Abstract
We use a geographically weighted regression (GWR) approach to examine how the relationships between a set of predictors and prenatal care vary across the continental US. At its most fundamental, GWR is an exploratory technique that can facilitate the identification of areas with low prenatal care utilization and help better understand which predictors are associated with prenatal care at specific locations. Our work complements existing prenatal care research in providing an ecological, place-sensitive analysis. We found that the percent of the population who was uninsured was positively associated with the percent of women receiving late or no prenatal care in the global model. The GWR map not only confirmed, but also demonstrated the spatial varying association. Additionally, we found that the number of Ob-Gyn doctors per 100,000 females of childbearing age in a county was associated with the percentage of women receiving late or no prenatal care, and that a higher value of female disadvantage is associated with higher percentages of late or no prenatal care. GWR offers a more nuanced examination of prenatal care and provides empirical evidence in support of locally tailored health policy formation and program implementation, which may improve program effectiveness.
Keywords: Geographically weighted regression, Spatial non-stationarity, Local modeling, Prenatal care
Introduction
Receiving prenatal care on time is essential for a healthy mother and her baby. Although there has been some debate in the literature regarding the actual effectiveness of prenatal care on preventing poor birth outcomes (Kogan et al. 1998; Nguyen and Chongsuvivatwong 1997; Lauderdale et al. 2010), prenatal care can help identify risk factors associated with low birth weight and infant mortality, as well as other pregnancy complications that may occur at any time during the pregnancy (Laditka et al. 2005; Lauderdale et al. 2010). When women receive prenatal care, they are provided with educational information regarding infant delivery, care, and nutrition (Alexander et al. 1999; Butz et al. 1993). Even though receiving prenatal care on time can provide many benefits for mothers and their babies, not all women receive prenatal care during the recommended first trimester of pregnancy, and some women do not receive prenatal care at all. There is also great variation in prenatal care use across different areas of the country, which is not evident from the annual averages of prenatal care usage (Hemminki et al. 1987).
Increasing the proportion of pregnant women who receive early and adequate prenatal care to 90 percent of live births has been one of the objectives of Healthy People 2010 (Centers for Disease Control and Prevention and Health Resources and Services Administration 2010a). While the proportion of pregnant women who receive prenatal care during the first trimester of pregnancy has been increasing (76% in 1990 to 83% in 1998), vast racial/ethnic and socioeconomic differences in use of timely prenatal care remain (Alexander et al. 2002). For example, the percentage of women receiving prenatal care during the first trimester of pregnancy in 1990 and 1998 are 61 and 73 percent of Black women, 60 and 69 percent of American Indian/Alaskan Native women, and 60 and 74 percent of Hispanic women (Centers for Disease Control and Prevention and Health Resources and Services Administration 2010a, 2010b). Women who have the greatest risk of experiencing poor pregnancy outcomes due to their socioeconomic status are the same women who have had less improvements in their use of prenatal care (Alexander et al. 2002; Kogan et al. 1998). If we are to attain the Healthy People targets, we need a better understanding of the use of prenatal care in the US and identifying the factors associated with late or no prenatal care can help health policy makers determine how to best deliver to all mothers the prenatal care that they need.
This paper will adopt a spatial explicit approach to the study of prenatal care in the lower 48 states in and around the year 2000. Specifically, we use a geographically weighted regression (GWR) approach to identify the factors that are associated with county-level percentages of mothers who receive late or no prenatal care and examine how the relationships between a set of predictors and prenatal care vary across the US. That is, while a standard ordinary least squares (OLS) regression can identify associations between predictors and the outcome, and spatial econometric approaches permit the incorporation of spatial dependence into a model, both analytical approaches generate a single model result or ‘global’ fit. GWR is preferred over these other types of regression analyses, because it can identify whether or not the factors associated with late or no prenatal care vary ‘locally’ in different areas across the US. Moreover, understanding the local patterns and relationships can help the analyst better specify their global model. At its most fundamental, GWR is valuable because it facilitates the identification of areas most in need of increasing the percentage of women who use prenatal care services on time and which predictors are associated at specific locations. This more nuanced examination can be beneficial for county or state health policy planning and program implementation.
In this study we are interested in answering four research questions: (1) How does the percentage of the population without health insurance effect the percentage of women receiving late or no prenatal care? (2) Is the number of Ob-Gyn doctors in a county per 100,000 females of childbearing age associated with the percentage of mothers receiving late or no prenatal care? (3) How does the female socioeconomic status (later referred to as female disadvantage) of the county effect the percentage of pregnant women receiving late or no prenatal care? And, (4) Are the associations above constant or non-stationary across different parts of the US?
Literature Review
Socioeconomic status should play an important role in understanding why women do not receive prenatal care (Link and Phelan 1995). Many studies reported multiple risk factors for why mothers receive prenatal care after their first trimester of pregnancy or not at all, and many of these risk factors are interrelated. For example, women may have low levels of education, which leads them to obtain jobs without health insurance coverage or the flexibility to take time off for medical appointments and treatment. If women have low incomes or are unemployed they may not have access to an adequate means of transportation to get to their prenatal care appointments (Phillippi 2009). Women with higher levels of education and higher incomes were more likely to receive prenatal care during their first trimester of pregnancy (Ayoola et al. 2010; Sunil et al. 2010).
The survey used by Sunil and colleagues identified financial barriers as one of the main reasons why some women were receiving delayed prenatal care or no prenatal care at all, which includes not having money to pay for prenatal care and not having health insurance coverage (2010). Epstein et al. (2009) also identified living in poverty as one of the major barriers for not receiving prenatal care on time. Lack of insurance coverage during pregnancy was an important factor for why pregnant women were not receiving adequate prenatal care in the survey analyzed by Egerter et al. (2002). They found that women without health insurance coverage during their pregnancy were three times as likely as women with private health insurance coverage to begin prenatal care after the first trimester (Egerter et al. 2002).
Compared to mothers who live in urban areas, mothers from rural areas are more likely to not have health insurance coverage, be poor, less educated, and younger, which are all risk factors for not receiving prenatal care on time (Hulme and Blegen 1999; Larson and Correa-de-Araujo 2006). Moreover, fewer Ob-Gyn doctors in rural areas translates into greater transportation (both distance and time cost) barriers and greater difficulties accessing prenatal care for rural mothers (Davis et al. 2004; Braveman et al. 2000). For example, Miller and colleagues (1996) found that women who live in rural areas are more likely to receive prenatal care late or not at all, regardless of their maternal risk profile.
In addition to socioeconomic status, health insurance coverage, and availability of Ob-Gyn doctors, race/ethnicity has been identified as a crucial determinant of receiving prenatal care. Specifically, African American women are less likely to enter prenatal care during their first trimester of pregnancy, compared to their white counter parts (73% vs. 88%) (Mathews et al. 2000). Not only are African American women less likely to receive prenatal care compared to white women, but also they are more likely to start prenatal care in their third trimester of pregnancy (Daniels et al. 2006) and have pregnancy complications (LaVeist et al. 1995; Haas et al. 1993). Clarke and colleagues (1995), using the same data as Miller et al. (1996), found that African American women in rural areas are more likely to have late or no prenatal care compared to white and Hispanic women.
In a recent study based on the Pregnancy Risk Assessment Monitoring System (PRAMS) data, which is representative of resident women of childbearing age in 29 states, Ayoola and colleagues (2010) found that non-Hispanic white women were the most likely to receive prenatal care on time, followed by American Indian/Alaskan Native women, black women, and Hispanic women, with Asian women being the least likely to receive prenatal care on time. However, Johnson and colleagues (2010) report that American Indian/Alaskan Native mothers have the highest rates of late or no prenatal care use compared to women of all other races.
While the earlier studies have examined the associations of socioeconomic status, access to care, and race/ethnicity with receiving prenatal care, we identify two major shortcomings in the literature. First, while some studies use ecological-level data, to our knowledge, no studies adopt an explicitly spatial perspective in their analysis. We use GWR techniques to better understand place-specific conditions across the US. In doing so, we investigate the underexplored non-stationarity among variables of interest, which can provide nuanced local insights to health researchers and policy-makers. Second, our analysis focuses on insurance status and access to care, predictors that are often residual to measures of socioeconomic status. A GWR approach will be used to examine the following four hypotheses: (1) counties with a higher percent of uninsured persons tend to have higher percentages of women receiving late or no prenatal care; (2) the more Ob-Gyn doctors in a county per 100,000 females of childbearing age the lower the percentage of mothers receiving late or no prenatal care (3) increases in female disadvantage are associated with increases in the percentage of pregnant women receiving late or no prenatal care; and (4) these relationships are stronger in some counties in the US than others.
Data
The data was compiled from multiple sources for the counties in the continental US for which data was available in and around 2000 (N=3,106). The dependent variable, percent late or no prenatal care, is a three-year county average (1999–2001) and was extracted from the Office on Women’s Health Quick Health Data Online whose data comes from the National Center for Health Statistics (NCHS) National Vital Statistics System Detail Natality Files (NCHS 1999–2001). The variable is measured as the percentage of mothers who received prenatal care after the first trimester of their pregnancy or did not receive any prenatal care at all. The measure is based on the county of residence of the mother.
The percent uninsured is the percentage of the total population who do not have health insurance coverage, according to the US Census Bureau’s Small Area Health Insurance Estimates Program (US Census Bureau 2000a). Data on the number of Ob-Gyn doctors per county come from the Area Resource File (2000). The Ob-Gyn per 100,000 Females Ages 15–44 is the total number of Ob-Gyn doctors in a county, divided by the female population ages 15–44, and then multiplied by 100,000.
The percentage of females with less than a high school education (the percentage of females 25 years and over with less than a high school degree), the percentage of unemployed females (percentage of the female population 16 years and over who are in the labor force and are unemployed), and the percentage of females in poverty (percentage of females who are in poverty of the total female population for whom poverty status is determined) measures were highly correlated: female poverty and female educational attainment (0.72), female poverty and female unemployment (0.69), and female educational attainment and female unemployment (0.52); all three were significant at the p≤ 0.001 level. In order to avoid problems with multicollinearity, we used factor analysis to create a composite measure of female disadvantage using these three census variables.
All of the other measures used in this analysis come from the US Census Bureau’s Summary Files 1 and 3 (2000b). All of the race/ethnicity variables used in this analysis are the percentage of females ages 15–44 who chose one race/ethnicity and identify as black (percent black females 15–44), American Indian/Alaskan Native (AIAN females 15–44), and Asian (Asian females 15–44). The percent Hispanic females 15–44 reflects the percentage of the female population ages 15–44 who identify as Hispanic; this measure combines Hispanics reporting white race and black race in this category. The percent foreign born is the percentage of the total population who indicated that they were either a US citizen by naturalization or were not a citizen of the US. Persons who are born abroad of American parents are not considered foreign born.
Methods
The first three research questions are tested using both OLS regression and GWR. While OLS is a traditional approach, the underlying independent and homoskedastic assumptions associated with the use of spatial data may not hold and alternative estimation strategies may be required, including strategies based on local and global specifications (the former allowing us to examine spatial non-stationarity). That is, GWR extends OLS by taking spatial structure into account and can estimate local rather than global model parameters. The GWR model can be expressed as:
where yi is the percentage of mothers receiving late or no prenatal care for county i, (ui,vi) denotes the coordinates of the centroid of county i, β0i and βni represents the local estimated intercept and effect of variable n for county i, respectively. To calibrate this formula, the bi-square weighting kernel function is used (Brunsdon et al. 1998). The counties near to i have a stronger influence in the estimation of βni(ui,vi) than do those located farther from i. This model demonstrates a strength of GWR—that localized parameter estimates can be obtained for any location—which in turn, allows for the creation of a map showing the continuous surface of parameter values and an examination the spatial variability (non-stationarity) of these parameters (Fotheringham et al. 2002).
We will use the Akaike Information Criterion (AIC) (Akaike 1974) to compare OLS with GWR. The AIC comparison will reveal whether the spatial perspective significantly improves the model fit. Both OLS and GWR models are implemented in the software of GWR 3.0 (Fotheringham et al. 2002). To address the fourth research question and test for spatial non-stationarity, we adopt the Monte Carlo approach (Hope 1968; Fotheringham et al. 2002; Brunsdon et al. 1998). Specifically, for a given relationship between the percentage of mothers receiving late or no prenatal care and an independent variable n at a given location i, the GWR yields a parameter estimate of βni(ui,vi) Suppose there are m observations within the weighting kernel of i, we can have m values of the parameter estimate and thus calculate the standard deviation of the m parameter estimates, say Sk. GWR then randomly permutes the observed data and obtains the variance of each permutation for m-1 times. As a result, we are able to compare Sk with m-1 simulated variances. The total m variance values will yield a distribution and we can obtain the ranking of Sk in this distribution, r. The p-value for testing non-stationarity will be r/m. If the p-value is less than or equal to 0.05, we then have sufficient evidence to reject the null hypothesis and conclude that the effect of variable n on the percentage of mothers receiving late or no prenatal care varies spatially (Brunsdon et al. 1998).
Our analytic strategy is to present the descriptive statistics of the variables used in this analysis, followed by the OLS (global) modeling outputs. These results not only provide a basic understanding of the data, but also offer a basis for the comparison with the GWR results. The GWR results can best be summarized through the maps of the parameter estimates (Fotheringham et al. 2002) and the Monte Carlo tests. We provide maps of the local R-squared and for each of the independent variables with a statistically significant Monte Carlo test.
Results
Descriptive Statistics and Global Model Results
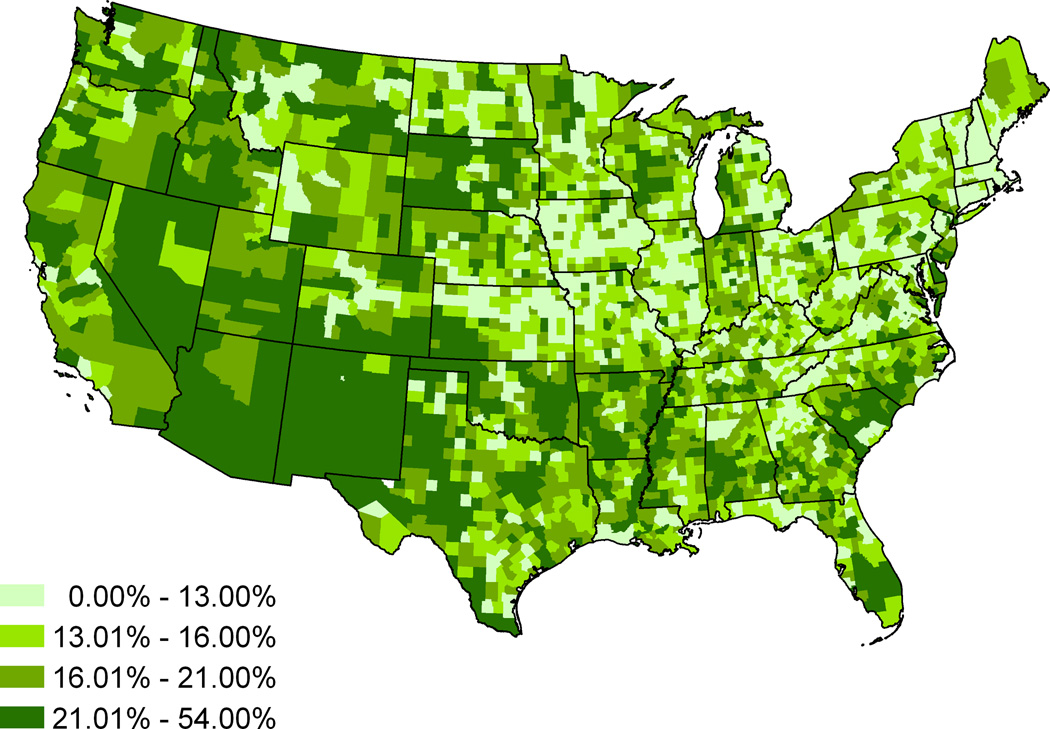
The descriptive statistics for the county-level percentage of mothers who receive late or no prenatal care and the other measures are provided in Table 1. On average, 17.39 percent of mothers in the US receive prenatal care late or do not receive prenatal care at all. The county-level percentages of mothers who receive late or no prenatal care range from zero percent to 54.05 percent. The county-level percentages of women receiving late or no prenatal care are mapped in Fig. 1. This map uses a quantile classification, with an equal number of counties in each of the four legend categories. The counties with the highest percentages of women receiving late or no prenatal care are located in the Mid- and Southwest, the black belt, and the Southeast.
Table 1.
Descriptive Statistics for the Percentage of Mothers Who Receive Late or No Prenatal Care (N=3106)
| Mean | Std. Dev. | Minimum | Maximum | |
|---|---|---|---|---|
| % Late or No Prenatal Care | 17.39 | 7.04 | 0.00 | 54.05 |
| % Uninsured | 14.75 | 4.99 | 3.80 | 38.00 |
| Female Disadvantage Composite | 0.00 | 1.00 | −2.06 | 5.75 |
| Ob-Gyn per 100,000 Females Ages 15–44 | 26.96 | 38.62 | 0.00 | 746.58 |
| % Black Females Ages 15–44 | 1.98 | 3.42 | 0.00 | 24.60 |
| % AIAN Females Ages 15–44 | 0.36 | 1.43 | 0.00 | 20.62 |
| % Asian Females Ages 15–44 | 0.21 | 0.42 | 0.00 | 7.33 |
| % Hispanic Females Ages 15–44 | 1.36 | 2.66 | 0.00 | 22.60 |
| % Foreign Born | 3.44 | 4.83 | 0.00 | 50.90 |
Fig. 1.
Map of the Percentages of Women Receiving Late or No Prenatal Care by County (1999–2001)
Because the female disadvantage measure was created using factor analysis, the mean is 0 and the standard deviation is 1. On average, 14.75 percent of the US population does not have health insurance coverage. There is an average of 26.96 Ob-Gyn doctors per 100,000 females ages 15–44. As for the racial/ethnic composition of US counties, on average, US counties have a 1.98 percent black, 0.36 percent American Indian/Alaskan native, 0.21 percent Asian, and 1.36 percent Hispanic female population ages 15–44. The total foreign born population in the US is 3.44 percent.
The OLS regression model results are provided in Table 2. These are the results of the global model. Every one percentage point increase in the population who is uninsured is associated with a 0.58 percent increase in mothers receiving late or no prenatal care. However, the female disadvantage composite measure was not significantly related to receiving prenatal care after the first trimester of pregnancy or not receiving prenatal care at al. As expected, the number of Ob-Gyn doctors that are available in counties is significantly associated with prenatal care. Specifically, with every one Ob-Gyn doctor increase per 100,000 females ages 15–44, the percentage of mothers receiving late or no prenatal care decreases by 0.01 percent.
Table 2.
OLS Regression Model Predicting the Percentage of Mothers Who Receive Late or No Prenatal Care (Global Regression Model) N=3106
| Estimate | Std. Error | Beta | VIF | |
|---|---|---|---|---|
| Intercept | 7.22*** | 0.41 | ||
| % Uninsured | 0.58*** | 0.03 | 0.44 | 3.00 |
| Female Disadvantage Composite | 0.00 | 0.00 | −0.03 | 2.57 |
| Ob-Gyn per 100,000 Females Ages 15–44 | −0.01* | 0.00 | −0.04 | 1.27 |
| % Black Females Ages 15–44 | 0.21*** | 0.04 | 0.11 | 1.65 |
| % AIAN Females Ages 15–44 | 0.89*** | 0.08 | 0.18 | 1.22 |
| % Asian Females Ages 15–44 | −2.26*** | 0.35 | −0.14 | 2.08 |
| % Hispanic Females Ages 15–44 | −0.03 | 0.07 | −0.01 | 3.13 |
| % Foreign Born | 0.30*** | 0.04 | 0.20 | 3.69 |
| Adjusted R-Square | 0.35 | |||
| Akaike Information Criterion | 19,617.91 |
Note:
p≤0.05;
p≤0.01;
p≤0.001
As for how the racial/ethnic and foreign born composition of a county is associated with the percentage of mothers receiving late or no prenatal care, the findings are consistent with our hypotheses. Increases in the percentage of black and American Indian/Alaskan native women ages 15–44 are associated with increases in the percentage of mothers receiving late or no prenatal care by 0.21 and 0.89 percentage points, respectively. As a county’s percentage of Asian females ages 15–44 increases by one percentage point, the percentage of mothers receiving late or no prenatal care decreases by 2.26 percentage points, while increases in the female Hispanic population of that same age group are not significantly associated with late or no prenatal care. With every one percentage point increase in the foreign born population, the percentage of mothers receiving late or no prenatal care increases by 0.30 percentage points.
We tested for multicollinearity utilizing the variance inflation factor (VIF), and the VIFs in Table 2 indicated that multicollinearity is not biasing the OLS estimations. The highest value is 3.69, which is well below the common cut-point of 10 (Menard 2002). This OLS model explains 35 percent of the total variance in the percentage of mothers who receive late or no prenatal care at the county level with the AIC 19,617.91. Though the OLS modeling offers some evidence for our hypotheses, it is still not clear if the spatial non-stationarity is a concern in our analysis. It is necessary to investigate the homoskedastic assumptions underlying the OLS with local modeling.
Local Model Results
The GWR 5-number parameter summary and Monte Carlo significance tests for spatial variability of parameter test results are displayed in Table 3. The Monte Carlo tests indicated that the associations between our independent and dependent variables are non-stationary across space, with the exception of the Ob-Gyn per 100,000 females ages 15–44 measure. Explicitly, the associations we found in OLS could not be generalized to anywhere in the US except for in the case of the association between Ob-Gyn per 100,000 females ages 15–44 and late or no prenatal care. In contrast to OLS, the GWR model explains 55 percent of the total variance among the dependent variable and has an AIC of 18,943.49. These diagnostics suggested that the GWR local model is statistically preferable to the OLS global model.
Table 3.
Geographically Weighted Regression 5-Number Parameter Summary Results and Monte Carlo Significance Test for Spatial Variability of Parameters (N=3106)
| Minimum | Lower Quartile |
Median | Upper Quartile |
Maximum | Monte Carlo Testing Status |
|
|---|---|---|---|---|---|---|
| Intercept | −17.32 | 2.95 | 7.66 | 13.43 | 25.72 | Non-Stationary*** |
| % Uninsured | −1.20 | 0.20 | 0.54 | 0.98 | 3.73 | Non-Stationary*** |
| Female Disadvantage Composite | −5.38 | −0.38 | 0.63 | 2.28 | 6.61 | Non-Stationary*** |
| Ob-Gyn per 100,000 Females Ages 15–44 | −0.08 | −0.02 | −0.01 | 0.01 | 0.10 | Stationary |
| % Black Females Ages 15–44 | −16.43 | −0.06 | 0.43 | 0.82 | 18.43 | Non-Stationary*** |
| % AIAN Females Ages 15–44 | −96.06 | −2.57 | −0.04 | 0.98 | 34.00 | Non-Stationary*** |
| % Asian Females Ages 15–44 | −30.35 | −6.38 | −2.86 | −0.07 | 23.58 | Non-Stationary*** |
| % Hispanic Females Ages 15–44 | −11.07 | −1.26 | 0.05 | 1.85 | 14.40 | Non-Stationary*** |
| % Foreign Born | −3.19 | −0.20 | 0.35 | 0.80 | 3.38 | Non-Stationary*** |
| Adjusted R-Square | 0.55 | |||||
| Akaike Information Criterion | 18,943.49 | |||||
Note:
p≤0.05;
p≤0.01;
p≤0.001
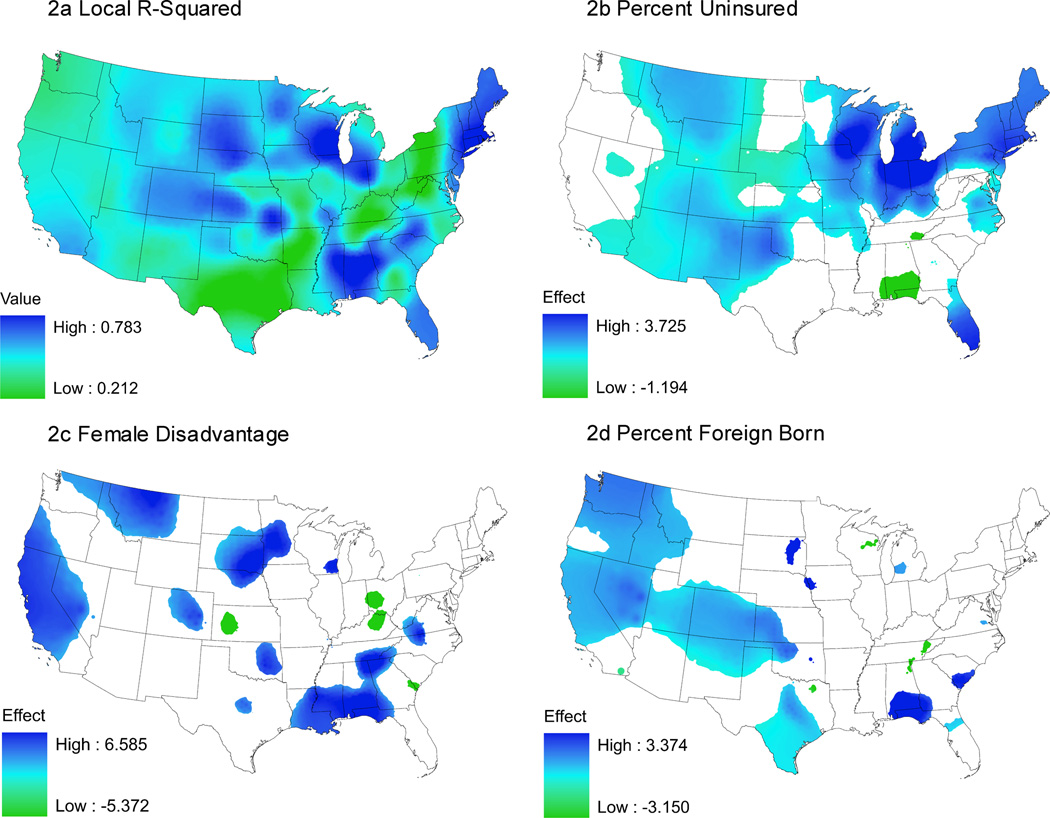
In Figures 2 and 3 we map the local R-squared and the significant local GWR parameter estimates for seven non-stationary variables in our model. Fig. 2 displays four maps, including the local R-square values across the contiguous US counties in Fig. 2a. As shown in the map, the total variance explained by the local model ranges from 21.2 to 78.3 percent. As you may recall, the total variance explained in the OLS model was 35 percent. This model fits the data well in many areas of the US, including the Northeast, black belt, the Midwest, and in Florida. Not surprising, these are many of the areas where significant associations were found and are areas that can be targeted to help increase the percentage of mothers who begin using prenatal care during the first trimester of pregnancy. This model does not fit the data as well in Texas and the Mid- and Northern Appalachia region. These are areas that may benefit from a model with additional covariates that may help explain why mothers receive prenatal care late or not at all, and could be tested in future research. Herein lies the value of the GWR approach, without the ability to map the local R-square, we would not know where our model could be improved with additional covariates.
Fig. 2.
Map of Local R-Square Estimates and GWR Estimates for Percent Uninsured, Female Disadvantage Composite, and Percent Foreign Born
Note: Significant Areas at +/− 1.96 level
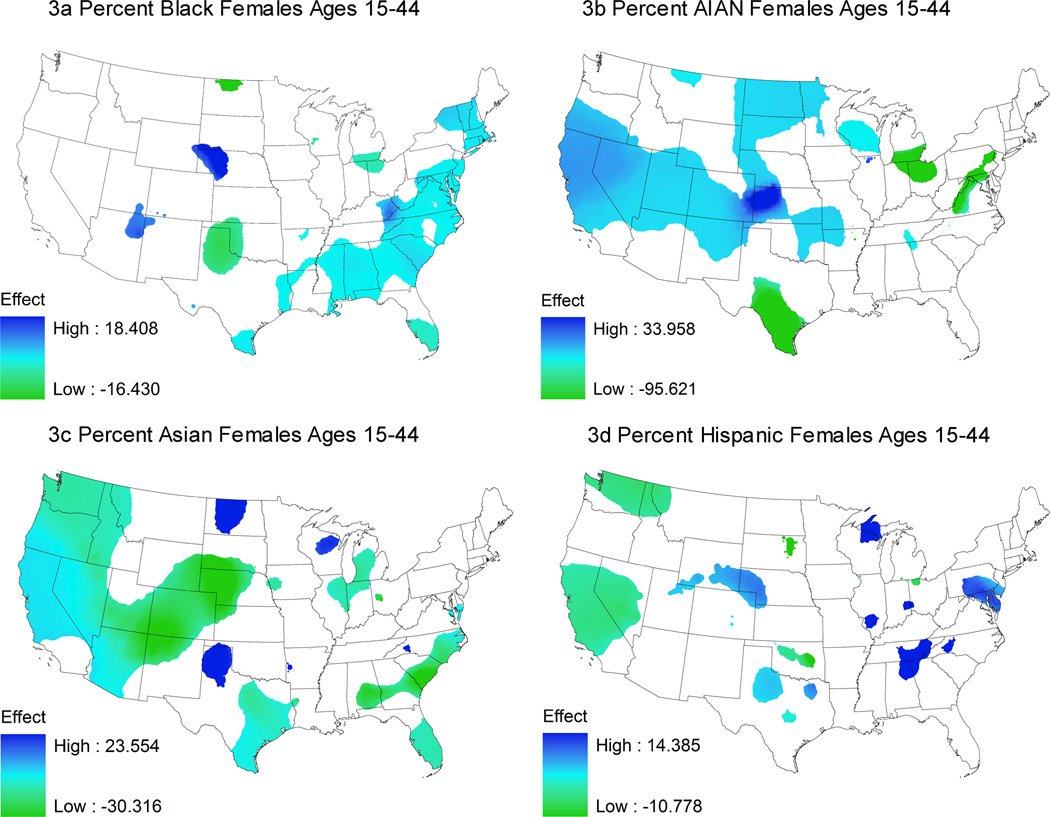
Fig. 3.
Map of GWR Estimates for Percent Black Females Ages 15–44, Percent American Indian/Alaskan Native Females Ages 15–44, Percent Asian Females Ages 15–44, and Percent Hispanic Females Ages 15–44
Note: Significant Areas at +/− 1.96 level
Fig. 2b displays the spatially varying association between percent uninsured and late or no prenatal care. Consistent with our hypothesis, we find that as the percentage uninsured increases in a county, the percentage of mothers receiving late or no prenatal care also increases in the majority of the significant areas. The significant associations for this measure cover a large portion of the US compared to all of the other measures in our model. That is, insurance status is a relevant variable in most places, though the strength of the association varied across the country, and we even found a negative effect in the Florida panhandle, Alabama, and Mississippi. The findings displayed in this map are very important—as they not only provide information on areas that could benefit from increases in timely prenatal care, but they also provide information on areas that can be targeted to make improvements on health insurance availability, which can in turn, improve the use of prenatal care among mothers.
Fig. 2c displays the effect of the female disadvantage composite measure on the percentage of mothers receiving late or no prenatal care. While no statistically significant effect was found in the OLS model, in many parts of the country, the more disadvantaged the female population, the higher the percentage of mothers receiving late or no prenatal care. Without the use of the GWR approach, we would not have been able to identify this effect, even though the literature supported this finding. Fig. 2d shows the effect of the percent foreign born on late or no prenatal care. As we found in the OLS model, as the percent foreign born increases in a county, the percentage of mothers receiving prenatal care after the first trimester of pregnancy or not at all also increases. This relationship is significant in many areas of the West and Midwest, including at least a partial area of all of the states along the US/Mexico border.
The effect of the race/ethnicity variables on late or no prenatal care are displayed in Fig. 3. We find that the association between the percentage of black females ages 15–44 and late or no prenatal care (Fig. 3a) is significant across the majority of the black belt area of the US (in this case positive association). In Fig. 3b, we find that there is a strong positive association between the percentage of American Indian/Alaskan Native females ages 15–44 and late or no prenatal care across many counties in the Midwest and West. This is not surprising, because these are areas where many of the American Indian reservations are located.
As was found in the OLS model, as the percentage of Asian females ages 15–44 increases in a county, the percentage of mothers receiving late or no prenatal care also increases (Fig. 3c). This strong relationship was found in many counties across the US including counties located in the southern coastal states, the Midwest, and the West. We do find a very strong positive association in North Dakota, Texas, and Wisconsin. These are areas that may benefit from some culturally sensitive prenatal care targeting efforts.
The varying association between percent Hispanic females ages 15–44 and late or no prenatal care is displayed in Fig. 3d. Here we find both a significant positive and negative association in the local model, but no significant relationship in the OLS (global) model. Again, this illustrates why local modeling is appropriate and potentially revealing, as without this approach, the varying relationship between percent Hispanic and late or no prenatal care would remain hidden. That is, the GWR map challenges the global model result by showing the local association between the percentage of Hispanic females ages 15–44 and receipt of prenatal care.
Discussion
The OLS and GWR results enable us to address our research questions. All four hypotheses were confirmed. Specifically, the percent of the population who was uninsured was positively associated with the percent of women receiving late or no prenatal care in the global model, and was consistent with the findings of Egerter et al. (2002). The GWR map helped confirm this association. While this association is almost ubiquitous across the US, it was not significant in many counties in the South, and switches sign in some cases.
In respect to our second and third hypotheses, we found that the number of Ob-Gyn doctors per 100,000 females of childbearing age in a county is associated with the percentage of women receiving late or no prenatal care, and that a higher value of female disadvantage is associated with higher percentages of late or no prenatal care. This latter finding is consistent with Sunil and colleagues who identified financial barriers as one of the main reasons why some women were receiving delayed prenatal care or no prenatal care at all and with Epstein and colleagues who found that living in poverty is one of the major barriers for not receiving prenatal care on time (Epstein et al. 2009; Sunil et al. 2010). Our fourth hypothesis, which predicted non-stationary associations, is confirmed for all of the independent variables with the exception of number of Ob-Gyns per 100,000 females of childbearing age. More explicitly, we might infer that the importance of the number of Ob-Gyn doctors in promoting adequate prenatal care is universal regardless of location.
Late or no prenatal care is detrimental to in-utero development, the health of the mother, the health of the infant once born, and potentially to later life outcomes too. Initiation of prenatal care in the first trimester of pregnancy is an important part of infant and maternal well-being (Epstein et al. 2009). We can ensure that all women have access to timely prenatal care by tailoring provision via policy, focusing attention to the multiple barriers identified in this paper. This can potentially reduce the risk of low birth weight babies and infant mortality.
One way that we may be able to improve prenatal care use in the US is to address many of these issues before women become pregnant, such as investing more in education and health insurance coverage. This way, women will have a better understanding of the importance of prenatal care and have the means to be able to obtain it. Other changes can be made to help reduce the racial/ethnic and socioeconomic disparities in early use of prenatal care. Efforts can be made to promote more culturally competent care (Brach and Fraser 2000) and improvements can be made to make prenatal care providers more accessible to women of low socioeconomic status by providing efficient transportation options and locating prenatal care providers in areas where services are lacking.
This study has some limitations. First, as an ecological analysis we cannot use our findings to make causal inferences about individual behaviors. Second, while the data used in this study are maintained by Federal agencies, and are of high quality, sampling error in the data collection designs may be a concern. Third, because of the racial/ethnic disparities in prenatal care utilization, it may have been more beneficial to examine the percentages of women receiving late or no prenatal care for specific racial/ethnic groups. However, the data on prenatal care utilization by race/ethnicity is not publicly available at the county-level, and even if the data were available, the sample would be too small in many counties.
Nevertheless, by using GWR, this study contributes to the prenatal care research in three ways. First, the local modeling has not only confirmed the findings in earlier research, but also addressed the recent concern in public health about both spatial inequality and the need for place-specific or place-sensitive forms of analysis (Goovaerts 2008; Young and Gotway 2010). That is, the parameter maps above suggest that some factors are more important than others in certain areas in the US, confirming our third hypotheses. Second, this study is ecological, based on county-level data. This type of analytical approach is important and can provide insights not necessarily apparent from individual-level data alone, and adds to the prenatal care literature, which has primarily been composed of individual-level analyses. Third, this study can help shed light on where to focus and where to tweak prenatal care policy by revealing the non-stationary associations. Explicitly, our findings offer an empirical basis for locally tailored policy formation, which may improve program effectiveness.
Contributor Information
Carla Shoff, Department of Agricultural Economics and Rural Sociology, and The Population Research Institute, The Pennsylvania State University, 13 Armsby Building, University Park, PA 16802 U.S.A., cms534@psu.edu.
Tse-Chuan Yang, Social Science Research Institute, The Pennsylvania State University, 803 Oswald Tower, University Park, PA 16802 U.S.A., tuy111@psu.edu.
Stephen A. Matthews, Associate Professor of Sociology, Anthropology and Demography, Population Research Institute, Social Science Research Institute, The Pennsylvania State University, 507 Oswald Tower, University Park, PA 16802 U.S.A., matthews@psu.edu
References
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- Alexander GR, Kogan MD, Himes JH. 1994–1996 US singleton birth weight percentiles for gestational age by race, Hispanic origin, and gender. Maternal and Child Health Journal. 1999;3:225–231. doi: 10.1023/a:1022381506823. [DOI] [PubMed] [Google Scholar]
- Alexander GR, Kogan MD, Nabukera S. Racial differences in prenatal care use in the United States: Are disparities decreasing? American Journal of Public Health. 2002;92(12):1970–1975. doi: 10.2105/ajph.92.12.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ARF. U.D.o.H.a.H. Services. Rockville, MD: Health Resources and Service Administration, Bureau of Health Professionals; 2000. Area Resource File. [Google Scholar]
- Ayoola AB, Nettleman MD, Stommel M, Canady RB. Time of pregnancy recognition and prenatal care use: A population-based study in the United States. Birth Issues in Perinatal Care. 2010;37(1):37–43. doi: 10.1111/j.1523-536X.2009.00376.x. [DOI] [PubMed] [Google Scholar]
- Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review. 2000;57(Supplemental 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, Marchi K, Egerter S, Pearl M, Neuhaus J. Barriers to timely prenatal care among women with insurance: the importance of pre-pregnancy factors. Obstetrics & Gynecology. 2000;95:874–880. doi: 10.1016/s0029-7844(00)00780-8. [DOI] [PubMed] [Google Scholar]
- Brunsdon C, Fotheringham AS, Charlton M. Geographically Weighted Regression: Modelling Spatial Non-Stationarity. Journal of the Royal Statistical Society: Series D (The Statistician) 1998;47(3):431–443. [Google Scholar]
- Butz M, Funkhouser A, Caleb L, Rosenstein BJ. Infant health utilization predicted by pattern of prenatal care. Pediatrics. 1993;92(1):50–54. [PubMed] [Google Scholar]
- Maternal Infant., editor. Centers for Disease Control and Prevention, & Health Resources and Services Administration. 16-6. Increase the proportion of pregnant women who receive early and adequate prenatal care. Child Health; 2010a. [Google Scholar]
- Maternal I, editor. Centers for Disease Control and Prevention, & Health Resources and Services Administration. Healthy People 2010. Child Health; 2010b. [Google Scholar]
- Clarke LL, Bono CA, Miller MK, Malone SC. Prenatal care use in nonmetropolitan and metropolitan America: racial/ethnic differences. Journal of Health Care for the Poor and Underserved. 1995;6(4):410–433. doi: 10.1353/hpu.2010.0002. [DOI] [PubMed] [Google Scholar]
- Daniels P, Noe GF, Mayberry R. Barriers to prenatal care among black women of low socioeconomic status. American Journal of Health Behavior. 2006;30:188–198. doi: 10.5555/ajhb.2006.30.2.188. [DOI] [PubMed] [Google Scholar]
- Davis K, Baksh L, Bloebaum L, Streeter N, Rolfs B. Barriers to adequate prenatal care in Utah. PRAMS Perspectives. 2004;1(1):1–8. [Google Scholar]
- Egerter S, Braveman P, Marchi K. Timing of insurance coverage and use of prenatal care among low-income women. American Journal of Public Health. 2002;92:423–427. doi: 10.2105/ajph.92.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein B, Grant T, Schiff M, Kasehagen L. Does rural residence affect access to prenatal care in Oregon? The Journal of Rural Health. 2009;25(2):150–157. doi: 10.1111/j.1748-0361.2009.00211.x. [DOI] [PubMed] [Google Scholar]
- Fotheringham AS, Brunsdon C, Charlton ME. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships. Chichester: Wiley; 2002. [Google Scholar]
- Goovaerts P. Geostatistical analysis of health data: State-of-the-art and perspectives. GeoENV VI-Geostatistics for Environmental Applications. 2008:3–22. [Google Scholar]
- Haas JS, Udvarhelyi S, Epstein AM. The effect of health coverage for uninsured pregnant women on maternal health and use of cesarean section. JAMA. 1993;270:61–64. [PubMed] [Google Scholar]
- Hemminki E, McNellis D, Hoffman HJ. Patterns of prenatal care in the United States. Journal of Public Health Policy. 1987 Autumn;:331–351. [PubMed] [Google Scholar]
- Hope ACA. A Simplified Monte Carlo Significance Test Procedure. Journal of the Royal Statistical Society: Series B (Methodological) 1968;30(3):582–598. [Google Scholar]
- Hulme PA, Blegen MA. Residential status and birth outcomes: Is the rural/urban distinction adequate? Public Health Nursing. 1999;16:176–181. doi: 10.1046/j.1525-1446.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- Johnson PJ, Call KT, Blewett LA. The importance of geographic data aggregation in assessing disparities in American Indian prenatal care. American Journal of Public Health. 2010;100(1):122–128. doi: 10.2105/AJPH.2008.148908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Martin JA, Alexander GR. The changing pattern of prenatal care utilization in the United States: 1981–1995, using different prenatal care indices. JAMA. 1998;279(20):1623–1628. doi: 10.1001/jama.279.20.1623. [DOI] [PubMed] [Google Scholar]
- Laditka SB, Laditka JN, Bennett KJ, Probst JC. Delivery complications associated with prenatal care access for Medicaid-insured mothers in rural and urban hospitals. The Journal of Rural Health. 2005;21(2):158–166. doi: 10.1111/j.1748-0361.2005.tb00076.x. [DOI] [PubMed] [Google Scholar]
- Larson S, Correa-de-Araujo R. Preventative health examinations: A comparison along the rural-urban continuum. Women’ Health Issues. 2006;16:80–88. doi: 10.1016/j.whi.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS, VanderWeele TJ, Siddique J, Lantos JD. Prenatal care utilization in excess of recommended levels: Trends from 1985 to 2004. Medical Care Research and Review. 2010;67(5):609–622. doi: 10.1177/1077558709351530. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Keith VM, Gutierrez ML. Black/white differences in prenatal care utilization: an assessment of predisposing and enabling factors. HRS: Health Service Research. 1995;30:43–58. [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior 35(Extra Issue: Forty Years of Medical Sociology: The State of the Art and Directions for the Future 1995) 1995:80–94. [PubMed] [Google Scholar]
- Mathews T, Curtain M, MacDorman M. Infant mortality statistics from the 1998 period linked birth/infant death data set. U.S. Department of Health and Human Services, CDC NCHS. National Vital Statistics Reports. 2000;48:1–9. [PubMed] [Google Scholar]
- Menard SW. Applied Logistic Regression Analysis. London: Sage; 2002. [Google Scholar]
- Miller MK, Clarke LL, Albrecht SL, Farmer FL. The interactive effects of race and ethnicity and mother's residence on the adequacy of prenatal care. The Journal of Rural Health. 1996;12:6–8. doi: 10.1111/j.1748-0361.1996.tb00768.x. [DOI] [PubMed] [Google Scholar]
- NCHS. U.S. Department of Health and Human Services. Washington, DC: The Office On Women's Health Quick Health Data Online; 1999–2001. National Vital Statistics System Detail Natality Files. [Google Scholar]
- Nguyen TH, Chongsuvivatwong V. Impact of prenatal care on perinatal mortality. SWHC. 1997;1:55–61. [PubMed] [Google Scholar]
- Phillippi JC. Women's perceptions of access to prenatal care in the United States: A literature review. Journal of Midwifery & Women's Health. 2009;54(3):219–223. doi: 10.1016/j.jmwh.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Sunil TS, Spears WD, Hook L, Castillo J, Torres C. Initiation of and barriers to prenatal care use among low-income women in San Antonio, Texas. Maternal and Child Health Journal. 2010;14:133–140. doi: 10.1007/s10995-008-0419-0. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. S. A. H. I. Estimates. Suitland, MD: 2000a. Health Insurance Coverage Status by Age for Counties and States. [Google Scholar]
- US Census Bureau. Summary File 3, Detailed Tables. Suitland, MD: GeoLytics; 2000b. [Google Scholar]
- Young LJ, Gotway CA. Using geostatistical methods in the analysis of public health data: the final frontier? GeoENV VII-Geostatistics for Environmental Applications. 2010;16:89–98. [Google Scholar]