Abstract
Background and Objectives
Although the association between single nucleotide polymorphisms (SNPs) of Serine/Threonine Kinase 39 (STK39) and hypertension has been reported, the prior studies have been inconsistent. The aim of this study is to evaluate the association between rs3754777 and rs6749447, the two SNPs of STK39, and hypertension and other cardiovascular risk factors in Koreans, residing in the Republic of Korea.
Subjects and Methods
We included 238 hypertensive patients and 260 controls. The associations between genotype and haplotype combination and hypertension were examined. In addition, possible SNP-related differences in the adjusted blood pressure and other cardiovascular risk factors were analyzed.
Results
There was no significant association between the two SNPs and hypertension. However, the carriers of AA genotype of rs3754777 showed lower blood glucose and cholesterol levels, particularly in females. Genotype of rs6749447 was associated with the waist circumference, triglyceride, and high density lipoprotein-cholesterol levels, only in gender-stratified analysis. The effects of haplotype combinations on risk factors were compatible with genotype effects of each SNP.
Conclusion
Associations between the two SNPs of STK39, rs3754777 and rs6749447, and hypertension were not significant. However, the two SNPs showed genotype-related differences in blood glucose, lipids, and waist circumference, especially in women. Further studies are needed to clarify the effect of STK39 variants in these cardiovascular risk factors.
Keywords: STK39 protein, human; Hypertension; Cholesterol; Waist circumference; Glucose
Introduction
The pathogenesis of essential hypertension is believed to be multifactorial and under the influence of multiple genetic and environmental factors. Genes associated with blood pressure (BP) are not sufficiently known as yet. A recent genome-wide association study examined single nucleotide polymorphisms (SNPs) in American Old Order Amish and identified SNPs in the Serine/Threonine Kinase 39 (STK39) that were associated with hypertension.1) STK39 encodes a serine/threonine kinase known as a Ste20-related proline-rich kinase (SPAK), one of STE20 family. These kinases were shown to interact with WNK kinases and cation-chloride cotransporters, and it was suggested that their functional change may cause BP dysregulation.1) SPAK also is related to cytoskeletal rearrangement, mitogen activated protein (MAP) kinases, and inflammation.2) Associations between the above mentioned SNPs and different STK39 SNPs and BP were confirmed in other Caucasian and Chinese cohorts.3),4) However, the influence of STK39 polymorphism on BP has been inconsistent, and the effects of the variants have not been found in other large studies.5-7) Although a few studies have been conducted to replicate the results in the Asian population, the association between STK39 variants and hypertension is still unclear in Asians.
Here we examined the effect of rs3754777 and rs6749447, the two representative SNPs of STK39, on hypertension in a South Korean cohort of 238 hypertensives and 260 controls. The primary purpose was to evaluate the association between the two SNPs and the risk of hypertension in females and males. In addition, we investigated the effects of the SNPs on other cardiovascular risk factors. In the present study, we found no significant association between the studied SNPs and hypertension. However, the two SNPs showed genotype-related differences in blood cholesterol, glucose levels, and waist circumference, especially in women. Our study is the first to systemically analyze the association between STK39 variants and multiple cardiovascular risk factors.
Subjects and Methods
Study population
We included 238 consecutive hypertensive patients along with age- and sex-matched 260 healthy controls. Patients were drawn from the Cardiovascular Genome Center registry, Yonsei University Health System. All consecutive patients who visited Severance Cardiovascular Hospital, Seoul, Korea were prospectively screened for hypertension. We recruited patients who had systolic BP greater than 135 mm Hg and/or diastolic BP greater than 85 mm Hg, before taking antihypertensive medications, during the three different. Patients who had already taken antihypertensive medications were also enrolled. Hypertensive patients who were diagnosed at 30-60 years of age were eligible for enrollment. The control subjects were recruited during the health check-up at the Health Promotion Center, Yonsei University Health System, Seoul, Korea. They were matched for sex and age (±5 years) and selected from subjects without history of hypertension. Control subjects had to have systolic BP <135 mm Hg and diastolic BP <85 mm Hg, without BP-lowering agents. Criteria for exclusion included structural heart disease, coronary artery disease, secondary hypertension, diabetes mellitus, or serum creatinine >1.4 mg/dL. The purpose of the study was thoroughly explained to all subjects, and the informed consent was obtained. The local institutional review board approved this study.
Clinical data collection and blood sample analysis
On the day of enrollment, clinical data including demographic variables, medical history, and antihypertensive medications were recorded. BP was measured by trained nurses at the right brachial artery, using a mercury sphygmomanometer. Subjects had 10 minutes of rest in the supine position before the measurements, and the average of at least three measurements were used in the study. To adjust for the drug effects, 8/4, 14/10, and 20/16 mm Hg were added to the measured systolic BP/diastolic BP of patients taking one, two, or three antihypertensive drugs, respectively.3) Venous blood samples were collected after an overnight fast, and samples were analyzed within 4 hours of collection. All analyses were conducted by a local laboratory, certified by the Korean Society of Laboratory Medicine.
Genotyping
Genomic deoxyribonucleic acid (DNA) was extracted from 5 mL of peripheral venous blood using a commercially available isolation kit (QuickGene SP Kit DNA Whole blood, Fujifilm, Tokyo, Japan). Based on prior reports1) on variants in STK39, two relevant polymorphisms, rs3754777 and rs6749447, were selected for analysis. Genotyping was performed using the TaqMan fluorogenic 5' nuclease assay (ABI, Foster City, CA, USA).
Statistical analysis
Group differences in the categorical variables, genotypes, and haplotypes were assessed by chi-square test, and continuous variables were examined by Student's t-test. The association between genotype and hypertension was evaluated using the odds ratios, 95% confidence intervals of the chi-square test, and logistic regression analysis. Possible genotype-related differences in BP and other cardiovascular risk factors were analyzed by Kruskal-Wallis test. Results are expressed as mean±SD or median (interquartile range) and 2-tailed value of p<0.05 was considered statistically significant. All data were analyzed using Statistical Package for the Social Sciences (SPSS) 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics and allele frequencies of the study population
The characteristics of the study population are presented in Table 1. The average age was 50 years, and the ratio of female subjects was 50%. Individuals with hypertension were more likely to have clinical features of metabolic syndrome: higher waist circumference, BP, blood glucose, triglyceride, and lower high density lipoprotein-cholesterol (HDL-C) levels. Two and fifteen subjects were taking glucose lowering and lipid lowering agents, respectively.
Table 1.
Characteristics of the study subjects
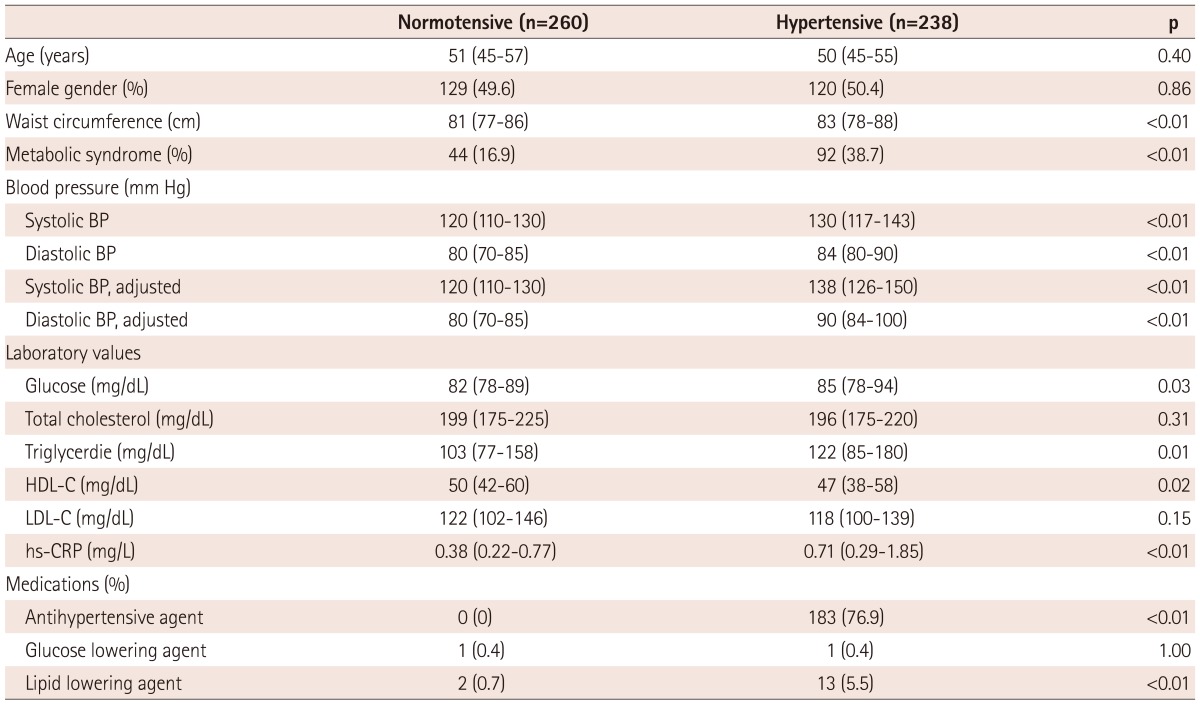
Values are median (interquartile range) or n (%). BP: blood pressure, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein
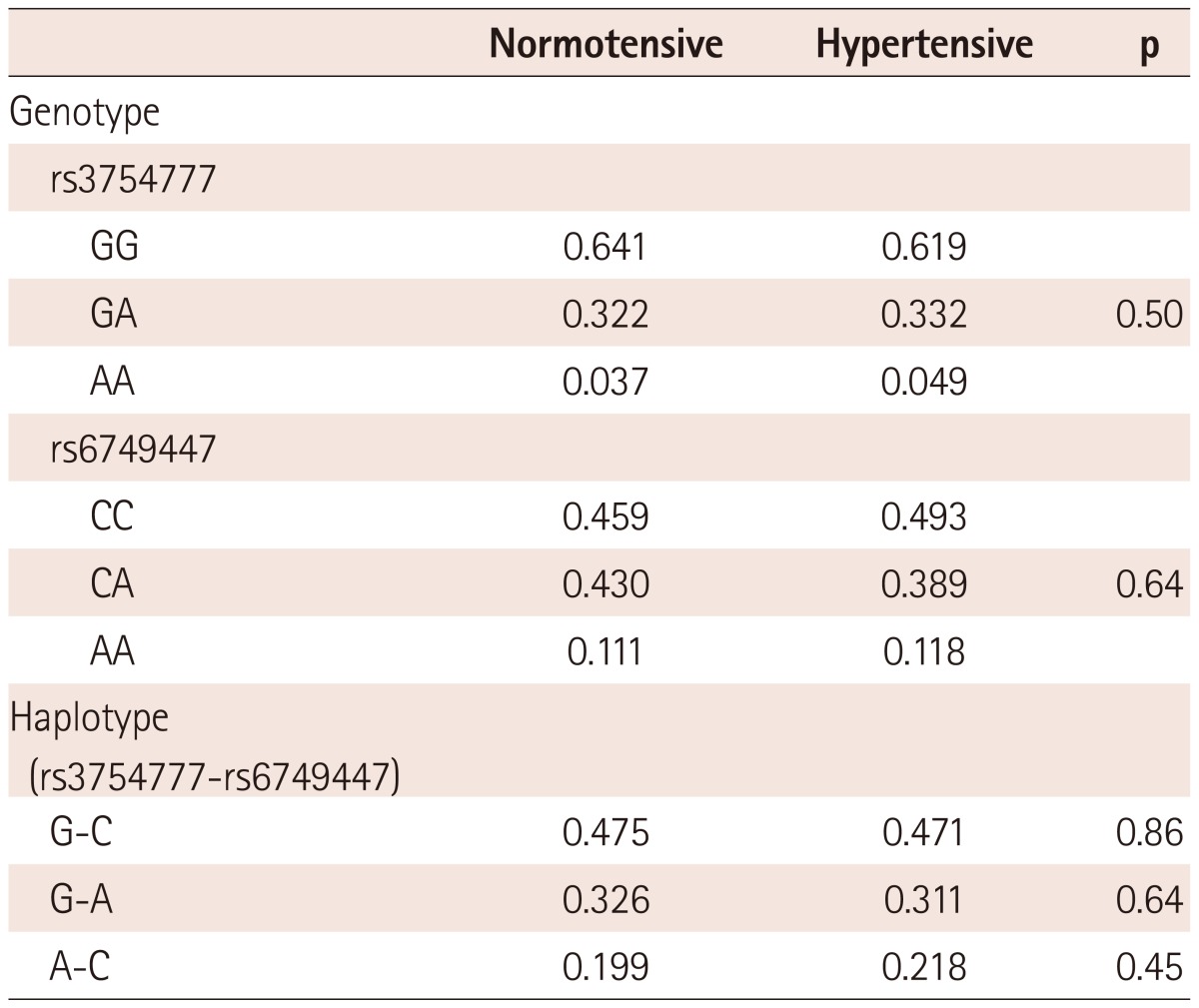
Minor allele frequencies were 0.206 and 0.319 for rs3754777 and rs6749447, respectively. The genotype and haplotype distributions of STK39 polymorphisms were not different between normotensive controls and hypertensive patients (Table 2).
Table 2.
Genotype and haplotype frequencies of the studied variants
Relationship between studied variants and hypertension
The relationship between hypertension risk and genotypes or haplotypes of STK39 in females and males are presented in Table 3. No association between genotypes and hypertension risk in any group reached statistical significance. The association in a subgroup of young subjects (<50 years old) was also significant (Supplementary Table 1). Likewise, the risks of hypertension were not different between the haplotype combinations, although A-C/A-C haplotype showed a tendency to have hypertension in the female subgroup.
Table 3.
Relative risk for hypertension based on genotype and haplotype of the studied variants
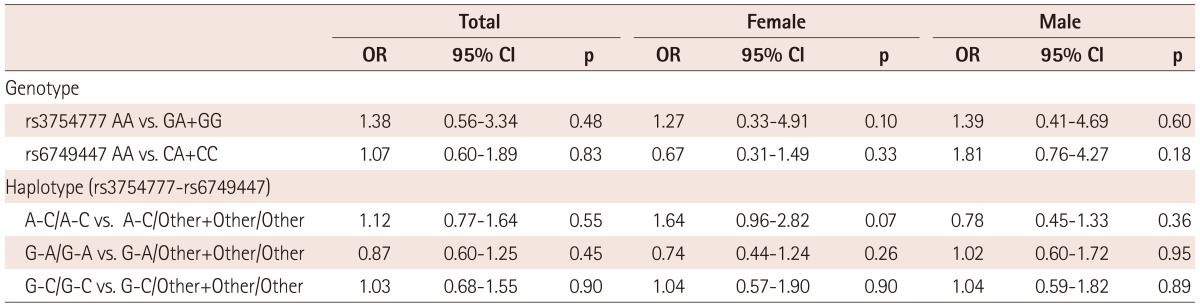
OR: odds ratio, CI: confidence interval
Supplementary Table 1.
Relative risk for hypertension based on genotype and haplotype of the studied variants (in subjects with age <50 years)
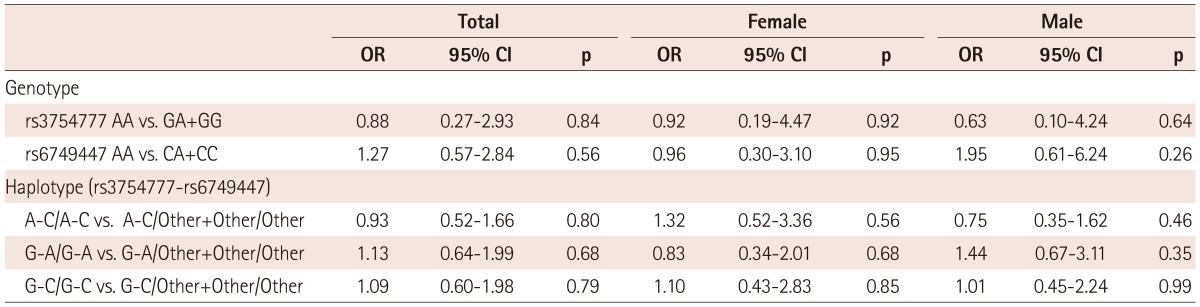
OR: odds ratio, CI: confidence interval
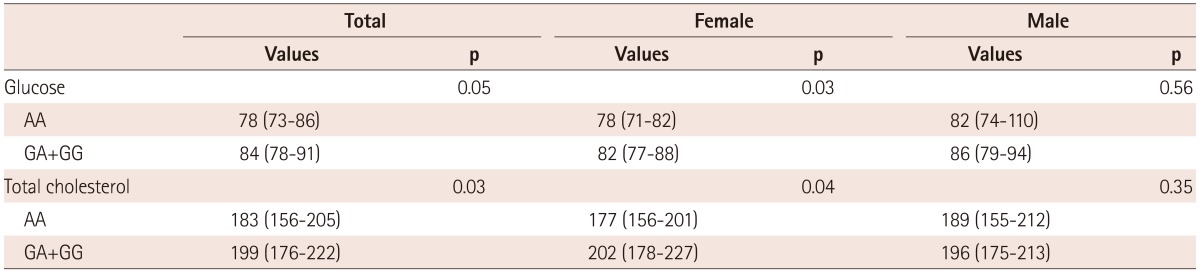
Relationship between studied variants, blood pressure, and cardiovascular risk factors
Mean±SD or median (interquartile range) and Kruskal-Wallis analysis p for cardiovascular risk factors for all genotypes are listed in Table 4. Adjusted systolic and diastolic BP were similar between all genotypes in both rs3754777 and rs6749447 variants. However, rs 3754777 showed significant genotype-related differences for glucose and total cholesterol. Subjects with AA genotype had lower glucose and cholesterol levels. In analyses stratified by the gender, this difference was statistically significant only in females. In analyses of subgroups not taking glucose or lipid lowering agents, the associations showed only minimal changes (p were 0.055 and 0.03 with regard to glucose and total cholesterol, respectively) (Supplementary Table 2). Low density lipoprotein-cholesterol (LDL-C) was lower in females with AA genotype of rs3754777. The genotype of rs6749447 was not related to specific risk factors. However, in gender-stratified analyses, AA genotype of rs6749447 showed lower waist circumference compared to other genotypes in females. In males, AA genotype revealed higher triglyceride and lower HDL-C levels.
Table 4.
Association of genotype of the studied variants and parameters of cardiovascular risk
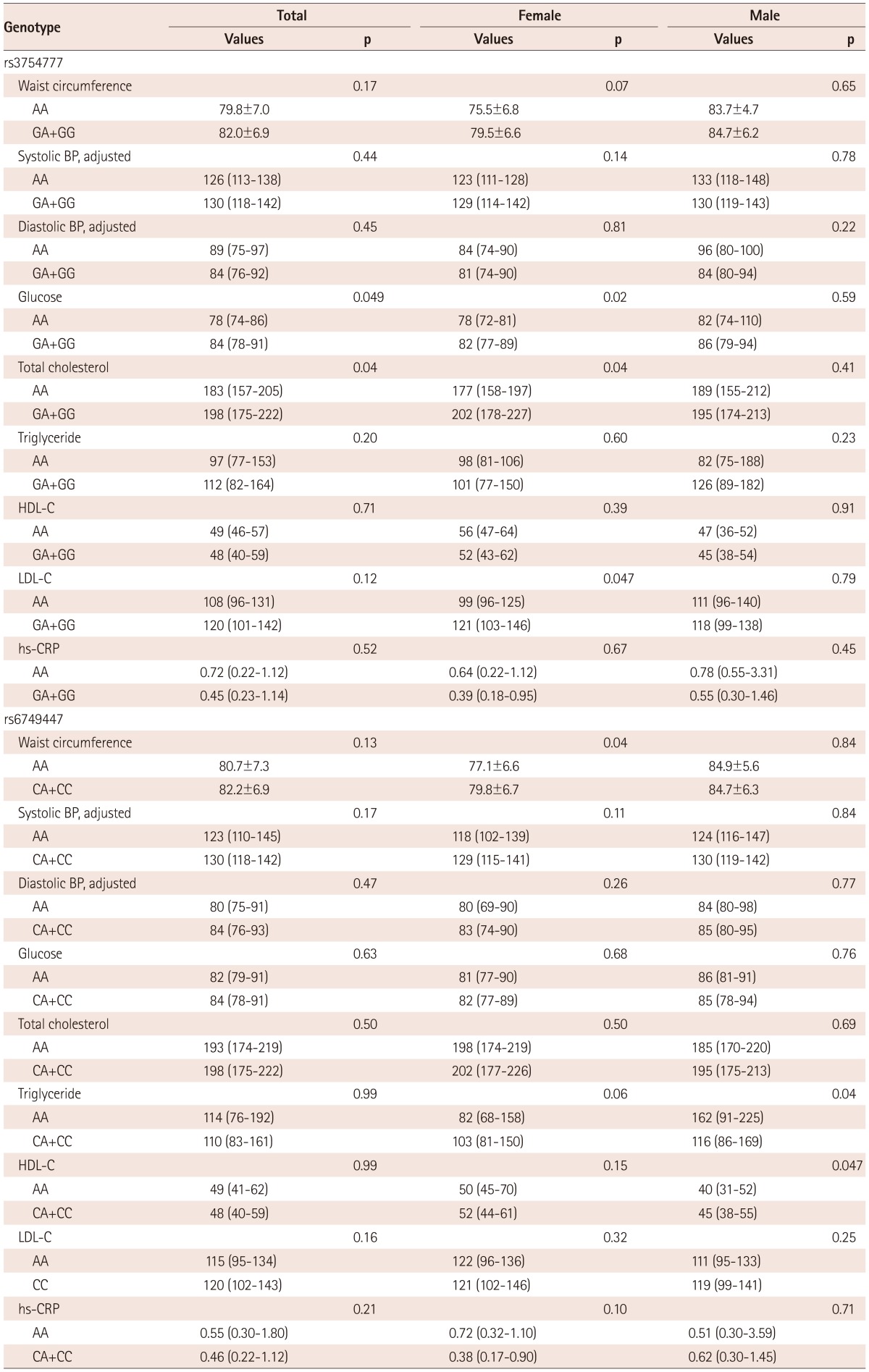
Values are mean±SD or median (interquartile range). BP: blood pressure, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein
Supplementary Table 2.
Association of genotype of rs3754777 and glucose and cholesterol (in subjects without glucose- or lipid lowering agents)
Values are median (interquartile range)
Association between STK39 rs3754777A-rs6759557C haplotype combinations and cardiovascular risk factors are largely compatible with those between the genotypes and risk factors (Supplementary Table 3). For instance, haplotype combination A-C was associated with lower glucose and total cholesterol values. Other gender-stratified findings are listed in the same table.
Supplementary Table 3.
Association between haplotype of the studied variants and parameters of cardiovascular risk
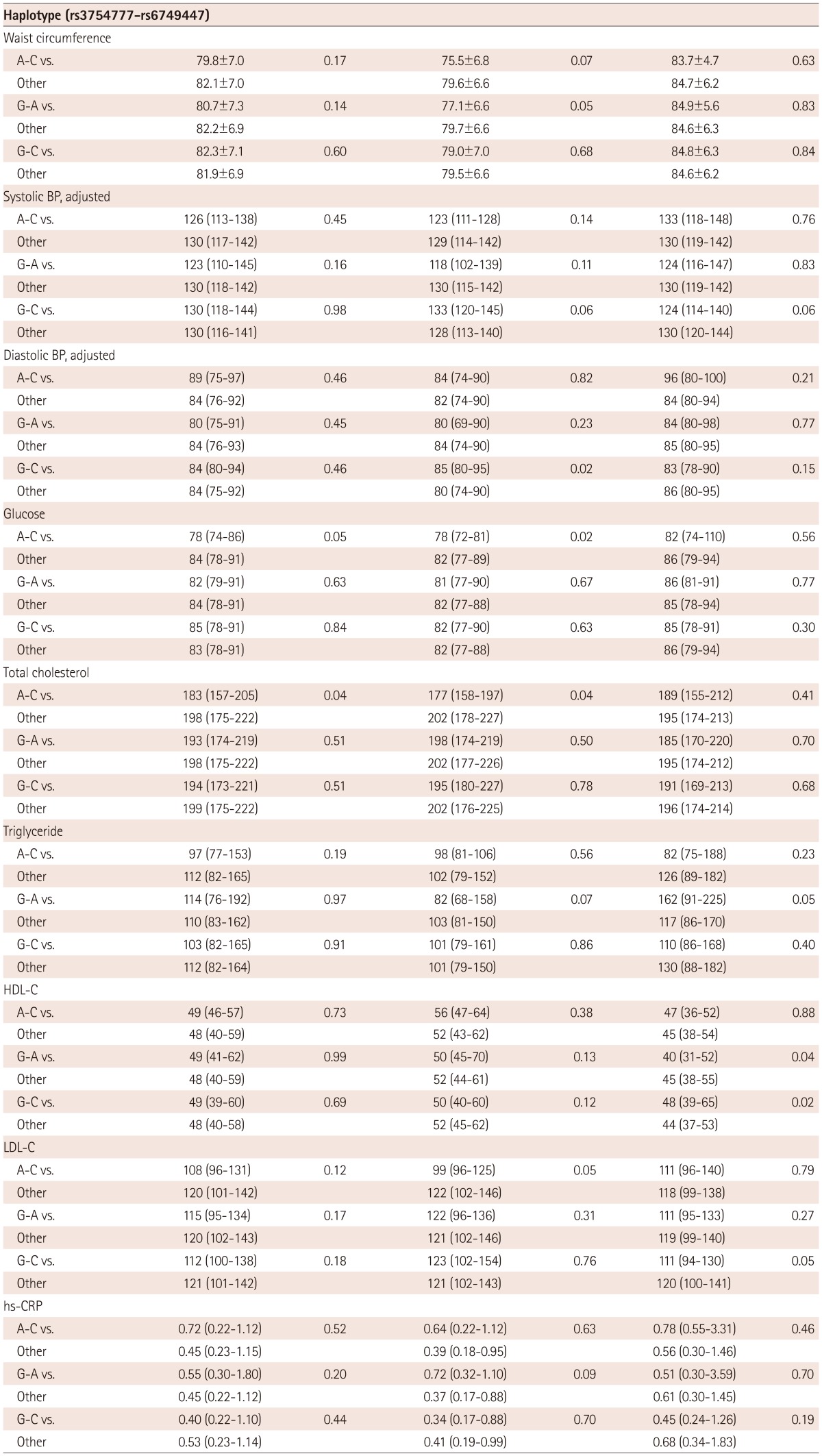
Values are mean±SD or median (interquartile range). BP: blood pressure, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein
Discussion
In the current study, we found no association between two SNPs, rs3754777 and rs6749447, located within STK39 and hypertension in a cohort of 498 Koreans. Although there was no implication of these SNPs on adjusted BPs, they were associated with other cardiovascular risk factors. The carriers of AA genotype of rs3754777 had lower blood glucose and cholesterol levels. This relationship was more obvious in females. Although genotype of rs6749447 was not related to specific risk factors, it was associated with waist circumference, triglyceride, and HDL-C levels in gender stratified analysis. Association between haplotype combination of studied SNPs and risk factors were compatible with genotype-risk factor relationship of each SNP.
Polymorphisms of STK39 were reported to be associated with BP first in Caucasian samples.1) In the meta-analysis combining four studies, Wang et al.1) showed the effects of SNPs of rs6749447 and rs3754777 on BP. Another SNP of STK39, rs35929607, was also related to the hypertension prevalence in women of two cohorts in Swedes.3) In the Chinese population, two SNPs of STK39, rs6433027 and 3754777, were found to be associated with hypertension.4)
In the results of this study, the associations between STK39 SNPs and hypertension or BP were not significant. Although the reason for the discrepancy is not clear, several possibilities may be suggested. First, all the samples were of Koreans residing in the Republic of Korea, and the STK39-BP relationship may be weaker in this population. The influence of STK39 polymorphism on BP has not been consistently confirmed. In the two large GWAS, using more than 60000 people, the effects of STK39 SNPs on BP were not found.5),6) In addition, in one British7) and one Chinese8) study, variants of STK39 were not associated with BP. Recently, Rhee et al.9) reported four previously reported SNPs associated with salt-sensitivity in 101 Koreans. However, in that study, no polymorphism of STK39 showed significant effects after adjusting for confounding factors. Second, although STK39 gene encodes for a protein that plays a role in BP regulation, its final effects may be too small to be detected consistently in every study cohort. Third, as the population size of this study is not sufficiently large, it cannot be completely ruled out that some variants with impacts may not have obtained statistical significance.
We found significant associations between STK39 variants and cardiovascular risk factors other than BP. They include glucose, total cholesterol, and LDL-C in rs3754777; and waist circumference, triglyceride, and HDL-C in rs6749447. Four of the factors belong to the characteristics of metabolic syndrome. The minor allele carriers of rs3754777 had the tendencies to have lower levels of risk factors. Those of rs6749447 showed contradictory results on waist circumference and triglyceride and HDL-C. Thus, it is difficult to tell what clinical association the genotype of the latter STK39 SNP may finally have. However, to our knowledge, this study is the first to demonstrate the association between STK39 variants and the above factors. In a prior study by Wang et al.,1) it was mentioned that STK39 SNPs were modestly associated with blood glucose level, insulin response to glucose, and triglyceride level in a subset of Amish population. In addition, two other STK39 SNPs were reported to be linked to multiple phenotypes of metabolic syndrome.10) In the present study, we have shown the relationship between STK39 SNPs and cardiovascular risk factors more systemically. It has been known that STK39 was located in an area in which BP, obesity, and diabetes-related rodent quantitative trait loci have been mapped. Furthermore, STK39/SPAK is able to activate the p38 MAP kinase pathway, providing evidence that it can act as a stress-mediated signals.11),12) It has been recently demonstrated that p38 MAP kinase plays a role in glucose13) and lipoprotein metabolism,14) and this may support the biological mechanism of the current data. Although investigating the functional mechanism of STK39 is beyond the scope of this study, further projects focusing on this issue may unveil the role of this gene on multiple cardiovascular risk factors.
In this study, the influence of STK39 variants on the risk factors was clearer in women. This finding is in accordance with prior studies that have shown gender-dependency of STK39 effect. In the study by Fava et al.,3) the association of STK39 rs35929607 variant and hypertension was evident only in women. However, in the study by Chen et al.,4) STK39 rs6433027 and rs3754777 had more significant association with hypertension in male. Sex differences in hypertension may be attributed to multiple factors such as lifestyle, diet, and genetic polymorphism.15) Interestingly, it has been documented that SPAK expression is affected by both androgen and estrogen in human prostate cancer cells.16) Nevertheless, further studies are needed to clarify the underlying mechanism of gender dependency in STK39 effect on cardiovascular risk factors.
The present study has several limitations. Although rs3754777 and rs6749447 were the first variants known to be hypertension susceptible in STK39 gene, other SNPs have been reported to have effects thereafter. Inclusion of more STK39 variants in the study may have been helpful to understand the role of STK39 in this Asian population more completely. As mentioned above, the study population was not sufficiently large, and some important analyses did not obtain statistical significance. However, it was strength of the study to systemically analyze and present the association between STK39 variants and multiple cardiovascular risk factors.
In conclusion, the associations between two SNPs of STK39, rs3754777 and rs6749447, and hypertension were not significant in this Korean cohort. However, we identified that AA genotype of rs3754777 had lower glucose and cholesterol levels, especially in females. Genotype of rs6749447 was associated with waist circumference, triglyceride, and HDL-C levels in gender stratified analysis only. The genotype of rs6759447 was related to blood glucose levels. Further studies are needed to clarify the effect of STK39 variants in these cardiovascular risk factors.
Acknowledgments
This study was supported by a grant (2009) from the Korean Society of Cardiology and a faculty research grant of Yonsei University College of Medicine for 2012 (6-2012-0086).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Wang Y, O'Connell JR, McArdle PF, et al. From the Cover: whole-genome association study identifies STK39 as a hypertension susceptibility gene. Proc Natl Acad Sci U S A. 2009;106:226–231. doi: 10.1073/pnas.0808358106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delpire E, Gagnon KB. SPAK and OSR1: STE20 kinases involved in the regulation of ion homoeostasis and volume control in mammalian cells. Biochem J. 2008;409:321–331. doi: 10.1042/BJ20071324. [DOI] [PubMed] [Google Scholar]
- 3.Fava C, Danese E, Montagnana M, et al. Serine/threonine kinase 39 is a candidate gene for primary hypertension especially in women: results from two cohort studies in Swedes. J Hypertens. 2011;29:484–491. doi: 10.1097/HJH.0b013e328342b2c1. [DOI] [PubMed] [Google Scholar]
- 4.Chen LY, Zhao WH, Tian W, et al. STK39 is an independent risk factor for male hypertension in Han Chinese. Int J Cardiol. 2012;154:122–127. doi: 10.1016/j.ijcard.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Newton-Cheh C, Johnson T, Gateva V, et al. Genome-wide association study identifies eight loci associated with blood pressure. Nat Genet. 2009;41:666–676. doi: 10.1038/ng.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy D, Ehret GB, Rice K, et al. Genome-wide association study of blood pressure and hypertension. Nat Genet. 2009;41:677–687. doi: 10.1038/ng.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cunnington MS, Kay C, Avery PJ, Mayosi BM, Koref MS, Keavney B. STK39 polymorphisms and blood pressure: an association study in British Caucasians and assessment of cis-acting influences on gene expression. BMC Med Genet. 2009;10:135. doi: 10.1186/1471-2350-10-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niu WQ, Zhang Y, Ji KD, Gao PJ, Zhu DL. Contribution of five top whole-genome association signals to hypertension in Han Chinese. J Hum Hypertens. 2011;25:278–280. doi: 10.1038/jhh.2010.114. [DOI] [PubMed] [Google Scholar]
- 9.Rhee MY, Yang SJ, Oh SW, et al. Novel genetic variations associated with salt sensitivity in the Korean population. Hypertens Res. 2011;34:606–611. doi: 10.1038/hr.2010.278. [DOI] [PubMed] [Google Scholar]
- 10.Mooser V, Waterworth D, Song KJ, Yuan X, Knouff CW, inventors. GlaxoSmithKline Crop, assignee. Metabolic syndrome genetics. US 0203012 A1. United States patent US. 2009 Aug 13;
- 11.Johnston AM, Naselli G, Gonez LJ, Martin RM, Harrison LC, DeAizpurua HJ. SPAK, a STE20/SPS1-related kinase that activates the p38 pathway. Oncogene. 2000;19:4290–4297. doi: 10.1038/sj.onc.1203784. [DOI] [PubMed] [Google Scholar]
- 12.Piechotta K, Garbarini N, England R, Delpire E. Characterization of the interaction of the stress kinase SPAK with the Na+-K+-2Cl-cotransporter in the nervous system: evidence for a scaffolding role of the kinase. J Biol Chem. 2003;278:52848–52856. doi: 10.1074/jbc.M309436200. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Sun C, Zhou Y, et al. p38 MAPK-mediated regulation of Xbp1s is crucial for glucose homeostasis. Nat Med. 2011;17:1251–1260. doi: 10.1038/nm.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kushiyama A, Shojima N, Ogihara T, et al. Resistin-like molecule beta activates MAPKs, suppresses insulin signaling in hepatocytes, and induces diabetes, hyperlipidemia, and fatty liver in transgenic mice on a high fat diet. J Biol Chem. 2005;280:42016–42025. doi: 10.1074/jbc.M503065200. [DOI] [PubMed] [Google Scholar]
- 15.Ruixing Y, Jinzhen W, Shangling P, Weixiong L, Dezhai Y, Yuming C. Sex differences in environmental and genetic factors for hypertension. Am J Med. 2008;121:811–819. doi: 10.1016/j.amjmed.2008.04.026. [DOI] [PubMed] [Google Scholar]
- 16.Qi H, Labrie Y, Grenier J, Fournier A, Fillion C, Labrie C. Androgens induce expression of SPAK, a STE20/SPS1-related kinase, in LNCaP human prostate cancer cells. Mol Cell Endocrinol. 2001;182:181–192. doi: 10.1016/s0303-7207(01)00560-3. [DOI] [PubMed] [Google Scholar]


