Abstract
Background
Arthralgia affects postmenopausal women receiving aromatase inhibitors (AI) for breast cancer. Given the existing evidence for electro-acupuncture (EA) for treatment of osteoarthritis in the general population, this study aims to establish the feasibility of studying EA for treating AI-related arthralgia.
Patients and Methods
Postmenopausal women with stage I-III breast cancer who reported AI-related arthralgia were enrolled in a single arm feasibility trial. EA was provided twice a week for two weeks followed by six weekly treatments. The protocol was based on Chinese medicine diagnosis of “Bi” syndrome with electro-stimulation of needles around the painful joint(s). Pain severity of the modified Brief Pain Inventory was used as the primary outcome. Joint stiffness, Joint interference, and Patient Global Impression of Change (PGIC) were secondary outcomes. Paired-t tests were used for analysis.
Results
Twelve women were enrolled and all provided data for analysis. From baseline to the end of intervention, patients reported reduction in pain severity (5.3 to 1.9), stiffness (6.9 to 2.4), and joint symptom interference (4.7 to 0.8), all P<0.001; 11/12 considered joint symptoms “very much better” based on PGIC. Subjects also reported significant decrease in fatigue (4.4 to 1.9, p=0.005) and anxiety (7.1 to 4.8, p=0.01). No infection or development or worsening of lymphedema was observed.
Conclusion
Preliminary data establishes the feasibility of recruitment and acceptance as well as promising preliminary safety and effectiveness. A randomized controlled trial is warranted to establish the efficacy of EA for AI-related arthralgia in breast cancer survivors.
Keywords: Acupuncture, breast neoplasm, clinical trial, Aromatase inhibitors/*adverse effects, joint diseases
INTRODUCTION
Aromatase inhibitors (AIs) have become an important standard adjuvant hormonal therapy for postmenopausal women with hormone receptor positive invasive breast cancer. Improvements in disease-free survival have been found in randomized controlled trials (RCTs) to be as high as 40% and greater compared to tamoxifen.1–4 With the increase in its use, AI-related arthralgia is emerging as a major source of symptom burden among its users, with a 28% relative increase compared to placebo.2 Although the understanding of this symptom is extremely limited, in a recent study among 200 ambulatory breast cancer survivors (BCS) receiving AIs, 47% reported AI-related joint pain and 44% reported AI-related stiffness.5 Arthralgia not only impairs function6 but also can lead to treatment discontinuation.7 As medical science introduces life prolonging therapies such as AIs, research is needed to identify and test effective strategies to minimize the side effects of AIs so that both the length and quality of survivorship can be enhanced.
Given the extensive use of complementary therapies by BCS,8, 9 acupuncture is promising as an acceptable non-pharmacological approach for the treatment of AI-related arthralgia. While the exact cause of arthralgia by AIs is unknown, one of the likely explanations is that the depleted estrogen level may decrease the generation of endogenous opioids thereby leading to lowered pain threshold.10 Numerous animal and human studies showed that electro-acupuncture (EA) stimulates the release of endogenous opioids in both brain and spinal cord.11 In addition, the short term (eight weeks) and long term (up to six months) efficacy of acupuncture for osteoarthritis of knee has recently been established through several high quality RCTs.12–14 These studies demonstrated acupuncture not only decreases pain and use of pain medications, but also improves function and quality of life.
Many previous trials of acupuncture suffered from poor methodological rigor and generated findings that were difficult to interpret.15 In order to begin evaluating the effects of acupuncture for AI-related arthralgia, we proposed a pilot study to test the feasibility of conducting a clinical trial of acupuncture for treatment of AI-related arthralgia among BCS. The specific aims of this study were to 1) Demonstrate the feasibility of recruitment and retention to an acupuncture trial; 2) Estimate preliminary effect size, variance, safety, and acceptability of the intervention; 3) Explore the effects of acupuncture on fatigue, anxiety/depression, and sleep; and 4) Explore the relationship between response expectancy towards acupuncture and clinical response measured as pain reduction.
METHODS
Study Patient Population
We recruited eligible patients from the Rowan Breast Cancer Center of the Abramson Cancer Center of the University of Pennsylvania (Philadelphia, PA). Potential participants included women age 18 or older; postmenopausal defined as cessation of menstrual period more than one year, with history of stage I, II, or III breast cancer; currently receiving aromatase inhibitors (Anastrozole, Letrozole, or Exemestane) as per chart documentation; can understand written English. Participants must have had joint pain attributable to AIs and had worst joint pain rated at least four or greater on an 11-point (0–10) numerical rating scale in the preceding week. Key exclusion criteria were metastatic (stage IV) breast cancer; having finished chemotherapy or radiation therapy less than four weeks prior to enrollment because chemotherapy and radiation therapy can cause temporary exacerbation of joint symptoms that typically resolve spontaneously, having had active intervention for pain (such as epidural injection, joint injection, acupuncture, etc.) in the last three months, and history of bleeding disorder because of the safety related to needle puncturing. Informed consent was conducted and obtained from all participants prior to enrollment. University of Pennsylvania Institutional Review Board approved the study protocol.
Study Intervention
Acupuncture was administered by J.M., a licensed physician acupuncturist with five years of experience practicing acupuncture in oncology settings. J.M. is also a pain and palliative medicine physician. Intervention was delivered twice a week for two weeks, then weekly for six more weeks for a total maximum of ten treatments over eight weeks. Subjects may opt to have fewer treatments if joint pain is perceived to be much improved. This type of treatment intensity and duration is common in other acupuncture clinical studies and actual clinical practices.
We developed a manualized protocol (i.e. protocol that is standardized in a manual, but allow the study acupuncturist to modify treatments based on patient clinical characteristics).16–18 We chose a manualized protocol over a fixed acupuncture point protocol because 1) It has been shown to be successful in other trials of acupuncture;13, 16 2) The location of joint pain in breast cancer patients can be variable; and 3) the baseline constitutional symptoms of each breast cancer patient are different. The manualized protocol is based on the Traditional Chinese Medicine (TCM) theory in which joint pain is generally considered as part of the Bi Syndrome.19, 20 The manualized protocol is modified from that described in the text of the Essence of Acupuncture and Moxibustion.19 In developing the protocol, the PI consulted with the faculty of the Beijing Institute of Acupuncture and Moxibustion at Beijing, China. The acupuncturist chose at least four local points around the joint with most pain. Additionally, at least four distant points were used to address the constitutional symptoms such as anxiety and fatigue that are commonly seen in conjunction with pain. This protocol allowed acupuncture to be practiced consistent with the way that is typically done in clinical practice, and also provided a structure for this research to be replicated in the future. The needles (25 mm or 40mm and 0.25 gauge, Seirin, Seirin-America Inc., Weymouth, MA) were inserted until “De Qi” (sensation of soreness, distention, tingling, etc) was reported by patients.21 Two pairs of electrodes were connected at the needles adjacent to the painful joint(s) with two hertz electro-stimulation provided by a TENS unit. The rationale for electro-stimulation was based on animal data suggesting a physiological basis,11, 22 clinical evidence from previous trials,12, 14 as well as PI’s clinical experience. The needles were left in place for 20 minutes with brief manipulation at the beginning and the end of therapy.
Data collection and Outcome measurement
Patient self-reported outcomes were used to measure intervention effects. Surveys were administrated at baseline and at week eight by an RA without the presence of the acupuncturist. Clinical information was obtained via chart abstraction.
To quantify joint symptom severity and functional interference, we developed the Brief Joint Symptom Inventory by modifying the Brief Pain Inventory (BPI). The BPI is one of the most widely used instruments to measure pain in cancer patients and has been demonstrated to be a reliable, valid and responsive measure.23 The numerical rating scale ranges from 0–10, with 10 indicating the greatest severity or interference. Because breast cancer patients may have many sources of pain such as neuropathy and post-surgical pain, we asked the patient to rate pain severity specific to symptoms “in and around joints” to make the measure more specific. We also added two items to quantify joint stiffness with one item asking the severity of stiffness “after first awakening in the morning”, and the other “after sitting, lying, or resting later in the day”, on the same 0 – 10 scale.
To define patient perceived clinical importance, we used Patient Global Impression of Change (PGIC). General questions of this type are often used to track the quality and rate of patient response to therapy.24 “How would you describe your joint pain since the beginning of therapy? I am: very much worse, much worse, a little worse, the same, a little better, much better, very much better.”
Other Symptom Measures: Because research suggests pain may often be accompanied by other concurrent symptoms such as fatigue, anxiety/depression, and sleep disturbance, we incorporated previously validated measures to evaluate the potential effect of acupuncture on these symptoms. Brief Fatigue Inventory (BFI): This nine-item instrument was designed to assess the construct of fatigue severity in cancer and non-cancer populations.25 The numerical rating scale ranges from 0–10, with 10 indicating the greatest severity or interference. The score of the scale was found to be reliable and valid in diverse cancer populations25, 26 and responded to changes seen in a pilot acupuncture study.27 Hospital Anxiety and Depression Scale (HADS): HADS is a 14-item scale with seven items measuring depression and seven items measuring anxiety.28 The scale uses varying response items. Factor analysis showed two distinct but correlated factors in cancer patients.29 The score of the scale has been shown to be both reliable and valid in diverse groups of cancer patients30 and appears to be a clinically useful instrument in cancer patient care.31 Pittsburgh Sleep Quality Index (PSQI): This global score was used to determine the effect of treatments on sleep. The psychometric properties of the PSQI have been supported widely in a variety of populations, including breast cancer survivors.32 Recently, this scale was used in a small study of acupuncture for nocturnal hot flashes and sleep quality among healthy postmenopausal women, which demonstrated significant correlations between improvements in PSQI and reductions in nocturnal hot flash severity and frequency.16
Because emerging research suggests the role of response expectancy in predicting outcome of acupuncture,33 we used a previously validated four-item Acupuncture Expectancy Scale (AES)34 to evaluate the change of response expectancy during acupuncture therapy and the relationship between response expectancy and clinical response to acupuncture.
Statistical Analysis and Sample Size Calculation
Data analysis was performed using the SAS software (SAS version 9.1, SAS Institute, Cary, NC) by Dr. Xie and Ms. Han. Descriptive and graphical methods were used to examine the distribution and normality of data. Normality assumption of the data was checked and found appropriate. The primary comparison between the week eight and baseline outcomes was compared using paired-t test. For the secondary analysis, we performed Pearson correlation test to examine whether the change in pain was also related to fatigue or anxiety. We also used Pearson correlation to examine the relationship between response expectancy and clinical outcome of acupuncture. All statistical tests were two-sided. We calculated the sample size based on assumption that standard deviation (SD) will be larger or equal to half of the mean. If acupuncture could have caused 40% reduction in pain severity, we would need ten subjects to detect such difference using a two-sided significance level of 0.05 and power of 80%. A loss to follow up rate of 15% would necessitate enrollment of 12 subjects to fall within the precision noted in the sample size calculation.
RESULTS
Participant Characteristics
Between July 2007 and December 2007, 40 patients were referred because of joint pain. Of this group, 13 did not return screening telephone calls; nine did not meet eligibility criteria: two had already stopped AIs; one was receiving acupuncture elsewhere; and six had other medical reasons (e.g. recent epidural injection, fracture, metastatic disease). Six patients refused enrollment: two due to distance, and four due to schedule conflicts. Twelve patients enrolled. Demographics of the participants are seen in Table 1.
Table 1.
Demographic and clinical characteristics of clinical trial participants (N=12)
| Median age, years (min-max) | 59 (52–70) |
| Race, No. (%) | |
| White | 10 (83.3%) |
| Black | 2 (16.7%) |
| Employment, no. (%) | |
| Full-time | 5 (41.7%) |
| Part-time | 2 (16.7%) |
| Not currently employed | 5 (41.7%) |
| Education | |
| High school or less | 2 (16.7%) |
| College | 3 (25.0%) |
| Graduate or professional school | 7 (58.3%) |
| Median years since menopause (min-max) | 9.6 (2–19) |
| Median body mass index, kg/m2 (min-max) | 28.8 (19.5–37.6) |
| Aromatase inhibitors, no. (%) | |
| Anastrozole | 5 (41.7%) |
| Letrozole | 4 (33.3%) |
| Exemestane | 3 (25.0%) |
| Stage of breast cancer, no. (%) | |
| I | 8 (66.7%) |
| II | 2 (16.7%) |
| III | 2 (16.7%) |
| Joint(s) with most pain | |
| Knee | 6 (50.0%) |
| Wrists/hands | 2 (16.7%) |
| Ankles/feet | 4 (33.3%) |
The mean age of the women enrolled was 59 years with a standard deviation of 20. Ten patients (83%) were non-Hispanic white, two (17%) were non-Hispanic black. Seven (59%) were currently employed, seven (58%) had graduate or professional schooling. Six (50%) reported worst joint pain in knees, two (17%) in wrists/hands, four (33%) in ankles/feet. Eight patients completed ten treatments, two completed nine treatments (both skipped one treatment because of very little pain towards the end of the intervention), one patient completed five treatments because her pain was very minimal after three visits, and one patient withdrew from the study intervention after five treatments due to development of herpes zoster (her acupuncture treatment was focused on knee pain). Her husband had received zoster vaccine two weeks prior. Safety: Despite needle placement in the same arm as breast cancer surgery, no case of infection, development of or worsening of lymphedema occurred based on patient self-report and clinician exam. Two grade one (mild) pain at the needling sites following acupuncture treatment were reported and spontaneously resolved. All patients provided final assessment and data were analyzed.
Improvement in Joint Symptoms
At baseline, mean joint pain severity rating (SD) was 5.31 (1.49), joint stiffness was 6.88(2.43), and joint functional interference was 4.74 (2.70). At the end of intervention, mean joint pain rating was 1.85(1.54), joint stiffness was 2.42(1.89), and joint functional interference was 0.81(0.83). This change represents an approximately 60% reduction in joint pain from baseline. At the end of intervention based on PGIC rating, 11 subjects considered their joint pain very much better, and one subject considered joint pain much better compared with baseline.
Changes in other symptoms related to Joint Pain
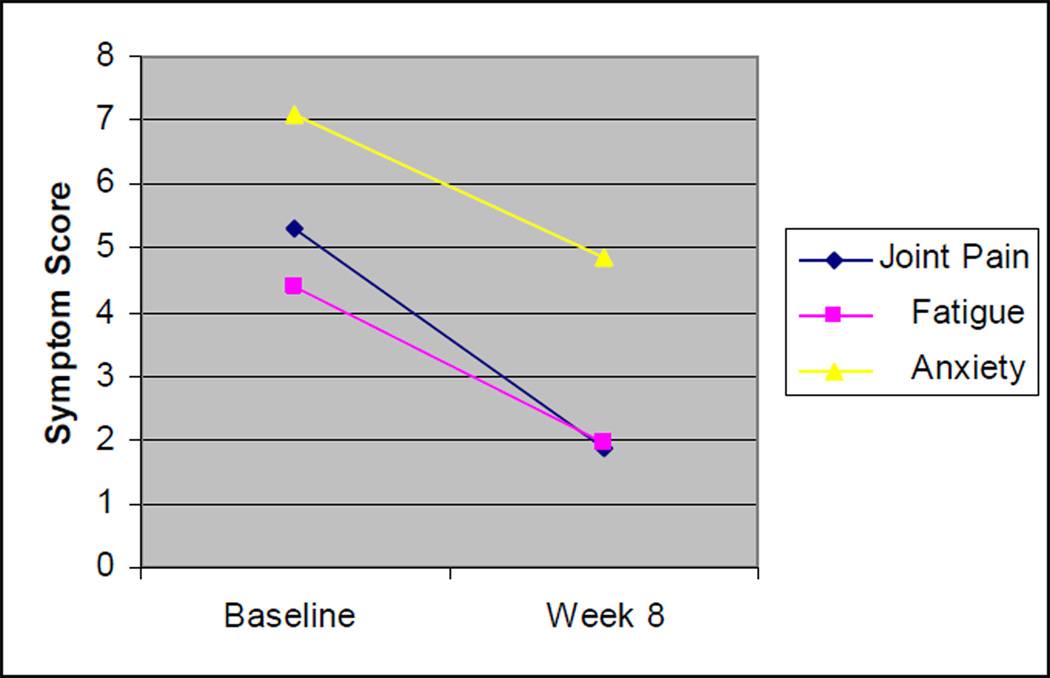
Subjects also experienced a significant reduction in fatigue (4.38 to 1.93, p=0.005), and anxiety (7.08 to 4.83, p=0.01). Subjects had a non-statistically significant reduction in depression (5.08 to 3.83, p=0.20). Global sleep score did not change before and after the intervention (6.83 to 6.17, p=0.47), see table 2. Although not statistically significant, change in joint pain demonstrated a trend towards correlation to change in fatigue (r=0.39, p=0.20) and change in anxiety (r=0.28, p=0.38), see Figure 1.
Table 2.
Change in joint pain and other symptom outcomes (N=12)
| Baseline Mean (SD) |
Week 8 Mean (SD) |
P-value* | |
|---|---|---|---|
| Brief Joint Symptom Inventory | |||
| Pain Severity | 5.31 (1.49) | 1.85 (1.54) | <0.0001 |
| Stiffness | 6.88 (2.43) | 2.42 (1.89) | <0.0001 |
| Joint Symptom Interference | 4.74 (2.70) | 0.81 (0.83) | 0.0001 |
| Brief Fatigue Inventory | 4.38 (2.48) | 1.93 (1.29) | 0.005 |
| Hospital of Anxiety and Depression Scale | |||
| Anxiety | 7.08 (4.72) | 4.83 (3.38) | 0.014 |
| Depression | 5.08 (4.25) | 3.83 (3.10) | 0.2 |
| Pittsburgh Sleep Quality Index (Global) | 6.83 (3.13) | 6.17 (2.41) | 0.47 |
P-value was evaluated base on paired t-test
Figure 1. Change in joint pain may relate to change in fatigue and anxiety.
*joint pain was measured by the Brief Joint Symptom Inventory, fatigue was measured by the Brief Fatigue Inventory, and anxiety was measured by the Hospital Anxiety and Depression Scale
Relationship between expectancy and pain improvement
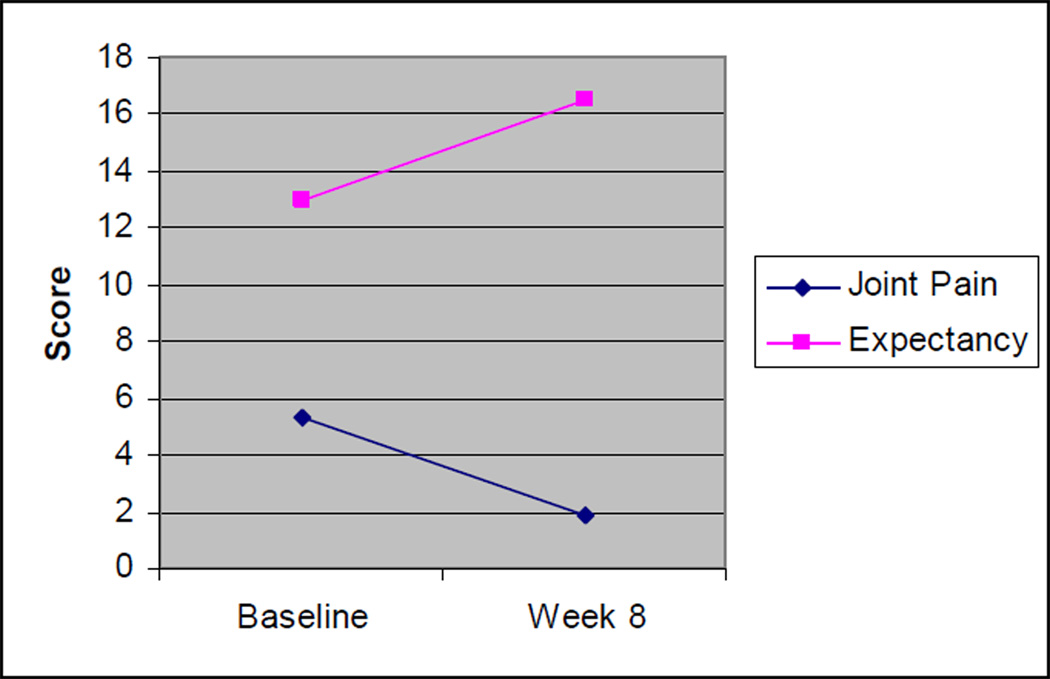
Response expectancy toward acupuncture increased during the course of the therapy from baseline (13.00, 3.85) to the end of intervention (16.50, 2.58), p<0.001. Baseline expectancy was not correlated to change in pain (r=0.12, p=0.72). Increase in response expectancy may be associated with reduction in pain, although statistically not significant in this small study (r=-0.26, p=0.45), see figure 2.
Figure 2. Change in joint pain may relate to change in acupuncture expectancy.
*Joint pain was measured by the Brief Joint Symptom Inventory, and expectancy was measured by the Acupuncture Expectancy Scale.
DISCUSSION
In this study, we demonstrated successful recruitment and retention to an acupuncture intervention for AI-related arthralgia, as well as preliminary efficacy and safety data. Patients reported approximately a 60% reduction in joint pain severity, stiffness, and functional interference. Acupuncture was well tolerated, and despite needling in arms on the side where breast cancer surgery was performed, no infection, development or worsening of lymphedema was reported. Acupuncture not only appeared to reduce pain, but also may have improved anxiety and fatigue. Furthermore, this is the first known study to demonstrate an increase in response expectancy during acupuncture therapy that may be related to clinical response to acupuncture.
It is important to acknowledge the limitations of the study. This single arm clinical trial aimed at establishing feasibility and preliminary effects. The lack of a control group negates the ability to exclude that findings were due to placebo effect, natural progression of disease, or regression to the mean effect. We did not measure long term follow up data after the intervention was completed. The acupuncturist is a physician acupuncturist with pain and palliative expertise which may limit generalizability of the intervention for application by general community acupuncturists. However, this type of early phase acupuncture trial offers an important opportunity to test recruitment and retention strategies, to refine the acupuncture procedure, and to obtain preliminary effect size and variance. Only by accomplishing such a step, can we appropriately design and power a randomized controlled study of acupuncture for symptom palliation in an oncology setting.35 As shown by our study, only 12 out of 40 potential subjects met eligibility requirement and agreed to participation; thus, future randomized controlled trials need to have a sufficient population base and decrease patient barriers to enhance the effective conduct of such studies.
The exact mechanism of action for acupuncture for AI-related arthralgia is not fully understood. Animal and human studies have demonstrated an analgesic effect that is mediated in part by endogenous opioid release.36 It is possible that increased endogenous opioid and other neurotransmitters may attenuate the pain detection threshold in AI-users.
Second, neuroimaging techniques including positron emission tomography (PET) scan,37–39 single-photon emission computed tomography (SPECT),40 and functional MRI41–44 have also provided preliminary evidence that acupuncture may modulate the limbic system,41, 45 which are involved in processing of cognitive and affective aspects of pain in humans. Furthermore, non-specific effects such as response expectancy may also play an integral part in mediating the CNS response to acupuncture.37, 39 Thus, future study of the effect of acupuncture for AI-related arthralgia using appropriate imaging techniques may establish the potential mechanism of acupuncture for AI-related arthralgia.
Third, data also suggests that acupuncture may affect peripheral tissue where needles are placed. There is some evidence that acupuncture can cause vasodilatation,46, 47 and connective tissue displacement.48–50 Chae et al. recently found in a rat model with acute paw edema (induced by carrageenan), acupuncture stimulation significantly reduced IL-6 level, beta-nerve growth factor, and tissue inhibitors of metalloproteinase-1.51
Based on the above findings, acupuncture may activate a combination of central and peripheral processes that may act synergistically to create persistent clinical changes for chronic symptoms such as AI-related arthralgia. Thus, using acupuncture and clinically relevant outcomes in both animals as well as humans may serve as an important translational model for understanding the etiology of AI-related arthralgia as well as the mechanisms of acupuncture.
We not only found significant improvement in pain but also associated improvement in anxiety and fatigue. These findings suggest that whether the effect of acupuncture is through CNS or peripheral modulation, the effects are likely to be systemic, i.e. affecting multiple symptoms simultaneously. Given that cancer patients and survivors often experience multiple symptoms, our finding is particularly encouraging, and future randomized controlled trials are needed to evaluate the effects of acupuncture on multiple co-occurring symptoms.
A recent large study that found response expectancy was predictive of outcome of acupuncture in multiple painful syndromes.33 We did not find a statistically significant correlation between response expectancy and pain outcome, but all the patients in this small study had a relatively high level of response expectancy and it stayed high. Second, all trial participants achieved a substantial clinical response; therefore, the lack of variability of response combined with small sample size may limit the power in detecting statistical significance. Nevertheless, we found that response expectancy increased during the acupuncture. This preliminary finding supports the hypothesis that clinical response may reinforce response expectancy. Therefore, the relationship between response expectancy and clinical outcome in acupuncture may be reciprocal and iterative. The appropriate use of a validated Acupuncture Expectancy Scale34 in future large randomized controlled clinical trials may help evaluate the mind-body interaction of acupuncture in achieving sustainable outcome for chronic symptom palliation.
In summary, we have conducted a successful feasibility trial of acupuncture to treat AI-related arthralgia. As AI-related arthralgia is a relatively new clinical phenomenon and very few intervention studies have been performed to address this clinical problem, we believe our effort is an important first step in demonstrating the feasibility of rigorous evaluation of acupuncture for this indication. Future randomized controlled trials are needed to establish the comparative efficacy of acupuncture to address AI-related arthralgia, a clinical problem affecting hundreds of thousands of breast cancer survivors.
Acknowledgements
This study is in part supported by grants from the American Cancer Society #IRG-78-002-30 and Pennsylvania Department of Aging. Dr. Mao is a recipient of the NCCAM 1 K23 AT004112 award. The funding agencies had no role in design or conduct of the study. We would like to acknowledge the contributions of the Recruitment, Retention, and Outreach Core Facility of the Abramson Cancer Center for assisting with the development and implementation of the recruitment and retention plan. We also thank Dingyun Chan, Jamie Wolf, and Brandon Greene for data entry and management. Sincere thanks also go to the patients, oncologists, nurse practitioners, and staff for their support of this study.
References
- 1.Jakesz R, Jonat W, Gnant M, et al. Switching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years' adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. Lancet. 2005 Aug 6–12;366(9484):455–462. doi: 10.1016/S0140-6736(05)67059-6. [DOI] [PubMed] [Google Scholar]
- 2.Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med. 2003 Nov 6;349(19):1793–1802. doi: 10.1056/NEJMoa032312. [DOI] [PubMed] [Google Scholar]
- 3.Howell A, Cuzick J, Baum M, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years' adjuvant treatment for breast cancer. Lancet. 2005 Jan 1–7;365(9453):60–62. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 4.Coombes RC, Hall E, Gibson LJ, et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med. 2004 Mar 11;350(11):1081–1092. doi: 10.1056/NEJMoa040331. [DOI] [PubMed] [Google Scholar]
- 5.Crew KD, Greenlee H, Capodice J, et al. Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol. 2007 Sep 1;25(25):3877–3883. doi: 10.1200/JCO.2007.10.7573. [DOI] [PubMed] [Google Scholar]
- 6.Morales L, Pans S, Paridaens R, et al. Debilitating musculoskeletal pain and stiffness with letrozole and exemestane: associated tenosynovial changes on magnetic resonance imaging. Breast Cancer Res Treat. 2006 Oct 24; doi: 10.1007/s10549-006-9394-6. [DOI] [PubMed] [Google Scholar]
- 7.Donnellan PP, Douglas SL, Cameron DA, Leonard RC. Aromatase inhibitors and arthralgia. J Clin Oncol. 2001 May 15;19(10):2767. [PubMed] [Google Scholar]
- 8.Boon HS, Olatunde F, Zick SM. Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health. 2007;7:4. doi: 10.1186/1472-6874-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao JJ, Palmer SC, Straton JB, et al. Cancer survivors with unmet needs were more likely to use complementary and alternative medicine. J Cancer Surviv. 2008 Jun;2(2):116–124. doi: 10.1007/s11764-008-0052-3. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Cummings SR. Aromatase inhibitors and the syndrome of arthralgias with estrogen deprivation. Arthritis Rheum. 2005 Sep;52(9):2594–2598. doi: 10.1002/art.21364. [DOI] [PubMed] [Google Scholar]
- 11.Han JS. Acupuncture and endorphins. Neurosci Lett. 2004 May 6;361(1–3):258–261. doi: 10.1016/j.neulet.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Vas J, Mendez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. Bmj. 2004 Nov 20;329(7476):1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005 Jul 9–15;366(9480):136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 14.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004 Dec 21;141(12):901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 15.Langevin HM, Hammerschlag R, Lao L, Napadow V, Schnyer RN, Sherman KJ. Controversies in acupuncture research: selection of controls and outcome measures in acupuncture clinical trials. J Altern Complement Med. 2006 Dec;12(10):943–953. doi: 10.1089/acm.2006.12.943. [DOI] [PubMed] [Google Scholar]
- 16.Huang MI, Nir Y, Chen B, Schnyer R, Manber R. A randomized controlled pilot study of acupuncture for postmenopausal hot flashes: effect on nocturnal hot flashes and sleep quality. Fertil Steril. 2006 Sep;86(3):700–710. doi: 10.1016/j.fertnstert.2006.02.100. [DOI] [PubMed] [Google Scholar]
- 17.Nir Y, Huang MI, Schnyer R, Chen B, Manber R. Acupuncture for postmenopausal hot flashes. Maturitas. 2007 Apr 20;56(4):383–395. doi: 10.1016/j.maturitas.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Schnyer RN, Iuliano D, Kay J, Shields M, Wayne P. Development of protocols for randomized sham-controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis-related pelvic pain. J Altern Complement Med. 2008 Jun;14(5):515–522. doi: 10.1089/acm.2007.0826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Essentials of Chinese Acupuncture. Beijing, P.R. China: Foreign Languages Press; 1993. Anonymous. [Google Scholar]
- 20.Cheng X, editor. Chinese acupuncture and moxibustion. Beijing, China: Foreign Languages Press; 1987. [Google Scholar]
- 21.Mao JJ, Farrar JT, Armstrong K, Donahue A, Ngo J, Bowman MA. De qi: Chinese acupuncture patients' experiences and beliefs regarding acupuncture needling sensation--an exploratory survey. Acupunct Med. 2007 Dec;25(4):158–165. doi: 10.1136/aim.25.4.158. [DOI] [PubMed] [Google Scholar]
- 22.Han JS, Xie GX, Zhou ZF, Folkesson R, Terenius L. Enkephalin and beta-endorphin as mediators of electro-acupuncture analgesia in rabbits: an antiserum microinjection study. Adv Biochem Psychopharmacol. 1982;33:369–377. [PubMed] [Google Scholar]
- 23.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994 Mar;23(2):129–138. [PubMed] [Google Scholar]
- 24.Sloan JA, Aaronson N, Cappelleri JC, Fairclough DL, Varricchio C, Clinical Significance Consensus Meeting G. Assessing the clinical significance of single items relative to summated scores. 2002 May;:479–487. [PubMed] [Google Scholar]
- 25.Mendoza TR, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999 Mar 1;85(5):1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 26.Lin CC, Chang AP, Chen ML, Cleeland CS, Mendoza TR, Wang XS. Validation of the Taiwanese version of the Brief Fatigue Inventory. J Pain Symptom Manage. 2006 Jul;32(1):52–59. doi: 10.1016/j.jpainsymman.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 27.Vickers AJ, Straus DJ, Fearon B, Cassileth BR. Acupuncture for postchemotherapy fatigue: a phase II study. J Clin Oncol. 2004 May 1;22(9):1731–1735. doi: 10.1200/JCO.2004.04.102. [DOI] [PubMed] [Google Scholar]
- 28.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 29.Moorey S, Greer S, Watson M, et al. The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. Br J Psychiatry. 1991 Feb;158:255–259. doi: 10.1192/bjp.158.2.255. [DOI] [PubMed] [Google Scholar]
- 30.Smith AB, Selby PJ, Velikova G, et al. Factor analysis of the Hospital Anxiety and Depression Scale from a large cancer population. Psychol Psychother. 2002 Jun;75(Pt 2):165–176. doi: 10.1348/147608302169625. [DOI] [PubMed] [Google Scholar]
- 31.Sellick SM, Edwardson AD. Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psychooncology. 2006 Sep 21; doi: 10.1002/pon.1085. [DOI] [PubMed] [Google Scholar]
- 32.Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL. Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum. 2004 May;31(3):591–5598. doi: 10.1188/04.onf.591-598. [DOI] [PubMed] [Google Scholar]
- 33.Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007 Apr;128(3):264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Mao JJ, Armstrong K, Farrar JT, Bowman MA. Acupuncture expectancy scale: development and preliminary validation in China. Explore (NY) 2007 Jul-Aug;3(4):372–377. doi: 10.1016/j.explore.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lao L, Berman B. [Evaluating the effects of acupuncture on knee osteoarthritis: a stepwise approach to research, University of Maryland experience] Zhong Xi Yi Jie He Xue Bao. 2005 Nov;3(6):421–425. doi: 10.3736/jcim20050601. [DOI] [PubMed] [Google Scholar]
- 36.Han JS. Acupuncture and endorphins. Neurosci Lett. 2003;361(1–3):258–261. doi: 10.1016/j.neulet.2003.12.019. Neurosci Lett. [DOI] [PubMed] [Google Scholar]
- 37.Lewith GT, White PJ, Pariente J. Investigating acupuncture using brain imaging techniques: the current state of play. Evid Based Complement Alternat Med. 2005 Sep;2(3):315–319. doi: 10.1093/ecam/neh110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Biella G, Sotgiu ML, Pellegata G, Paulesu E, Castiglioni I, Fazio F. Acupuncture produces central activations in pain regions. Neuroimage. 2001 Jul;14(1 Pt 1):60–66. doi: 10.1006/nimg.2001.0798. [DOI] [PubMed] [Google Scholar]
- 39.Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005 May 1;25(4):1161–1167. doi: 10.1016/j.neuroimage.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 40.Newberg AB, Lariccia PJ, Lee BY, Farrar JT, Lee L, Alavi A. Cerebral blood flow effects of pain and acupuncture: a preliminary single-photon emission computed tomography imaging study. J Neuroimaging. 2005 Jan;15(1):43–49. doi: 10.1177/1051228404271005. [DOI] [PubMed] [Google Scholar]
- 41.Hui KK, Liu J, Makris N, et al. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Human Brain Mapping. 2000;9(1):13–25. doi: 10.1002/(SICI)1097-0193(2000)9:1<13::AID-HBM2>3.0.CO;2-F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fang JL, Krings T, Weidemann J, Meister IG, Thron A. Functional MRI in healthy subjects during acupuncture: different effects of needle rotation in real and false acupoints. Neuroradiology. 2004 May;46(5):359–362. doi: 10.1007/s00234-003-1125-7. [DOI] [PubMed] [Google Scholar]
- 43.Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp. 2005 Mar;24(3):193–205. doi: 10.1002/hbm.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu MT, Sheen JM, Chuang KH, et al. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage. 2002 Aug;16(4):1028–1037. doi: 10.1006/nimg.2002.1145. [DOI] [PubMed] [Google Scholar]
- 45.Hui KK, Liu J, Marina O, et al. The integrated response of the human cerebro-cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. Neuroimage. 2005 Sep;27(3):479–496. doi: 10.1016/j.neuroimage.2005.04.037. [DOI] [PubMed] [Google Scholar]
- 46.Boutouyrie P, Corvisier R, Azizi M, et al. Effects of acupuncture on radial artery hemodynamics: controlled trials in sensitized and naive subjects. Am J Physiol Heart Circ Physiol. 2001 Feb;280(2):H628–H633. doi: 10.1152/ajpheart.2001.280.2.H628. [DOI] [PubMed] [Google Scholar]
- 47.Litscher G, Wang L, Huber E, Nilsson G. Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci. 2002;17(1):19–25. doi: 10.1007/s10103-002-8262-9. [DOI] [PubMed] [Google Scholar]
- 48.Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002 Dec 15;269(6):257–265. doi: 10.1002/ar.10185. [DOI] [PubMed] [Google Scholar]
- 49.Langevin HM, Churchill DL, Wu J, et al. Evidence of connective tissue involvement in acupuncture. Faseb J. 2002 Jun;16(8):872–874. doi: 10.1096/fj.01-0925fje. [DOI] [PubMed] [Google Scholar]
- 50.Langevin HM, Konofagou EE, Badger GJ, et al. Tissue displacements during acupuncture using ultrasound elastography techniques. Ultrasound Med Biol. 2004 Sep;30(9):1173–1183. doi: 10.1016/j.ultrasmedbio.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 51.Chae Y, Hong MS, Kim GH, et al. Protein array analysis of cytokine levels on the action of acupuncture in carrageenan-induced inflammation. Neurol Res. 2007;29(Suppl 1):S55–S58. doi: 10.1179/016164107X172365. [DOI] [PubMed] [Google Scholar]