Abstract
In the United States, more women than men seek health care services for symptoms of irritable bowel syndrome (IBS). A number of explanations are given for this gender difference including the higher rates of somatic non-gastrointestinal symptoms and increased psychological distress reported by women with IBS. However, these gender differences are found in studies that rely on retrospective recall with little attention to age or reproductive status. The purpose of the current analysis was to prospectively compare the frequency (days/month of moderate to severe based on a daily diary) of somatic, gastrointestinal (GI), and psychological distress symptoms, in menstruating women (N=89) and postmenopausal women (N=66) to men (N=32) with IBS. In addition, the correlation between daily symptoms and daily report of overall health was evaluated. Postmenopausal women reported significantly more GI pain/discomfort symptoms, especially bloating and abdominal distension, than men, however these differences are greatly attenuated when age is controlled for. Both postmenopausal and menstruating women reported significantly more somatic symptoms (especially joint pain and muscle pain) than men with IBS. The effect was stronger in postmenopausal women, whose somatic symptoms were also higher than menstruating women (p=.014). Fatigue and stress were higher in women than men but anxiety and depression were not. All three types of symptom were strongly correlated with self-rating of health, both across and within-person.
Conclusion
Gender-related differences in GI and somatic symptoms are apparent in persons with IBS, more strongly in postmenopausal women. The presence of somatic symptoms in postmenopausal women with IBS may challenge clinicians to find suitable therapeutic options.
Introduction
In the United States and other western industrialized countries, more women than men seek health care services for irritable bowel syndrome (IBS) (1,2). As compared to men with IBS, women with IBS are more likely to report additional functional gastrointestinal (GI) conditions including globus, dysphagia, bloating, constipation, fecal incontinence and pelvic floor dysfunction (3, 4). Somatic and non-gastrointestinal symptoms, collectively referred to as “extra-intestinal” are also more frequently reported by women with IBS (3, 4). Extra-intestinal symptoms include temporomandibular pain, dysmenorrhea, premenstrual distress syndrome, migraine headache, fibromyalgia, joint pain, muscle pain, interstitial cystitis, and chronic pelvic pain (5, 6). Women with IBS more frequently report affective or mood symptoms including anxiety and depression as compared to women without IBS (7).
Prior work by our group as well as others has shown that menstrual cycle variations exist in GI symptom reporting by women with IBS (8–10). Houghton and colleagues have shown that visceral sensitivity is heightened at menses as compared to other phases of the menstrual cycle (follicular, luteal, ovulatory) (11). In addition, psychological distress and somatic symptom reports also tend to increase prior to and during menses (12–14). Women with IBS who report the co-existence of menstrual cycle associated conditions, i.e., premenstrual distress syndrome (PMS), dysmenorrhea, prospectively report more severe GI and somatic symptoms particularly at the time of menstruation (9). For some women the menopause transition can be a time of heightened symptoms including those emanating from the GI tract, e.g., bloating (15,16). Together, these results suggest that when examining the pattern of symptom reporting between genders in a prospective fashion, menstrual cycle phase as well as menopausal status should be considered.
The main purpose of the current analysis was to compare prospectively reported GI, somatic and psychological distress symptoms in menstruating and postmenopausal women with IBS versus men with IBS. It was hypothesized that both categories of women would have higher severity of symptoms than men. An additional goal was to evaluate the strength of association between the three different types of symptoms and daily ratings of overall health, in the three subject groups. It was hypothesized more severe symptoms would be associated with worse rating of health.
Methods
Sample
This report presents a secondary analysis of baseline data from subjects in a randomized trial comparing a comprehensive self-management intervention to usual care in patients with IBS. Women and men with IBS, 18 to 70 years of age, were recruited through community advertisements. They were screened for eligibility over the telephone. To be enrolled patients had to have a medical diagnosis of IBS and meet Rome-II criteria for IBS (1). Men and women were excluded if they had a significant co-morbid condition (treated hypothyroidism, mild asthma or had a history of co-existing GI pathology (e.g., inflammatory bowel disease, celiac disease), surgery (e.g., bowel resection); or reproductive organ surgery (e.g., oophorectomy, prostatectomy, hysterectomy), or 2) were taking medications that significantly affect GI symptoms (e.g., narcotics, iron supplements, ACE inhibitors) or medications that would alter urinary cortisol or catecholamine levels. For this secondary analysis, women were classified as either menstruating or post menopausal and women who could not be clearly classified were excluded. Human subjects’ approval was obtained prior to recruitment.
Procedures
Participants were seen in person for their initial interview, gave informed consent, and completed questionnaires. They began a daily diary after this initial visit and continued for 28 days. The participants were financially compensated for their participation in the study.
Daily Symptom Diary
Subjects completed a symptom diary that contained 26 symptoms, which were rated every evening. Each symptom was rated on a scale from 0 (not present) to 4 (extreme). GI pain/discomfort symptoms in the daily diary included abdominal pain, abdominal distension, bloating, and intestinal gas. GI symptoms related to stool characteristics were diarrhea, constipation, and urgency. Psychological/ emotional items include anger, anxiety, panic feelings, depressed or blue, decreased desire to talk/move, stressed, fatigue/tiredness, hard to concentrate, and sleepiness during the day. Somatic symptoms were backache, headache, joint pain and muscle pain. A single item measured health status on each day, with the categories being ‘poor’, ‘fair’, ‘good’, ‘very good’, ‘excellent’. Health status is coded with ‘poor’ as 5 and ‘excellent’ as 1, so that positive correlation with symptoms means worse symptoms are associated with worse health. Women also indicated days which menstrual bleeding occurred. Only participants who completed the daily diary were included in the analyses.
Other variables
Demographic information included age, marital status, years of education, ethnic affiliation, occupation, body mass index, age when IBS pain began, and medication use. A retrospective measure of psychological distress was also used. The Brief Symptom Inventory (BSI) includes 53 items that measure psychological distress (17). Participants were asked to rate how much the symptom distressed or bothered them over the prior 7 days on a scale from not at all ‘0’ to extremely distressing ‘4’. For this study the Global Severity Index (GSI: mean of all 53 items) and the depression and anxiety subscales are reported. Acceptable indicators of validity and reliability have been described (17). The internal consistency of the GSI was α = .96 in this study.
Definition of subgroups
Menopausal status was determined based on self-reported answers on a health-history questionnaire and on the diary data. Women who reported that they had experienced menopause were classified as postmenopausal, while women who reported that they were still menstruating were classified as menstruating. Seven women were difficult to classify into one of these two categories because they had conflicting answers to these questions and others such as date of last menstrual period, and whether they had any menstrual bleeding during the 28 day calendar, or their answers indicated they may be perimenopausal. These few women were excluded from analysis in order to focus on the two well-defined groups. Based on a prior study demonstrating few differences in GI symptom reporting between women on oral contraceptives and those not (Heitkemper, Cain 2003 et al), women on oral contraceptives were included in the analyses. The 15 postmenopausal women taking hormone replacement therapy did not differ from the other postmenopausal women and hence are retained in the analyses.
For each subject, symptom severity is summarized as the percent of days on which the symptom is rated at least moderate (moderate, severe, very severe). In addition to reporting results for individual symptoms, some of the symptoms were combined into three summary scales, computed as the mean of the severity summaries of the individual symptoms in that scale: GI pain/discomfort scale (abdominal pain, abdominal distension, bloating, intestinal gas), somatic scale (backache, headache, joint pain, muscle pain), and anxiety/depression scale (anger, anxiety, panic feelings, decreased desire to talk or move, depressed/sad or blue). For menstruating women, diary data from the 4 days before and the 4 days after the first day of menses were not used in analyses since some symptoms are amplified in the days surrounding menses (8, 9). This decision was made so that any differences found between menstruating women and men could not be merely attributed to women having higher symptoms during menses.
Data Analysis
Descriptive statistics were compared across the three groups of subjects (men, menstruating women, postmenopausal women) using Analysis of Variance (ANOVA) and chi-square tests. Primary analyses compared the mean symptom severity across the three groups: men, menstruating women, and postmenopausal women. Analysis of variance was used to test for group differences. Contrasts within the ANOVA were used to compare men to each of the groups of women, and the two female groups to each other. Since the distribution of most outcome variables were skewed to the right, a square root transform was applied before testing group differences. Means of the untransformed variables are shown in the table of results, while transformed values are used for hypothesis testing and in scatter plots showing group differences. Since many variables had a non-normal distribution even after this transformation, the robust sandwich estimator (18) was used to get estimates of standard errors that are robust to non-normality and heteroscedasticity (non-uniformity of conditional variance). Since age may be a confounder, all analyses were repeated using analysis of covariance to control for age.
Correlations were computed between each of the three symptom scales and health status. This was done in two ways. First, the means across all diary days (for menstruating women this excluded 4 days prior to and 4 days following the onset of menses as described above) were taken for each subject, then the across-subject correlation was computed. Second, a within-subject correlation was computed for each subject, reflecting the extent to which health was worse on days with higher symptoms compared to days with lower symptoms. Then the distribution of these within-subject correlations were examined and compared across gender groups and across symptom scales using boxplots. ANOVA was used to test whether the strength of within-subject correlations differ by gender group, and paired t-tests are used to compare correlations with different symptom scales within each group.
Results
Sample
Thirty-two men and 140 women completed the study. As seen in Table 1, the sample was mostly white and well educated. There were some differences between groups in demographic characteristics. As expected, age differs greatly between pre and postmenopausal women, with the mean age for men being in between. Age when IBS pain began is fairly similar in men and postmenopausal women but much younger in menstruating women, while years since pain began is similar in men and menstruating women and much longer in postmenopausal women. If the two groups of women are combined into one, their mean age (41.8) is very similar to men, while their mean age at first pain is somewhat lower (25.6, p=.069) and their mean years since pain began is somewhat longer (16.4, p=.042) than men. Interestingly, there are no significant gender differences in psychological distress as measured on the BSI. This is contrary to expectations, since values reported here are raw scores, not t-scores, and in general, women have higher raw scores than men (17).
Table 1.
Comparisons of Demographic and IBS Characteristics of Men, Menstruating Women, and Postmenopausal Women with Irritable Bowel Syndrome
| Men (n=31) | Menstruating Women (n=89) | Postmenopausal Women (n=66) | p-valuea | |
|---|---|---|---|---|
| N (%) | ||||
| Married/partnered | 19 (59%) | 30 (34%) | 33 (50%) | .020 |
| Work full time | 19 (59%) | 45 (51%) | 23 (35%) | .042 |
| Education – college grad | 25 (78%) | 55 (62%) | 43 (65%) | NS |
| Professional job | 12 (41%) | 37 (43%) | 29 (46%) | NS |
| Race white | 25 (89%) | 75 (88%) | 58 (84%) | NS |
| Family income > $40,000 | 18 (56%) | 47 (53%) | 44 (67%) | NS |
| Predominant bowel pattern | .171 | |||
| Constipation | 4 (12%) | 17 (19%) | 20 (30%) | |
| Diarrhea | 20 (62%) | 44 (49%) | 30 (46%) | |
| Alternating | 7 (22%) | 23 (26%) | 11 (17%) | |
| Mean (SD) | ||||
| Age | 41.2 (13.8) | 32.9 (9.3) | 58.4 (5.3) | <.001 |
| Age IBS pain began | 30.5 (13.6) | 21.1 (9.6) | 33.0 (15.5) | <.001 |
| Years since IBS pain began | 11.2 (8.8) | 11.9 (9.5) | 25.4 (15.5) | <.001 |
| BMI | 25.5 (4.6) | 24.7 (6.5) | 26.4 (6.8) | NS |
| BSI – GSI | 0.44 (0.51) | 0.46 (0.37) | 0.49 (0.29) | NS |
| BSI – depression | 0.44 (0.51) | 0.48 (0.57) | 0.43 (0.41) | NS |
| BSI – anxiety | 0.62 (0.75) | 0.56 (0.52) | 0.63 (0.51) | NS |
| NS = not significant, p>.20 | ||||
p-values compare the three groups, based on Chi-square test or ANOVA.
Diary Symptoms
Table 2 shows symptom severity for menstruating women and postmenopausal women, compared to men. Symptom severity is summarized as the percent of days with symptom severity at least moderate. Postmenopausal women have very high levels of symptoms relating to gas and bloating (abdominal distension, bloating, intestinal gas), all of which are moderate or worse on more that 40% of days, and are more severe than in men. In contrast these symptoms are similar in menstruating women and in men. Abdominal pain is also quite prevalent in menstruating and postmenopausal women (38% and 37% of days moderate or worse, respectively), not quite significantly worse than men. These differences are reflected in the composite scale measuring GI pain/discomfort, which is highly significantly worse in postmenopausal women. The results for the symptoms of constipation, diarrhea, and urgency are consistent with the fact that men with IBS generally have more diarrhea and less constipation than women with IBS.
Table 2.
Comparison of Percent of Days with Reports of Moderate to Severe GI, Psychological Distress, and Somatic Symptoms in Men and Women with Irritable Bowel Syndrome
| Men (n=32) | Menstruating women (n=89) | Postmenopausal women (n=66) | p-valuec | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p-valuesa | Mean (SD) | p-valuesb | ||
| GI Symptoms | ||||||
| Abdominal paind | 28.7(22.0) | 37.7(26.1) | .095 / .135 | 37.5(25.6) | .134 / .125 | NS |
| Abdominal distensiond | 20.8(25.5) | 26.0(29.5) | NS / .134 | 42.4(35.0) | .001 / .063 | .003 |
| Bloating d | 27.2(28.6) | 26.0(27.6) | NS / NS | 45.1(33.0) | .005 / .108 | <.001 |
| Intestinal gasd | 37.5(29.0) | 31.6(28.5) | .179 / NS | 51.1(30.1) | .061 / NS | <.001 |
| Constipation | 15.2(20.7) | 22.9(22.7) | .026 / .035 | 21.8(26.2) | .104 / .161 | NS |
| Diarrhea | 17.7(20.5) | 14.2(20.3) | NS / NS | 13.2(17.7) | .127 / NS | NS |
| Passing gas | 41.1(31.7) | 37.2(29.1) | NS / NS | 51.8(30.1) | .100 / NS | .003 |
| Urgency | 25.3(28.1) | 20.2(22.9) | NS / NS | 16.4(20.3) | .064 / .141 | NS |
| Heartburn | 10.2(20.2) | 6.6(14.3) | NS / NS | 10.0(17.9) | NS / NS | .098 |
| Nausea | 5.7(14.1) | 8.9(13.7) | .048 / NS | 6.6(13.9) | NS / .037 | .116 |
| Stomach pain | 20.5(23.8) | 23.6(26.6) | NS / NS | 21.8(23.6) | NS / NS | NS |
| Scale: GI pain/discomfort | 28.5(21.8) | 30.3(23.7) | NS / NS | 44.0(26.9) | .006 / .121 | .002 |
| Somatic symptoms | ||||||
| Backachee | 7.6(15.9) | 16.4(24.7) | .023 / .063 | 19.1(26.1) | .005 / .005 | NS |
| Headachee | 7.6(14.5) | 13.8(19.6) | .020 / .090 | 12.6(17.8) | .023 / .002 | NS |
| Joint paine | 5.2(12.6) | 11.3(22.6) | .061 / .014 | 28.4(31.6) | <.001 / .001 | <.001 |
| Muscle paine | 5.2(9.1) | 14.8(24.5) | .011 / .011 | 26.7(30.0) | <.001 / <.001 | .003 |
| Scale: somatic | 6.4(8.9) | 14.1(17.8) | .001 / .004 | 21.7(22.0) | <.001 / <.001 | .014 |
| Psychological and Emotional | ||||||
| Angerf | 5.5(9.5) | 7.5(13.4) | NS / NS | 6.6(11.0) | NS / NS | NS |
| Anxietyf | 15.8(24.0) | 18.0(21.6) | NS / NS | 28.8(19.4) | .114 / .187 | NS |
| Panic feelingsf | 7.8(21.1) | 6.3(15.1) | NS / NS | 3.5(7.4) | NS / NS | NS |
| Decreased desire to talk/movef | 8.8(12.6) | 12.34(17.0) | NS / NS | 8.5(11.9) | NS / .063 | .127 |
| Depressed or bluef | 7.3(15.6) | 11.1(17.9) | .167 / NS | 9.6(16.3) | NS / .061 | NS |
| Fatigue/tiredness | 24.0(21.2) | 33.4(25.1) | .070 / .120 | 39.0(27.2) | .004 / .007 | .155 |
| Hard to concentrate | 8.4(14.4) | 14.7(21.8) | .060 / .089 | 13.8(19.7) | .068 / .115 | NS |
| Sleepiness during day | 20.5(19.4) | 25.4(24.3) | NS / NS | 26.8(25.7) | NS / NS | NS |
| Stressed | 19.0(25.7) | 25.5(25.1) | .034 / .102 | 25.1(23.6) | .035 / .012 | NS |
| Scale: anxiety/depression | 9.0(12.3) | 11.1(14.2) | NS / NS | 9.4(10.3) | NS / .174 | NS |
NS = p>0.20
p-values are comparing menstruating women to men, by regression with robust standard error estimates, and the square root transform applied to normalize the distributions. The first p-value is unadjusted, the second is controlled for age.
p-values are comparing postmenopausal women to men, by regression with robust standard error estimates, and the square root transform applied to normalize the distributions. The first p-value is unadjusted, the second is controlled for age.
p-value are comparing postmenopausal women to menstruating women, not controlling for age. Controlling for age makes all p-values non-significant
items included in the pain/discomfort scale
items included in the anxiety/depression scale
items included in the somatic scale
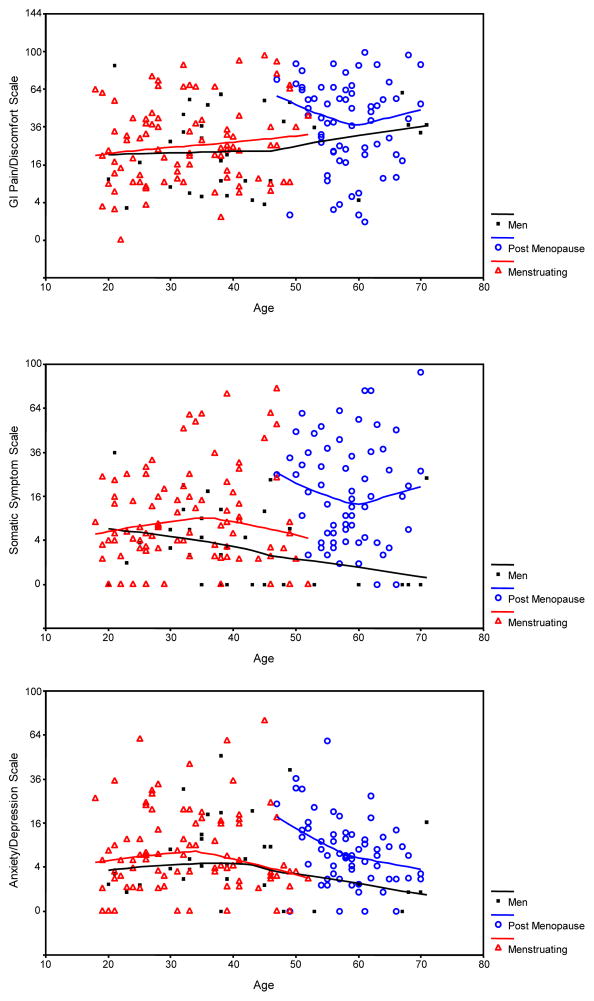
As seen in Figure 1a, the GI pain/discomfort scale increases with age. When age is controlled for, differences in GI pain/discomfort become nonsignificant (p=.121).
Figure 1.
Scatterplot of percent of days (n=28) when symptom scales were rated as moderate to severe in men and women with irritable bowel syndrome. A) GI pain/discomfort, B) Somatic symptom scale, C) Anxiety/depression scale.
Both female groups have higher somatic symptoms than men, as seen in Table 2 and Figure 1b. The mean percent of days with moderate/severe symptoms is between 5% and 8% for the four somatic symptoms in men, and as seen in Figure 1b about a third of men have zero days with moderate/severe somatic symptoms. In contrast, in women these means range from 11% to 28%. It is especially striking that postmenopausal women have very high levels of joint and muscle pain, over 25% of days with moderate or severe symptoms. Gender differences in the somatic scale variable persist even in the analyses controlling for age.
There are no significant gender differences in the anxiety/depression scale, as seen in Table 2 and Figure 1c. Postmeopausal women are significantly higher than men on the symptoms of fatigue/tiredness and stressed. It should be noted that levels of fatigue are very high among women, with fatigue being moderate or worse on 33% and 39% of days in menstruating and postmenopausal women respectively.
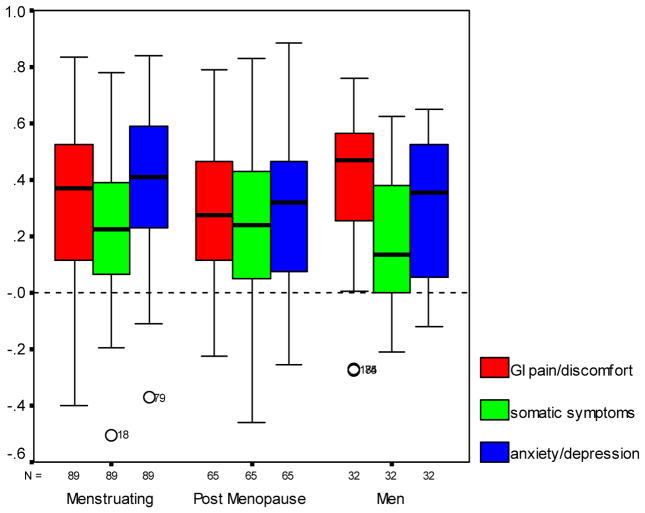
Correlation of Symptom Scores with Self Rating of Health
Across-subject correlations of health status with the GI pain/discomfort scale were .35, .39, and .39 for menstruating women, postmenopausal women and men respectively. Correlations of health status with the somatic scale were .40, .53, and .51 and with the anxiety/depression scale were .44, .31, and .47 for the three groups respectively. Thus for all three subject groups, persons with worse symptoms have poorer quality of life, and this is true for all three symptom scales.
The boxplots in Figure 2 show the distribution of within-subject correlations between daily health status and daily symptom scores. Note that for all three symptom scores, the vast majority of subjects have positive correlations between health status and symptoms scores. This means that for almost all subjects, their self-rating of health status is worse on days with worse symptoms. This is true for all three symptom scores: GI pain/discomfort, somatic, and anxiety/depression. Among both menstruating women and men, the within-subject correlations are significantly weaker (p<.05) for the somatic symptom scale than for both the GI pain/discomfort scale and the anxiety/depression scale. There are no statistically significant differences among the three groups in the degree to which each symptom scale influenced daily reports of health status.
Figure 2.
Boxplots showing distribution of within-person correlations between symptom scales and daily health rating.
Discussion
Using prospective data collection we have shown that somatic symptoms have the greatest differences in overall symptom reporting between men and women with IBS. This gender-related difference is most pronounced when postmenopausal women are compared to men. More specifically the number of days with moderate to severe muscle and joint pain was 5 times greater in postmenopausal women as compared to men while days with moderate to severe backache was higher in men. Gender differences were much weaker for GI symptoms and all psychological/emotional symptoms except for fatigue and stress, especially in the analysis which controlled for age.
In general, pain or discomfort symptoms are more frequently reported by women as compared to men (19). The explanations given for these gender-related differences are multiple and include biologic factors (e.g., sex hormones), acquired risks (e.g., occupation), psychosocial characteristics of the pain symptoms, and health care seeking behavior (19–22). In addition, this gender effect varies across the lifespan for conditions such as fibromyalgia which is more common in older as compared to younger women. In studies of healthy men and women, gender related differences in visceral pain sensitivity are inconsistently found (3). In addition, data from IBS patients are also mixed. Two studies comparing rectal sensitivity in men and women with IBS (23, 24) found lower thresholds in women with IBS while another found no differences between men and women with IBS (25).
Little is known about the trajectory of IBS symptoms across the natural lifespan of men and women. In analyzing the United Kingdom (UK) General Practice Research Database, Garcia Rodríguez et al. (26) found that while there was a much higher incidence rate of IBS diagnoses in women than men in young adulthood, there was a steady decline with age among women converging with that in men by the 7th decade of life (26). In contrast, the incidence in men remained relatively stable between the ages of 20–69.
In the current study seven women were excluded from the analysis due to history and diary data that were either inconsistent or suggestive of perimenopausal transition. Women experiencing the menopause transition often report a variety of symptoms including depression, vasomotor symptoms, (i.e., hot flashes and night sweats) and sleep disruption. Longitudinal as well as cross sectional studies have demonstrated that women transitioning to menopause report greater bodily pain and discomfort as well as limitations due to their symptoms and poorer perceived health (for a review see 15). Figure 1 shows somewhat elevated symptoms of abdominal discomfort and anxiety/depression among the youngest of the postmenopausal women, perhaps reflecting women who are early postmenopause. Unfortunately, in this secondary data analysis the date of last menstrual period was often missing and not considered reliable so this conjecture could not be checked directly. However such a pattern would be consistent with the model proposed by Matthew and Bromberger (15) in which self report of health quality decreases during the perimenopause phase but returns closer to premenopausal levels during the later postmenopausal years. The study of the perimenopause phase in terms of a condition such as IBS would require careful staging using criteria such as that established by the Staging of Reproductive Aging Workshop (STRAW) (27) report as well as attention to circulating reproductive hormone levels.
The increase in bloating and intestinal symptoms at menopause is not unique to women with IBS. Triadafilopoulos (16) in a prospective study of postmenopausal and menstruating women without a diagnosis of IBS found that the presence of IBS-type complaints (e.g., abdominal pain) peaked between the ages of 40–49. The increase in GI symptoms after menopause in women with IBS may be part of a symptom complex that includes vasomotor instability, sleep disruption, bodily pain, and mood alterations. The question is whether a single physiological factor or trigger linked to the menopause transition accounts for these diverse symptom patterns. To date, GI symptoms during the perimenopause transition have remained unexplored. A few studies have examined GI transit in postmenopausal women (28, 29) and a recent clinical study showed that administration of micronized progesterone improved symptoms of constipation in postmenopausal women (30). These results are intriguing and suggest that the cessation of hormone cycling may be involved. Studies that incorporate measures of multiple symptom complexes as well as biological markers are needed.
The presence of somatic symptoms has been linked to decreased quality of life (QOL) in patients with IBS and greater GI health care use costs once diagnosed. Spiegel (31) reviewing charts from 770 IBS patients, found that extra-intestinal symptoms such as fatigue, anxiety, and insomnia were related to lower health-related QOL. However, Lembo (32) found that the extraintestinal symptoms reported by IBS patients were less frequently identified as the ‘worst’ symptoms when compared to GI symptoms. In the current study mean rating of health was significantly correlated with mean symptom scores, across-person. Whether these co-existing conditions share a similar pathophysiological basis remains to be determined. Whitehead (5) using data from 3,153 participants in a health maintenance organization suggested that comorbidity in patients with IBS is due to greater amplification of symptom reporting and care provider consultation rather than a shared pathophysiology.
Correlating symptoms with daily health status showed that GI pain/discomfort, somatic symptoms and psychological distress were all strongly associated with worse health status. Almost all women reported worse health status on days with more severe symptoms. The strength of these within-person associations with health status was somewhat stronger for GI pain/discomfort and anxiety/depression than for the somatic symptom scale. In a prior analysis with data from only menstruating women, we found that abdominal pain severity had the strongest correlation with daily impact and health related QOL (33). The current study extends those findings by illustrating that GI symptoms along with psychological distress and somatic symptoms are strongly associated with health status. The increase in somatic symptoms with aging in women, especially muscle and joint pain, and their overall impact on health perception is not surprising.
While women in the current study reported more fatigue and stress than men, the anxiety/depression scale showed no gender differences. While the prevalence of depression and anxiety are known to be higher in women in the general population (34), there is less agreement in patients with IBS. Kim et al found no gender differences in a population of Korean adults with IBS (25). Studies that recruit from tertiary care clinics may represent a population with higher psychiatric co-morbidity than those samples recruited from the community.
The study of gender differences in IBS is challenged by the under-representation of men making comparisons based on gender difficult (3). A limitation in the current study was the small number of men with IBS, particularly older men. However, similar to a large epidemiological survey of the Canadian population, men in the current study reported higher levels of back pain as compared to women (34).
In summary, we have seen that among people with IBS, the biggest gender differences are in somatic pain symptoms. Both menstruating and postmenopausal women have more severe somatic symptoms than men, with joint and muscle pain being very prevalent among postmenopausal women. Curiously, psychological and emotional symptoms showed few gender differences, the exceptions being fatigue and stress. GI symptoms were higher in postmenopausal women than in men, but these differences mainly disappear when controlled for age . All three types of symptoms are related to self-rated health on a daily basis. It thus appears that extra-intestinal symptoms are important to people with IBS, and most especially in postmenopausal women
Acknowledgments
Supported by a grants NIH NR01094, P30 NR04001
Abbreviations
- IBS
irritable bowel syndrome
- PMS
premenstrual distress
- HRT
hormone replacement therapy
References
- 1.Drossman D, Corazziari E, Thompson W, et al. Rome II: The functional gastrointestinal disorders. 2. McLean, Degnon Associates; 2000. [Google Scholar]
- 2.Chial HJ, Camilleri M. Gender differences in irritable bowel syndrome. J Gend Specif Med. 2002;5:37–45. [PubMed] [Google Scholar]
- 3.Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterol. 2006;130:1435–46. doi: 10.1053/j.gastro.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 4.Lee OY, Mayer EA, Schmulson M, et al. Gender-related differences in IBS symptoms. Am J Gastroenterol. 2001;96:2184–93. doi: 10.1111/j.1572-0241.2001.03961.x. [DOI] [PubMed] [Google Scholar]
- 5.Whitehead WE, Palsson OS, Levy RR, et al. Comorbidity in irritable bowel syndrome. Am J Gastroenterol. 2007;102:2767–76. doi: 10.1111/j.1572-0241.2007.01540.x. [DOI] [PubMed] [Google Scholar]
- 6.Chang L, Heitkemper MM. Gender differences in irritable bowel syndrome. Gastroenterol. 2002;123:1686–1701. doi: 10.1053/gast.2002.36603. [DOI] [PubMed] [Google Scholar]
- 7.Cohen H, Jotkowitz A, Buskila D, et al. Post-traumatic stress disorder and other co-morbidities in a sample population of patients with irritable bowel syndrome. Eur J Intern Med. 2006;17:567–571. doi: 10.1016/j.ejim.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Heitkemper M, Cain K, Jarrett ME, et al. Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am J of Gastroenterol. 2003;98:420–30. doi: 10.1111/j.1572-0241.2003.07233.x. [DOI] [PubMed] [Google Scholar]
- 9.Altman G, Cain K, Motzer S, Jarrett M, Heitkemper M. Increased symptoms in female IBS patients with dysmenorrhea and PMS. Gastroenterol Nrsg. 2006;29:4–11. doi: 10.1097/00001610-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Heitkemper M, et al. Daily GI symptoms in women with & without a diagnosis of IBS. Dig Dis Sci. 1995;40:1511. doi: 10.1007/BF02285200. [DOI] [PubMed] [Google Scholar]
- 11.Houghton LA, Lea R, Jackson N, et al. The menstrual cycle affects rectal sensitivity in patients with irritable bowel syndrome but not healthy volunteers. Gut. 2002;50:471–4. doi: 10.1136/gut.50.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laessle RG, Tuschi RJ, Schweiger LI, et al. Mood changes and physical complaints during the normal menstrual cycle in healthy young women. Psychoneuroendocrin. 1990;15:131–8. doi: 10.1016/0306-4530(90)90021-z. [DOI] [PubMed] [Google Scholar]
- 13.LeResche L, Manci L, Sherman JJ, et al. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain. 2003;106:253–61. doi: 10.1016/j.pain.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Rubinow DR, Schmidt PJ. Gonadal steroid regulation of mood: the lessons of premenstrual syndrome. Front Neuroendocrinol. 2006;27:210–6. doi: 10.1016/j.yfrne.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Matthews KA, Bromberger JT. Does the menopausal transition affect health-related quality of life? Am J Med. 2005;19(118 Suppl 12B):25–36. doi: 10.1016/j.amjmed.2005.09.032. [DOI] [PubMed] [Google Scholar]
- 16.Triadafilopoulos G, Finlayson M, Grellet C. Bowel dysfunction in postmenopausal women. Women Health. 1998;27:55–66. doi: 10.1300/J013v27n04_04. [DOI] [PubMed] [Google Scholar]
- 17.Derogatis L. BSI: Brief Symptom Inventory; Administration, Scoring and Procedures Manual. 4. Minneapolis: National Computer Systems; 1993. [Google Scholar]
- 18.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–830. [Google Scholar]
- 19.Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med. 1998;60:150–5. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Bertakis KD, Azari R. Patient gender and physician practice style. J Womens Health (Larchmt) 2007;16:859–68. doi: 10.1089/jwh.2006.0170. [DOI] [PubMed] [Google Scholar]
- 21.Bingefors K, Isacson D. Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain--a gender perspective. Eur J Pain. 2004;8:435–50. doi: 10.1016/j.ejpain.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Gran JT. The epidemiology of chronic generalized musculoskeletal pain. Best Pract Res Clin Rheumatol. 2003;17:547–61. doi: 10.1016/s1521-6942(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 23.Chang L, Mayer EA, Labus J, et al. Effect of sex on perception of rectosigmoid stimuli in irritable bowel syndrome. Am J Physiol Regul Integr Comp Physiol. 2006;291:277–284. doi: 10.1152/ajpregu.00729.2005. [DOI] [PubMed] [Google Scholar]
- 24.Ragnarsson G, Hallbook O, Bodemar G. Abdominal symptoms are not related to anorectal function in the irritable bowel syndrome. Scand J Gastroenterol. 1999;34:250–258. doi: 10.1080/00365529950173645. [DOI] [PubMed] [Google Scholar]
- 25.Kim HS, Rhee PL, Park J, et al. Gender-related differences in visceral perception in health and irritable bowel syndrome. J Gastroenterol Hepatol. 2006;21:468–73. doi: 10.1111/j.1440-1746.2005.04060.x. [DOI] [PubMed] [Google Scholar]
- 26.Garcia Rodriguez LA, Ruigomez A, Wallander MA, et al. Detection of colorectal tumor and inflammatory bowel disease during follow-up of patients with initial diagnosis of irritable bowel syndrome. Scand J Gastroenterol. 2000;35:306–311. doi: 10.1080/003655200750024191. [DOI] [PubMed] [Google Scholar]
- 27.Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N. Executive summary: Stages of reproductive aging workshop (STRAW) Climacteric. 2001;4:267–72. [PubMed] [Google Scholar]
- 28.Hutson WR, Roehrkasse RL, Wald A. Influence of gender and menopause on gastric emptying and motility. Gastroenterol. 1989;96:11–17. doi: 10.1016/0016-5085(89)90758-0. [DOI] [PubMed] [Google Scholar]
- 29.Wald A, Van Thiel DH, Hoechstetter L, et al. Gastrointestinal transit: the effect of the menstrual cycle. Gastroenterol. 1981;80:1497–500. [PubMed] [Google Scholar]
- 30.Gonenne J, Esfandyari T, Camilleri M, et al. Effect of female sex hormone supplementation and withdrawal on gastrointestinal and colonic transit in postmenopausal women. Neurogastroenterol Motil. 2006;18:911–8. doi: 10.1111/j.1365-2982.2006.00808.x. [DOI] [PubMed] [Google Scholar]
- 31.Spiegel M, Kanwal F, Naliboff B, et al. The impact of somatization on the use of gastrointestinal health-care resources in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:2262–73. doi: 10.1111/j.1572-0241.2005.00269.x. [DOI] [PubMed] [Google Scholar]
- 32.Lembo A, Ameen VZ, Drossman DA. Irritable bowel syndrome: Toward an understanding of severity. Clin Gastroenterol Hepatol. 2005;3:717–25. doi: 10.1016/s1542-3565(05)00157-6. [DOI] [PubMed] [Google Scholar]
- 33.Cain KC, Headstrom P, Jarrett ME, et al. Abdominal pain impacts quality of life in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:124–32. doi: 10.1111/j.1572-0241.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 34.Munce SE, Stewart DE. Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics. 2007;48:394–9. doi: 10.1176/appi.psy.48.5.394. [DOI] [PubMed] [Google Scholar]