Abstract
A PCR-based assay to identify Streptococcus gallolyticus has been developed. The assay uses an oligonucleotide primer pair targeting a partial sequence of the manganese-dependent superoxide dismutase gene (sodA). The assay distinguished members of the S. gallolyticus group from other, closely related taxa successfully by yielding a 408-bp specific amplicon.
Streptococcus gallolyticus is often found as a normal member of the gut microflora of various animals (15), while it has been reported to cause mastitis in cattle (8), septicemia in pigeons (3), and meningitis, sepsis, and endocarditis in humans (2, 4, 12). There have also been a number of case reports that suggest an etiological link between underlying infection with this organism and colon cancers in human (1, 5, 9, 10, 11). Most, if not all, of the strains belonging to this species are able to decarboxylate gallate as well as produce tannase, by which a hydrolyzable tannin (i.e., gallotannin) is hydrolyzed to release gallic acid, which is subsequently decarboxylated to pyrogallol (14). The species, which includes strains formerly identified as S. bovis biotypes I and II/2, can be distinguished from other, related taxa or biotypes (i.e., S. equinus, S. bovis biotype II/1) on the basis of the results of DNA-DNA reassociation experiments (14). In a recent taxonomic review, Facklam (6) has suggested that all human isolates of S. bovis biotypes I and II/2 are officially identified as S. gallolyticus. Nevertheless, the use of the name S. bovis biotype I or II/2 instead of S. gallolyticus has been a common occurrence in clinical microbiology despite the clearly established status of the latter name (14). This situation seems to have come about in order to avoid confusion among clinical microbiologists. Recently, Poyart et al. (18) demonstrated that a partial sequence of the manganese-dependent superoxide dismutase gene (sodA) provides useful information for the differentiation of species of the so-called S. bovis-S. equinus group. Here we evaluated the use of a PCR-based method for identification of S. gallolyticus that uses a primer pair targeting sodA by using strains of the S. bovis-S. equinus group from our culture collection with known DNA-DNA homology status.
Twenty-three streptococcal strains that had been previously designated S. gallolyticus (14) and seven strains that had been assigned by Farrow et al. (7) to S. equinus were used in the present study. Whole genomic DNA-DNA homology had been used previously (14) to determine the taxonomic position of these strains, in which the relative percent DNA binding of each strain with S. gallolyticus ACM 3611T was measured (Table 1). The S. gallolyticus strains consisted of 12 fecal or rumen isolates from various animals and 11 clinical isolates from cases of cow mastitis and human septicemia or endocarditis. It should be noted that the seven S. equinus strains included five strains originally received as S. bovis. All strains were cultured at 37°C on Columbia blood agar (Oxoid Ltd., Basingstoke, United Kingdom) with 5% defibrinated horse blood prior to use. The strains were characterized for their biochemical properties with a commercial identification kit (API 20 Strep; bioMérieux, Lyon, France). Tannase and gallic acid decarboxylating activities of strains were determined by visual methods described elsewhere (16, 17).
TABLE 1.
Strains used in this study and their biochemical and genotypic characteristics
| Straina | Source | % Binding with S. gallo- lyticus ACM 3611T DNAb | Phenotypic identity deter- mined by API 20 Strep | Tannase | Gallate decar- boxylation | Result of PCR targeting sodA |
|---|---|---|---|---|---|---|
| S. gallolyticus fecal isolates | ||||||
| ACM 3611T | Koala feces | 100 | S. bovis biotype I | + | + | + |
| ACM 3612 | Koala feces | 74 | S. bovis biotype I | + | + | + |
| ACM 3609 | Brushtail possum feces | 98 | S. bovis biotype I | + | + | + |
| ACM 3593 | Kangaroo feces | 81 | S. bovis biotype I | + | + | + |
| ACM 3850 | Ringtail possum feces | 72 | S. bovis biotype I | + | + | + |
| ACM 3849 | Cow feces | 69 | S. bovis biotype I | + | + | + |
| ACM 3551 (= NCDO 2572) | Cow rumen | 64 | S. bovis biotype I | + | + | + |
| ACM 3852 | Dog feces | 79 | S. bovis biotype I | + | + | + |
| ACM 3853 | Dog feces | 63 | S. bovis biotype I | + | + | + |
| ACM 3848 | Horse feces | 96 | S. bovis biotype I | + | + | + |
| ACM 3847 | Pig feces | 83 | S. bovis biotype I | + | + | + |
| ACM 3845 | Guinea pig feces | 87 | S. bovis biotype I | + | + | + |
| S. gallolyticus clinical isolates | ||||||
| ACM 3546 (= NCDO 2019) | Cow mastitis lesion | 74 | S. bovis biotype I | + | + | + |
| ACM 3547 (= NCDO 2088) | Cow mastitis lesion | 94 | S. bovis biotype I | + | + | + |
| ACM 3548 (= NCDO2134) | Cow mastitis lesion | 79 | S. bovis biotype I | + | + | + |
| ACM 3552 (= NCDO2631) | Human clinical case | 82 | S. bovis biotype I | + | + | + |
| ACM 3874 (= F-1867) | Human clinical case | 72 | S. bovis biotype I | + | + | + |
| ACM 3873 (= Vitec 1616) | Human clinical case | 82 | S. bovis biotype I | + | + | + |
| ACM 3902 (= CDC 002) | Human clinical case | 60 | S. bovis biotype I | + | + | + |
| ACM 3903 (= MG Eath) | Human clinical case | 77 | S. bovis biotype I | + | + | + |
| ACM 3870 (= CDC 1723-81) | Human clinical case | 60 | S. bovis biotype II/2 | − | + | + |
| ACM 3869 (= CDC 2266-81) | Human clinical case | 64 | S. bovis biotype II/2 | − | + | + |
| ACM 3871 (= CDC 008) | Human clinical case | 66 | S. bovis biotype II/2 | − | + | + |
| Strains of related taxa | ||||||
| S. bovis | ||||||
| ACM 3539 (= NCDO597T) | Cow feces | 25 | S. bovis biotype II/1 | − | − | − |
| ACM 3540 (= NCDO 598) | Cow feces | 26 | S. bovis biotype II/1 | − | − | − |
| ACM 3542 (= NCDO 1251) | Sheep rumen | 10 | S. bovis biotype II/1 | − | − | − |
| ACM 3543 (= NCDO 2128) | Cow feces | 20 | S. bovis biotype II/1 | − | − | − |
| S. equinus | ||||||
| ACM 3541 (= NCDO 1037T) | Horse feces | 15 | S. salivarius | − | − | − |
| ACM 3544 (= NCDO2445) | Horse feces | 10 | S. equinus | − | − | − |
| ACM 3545 (= NCDO 2446) | Horse feces | 23 | Unidentifiable | − | − | − |
ACM, Australian Collection of Microorganisms, Department of Microbiology, University of Queensland, St. Lucia, Queensland, Australia; NCDO, National Collection of Dairy Organisms, Reading, United Kingdom; CDC, Centers for Disease Control and Prevention strains; Vitec 1616, MG Eath, and F-1867, gifts from R. G. Knight, Department of Veterans Affairs Medical Center 10701, East London, United Kingdom.
As described in reference 20.
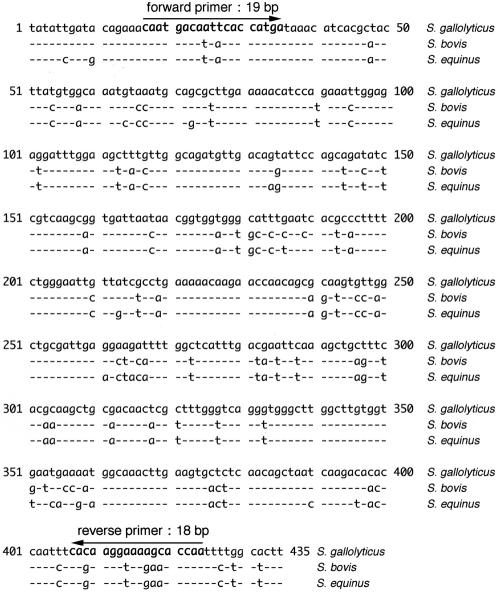
The sodA gene sequences of S. gallolyticus CIP105428T (GenBank accession no. AJ297183), S. bovis CIP102302 (GenBank accession no. Z95896), and S. equinus 102504T (GenBank accession no. Z95903) from the GenBank database were aligned and scanned for variable regions that could provide a suitable primer set specific to S. gallolyticus (Fig. 1). On the basis of this analysis, forward primer SgsodA-F (5′-CAATGACAATTCACCATGA-3′; positions 17 to 34) and reverse primer SgsodA-R (5′-TTGGTGCTTTTCCTTGTG-3′; positions 424 to 407) were designed as shown in Fig. 1. With this primer set, PCR amplification was performed in a total volume of 20 μl. Whole genomic DNA from each isolate was prepared by the method of Marmur (13). Two microliters of each genomic DNA preparation (10 ng of DNA/μl of Tris-EDTA) was added to the PCR master mixture, which consisted of 2 μl of 10× PCR buffer (Mg2+ free; Promega Corporation, Madison, Wis.), 2 μl of 25 mM MgCl2, 0.4 μl of a 10 mM deoxynucleoside triphosphate mixture, 0.5 μl of each primer (10 pmol/μl), and 0.1 μl (0.5 U) of Taq DNA polymerase (Promega), with the remaining volume consisting of distilled water. A GeneAmp PCR System 2700 thermal cycler (Applied Biosystems, Foster City, Calif.) was used for PCR amplification consisting of an initial denaturation at 94°C for 5 min; 30 cycles of denaturation at 94°C for 60 s, annealing at 54°C for 30 s, and extension at 72°C for 30 s; and a final extension at 72°C for 7 min. Five microliters of the PCR products was electrophoresed on 2% agarose gels, stained with ethidium bromide (0.25 μg/ml), and photographed under UV light.
FIG. 1.
Alignments of the sodA gene DNA sequences used in the present study and retrieved from the GenBank database (S. gallolyticus CIP105428T [GenBank accession no. AJ297183], S. bovis CIP102302 [GenBank accession no. Z95896], and S. equinus 102504T [GenBank accession no. Z95903]). Boldface letters indicate the positions of the primers in the sequences. The hyphens indicate the same bases as shown in S. gallolyticus CIP102302.
The PCR yielded an amplicon of 408 bp from all 23 S. gallolyticus strains, while other S. bovis-equinus strains did not (Table 1), suggesting that the assay is a useful molecular tool for the identification of S. gallolyticus. Further work with more strains of S. gallolyticus and other, related species is in progress in order to confirm the reliability of the PCR-based method as a diagnostic tool. With recently accumulating evidence of its taxonomic distinction and its etiological significance, we propose that the name S. gallolyticus be adopted for use by clinical microbiologists.
REFERENCES
- 1.Ballet, M., G. Gevigney, J. P. Gare, F. Delahaye, J. Etienne, and J. P. Delahaye. 1975. Infective endocarditis due to Streptococcus bovis. A report of 53 cases. Eur. Heart J. 16:1975-1980. [DOI] [PubMed] [Google Scholar]
- 2.Cohen, L., S. Dunbar, and J. E. Clarridge. 1997. Streptococcus bovis infection of the central nervous system: report of two cases and review. Clin. Infect. Dis. 25:819-823. [DOI] [PubMed] [Google Scholar]
- 3.Devriese, L. A., E. Uyttebroeck, D. Gevaert, P. Vandekerckhove, and K. Ceyssens. 1990. Streptococcus bovis infections in pigeons. Avian Pathol. 19:429-434. [DOI] [PubMed] [Google Scholar]
- 4.Duval, X., V. Papastamopoulos, P. Longuet, C. Benoit, C. Perronne, C. Leport, and J. L. Vilde. 2001. Definite Streptococcus bovis endocarditis: characteristics in 20 patients. Clin. Microbiol. Infect. 7:3-10. [DOI] [PubMed] [Google Scholar]
- 5.Ellmerich, S., M. Scholler, B. Duranton, F. Gosse, M. Galluser, J. P. Klein, and F. Raul. 2000. Promotion of intestinal carcinogenesis by Streptococcus bovis. Carcinogenesis 21:753-756. [DOI] [PubMed] [Google Scholar]
- 6.Facklam, R. 2002. What happened to the streptococci: overview of taxonomic and nomenclature changes. Clin. Microbiol. Rev. 15:613-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farrow, J. A. E., J. M. Kruze, B. A. Phillips, A. J. Bramley, and M. Collins. 1984. Taxonomic studies on Streptococcus bovis and Streptococcus equinus: description of Streptococcus alactolyticus sp. nov. and Streptococcus saccharolyticus sp. nov. Syst. Appl. Microbiol. 5:467-482. [Google Scholar]
- 8.Garvie, E. I., and A. J. Bramley. 1979. Streptococcus bovis—an approach to its classification and its importance as a cause of bovine mastitis. J. Appl. Bacteriol. 46:557-566. [DOI] [PubMed] [Google Scholar]
- 9.Grinberg, M., A. J. Mansur, D. O. Ferreira, G. Bellotti, and F. Pileggi. 1990. Endocarditis caused by Streptococcus bovis and colorectal neoplasms. Arq. Bras. Cardiol. 54:265-269. [PubMed] [Google Scholar]
- 10.Hønberg, P. Z., and E. Gutschik. 1987. Streptococcus bovis bacteraemia and its association with alimentary-tract neoplasm. Lancet ii:163-164. [DOI] [PubMed] [Google Scholar]
- 11.Klein, R. S., R. A. Recco, M. T. Catalano, S. C. Edberg, J. I. Casey, and N. H. Steigbigel. 1977. Association of Streptococcus bovis with carcinoma of the colon. N. Engl. J. Med. 297:800-802. [DOI] [PubMed] [Google Scholar]
- 12.Kupferwasser, I., H. Darius, A. M. Muller, S. Mohr-Kahaly, T. Westermeier, H. Oelert, R. Erbel, and J. Meyer. 1998. Clinical and morphological characteristics in Streptococcus bovis endocarditis: a comparison with other causative microorganisms in 177 cases. Heart 70:276-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marmur, L. J. 1961. A procedure for the isolation of deoxyribonucleic acid from microorganisms. J. Mol. Biol. 3:208-218. [Google Scholar]
- 14.Osawa, R., T. Fujisawa, and L. I. Sly. 1995. Streptococcus gallolyticus sp. nov.; gallate degrading organisms formerly assigned to Streptococcus bovis. Syst. Appl. Microbiol. 18:74-78. [Google Scholar]
- 15.Osawa, R., and L. I. Sly. 1992. Occurrence of tannin-protein complex degrading Streptococcus sp. in various animals. Syst. Appl. Microbiol. 15:144-147. [Google Scholar]
- 16.Osawa, R., and T. P. Walsh. 1993. Visual reading method for detection of bacterial tannase. Appl. Environ. Microbiol. 59:1251-1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osawa, R., and T. P. Walsh. 1995. Detection of bacterial gallate decarboxylation by visual color discrimination. J. Gen. Appl. Microbiol. 41:165-170. [Google Scholar]
- 18.Poyart, C., G. Quesne, and P. Trieu-Cuot. 2002. Taxonomic dissection of the Streptococcus bovis group by analysis of manganese-dependent superoxide dismutase gene (sodA) sequences: reclassification of ‘Streptococcus infantarius subsp. coli’ as Streptococcus lutetiensis sp. nov. and of Streptococcus bovis biotype II.2 as Streptococcus pasteurianus sp. nov. Int. J. Syst. Evol. Microbiol. 52:1247-1255. [DOI] [PubMed] [Google Scholar]