. [DOI] [PubMed] [Google Scholar]
- 17.The Leapfrog Group [Accessed May 10, 2012];Hospitals Reporting Magnet Status to the 2011 Leapfrog Hospital Survey. 2011 Available at: http://www.leapfroggroup.org/MagnetRecognition.
- 18.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 19.Kane RL, Shamliyan T, Mueller C, et al. Nursing Staffing and Quality of Patient Care. Agency for Healthcare Research and Quality; Rockville, MD: 2007. [Google Scholar]
- 20.Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 21.Aiken LH, Clarke SP, Cheung RB, et al. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kendall-Gallagher D, Aiken LH, Sloane DM, et al. Nurse specialty certification, inpatient mortality, and failure to rescue. J Nurs Scholarsh. 2011;43:188–194. doi: 10.1111/j.1547-5069.2011.01391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aiken LH, Cimiotti JP, Sloane DM, et al. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49:1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duffield C, Diers D, O’Brien-Pallas L, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res. 2010 doi: 10.1016/j.apnr.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 25.American Nurses Credentialing Center . The Magnet Model Components and Sources of Evidence: Magnet Recognition Program. ANCC; Silver Spring, MD: 2008. [Google Scholar]
- 26.Kutney-Lee A, McHugh MD, Sloane DM, et al. Nursing: a key to patient satisfaction. Health Aff (Millwood) 2009;28:w669–w677. doi: 10.1377/hlthaff.28.4.w669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McHugh MD, Kutney-Lee A, Cimiotti JP, et al. Nurses’ widespread job dissatisfaction, burnout and frustration with health benefits signal problems for patient care. Health Aff (Millwood) 2011;30:202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aiken LH, Sloane DM, Cimiotti JP, et al. Implications of the California nurse staffing mandate for other states. Health Serv Res. 2010;45:904–921. doi: 10.1111/j.1475-6773.2010.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 30.Hartz AJ, Krakauer H, Kuhn EM, et al. Hospital characteristics and mortality rates. N Engl J Med. 1989;321:1720–1725. doi: 10.1056/NEJM198912213212506. [DOI] [PubMed] [Google Scholar]
- 31.Brennan TA, Hebert LE, Laird NM, et al. Hospital characteristics associated with adverse events and substandard care. JAMA. 1991;265:3265–3269. [PubMed] [Google Scholar]
- 32.Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Silber JH, Rosenbaum PR, Romano PS, et al. Hospital teaching intensity, patient race, and surgical outcomes. Arch Surg. 2009;144:113–120. doi: 10.1001/archsurg.2008.569. discussion 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45:918–925. doi: 10.1097/MLR.0b013e31812e01cc. [DOI] [PubMed] [Google Scholar]
- 35.Glance LG, Dick AW, Osler TM, et al. Does date stamping ICD-9-CM codes increase the value of clinical information in administrative data? Health Serv Res. 2006;41:231–251. doi: 10.1111/j.1475-6773.2005.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 38.Silber JH, Williams SV, Krakauer H, et al. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care. 1992;30:615–629. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice. Biometrics. 1996;52:249–264. [PubMed] [Google Scholar]
- 40.Stuart E. Matching methods for causal inference: A review and a look forward. Stat Sci. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–838. [Google Scholar]
- 42.Kimberly JR, Evanisko MJ. Organizational innovation: The influence of individual, organizational, and contextual factors on hospital adoption of technological and administrative innovations. Acad Manage J. 1981:689–713. [PubMed] [Google Scholar]
- 43.Havens DS, Aiken LH. Shaping systems to promote desired outcomes: the magnet hospital model. J Nurs Adm. 1999;29:14. doi: 10.1097/00005110-199902000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Gilmore TN, Shea GP, Useem M. Side effects of corporate cultural transformations. The J Appl Behav Sci. 1997;33:174. [Google Scholar]
- 45.Aiken M, Hage J. The organic organization and innovation. Sociology. 1971;5:63–82. [Google Scholar]
- 46.Miller L, Anderson F. Lessons learned when Magnet designation is not received. J Nurs Adm. 2007;37:131. doi: 10.1097/01.NNA.0000262733.21747.f1. [DOI] [PubMed] [Google Scholar]
- 47.Upenieks VV, Sitterding M. Achieving magnet redesignation: a framework for cultural change. J Nurs Adm. 2008;38:419. doi: 10.1097/01.NNA.0000338154.25600.e0. [DOI] [PubMed] [Google Scholar]
- 48.Stolzenberger KM. Beyond the Magnet award: The ANCC Magnet program as the framework for culture change. J Nurs Adm. 2003;33:522–531. doi: 10.1097/00005110-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 49.Hickey P, Gauvreau K, Connor J, et al. The Relationship of Nurse Staffing, Skill Mix, and Magnet (R) Recognition to Institutional Volume and Mortality for Congenital Heart Surgery. J Nurs Adm. 2010;40:226–232. doi: 10.1097/NNA.0b013e3181da3f71. [DOI] [PubMed] [Google Scholar]
- 50.Goode CJ, Blegen MA, Park SH, et al. Comparison of Patient Outcomes in Magnet® and Non-Magnet Hospitals. J Nurs Adm. 2011;41:517–523. doi: 10.1097/NNA.0b013e3182378b7c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPLEMENTAL TABLE 1 Title: Surgical Patient Diagnosis Related Groups
SUPPLEMENTAL TABLE 2. Title: Propensity Score Model Logit Coefficients
Note: Logit coefficients represent the change in the log odds of being a Magnet (versus a non-Magnet) hospital for every one unit change in independent variable
SUPPLEMENTAL TABLE 3. Title: Full regression models
SUPPLEMENTAL TABLE 4 Title: Odds Ratios Indicating Effects of Eventual Magnet Hospital Status (after 2006-07) and Composite Measure of Nursing on 30-day Mortality and Failure-to-Rescue in Non-Magnet Hospitals
SUPPLEMENTAL TABLE 5 Title: Mean Composite Measure of Nursing for Magnet Hospitals, Hospitals that Eventually Became Magnet Hospitals after 2007, and Non-Magnet Hospitals