Abstract
Objectives
To determine whether body mass index (BMI) at the time of hospitalization or weight change in the period immediately following hospitalization predict physical function in the year after hip fracture.
Design
Prospective observational study.
Setting
Two hospitals in Baltimore, Maryland.
Participants
Female hip fracture patients age 65 years or older (N=136 for BMI analysis, N=41 for analysis of weight change).
Measurements
Body mass index was calculated based on weight and height from the medical chart. Weight change was based on DXA scans at 3 and 10 days post fracture. Physical function was assessed at 2, 6 and 12 months following fracture using the Lower Extremity Gain Scale (LEGS), walking speed and grip strength.
Results
LEGS score and walking speed did not differ across BMI tertiles. However, grip strength differed significantly across BMI tertiles (p=0.029), with underweight women having lower grip strength than normal weight women at all time points. Women experiencing the most weight loss (>4.8%) had significantly lower LEGS scores at all time points, slower walking speed at 6 months, and weaker grip strength at 12 months post-fracture relative to women with more modest weight loss. In adjusted models, overall differences in function and functional change across all time points were not significant. However, at 12 months post fracture, women with the most weight loss had an average grip strength 7.0kg lower than women with modest weight loss (p=0.030).
Conclusions
Adjustment for confounders accounts for much of the relationships between BMI and function and weight change and function in the year after fracture. However, weight loss is associated with weakness during hip fracture recovery. Weight loss during and immediately after hospitalization appears to identify women at risk of poor function and may represent an important target for future interventions.
Keywords: Hospitalization, hip fracture, disability, strength, weight loss
Introduction
Overweight and obesity are associated with increased risk of developing disability in older adults (1, 2). However, little is known about the relationship between body mass index (BMI) and physical function after hospitalization, and the health effects of excess BMI may differ in this context. For example, obesity is associated with reduced post-hospitalization mortality for cardiac admissions (3–5) and reduced risk for some complications of hospitalization, such as pressure ulcers (6). Hospitalization is also associated with weight loss (7–9). Although weight loss is an important predictor of disability, little research has examined the association between weight change and function after hospitalization (10).
The purpose of this study is to examine the association between weight and physical function in older women hospitalized for a hip fracture using two different measures of weight. Specifically, this study examines how BMI at the time of hospitalization and weight change occurring during and after hospitalization effect function in the year following hip fracture. This research extends prior work in three ways. First, although research has emphasized lean mass declines following fracture (11), little research has examined total weight. Weight may be more amenable for use as an intervention target in clinical practice, because it can be measured easily in the hospital or outpatient setting. Second, little research has examined the effects of weight change in the period immediately after hip fracture. This is particularly important because the changes in body composition are greatest in the first two months after fracture (12). Third, few studies have addressed the association between BMI and physical performance longitudinally after hospitalization (13).
Methods
Data
Participants for the third Baltimore Hip Study, a prospective study of hip fracture recovery, were recruited from two area hospitals from 1992–1995. Participants were recruited within 48 hours of admission and included 205 Caucasian women age 65 years or older with a new hip fracture of the proximal femur. Participants were evaluated at 3 and/or 10 days after hospital admission and at 2, 6 and 12 months later (12). When possible, assessments were conducted at both 3 and 10 days. However, because of the instability of patient health during the immediate post-fracture period, many participants did not participate in both assessments.
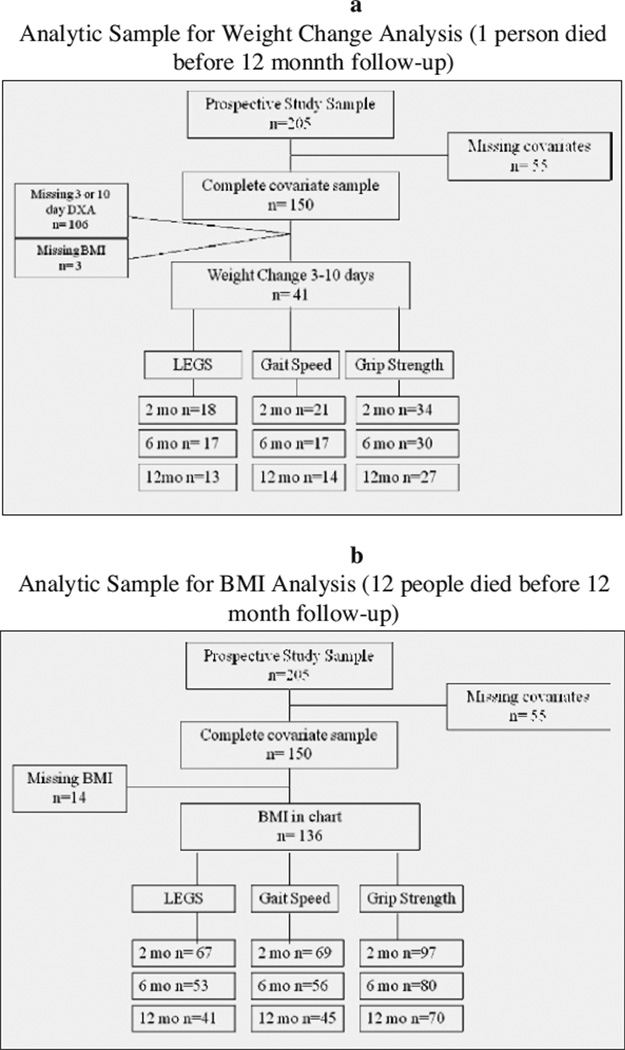
The analytic sample for BMI analysis included 136 participants with complete covariate data and a record of BMI at hospital admission. The analytic sample for weight change analysis included 41 participants with complete covariate data and a DXA scan at 3 and 10 days post-fracture (Figure 1). Women who were excluded from the BMI sample due to missing data (N=69) were older and had longer lengths of hospital stay, higher anesthesia scores, and lower cognitive scores compared to the remaining sample, but did not differ in terms of co-morbidities, smoking status or pre-fracture difficulty with lower extremity activities of daily living. Women who were excluded from the analytic sample for weight change due to missing data (N=164) had a longer length of stay but did not differ with regard to age, co-morbidities, anesthesia score, smoking status, cognitive function, or pre-fracture disability.
Figure 1.
Measures
Physical function was assessed at 2, 6 and 12 months following fracture. The Lower Extremity Gain Scale (LEGS) is a performance-based measure of function for use in hip fracture patients (14, 15). The LEGS includes timed performance on nine tasks scored from 0 to 4. Higher scores represent better performance (summary range: 0–36). Participants unable to complete a task are assigned a score of 0 for that task. Walking speed was measured by timing participants walking three meters at their usual pace. Maximum grip strength was measured using a hand-held dynamometer (Jamar, Clifton NJ).
BMI (kg/m2) was calculated using height and weight recorded in the medical record at hospital admission. Weight change between 3 and 10 days after admission was measured based on total body mass from DXA.
Age, number of co-morbidities, anesthesia score, length of hospitalization and number of post-operative complications were abstracted from the medical record. Number of co-morbidities was summed across eight conditions: osteoarthritis, coronary heart disease, congestive heart failure, stroke, dementia, diabetes, chronic obstructive pulmonary disease and peripheral vascular disease (16). The American Society of Anesthesiologists (ASA) rating of operative risk was used as a proxy for severity of health problems at hospital admission (17, 18). Number of post operative-complications was summed across twenty nine complications (e.g., pressure sores, infection, anemia).
Pre-fracture function, current smoking status, and cognition were assessed through patient interviews conducted at the 3 or 10 day visit. Pre-fracture function was measured as the number of limitations with 11 activities of daily living requiring lower extremity function (LE-ADLs) (19). Smoking status was assessed based on self-report of current smoking. Cognition was assessed using the Mini Mental State Exam (20).
Analysis
Differences in baseline characteristics were compared across tertiles of BMI and percent weight change using ANOVA and Fisher’s exact tests. To assess the effects of BMI and percent weight change on strength and function during the 12 months following hip fracture, mixed effect models were fit predicting each outcome based on BMI or weight change tertiles, with the middle tertile serving as the referent group. Models were fit by maximum likelihood estimation, allowing the use of outcome data for all individuals with at least one observation. Models were adjusted for covariates significantly associated with the outcome at 12 months. All analyses were conducted using STATA-V9.
Results
Characteristics of the BMI and weight change study samples are described in Table 1. Tertiles of BMI were generally consistent with standard classification (21): underweight (BMI<20.5), normal weight (BMI 20.5–24.0), and overweight or obese (BMI> 24.6). Only age (p=0.003) and percent weight loss (p=0.037) differed significantly across BMI groups. Tertiles of percent weight change reflect women who experienced the greatest weight loss (4.8–10.4%), modest weight loss (0.4–4.3%), and who remained weight stable (weight loss <0.5% to gaining 4.8%). Only ASA rating (p=0.004) differed significantly across weight change groups.
Table 1.
Study Sample Characteristics: Mean (SD) or %
| BMI (n= 136) Tertiles n, (range, kg/m2) |
Percent Weight Change (n=41) Tertiles n, (range, %) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Low (14.8, 20.5) |
Med (20.5, 24.0) |
High (24.6, 33.2) |
P value* | Low (−10.4, −4.8) |
Med (−4.3, −0.4) |
High (−0.3, 4.8) |
P value* | |
| Age at admission, mean y (SD) | 82.5 (7.8) | 77.2 (5.9) | 80.0 (7.8) | 0.003 | 81.4 (8.3) | 80.6 (8.2) | 78.0 (7.7) | 0.503 |
| Co-morbidities, mean (SD) (0–8) |
1.7 (1.2) | 1.4 (1.4) | 1.5 (1.4) | 0.716 | 1.3 (1.3) | 1.5 (1.6) | 1.4 (1.3) | 0.921 |
| Anesthesiologist Risk Rating, mean (SD) (0–4) |
2.7 (0.58) | 2.6 (0.62) | 2.4 (0.58) | 0.094 | 2.9 (0.46) | 2.4 (0.51) | 2.3 (0.61) | 0.004 |
| % Smokers | 21.7 | 11.1 | 11.1 | 0.254 | 13.3 | 0 | 14.3 | 0.319 |
| Length of Stay, mean # of days (SD) (2–38) |
8.4 (4.5) | 7.0 (3.1) | 7.1 (2.4) | 0.102 | 9.0 (6.2) | 5.8 (1.8) | 6.0 (1.7) | 0.052 |
| Cognition, mean MMSE score, (SD) (0–30) |
24.5 (4.5) | 25.5 (3.7) | 25.8 (3.9) | 0.288 | 24.1 (4.2) | 25.5 (6.4) | 25.5 (3.3) | 0.658 |
| Pre-fracture LE-ADL score, mean (SD) (0–12) |
4.5 (3.4) | 3.8 (2.9) | 4.3 (3.1) | 0.525 | 5.7 (3.6) | 3.2 (2.8) | 4.8 (3.2) | 0.126 |
| BMI, mean (SD) | 18.3 (1.6) | 22.5 (1.1) | 27.7 (2.5) | <0.001 | 20.5 (4.6) | 23.5 (3.8) | 22.5 (3.2) | 0.137 |
| % Weight Change 3–10 days, mean, (SD) n=44 |
−4.6 (3.6) | −1.3 (3.6) | −2.7 (2.7) | 0.037 | −6.7 (1.7) | −2.7 (1.1) | 1.3 (1.4) | <0.001 |
| Number of Post Operative Complications, mean (SD) (0–29) |
1.0 (1.1) | 1.0 (1.2) | 0.8 (1.1) | 0.811 | 1.5 (1.4) | 0.7 (0.9) | 0.6 (0.8) | 0.067 |
MMSE- Mini Mental State Exam; LE-ADL- Lower Extremity Activities of Daily Living; BMI- Body Mass Index;
p value compares differences across tertiles of BMI and weight change
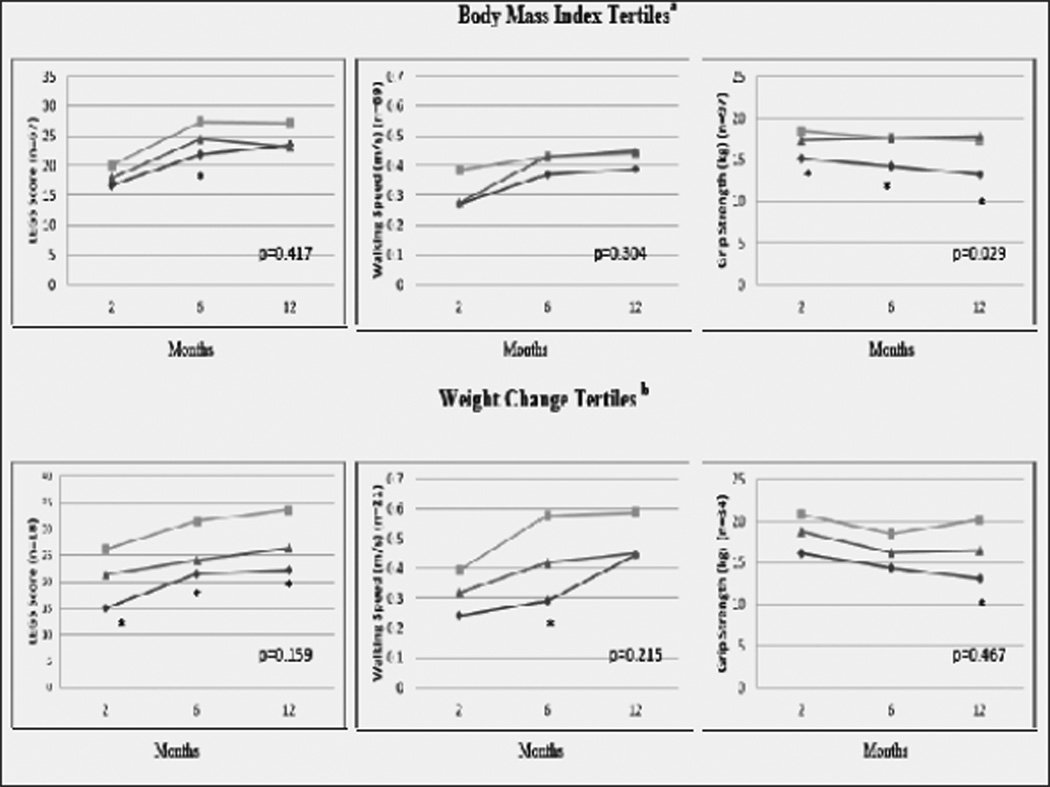
Figure 2 illustrates unadjusted trajectories in LEGS score, walking speed and grip strength by tertile of BMI and percent weight change. LEGS score and walking speed trajectories did not differ across BMI tertiles. However, grip strength trajectories were significantly different (p=0.029), with underweight women having lower grip strength than normal weight women at all time points. Women experiencing the greatest weight loss (>4.8%) had significantly lower LEGS scores at all time points, slower walking speed at 6 months, and weaker grip strength at 12 months post-fracture relative to women with modest weight loss.
Figure 2.
Physical Function at 2, 6, and 12 months following hip fracture by tertiles of body mass index and weight change
The p value displayed on graphs represents the statistical test that all differences between all three trajectories=0; *p<0.05 for the difference between low and medium tertiles; LEGS=Lower Extremity Gain Scalea. Low tertile (14.8, 20.5 kg/m2), Med tertile (20.5, 24.0 kg/m2), High tertile (24.6, 33.2 kg/m2); b. Low tertile (−10.4, −4.8%); Med tertile (−4.3, −0.4%), High tertile (−0.3, 4.8%)
Table 2 provides the adjusted change in LEGS score, walking speed and grip strength between 2 and 12 months post-fracture across tertiles of BMI and weight change. In adjusted models, rates of change between 2 and 12 months did not differ across tertiles of BMI or weight change. However, differences in grip strength across tertiles of weight change at 12 months post-fracture remained significant. Women with the greatest weight loss had an average grip strength 7.0kg lower than women with modest weight loss (p=0.030) 12 months post-fracture.
Table 2.
Differences in Physical Function between 2 and 12 Months Following Hip Fracture by Tertile of BMI and Weight Change
| LEGSa | Walking Speedb | Grip Strengthc | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2m | 12m | Change | p | 2m | 12m | Change | p | 2m | 12m | Change | p | |
| BMId | n=67 | n=69 | n=97 | |||||||||
| 0.383f | 0.466f | 0.307f | ||||||||||
| Low | 16.75 | 23.41 | 6.66 | 0.784 | 0.31 | 0.43 | 0.12 | 0.476 | 15.99 | 14.11 | −1.88 | 0.560 |
| Med | 18.75 | 26.11 | 7.36 | - | 0.31 | 0.40 | 0.09 | 17.85 | 16.77 | −1.08 | - | |
| High | 19.21 | 24.62 | 5.41 | 0.334 | 0.29 | 0.46 | 0.17 | 0.072 | 17.23 | 17.67 | 0.44 | 0.275 |
|
Weight Changee |
n=18 | n=21 | n=34 | |||||||||
| 0.921f | 0.236f | 0.498f | ||||||||||
| Low | 20.83 | 27.09 | 6.26 | 0.787 | 0.28 | 0.47 | 0.19 | 0.991 | 16.13 | 13.09g | −3.04 | 0.478 |
| Med | 23.34 | 30.63 | 7.29 | - | 0.38 | 0.57 | 0.19 | 20.70 | 20.09 | −0.61 | - | |
| High | 21.82 | 27.05 | 5.23 | 0.582 | 0.32 | 0.46 | 0.14 | 0.637 | 18.71 | 16.50 | −2.21 | 0.622 |
BMI models adjusted for LEADLs, and number of post operative complications; weight change models adjusted for BMI, ASA score, LEADLs, and complications;
BMI models adjusted for age, comorbidities, length of stay, MMSE score and LEADLs; weight change models adjusted for BMI, age, comorbidities and LEADLs;
BMI models adjusted for age, smoking status, MMSE score, LEADLs, and complications; weight change models adjusted for BMI and MMSE score;
Low tertile (14.8, 20.5 kg/m2), Med tertile (20.5, 24.0 kg/m2), High tertile (24.6, 33.2 kg/m2);
Low tertile (−10.4, −4.8%); Med tertile (−4.3, −0.4%), High tertile (−0.3, 4.8%);
The p value representing the statistical test that differences between all three trajectories=0. All other p values represent the difference between low and medium or high and medium tertile in the change in function between 2 and 12 months;
Time specific difference is significantly different from medium tertile (p<0.05)
Additional sensitivity analysis compared tertiles based on absolute weight change, rather than percent weight change. Results were similar. Generally, the estimated differences between BMI and weight change groups were greater, suggesting that the main analysis, using relative weight change, represents a conservative approach to estimating the effect of weight change on function.
Discussion
In this study of older women hospitalized for a hip fracture, women who were underweight (<20.5kg/m2) or experienced the greatest weight loss (>4.8%) had worse physical function and strength in the 12 months after fracture relative to women who were normal weight or who experienced modest weight loss. Adjusting for confounders accounted for differences in lower extremity function, walking speed, and grip strength.
Importantly, although we found no differences in the rate of change in functional outcomes during hip fracture recovery, the associations between weight change and grip strength remained significant 12 months following fracture even after adjustment for confounders. This suggests that weight change does not impact the rate of recovery or strength decline, per se, but does predict level of strength during recovery. Women who lost the most weight had an average grip strength 7kg lower than women who lost less weight (p=0.030). Hand grip strength is predictive of disability in older adults and is highly correlated with motor function after hip fracture (22, 23). Weight loss in the period during and after hospitalization may be a risk factor for poor strength in the year following a fracture or may be an indicator of underlying frailty or cachexia.
Although we did not directly compare these two measures because of differences in the study sample available for each, results provide some evidence that differences in strength and function were greater across tertiles of percent weight change than across tertiles of BMI. This suggests that weight loss during and immediately following hospitalization may be a stronger predictor of post-hip fracture function than BMI. Interestingly, relative to their starting weight, underweight women lost the most weight (4.6% versus 1.3% in normal weight and 2.7% in overweight women), suggesting they are at higher risk of adverse outcomes as a result of weight loss and might be considered a potential target for interventions aimed at reducing weight loss during hospitalization.
There were no differences in high compared with medium tertiles. While excess weight has been associated with disability in older adults, overweight women in this study did not perform worse on measures of lower extremity function and walking speed and were no weaker than women of normal weight 12 months following fracture, suggesting these women are not at increased risk of disability in the year after hospitalization for fracture.
Our study builds on previous research by examining the effects of weight change in the period during and after hospitalization. Only a few studies have quantified weight change associated with hospitalization (8, 9). The majority of research on the health effects of weight in acute settings has focused on measures of malnutrition (30–32). Strengths of this study include repeated measures of objective physical function in the year following hip fractures, as well as the availability of BMI ascertained at hospital admission and weight change in the period immediately after fracture.
This study also has limitations. First, primary analysis was limited to subjects with complete data, and only a small number of women received a DXA scan at 3 and 10 days post-fracture. However, in multivariate models none of the covariates predicted the likelihood of being observed, suggesting little sampling bias based on these characteristics. Second, if weight loss occurs during the first three days of hospitalization, weight change based on DXA at 3 days may underestimate percent change since injury. Weight change may have also been influenced by swelling or edema in the fractured leg. However, results were similar in sensitivity analyses correcting for edema. Third, statistical power was limited by our small sample size. Fourth, mortality varied by BMI and was greatest in the underweight group, which could result in an underestimation of the association between underweight and function. Fifth, DXA provides a more accurate measure of weight than self- reported weight, and the use of multiple measures of DXA may reduce measurement error. These measurement differences could contribute to differences in the strength of the association between weight and function across different measures (i.e., DXA-assessed weight change versus BMI from self-reported weight). Finally, length of hospital stay for hip fracture has declined since the time this study was conducted, and it is unclear how this might impact results.
In summary, although both high and low BMI have been associated with poorer function in community-based studies of older adults, we find that the association between weight and function differs in an acute setting. In women with hip fracture, both low BMI and weight loss were associated with poor function after fracture, but these relationships were largely accounted for by adjustment for covariates. We did find some evidence that weight loss occurring during and after hospitalization predicts weakness in the year following discharge. Weight loss may identify women at risk of poor function post-fracture and may represent an important target for future interventions.
Acknowledgments
Funding Source(s): Dr. Alley was supported by grant K12 HD043489, and Dr. Miller was supported by grant K23 AG019161 from the National Institutes of Health. Baltimore Hip Studies data collection and analytic work was supported by grant R37 AG09901 and P30 AG028747 from the National Institutes of Health.
Footnotes
Conflict of Interest Statement: L. Reider, W. Hawkes, J.R. Hebel, C. D’Adamo, D. Orwig, and D. Alley have no conflicts of interest to report. Dr. Miller is a full time employee of GlaxoSmithKline. Dr. Magaziner has provided academic consulting for Amgen, Eli Lilly and Sanofi Aventis, and served on advisory boards for Amgen, GlaxoSmithKline, Novartis, and Eli Lilly and received grants from Merck, Eli Lilly and Novartis. All of these companies have approved products or products in development intended to improve outcomes from hip fracture and/or other musculoskeletal conditions.
References
- 1.Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010 Aug;11(8):568–579. doi: 10.1111/j.1467-789X.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- 2.Stenholm S, Alley D, Bandinelli S, et al. The effect of obesity combined with low muscle strength on decline in mobility in older persons: Results from the InCHIANTI study. Int J Obes (Lond) 2009 Jun;33(6):635–644. doi: 10.1038/ijo.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eisenstein EL, McGuire DK, Bhapkar MV, et al. Elevated body mass index and intermediate-term clinical outcomes after acute coronary syndromes. Am J Med. 2005 Sep;118(9):981–990. doi: 10.1016/j.amjmed.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 4.Nigam A, Wright RS, Allison TG, et al. Excess weight at time of presentation of myocardial infarction is associated with lower initial mortality risks but higher long-term risks including recurrent re-infarction and cardiac death. Int J Cardiol. 2006 Jun 16;110(2):153–159. doi: 10.1016/j.ijcard.2005.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Lopez-Jimenez F, Wu CO, Tian X, et al. Weight change after myocardial infarction--the enhancing recovery in coronary heart disease patients (ENRICHD) experience. Am Heart J. 2008 Mar;155(3):478–484. doi: 10.1016/j.ahj.2007.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Compher C, Kinosian BP, Ratcliffe SJ, et al. Obesity reduces the risk of pressure ulcers in elderly hospitalized patients. J Gerontol A Biol Sci Med Sci. 2007 Nov;62(11):1310–1312. doi: 10.1093/gerona/62.11.1310. [DOI] [PubMed] [Google Scholar]
- 7.Newman AB, Yanez D, Harris T, et al. Weight change in old age and its association with mortality. J Am Geriatr Soc. 2001 Oct;49(10):1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- 8.McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ. 1994 Apr 9;308(6934):945–948. doi: 10.1136/bmj.308.6934.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alley DE, Koster A, Mackey D, et al. Hospitalization and change in body composition and strength in a population-based cohort of older persons. J Am Geriatr Soc. 2010 Nov;58(11):2085–2091. doi: 10.1111/j.1532-5415.2010.03144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gill TM, Gahbauer EA, Han L, et al. Factors associated with recovery of prehospital function among older persons admitted to a nursing home with disability after an acute hospitalization. J Gerontol A Biol Sci Med Sci. 2009 Dec;64(12):1296–1303. doi: 10.1093/gerona/glp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Visser M, Harris TB, Fox KM, et al. Change in muscle mass and muscle strength after a hip fracture: Relationship to mobility recovery. J Gerontol A Biol Sci Med Sci. 2000 Aug;55(8):M434–M440. doi: 10.1093/gerona/55.8.m434. [DOI] [PubMed] [Google Scholar]
- 12.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11(1):31–35. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 13.Di Monaco M, Vallero F, Di Monaco R, et al. Body mass index and functional recovery after hip fracture: A survey study of 510 women. Aging Clin Exp Res. 2006 Feb;18(1):57–62. doi: 10.1007/BF03324641. [DOI] [PubMed] [Google Scholar]
- 14.Zimmerman S, Hawkes WG, Hebel JR, et al. The lower extremity gain scale: A performance-based measure to assess recovery after hip fracture. Arch Phys Med Rehabil. 2006 Mar;87(3):430–436. doi: 10.1016/j.apmr.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 15.Hawkes WG, Williams GR, Zimmerman S, et al. A clinically meaningful difference was generated for a performance measure of recovery from hip fracture. J Clin Epidemiol. 2004 Oct;57(10):1019–1024. doi: 10.1016/j.jclinepi.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Miller RR, Zhang Y, Silliman RA, et al. Effect of medical conditions on improvement in self-reported and observed functional performance of elders. J Am Geriatr Soc. 2004 Feb;52(2):217–223. doi: 10.1046/j.0002-8614.2004.52057.x. [DOI] [PubMed] [Google Scholar]
- 17.Feng M, Zhang J, Shen H, et al. Predictors of prognosis for elderly patients with poststroke hemiplegia experiencing hip fractures. Clin Orthop Relat Res. 2009 Nov;467(11):2970–2978. doi: 10.1007/s11999-009-0835-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michel JP, Klopfenstein C, Hoffmeyer P, et al. Hip fracture surgery: Is the pre-operative american society of anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res. 2002 Oct;14(5):389–394. doi: 10.1007/BF03324467. [DOI] [PubMed] [Google Scholar]
- 19.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000 Sep;55(9):M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21. [Last accessed 4/11/2012];Global database on body mass index: BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 22.Rantanen T, Guralnik JM, Foley D, et al. Midlife hand grip strength as a predictor of old age disability. JAMA. 1999 Feb 10;281(6):558–560. doi: 10.1001/jama.281.6.558. [DOI] [PubMed] [Google Scholar]
- 23.Beloosesky Y, Weiss A, Manasian M, et al. Handgrip strength of the elderly after hip fracture repair correlates with functional outcome. Disabil Rehabil. 2010;32(5):367–373. doi: 10.3109/09638280903168499. [DOI] [PubMed] [Google Scholar]
- 24.Feldblum I, German L, Castel H, et al. Individualized nutritional intervention during and after hospitalization: The nutrition intervention study clinical trial. J Am Geriatr Soc. 2010 Nov 18; doi: 10.1111/j.1532-5415.2010.03174.x. [DOI] [PubMed] [Google Scholar]
- 25.Boudville A, Bruce DG. Lack of meal intake compensation following nutritional supplements in hospitalised elderly women. Br J Nutr. 2005 Jun;93(6):879–884. doi: 10.1079/bjn20041359. [DOI] [PubMed] [Google Scholar]
- 26.Carlsson P, Tidermark J, Ponzer S, et al. Food habits and appetite of elderly women at the time of a femoral neck fracture and after nutritional and anabolic support. J Hum Nutr Diet. 2005 Apr;18(2):117–120. doi: 10.1111/j.1365-277X.2005.00594.x. [DOI] [PubMed] [Google Scholar]
- 27.Gill TM, Allore H, Guo Z. The deleterious effects of bed rest among community-living older persons. J Gerontol A Biol Sci Med Sci. 2004 Jul;59(7):755–761. doi: 10.1093/gerona/59.7.m755. [DOI] [PubMed] [Google Scholar]
- 28.Siebens H, Aronow H, Edwards D, et al. A randomized controlled trial of exercise to improve outcomes of acute hospitalization in older adults. J Am Geriatr Soc. 2000 Dec;48(12):1545–1552. doi: 10.1111/j.1532-5415.2000.tb03862.x. [DOI] [PubMed] [Google Scholar]
- 29.Nolan J, Thomas S. Targeted individual exercise programmes for older medical patients are feasible, and may change hospital and patient outcomes: A service improvement project. BMC Health Serv Res. 2008 Dec 10;8:250. doi: 10.1186/1472-6963-8-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Nes MC, Herrmann FR, Gold G, et al. Does the mini nutritional assessment predict hospitalization outcomes in older people? Age Ageing. 2001 May;30(3):221–226. doi: 10.1093/ageing/30.3.221. [DOI] [PubMed] [Google Scholar]
- 31.Covinsky KE, Martin GE, Beyth RJ, et al. The relationship between clinical assessments of nutritional status and adverse outcomes in older hospitalized medical patients. J Am Geriatr Soc. 1999 May;47(5):532–538. doi: 10.1111/j.1532-5415.1999.tb02566.x. [DOI] [PubMed] [Google Scholar]
- 32.Braunschweig C, Gomez S, Sheean PM. Impact of declines in nutritional status on outcomes in adult patients hospitalized for more than 7 days. J Am Diet Assoc. 2000 Nov;100(11) doi: 10.1016/S0002-8223(00)00373-4. 1316,22; quiz 1323-4. [DOI] [PubMed] [Google Scholar]