Abstract
Background
Abetalipoproteinemia is a rare disorder of fat absorption, characterized by vitamin deficiency, acanthocytosis, and neurologic symptoms including ataxia and tremor.
Case Report
A 41-year-old male with abetalipoproteinemia is presented. He underwent staged bilateral thalamic deep brain stimulation (DBS) for the treatment of his tremors. After DBS, the patient achieved significant improvements in his tremors, ataxia, and quality of life.
Discussion
Thalamic DBS proved to be both safe and efficacious in the management of ataxia and tremors in a patient with abetalipoproteinemia. This is the first report of DBS in abetalipoproteinemia in the literature.
Keywords: Deep brain stimulation, tremor, ataxia, abetalipoproteinemia
Introduction
Abetalipoproteinemia or Bassen–Kornzweig syndrome was first reported by Bassen and Kornzweig1 in 1950, when they observed the malformation of erythrocytes in a case of retinitis pigmentosa. The association of this syndrome with hypocholesterolemia was made in 1958 by Jampel and Falls.2 The term abetalipoproteinemia was coined by Salt et al.3 in 1960, when he noticed the absence of beta-lipoprotein in the serum of a patient with acanthocytosis and steatorrhea. The cause of abetalipoproteinemia is attributed to a mutation in the microsomal triglyceride transfer protein, whose large subunit is found on chromosome 4q22-24.4,5 This subunit forms a heterodimer with protein disulfide isomerase, and the complex facilitates the transfer of lipids onto apolipoprotein B.6,7 The net result of this is the absence of apolipoprotein B-containing lipoproteins, such as chylomicrons, very-low-density lipoproteins, and low-density lipoprotein. The absorption of fat and fat-soluble vitamins is deficient, resulting in vitamin E deficiency, which leads to many of the neurologic sequelae including retinal degeneration, hyporeflexia, reduced proprioceptive and vibratory sense, and ataxia. Tremor, although not a classic feature of the disease, has also been reported in the literature, but as a rest tremor.8 We report on a case of a 41-year-old male with abetalipoproteinemia and a family history of tremors, who underwent staged bilateral thalamic deep brain stimulation (DBS) for tremors and ataxia, with significant improvement.
Case report
The patient is a 41-year-old right-handed male who developed a voice tremor around the age of 15, followed soon thereafter by axial tremors that impaired his walking, and then bilateral upper extremity tremors. He had a family history of tremors, including a maternal aunt and cousin with “hunchback” and tremors of an unspecified type, and a mother with “thumb tremors”. None of the affected family members was examined, and the nature of the tremors could thus not be assessed; however, no family members had a diagnosis of abetalipoproteinemia. At age 17, he was diagnosed with abetalipoproteinemia, based on clinical phenomenology and an extensive work-up; pertinent findings included a cholesterol of 49 mg/dl (150–300), elevated liver function tests, and creatine phosphokinase = 759 U/liter (1–50), 85% acanthocytes on peripheral smear, 72-hour fecal fat collection on high-fat diet resulting in diarrhea and 19% dietary fat malabsorbed, vitamin E level of 1.8 (5.5–18), a mild sensorimotor neuropathy on electromyography (EMG), and normal amino acid and lysosomal battery. A written report in the records documented that he was “homozygous for abetalipoproteinemia”, but the family was unable to locate any corroborating genetic report. He was subsequently started on treatment with vitamin E. His tremors and ataxia, which had progressed rapidly to that point, stabilized, but left him with significant disability. EMG and accelerometry recording to assess physiological properties of the tremor demonstrated a 3–4 Hz tremor of the head that was alcohol-responsive, and an intention cerebellar tremor of the extremities not responsive to alcohol. The patient reported mild tremor relief with alcohol but trials of sodium oxybate (up to 9 mg/day), propranolol (up to 240 mg/day), gabapentin (900 mg/day), and clonazepam and primidone (maximum doses not recalled by patient but both limited by sedation) provided minimal benefit. At the time of presentation to our center, he was taking sodium oxybate 2.25 q.i.d., propranolol 120 mg extended release, and vitamin E. His neurologic examination was significant for hyporeflexia, diminished distal vibration and joint position sense, dysmetria on finger–nose testing, tremulous speech with lack of prosody, a prominent bilateral action tremor that was present with sustention and in the wing position but was maximal with finger–nose testing, a “no–no” type head tremor, and marked axial tremor characterized by oscillatory swaying of the torso, neck, and head that was particularly disabling upon standing and severe enough to necessitate a wide base and holding on to walls to prevent falling. The combination of hand tremors and ataxia was such that he was unable to hold a cup with one hand without spilling at least half the contents, and spilled almost the entirety on bringing it to his mouth. His handwriting was illegible due to a combination of ataxia and tremor and spirals demonstrated a prominent axis (Figure 1). His gait was wide-based and affected by the axial tremors with a subtle dystonic element characterized by turning in of the right leg. Magnetic resonance imaging (MRI) of the brain with contrast was within normal limits. Given the atypical nature of the tremors, the prominent ataxia and the relatively static course since beginning vitamin E, it was felt that the abetalipoproteinemia was the significant source of his impairment. After detailed discussions with the patient regarding the role of thalamic DBS for refractory tremor, the decision was made to pursue this as a staged procedure, so as to better gauge the degree of benefit.
Figure 1. Spiral Drawings Before and After Initial Programming.
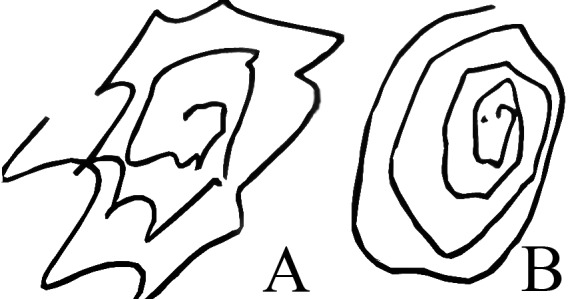
Spiral drawings before (A) and after (B) initial programming, demonstrating improvement in tremor with stimulation.
The patient underwent left followed by right DBS of the ventral intermediate (VIM) thalamus, 2 months apart. Since the patient was right-handed, the left side was done first. A Leksell stereotactic frame was fixed to the patient's head, and stereotactic non-contrast computed tomography (CT) was performed and then fused to a previously obtained contrast-enhanced MRI scan. The procedure was performed under local anesthesia, with microelectrode recording, with a combination of propofol and dexmeditomidine (Precedex) for sedation. The width of the third ventricle was 2.2 mm and the anterior commissure–posterior commissure (AC–PC) length was 27.4 mm. The initial VIM target was set at X = 11.0 mm lateral to the wall of the third ventricle, Y = 25% of the AC–PC length anterior to the PC, and Z = 0 (on the AC–PC line). Macrostimulation yielded improvement in spiral drawing and mild transient facial paresthesias, which led to implantation with Medtronic model 3387 electrodes slightly anterolateral to the initial target. Postoperative CT imaging fused to the preoperative MRI scan revealed the location of contact 0 to be 12.3 mm lateral to midline, 7.18 mm (26.4% * AC–PC) posterior to the midcommissural point, and 1.1 mm below the AC–PC plane. One week later, the patient underwent implantation of a Medtronic Soletra pulse generator. Initial programming revealed excellent tremor control, with the most ventral contact in monopolar stimulation but the presence of facial paresthesias at higher settings. This eventually led to employment of a bipolar configuration for optimal tremor control and tolerability.
At the follow-up visit, the patient reported significant improvements in his right upper extremity tremor. He was now able to drink and use a spoon. The head tremor remained unchanged. Given the patient's satisfaction, the decision was made to proceed with stimulation on the right hemisphere. The patient was operated on 2 months later for DBS of the right VIM, which was performed in a similar fashion to the contralateral side. Intraoperative macrostimulation at the predetermined target was limited by strong facial paresthesias that were found to be less prominent on a second, more lateral trajectory. The location of contact 0 on the right side was 12.3 mm lateral to midline, 6.9 mm (25% * ACPC) posterior to the midcommissural point, and 0.8 mm above the ACPC plane. As with the left DBS, initial programming revealed good tremor reduction with the two most ventral contacts, but a narrow therapeutic window before facial paresthesias and a perception of worsening balance emerged. A bipolar configuration provided good tolerability and tremor reduction.
At 8 months' follow-up, he demonstrated significant improvement in bilateral upper extremity tremors. He also experienced improvement in his axial tremors, although not as dramatic as was seen in the extremities. His gait, which had transiently worsened post-operatively, stabilized, and improved somewhat compared with baseline, as was also evidenced by comparing his ON vs. OFF-stimulation examination (see Video 1). The pre- and post-stimulation video was analyzed by a movement disorder specialist not involved with the case and blinded to stimulator status in regards to the clinical efficacy of stimulation. These assessments were made using the essential tremor rating assessment scale (TETRAS), rating head, right upper extremity, left upper extremity, standing and spiral (scored 1–4, with 1 being least severe), and the brief ataxia rating scale (BARS), scoring gait (scored 0–8, with 0 being normal), and left and right finger-to-nose (scored 0–4, with 0 being normal). These results are summarized in Table 1.
Table 1. Motor Rating Scales pre- and post- DBS.
| Pre-DBS | Post-DBS | |
| TETRAS | ||
| Head | 3 | 2 |
| Right upper extremity | 3 | 2 |
| Left upper extremity | 3 | 2 |
| Standing | 3 | 1 |
| Spiral | 3.5 | 1 |
| BARS | ||
| Right finger–nose | 3 | 1 |
| Left finger–nose | 4 | 1 |
| Gait | 4 | 2 |
Abbreviations: BARS, brief ataxia rating scale; DBS, deep brain stimulation; TETRAS, The Essential Tremor Rating Assessment Scale.
Video 1. Video Segment 1. Post-Operative Video of the Patient with Stimulation Off and Then On.
In a state of “OFF” stimulation there are significant extremity and axial tremors. With the stimulator “ON”, there are significant improvement in both the extremity and axial tremors, as well as gait.
He was weaned off sodium oxybate and reduced his propranolol dose by one-third. His stimulator settings were as follows: Left: 3+0-1-2-, 3.6 V, 90 μs, 145 Hz; Right: 3+0-1-2-, 3.6 V, 90 μs, 135 Hz.
Discussion
Thalamic DBS is a well-established modality for the treatment of refractory tremor and is currently approved for treatment of essential tremor and Parkinson's disease. Targeting the VIM thalamus for many different tremor types has been extensively reviewed in the literature.9–11 We are not aware, however, of any previously reported cases of DBS in the treatment of tremor associated with abetalipoproteinemia.
In this report, we present the case of a patient with a history of abetalipoproteinemia whose presenting symptom was axial and appendicular action tremor. The patient responded well to stimulation, with marked improvement of the appendicular component of the tremors, and moderate but appreciable improvement of the axial symptoms following bilateral VIM stimulation. Interestingly, rather high settings using multiple contacts were required. These settings could reflect the need to compensate for paresthesias found using monopolar stimulation. It is also possible, however, that more medial stimulation (as suggested by the presence of facial paresthesias) was a factor contributing to improvement of the midline tremors. We further hypothesize that the extensively involved somatotopy (axial and appendicular) required a wider field of stimulation. Given the unblinded nature of the report, the possibility of a placebo component cannot be excluded, but the dramatic improvement beyond 6 months and immediate return of symptom severity off stimulation noted on numerous assessments argues against this being a prominent confound. Evaluation of a pre- and post-stimulation video performed by a movement disorder specialist not involved in the case and blinded to stimulator status also supports the clinical efficacy of the intervention (Table 1).
Bilateral DBS of the VIM thalamus can be effective in the treatment of tremors associated with abetalipoproteinemia and should be considered in cases refractory to medications. This is the only report of DBS being used in abetalipoproteinemia. Further experience is necessary, but these results encourage consideration of DBS even when there is a component of concomitant ataxia.
Footnotes
Funding: None.
Financial Disclosures: Dr. Mogilner receives consulting fees and grant support from Medtronic Neurological; Dr. Mammis received fellowship grant support from Medtronic Neurological.
Conflict of Interest: The authors report no conflict of interest.
References
- 1.Bassen FA, Kornzweig AL. Malformation of the erythrocytes in a case of atypical retinitis pigmentosa. Blood. 1950;5:381–387. [PubMed] [Google Scholar]
- 2.Jampel RS, Falls HF. Atypical retinitis pigmentosa, acanthocytosis, and heredodegenerative neuromuscular disease. AMA Arch Ophthalmol. 1958;59:818–820. doi: 10.1001/archopht.1958.00940070032002. [DOI] [PubMed] [Google Scholar]
- 3.Salt HB, Wolff OH, Lloyd JK, Fosbrooke AS, Cameron AH, Hubble DV. On having no beta-lipoprotein. A syndrome comprising a-beta-lipoproteinaemia, acanthocytosis, and steatorrhoea. Lancet. 1960;2:325–329. doi: 10.1016/S0140-6736(60)91478-1. [DOI] [PubMed] [Google Scholar]
- 4.Shoulders CC, Brett DJ, Bayliss JD, et al. Abetalipoproteinemia is caused by defects of the gene encoding the 97 kDa subunit of a microsomal triglyceride transfer protein. Hum Mol Genet. 1993;2:2109–2116. doi: 10.1093/hmg/2.12.2109. [DOI] [PubMed] [Google Scholar]
- 5.Wetterau JR, Aggerbeck LP, Bouma ME, et al. Absence of microsomal triglyceride transfer protein in individuals with abetalipoproteinemia. Science. 1992;258:999–1001. doi: 10.1126/science.1439810. [DOI] [PubMed] [Google Scholar]
- 6.Narcisi TM, Shoulders CC, Chester SA, et al. Mutations of the microsomal triglyceride-transfer-protein gene in abetalipoproteinemia. Am J Hum Genet. 1995;57:1298–1310. [PMC free article] [PubMed] [Google Scholar]
- 7.Zamel R, Khan R, Pollex RL, Hegele RA. Abetalipoproteinemia: Two case reports and literature review. Orphanet J Rare Dis. 2008;3:19. doi: 10.1186/1750-1172-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soejima N, Ohyagi Y, Kikuchi H, Murai H, Shigeto H, Kira J. An adult case of probable Bassen-Kornzweig syndrome, presenting resting tremor. Rinsho Shinkeigaku. 2006;46:702–706. [PubMed] [Google Scholar]
- 9.Bronstein JM, Tagliati M, Alterman RL, et al. Deep brain stimulation for Parkinson Disease: An expert consensus and review of key issues. Arch Neurol. 2011;68:165. doi: 10.1001/archneurol.2010.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flora ED, Perera CL, Cameron AL, Maddern GJ. Deep brain stimulation for essential tremor: A systematic review. Mov Disord. 2010;25:1150–1559. doi: 10.1002/mds.23195. [DOI] [PubMed] [Google Scholar]
- 11.Torres CV, Moro E, Lopez-Rios AL, et al. Deep brain stimulation of the ventral intermediate nucleus of the thalamus for tremor in patients with multiple sclerosis. Neurosurgery. 2010;67:646–651. doi: 10.1227/01.NEU.0000375506.18902.3E. [DOI] [PubMed] [Google Scholar]


