Abstract
Objective
Evaluate the efficacy of phototherapy (PT) devices and the outcomes of extremely premature infants treated with those devices.
Study Design
This substudy of the National Institute of Child Health and Human Development Neonatal Research Network PT trial included 1404 infants treated with a single type of PT device during the first 24±12 h of treatment. The absolute (primary outcome) and relative decrease in total serum bilirubin (TSB) and other measures were evaluated. For infants treated with one PT type during the 2-week intervention period (n =1223), adjusted outcomes at discharge and 18 to 22 months corrected age were determined.
Result
In the first 24 h, the adjusted absolute (mean (±s.d.)) and relative (%) decrease in TSB (mg dl−1) were: light-emitting diodes (LEDs) −2.2 (±3), −22%; Spotlights −1.7 (±2), −19%; Banks −1.3 (±3), −8%; Blankets −0.8 (±3), −1%; (P<0.0002). Some findings at 18 to 22 months differed between groups.
Conclusion
LEDs achieved the greatest initial absolute reduction in TSB but were similar to Spots in the other performance measures. Long-term effects of PT devices in extremely premature infants deserve rigorous evaluation.
Keywords: extremely low birth weight, neonatal jaundice, neurodevelopmental outcome, phototherapy
Introduction
The first phototherapy (PT) device used fluorescent bulbs and was described in 1958.1 PT has long since become the primary therapy for hyperbilirubinemia in neonates. Current options for PT include conventional fluorescent lights (Banks), halogen spotlights (Spots), fiberoptic blankets (Blankets) and the relatively new blue light-emitting diode (LED) lights.2 The theoretical advantages of LED lights include a narrow light spectrum in the blue range, minimal heat production, power efficiency and low-maintenance requirements.3
Although these types of PT devices are used routinely in neonatal units around the world, there are relatively few studies in premature infants. A few small studies have compared the effectiveness of conventional PT with Blankets in premature infants.4–9 Comparisons of LEDs with other types of PT have been limited to small trials of term or preterm infants.10–13 For extremely low birth weight (ELBW) infants, very little is known about the efficacy of the various PT devices under ‘real world’ conditions or any effects on clinical outcomes. Important effects on later outcomes would be most likely seen in ELBW infants whose skin is relatively translucent and would allow deeper penetration of the PT lights.14
The National Institute of Child Health and Human Development (NICHD) Neonatal Research Network conducted a randomized trial comparing the use of aggressive PT with more conservative PT in ELBW infants.15 We used data from this trial to perform a prospective non-randomized comparison of the effectiveness of different PT devices in the ELBW population. Our primary outcome was the absolute decrease in total serum bilirubin (TSB) in the first 24 h of treatment. Secondary outcomes included length of PT, irradiance levels, proportion of infants whose TSB increased to within 2 mg dl−1 of the exchange transfusion criterion, the incidence of medical morbidities and adverse neurodevelopmental outcomes. Based on their theoretical advantages, we hypothesized that LEDs would produce the largest drop in TSB during the first 24 h of treatment. No specific hypotheses were formulated about other outcomes.
Methods
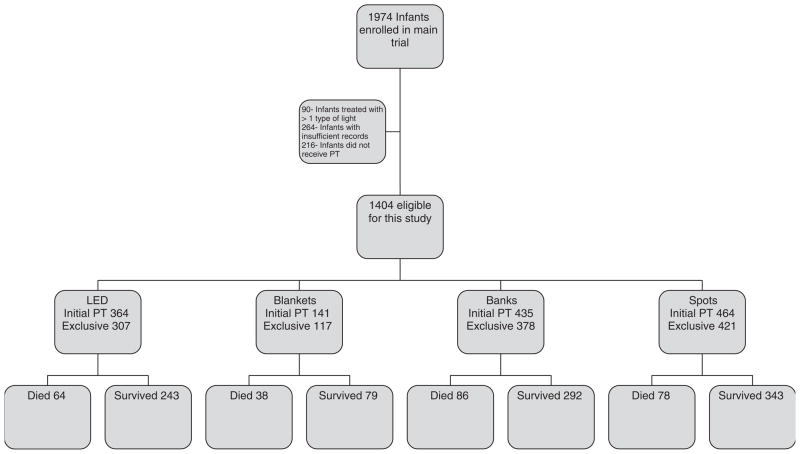
The Neonatal Research Network trial was approved by the Institutional Review Board of all the participating centers (see Appendix). Written informed consent was obtained for all infants (n =1974). Infants were stratified by birth weight (501 to 750 g and 751 to 1000 g) and center and then randomized to either aggressive or conservative PT. For this substudy, we excluded infants who were initially treated with more than one type of PT light (n =90), had type of PT-light information missing (n =264) or received no PT in the main trial (n =216). The remaining 1404 infants were included in evaluating the performance of the PT devices in the first 24±12 h. (Figure 1) Medical morbidities and neurodevelopmental outcomes were evaluated in the 1223 infants who were treated with only one type of PT during the 2-week intervention period.
Figure 1.
Enrollment, PT type and survival of study patients.
The absolute decrease in TSB in the first 24 h was selected as the primary outcome because it was considered the most direct measure of the efficacy of the PT device. The pretreatment TSB was mandatory in the first 200 infants enrolled in the PT trial but was subsequently optional because of concerns of excessive blood loss and refusal of consent by parents. Therefore, the TSB within 4 h before the initial start of PT was collected and then repeated within 24±12 h in 1142 of the infants. The mean absolute and relative change in TSB was calculated for each device group. We considered a decrease in TSB of >1.5 mg dl−1 to be clinically significant and calculated the proportion of infants attaining this in the first 24 h for each device group.
The criteria for starting PT, for performing an exchange transfusion and for stopping and restarting PT during the first 14 days were previously described.15 The medical staff selected the type of PT device. Any time PT was started it was continued for a minimum of 24 h. PT was intensified at TSB values of 11 mg dl−1 for infants 501 to 750 g and 13 mg dl−1 for infants 751 to 1000 g. The definition of ‘high TSB’ was predefined as a TSB within 2 mg dl−1 of the predetermined exchange transfusion criterion (≥11 mg dl−1 for 501 to 750 g infants and ≥13 mg dl−1 for 751 to 1000 g infants). By protocol, an exchange transfusion was indicated in both the treatment groups if the TSB exceeded the threshold values after 8 h of intensified treatment. Among all the infants in the main trial, two infants in the aggressive cohort and three infants in the conservative cohort received an exchange transfusion.
Devices were categorized as Banks, Blankets, Spots and LEDs. The irradiance levels were maintained between 15 and 40 μW cm−2 nm and were monitored by research nurses on weekdays and by bedside nurses per nursery routine. Irradiance was measured at the umbilicus for supine infants and the lumbar area for prone infants using an Ohmeda Biliblanket Meter. (Biliblanket meter no. 66000198-900; Ohmeda Medical, Laurel, MD, USA). To minimize handling of infants treated with Blankets, the irradiance was measured only on the first day. The mean irradiance level was determined for each device group among the 1223 infants who received only one type of PT light throughout the intervention period.
Other secondary outcomes were determined for infants treated with only one type of PT for the duration of the 14-day study period. The secondary outcomes evaluated and included the total duration of PT, the proportion of infants who reached a high TSB, medical morbidities and neurodevelopmental outcomes as determined by trained and certified examiners. Pre-discharge medical morbidities recorded by research nurses using pre-specified definitions included bronchopulmonary dysplasia (oxygen administration at 36 weeks post menstrual age), patent ductus arteriosus (PDA), retinopathy of prematurity, intraventricular hemorrhage grade 3 or 4, necrotizing enterocolitis and death.15 Neurodevelopmental impairment at 18 to 22 months corrected age was defined as at least one of the following: blindness (no functional vision in either eye), severe hearing loss (any hearing loss with bilateral hearing aids prescribed), moderate or severe cerebral palsy, or Bayley Scales of Infant Development II mental development index (MDI) or psychomotor development index <70 (two s.d. below the mean).16
Statistical analysis
The demographic and perinatal variables were compared by using analysis of variance for continuous variables and χ2 tests for categorical variables. Model-based analyses were used to obtain adjusted estimates of device effects after controlling for treatment group, stratifying variables (center and birth weight group) and other potential confounders (sex, race and gestational age (continuous)), and the dichotomous measure of 5 min Apgar score <5. Each model was initially fit with a device by treatment arm interaction to assess the potential effect modification of treatment on device type. Because these models showed no evidence of an interaction, only the results for the main effect of device-type controlling for treatment are presented. For binary outcome measures, an overall test of device effect and adjusted relative risk (RR) estimates (with LEDs as the reference category) were calculated using robust Poisson regression in a generalized estimating equation model.17 For continuous outcome measures, the overall test of device effect and adjusted device-specific means were obtained using general linear models. No adjustments were made for multiple comparisons. All the analyses were conducted using SAS (v 9.2) software (SAS Institute, Cary, NC, USA).
Results
The number and proportion of infants initially treated with each PT device were: Spots 464 (33%), Banks 435 (31%), LEDs 364 (26%) and Blankets 141 (10%). The baseline demographics and perinatal variables are listed in Table 1. Race was significantly different between device types (P<0.001). Marginally significant differences were observed for birth weight and gestational age. Although the adjusted model showed statistically significant differences in the pretreatment TSB across PT device types, the small differences have doubtful clinical importance (Table 2).
Table 1.
Baseline characteristics
| LEDs n =364 | Blankets n =141 | Banks n =435 | Spots n =464 | P-value | |
|---|---|---|---|---|---|
| Birth weight (g)a | 771±136 | 784±138 | 766±137 | 789±128 | 0.05 |
| Gestational age (weeks)a | 25.8±1.9 | 26.1±1.9 | 25.8±1.9 | 26.1±1.9 | 0.07 |
| Race n (%) | <0.001 | ||||
| Black | 156 (43) | 90 (64) | 188 (43) | 142 (31) | |
| White | 109 (30) | 44 (31) | 121 (28) | 239 (52) | |
| Hispanic/other | 99 (27) | 7 (5) | 126 (29) | 83 (18) | |
| Male n (%) | 192 (53) | 63 (45) | 222 (51) | 241 (52) | 0.42 |
| 5 min Apgar <5 n (%) | 58 (16) | 13 (9) | 52 (12) | 63 (14) | 0.17 |
| Age at start of PT (h)a | 35±22 | 34±25 | 36±25 | 36±23 | 0.62 |
Abbreviations: Banks, fluorescent lights; Blankets, fiberoptic blankets; LED, light-emitting diode; Spots, halogen spotlights.
Mean±s.d.
Table 2.
Total serum bilirubin and phototherapy results
| Variable | Unadjusted means or proportions
|
Adjusted means or proportions
|
Adjusted P-valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|
| LEDs | Blankets | Banks | Spots | LEDs | Blankets | Banks | Spots | ||
| Pretreatment TSBb,c (n =1198) | 7.2±3 | 6.8±3 | 6.7±3 | 7.0±3 | 7.5±3 | 6.9±3 | 7.5±3 | 7.3±3 | 0.04 |
| TSB at 24±12 h after starting PTb,c (n =1325) | 4.9±2 | 6.5±2 | 5.6±2 | 5.4±2 | 5.2±2 | 6.3±2 | 6.2±2 | 5.6±2 | <0.0001 |
| Absolute change in TSB at 24±12 hb,c (n =1142) | −2.1±3 | −0.4±3 | −1.1±3 | −1.5±2 | −2.2±3 | −0.8±3 | −1.3±3 | −1.7±2 | <0.0001 |
| Relative change in TSB at 24±12 h (n =1142) | −18% | −4% | −3% | −13% | −22% | −1% | −8% | −19% | <0.01 |
| Infants with >1.5 mg dl−1 drop in TSB (n =1142)d | 52% | 28% | 38% | 44% | 58% | 23% | 40% | 47% | <0.01 |
| Infants with high TSB n (%) (n =1392)d | 16 (4) | 13 (9) | 18 (4) | 16 (4) | NA | NA | NA | NA | NA |
| Mean irradiance levels in first 14 days (μW cm−2 nm)b (n =1392) | 24±6 (n =364) | 27±9 (n =141) | 20±6 (n =435) | 24±9 (n =464) | 23±6 | 26±8 | 18±6 | 25±9 | <0.0001 |
| Duration of PT (h)b (Median–h) (n =1330) | 66±40; (54) (n =301) | 85±56; (57) (n =102) | 68±42; (57) (n =358) | 69±44; (58) (n =406) | 65±40 | 85±55 | 76±45 | 70±44 | <0.001 |
Abbreviations: Banks, fluorescent lights; Blankets, fiberoptic blankets; LED, light-emitting diode; NA, not available; PT, phototherapy; Spots, halogen spotlights; TSB, total serum bilirubin.
NA, adjusted model could not be performed for this variable because of small number of events.
Model adjusted for center, birth weight group, treatment group, device type, sex, race, 5 min APGAR <5 (yes/no) and gestational age (continuous). Denominator for each outcome was the number of infants for whom the result was known.
Mean±s.d.
TSB measured in mg dl−1.
n (proportion).
The differences in the mean TSB levels 24±12 h after initial start of PT, the absolute decrease (primary outcome) and relative decrease in TSB across the PT devices were statistically significant in unadjusted and adjusted models. The adjusted absolute decrease in TSB for LEDs (−2.2 mg dl−1) was significantly greater than that for Spots (−1.7 mg dl−1; P =0.0038), Banks (−1.3 mg dl−1; P<0.0001) and Blankets (−0.8 mg dl−1; P<0.001). The adjusted absolute decrease in TSB for Spots was significantly greater than that for Blankets (P =0.007) and Banks (P =0.042). The adjusted absolute decrease in TSB for Banks compared with that for Blankets was similar. LEDs and Spots had a similar adjusted relative decrease in TSB (−22% and −19%, respectively) and both were significantly greater than Banks (−8%; vs LEDs P =0.0025; vs Spots P =0.032) and Blankets (−1%; vs LEDs P =0.0087; vs Spots P =0.015).
The unadjusted and adjusted proportion of infants in each group with >1.5 mg dl−1 decrease in TSB in the first 24 h of treatment differed among the groups. LEDs were more likely to achieve this decrease than either Blankets or Banks (P =0.0006 and P =0.0066, respectively) and Spots were more likely to achieve this decrease than Blankets (P =0.0070). The unadjusted proportions of infants who reached a high TSB were similar between the device groups (P =0.74). The adjusted analyses could not be performed for this variable because of the small number of events in each group.
The mean irradiance levels over the intervention period were statistically different with Banks having the lowest irradiance of all groups. Spots and Blankets were statistically similar and had the highest mean irradiance levels. (Table 2) The adjusted mean duration of PT treatment was different between the device groups. LEDs had the shortest duration of PT, significantly less than Blankets or Banks (P =0.0011 and P =0.0014, respectively), but not different from Spots (P =0.18). The adjusted duration of PT for Blankets and Banks was statistically similar.
Over the 14-day intervention period, 1223 infants received a single type of PT: LEDs 307 (25%), Blankets 117 (10%), Banks 378 (31%) and Spots 421 (34%). The medical outcomes for these infants prior to discharge are shown in Table 3. After adjusting for the variables in our model, the only statistically significant comparisons were a decreased RR for PDA (RR (95% confidence interval (CI)) 0.65 (0.44, 0.96)) and PDA or death (RR (95% CI) 0.68 (0.49, 0.92)) for infants treated with Blankets compared with LEDs. In adjusted results not shown in Table 3, Blankets also showed a decreased RR for PDA compared with Banks (RR (95% CI) 0.55 (0.37, 0.82)) and Spots (RR (95% CI) 0.66 (0.46, 0.95)) and a decreased RR for PDA or death compared with Banks (RR (95% CI) 0.60 (0.44, 0.83)) and Spots (RR (95% CI) 0.69 (0.51, 0.92)). For necrotizing enterocolitis, there was a decreased RR for Blankets compared with Spots (RR (95% CI) 0.40 (0.17, 0.96)).
Table 3.
Outcomes at discharge for infants treated with a single type of phototherapy
| Outcome | Phototherapy device n (%)
|
Adjusted RR (95% CI)a
|
|||||
|---|---|---|---|---|---|---|---|
| LEDs | Blankets | Banks | Spots | Blankets/LEDs | Banks/LEDs | Spots/LEDs | |
| Death within 14 days of birth | 29 (9) | 16 (14) | 39 (10) | 20 (5) | 0.80 (0.31, 2.06) | 1.10 (0.62, 1.97) | 0.60 (0.31, 1.17) |
| Death before discharge | 63 (21) | 36 (31) | 75 (20) | 69 (16) | 0.84 (0.45, 1.55) | 0.77 (0.53, 1.12) | 0.89 (0.60, 1.32) |
| IVH grade 3 or 4 | 80 (26) | 28 (25) | 95 (25) | 65 (16) | 0.81 (0.46, 1.42) | 0.92 (0.66, 1.28) | 0.70 (0.49, 1.02) |
| Death or IVH grade 3 or 4 | 99 (32) | 42 (36) | 118 (31) | 86 (21) | 0.89 (0.55, 1.44) | 0.95 (0.71, 1.26) | 0.73 (0.53, 1.01) |
| BPD at 36 weeks | 112 (45) | 44 (51) | 145 (46) | 150 (42) | 0.81 (0.55, 1.20) | 1.00 (0.79, 1.26) | 0.89 (0.69, 1.14) |
| Death or BPD at 36 weeks | 167 (55) | 73 (63) | 205 (54) | 209 (51) | 0.94 (0.71, 1.24) | 1.00 (0.84, 1.18) | 0.95 (0.79, 1.14) |
| PDA | 155 (50) | 39 (33) | 216 (57) | 195 (46) | 0.65 (0.44, 0.96)* | 1.17 (0.98, 1.41) | 0.99 (0.80, 1.22) |
| Death or PDA | 179 (58) | 58 (50) | 245 (65) | 222 (53) | 0.68 (0.49, 0.92)* | 1.12 (0.96, 1.31) | 0.99 (0.82, 1.18) |
| NEC | 36 (12) | 8 (7) | 36 (10) | 65 (15) | 0.44 (0.17, 1.11) | 1.18 (0.69, 2.02) | 1.10 (0.67, 1.82) |
| Death or NEC | 83 (27) | 39 (33) | 94 (25) | 108 (26) | 0.69 (0.41, 1.17) | 0.95 (0.70, 1.31) | 1.03 (0.74, 1.43) |
| ROP stage 3–5 | 48 (19) | 20 (24) | 65 (21) | 67 (19) | 1.73 (0.94, 3.18) | 1.50 (0.99, 2.27) | 1.13 (0.73, 1.75) |
| Death or ROP stage 3–5 | 110 (36) | 55 (50) | 136 (37) | 132 (33) | 1.23 (0.84, 1.82) | 1.11 (0.87, 1.42) | 0.98 (0.76, 1.27) |
Abbreviations: Banks, fluorescent lights; Blankets, fiberoptic blankets; BPD, bronchopulmonary dysplasia; CI, confidence interval; IVH, intraventricular hemorrhage; LED, light-emitting diode; NEC, necrotizing enterocolitis; PDA, patent ductus arteriosus; ROP, retinopathy of prematurity; RR, relative risk; Spots, halogen spotlights; TSB, total serum bilirubin.
Model adjusted for center, birth weight group, treatment group, device type, sex, race, 5 min APGAR <5 (yes/no) and gestational age (continuous). Device type by treatment interaction was not significant and hence not included in the model.
P<0.05, denominator for each outcome was the number of infants for whom the result was known.
The infant outcomes at 18 to 22 months corrected age are shown in Table 4. For death or neurodevelopmental impairment (primary outcome of main trial), neither the unadjusted nor the adjusted analyses showed a difference in risk among the PT devices. The only significant infant outcomes were in relation to MDI <85 and death or MDI <85. For MDI <85, Blankets were associated with a decreased risk compared with LEDs (RR (95% CI) 0.68 (0.48, 0.96)), whereas Banks showed an increased risk compared with LEDs (RR (95% CI) 1.23 (1.02, 1.49)). In results not shown in Table 4, Blankets had a decreased risk of MDI <85 compared with Banks (RR (95% CI) 0.55 (0.39, 0.79)) and Banks had an increased risk compared with Spots (RR (95% CI) 1.54 (1.21, 1.96)). For death or MDI <85, Banks showed an increased risk compared with the other devices: LEDs (RR (95% CI) 1.16 (1.02, 1.33)), Spots (RR (95% CI) 1.26 (1.08, 1.48)) and Blankets (RR (95% CI) 1.43 (1.12, 1.85)).
Table 4.
Outcomes at 18–22 months for infants treated with a single type of phototherapy
| Outcome | Phototherapy device n (%)
|
Adjusted RR (95% CI)a
|
|||||
|---|---|---|---|---|---|---|---|
| LEDs | Blankets | Banks | Spots | Blankets/LEDs | Banks/LEDs | Spots/LEDs | |
| Death or NDI | 87 (39) | 24 (35) | 96 (37) | 102 (35) | 0.96 (0.69, 1.33) | 0.97 (0.81, 1.18) | 1.01 (0.82, 1.25) |
| NDI | 151 (52) | 62 (58) | 182 (53) | 180 (49) | 0.89 (0.53, 1.50) | 0.94 (0.70, 1.27) | 0.92 (0.65, 1.31) |
| Death | 64 (21) | 38 (33) | 86 (24) | 78 (20) | 0.86 (0.47, 1.55) | 0.95 (0.67, 1.35) | 1.05 (0.72, 1.54) |
| Moderate/severe CP | 11 (5) | 3 (4) | 16 (6) | 26 (9) | 0.81 (0.25, 2.68) | 0.98(0.44, 2.17) | 1.18 (0.56, 2.49) |
| Death or moderate/severe CP | 75 (25) | 41 (37) | 102 (28) | 104 (27) | 0.90 (0.54, 1.50) | 0.97 (0.71, 1.32) | 1.11 (0.80, 1.54) |
| Severe hearing lossb | 8 (4) | 1 (1) | 4 (1) | 10 (3) | 0.47 (0.07, 3.31) | 0.49 (0.16, 1.51) | 0.92 (0.38, 2.25) |
| Death or severe hearing loss | 72 (25) | 39 (35) | 90 (25) | 88 (23) | 0.72 (0.42, 1.24) | 0.87 (0.62, 1.22) | 0.92 (0.64, 1.32) |
| MDI <70 | 70 (31) | 19 (28) | 77 (30) | 76 (26) | 0.76 (0.40, 1.43) | 0.96 (0.68, 1.37) | 0.85 (0.55, 1.31) |
| Death or MDI <70 | 134 (46) | 57 (53) | 163 (47) | 154 (41) | 0.90 (0.63, 1.31) | 0.99 (0.80, 1.22) | 1.01 (0.79, 1.28) |
| MDI <85 | 139 (62) | 36 (52) | 160 (62) | 153 (52) | 0.68 (0.48, 0.96)* | 1.23 (1.02, 1.49)* | 0.80 (0.64, 1.00) |
| Death or MDI <85 | 203 (70) | 74 (69) | 246 (71) | 231 (62) | 0.81 (0.64, 1.02) | 1.16 (1.02, 1.33)* | 0.92 (0.79, 1.07) |
| PDI <70 | 47 (21) | 15 (22) | 52 (20) | 70 (24) | 1.38 (0.68, 2.81) | 1.06 (0.67, 1.67) | 1.36 (0.83, 2.23) |
| Death or PDI <70 | 111 (39) | 53 (50) | 138 (40) | 148 (40) | 1.13 (0.76, 1.69) | 1.02 (0.80, 1.30) | 1.17 (0.90, 1.52) |
| PDI <85 | 95 (43) | 58 (78) | 100 (38) | 126 (43) | 0.95 (0.59, 1.54) | 1.14 (0.86, 1.51) | 1.10 (0.80, 1.51) |
| Death or PDI <85 | 159 (56) | 64 (60) | 186 (54) | 204 (55) | 1.00 (0.74, 1.36) | 1.08 (0.90, 1.29) | 1.11 (0.91, 1.35) |
| Normal gross motor function | 177 (77) | 58 (78) | 213 (78) | 232 (77) | 1.13 (0.92, 1.39) | 1.06 (0.95, 1.20) | 1.05 (0.92, 1.20) |
| Walk fluently | 177 (77) | 56 (76) | 204 (75) | 226 (75) | 0.98 (0.79, 1.21) | 0.97 (0.86, 1.10) | 0.94 (0.82, 1.08) |
| Fine pincer grasp | 197 (85) | 63 (85) | 231 (85) | 254 (84) | 1.08 (0.92, 1.28) | 1.09 (0.99, 1.19) | 1.05 (0.94, 1.16) |
Abbreviations: Banks, fluorescent lights; Blankets, fiberoptic blankets; CI, confidence interval; CP, cerebral palsy; LED, light-emitting diode; MDI, mental development index; NA, not available; NDI, neurodevelopmental impairment; PDI, psychomotor development index; RR, relative risk; Spots, halogen spotlights; TSB, total serum bilirubin.
Model adjusted for center, birth weight group, treatment group, device type, sex, race, 5 min APGAR <5 (yes/no) and gestational age (continuous). Device type by treatment interaction was not significant and hence not included in the model.
Because of rarity of outcome, center was excluded from the model.
P<0.05, denominator for each outcome was the number of infants for whom the result was known.
Discussion
Among PT devices used to treat hyperbilirubinemia in this large group of ELBW infants, LEDs were associated with the largest absolute decrease in TSB in the first 24±12 h of PT. LEDs and Spots were similar for the relative decrease in TSB and duration of treatment. LEDs performed better than Banks and Blankets but similar to Spots in reducing TSB >1.5 mg dl−1 within 24±12 h of PT. Overall, LEDs and Spots appeared to have similar effectiveness and duration of treatment. This information could be important for clinicians starting PT on ELBW infants with a high TSB where a rapid response is desired to minimize the possibility of bilirubin encephalopathy, need for an exchange transfusion and exposure to PT. The LED devices were effective despite a relatively lower irradiance probably because the emitted light is in the maximally effective range of 450 to 470 nm and not diluted with other wavelengths that would be included in the measurement range (400 to 520 nm) of the Ohmeda Biliblanket Meter.
Maintaining and monitoring irradiance levels will be important for obtaining similar results in clinical practice. The NICHD PT trial had a PT target range of 15 to 40 μW cm−2 nm which was significantly higher than the estimated irradiance of 6 to 10 μW cm−2 nm used in the first NICHD PT trial.18 This irradiance may be higher than some older PT devices can attain. Even with the newer PT lights, the positioning of the light and distance from the infant can dramatically affect the achieved irradiance levels and the surface area affected.19
In this study, the poor performance of the Banks could be related to the relatively low irradiance levels achieved either from older PT units or positioning. The Blankets had the highest mean irradiance level but were not very effective. A potential explanation for this could be the skin surface area irradiated by the Blankets. Dicken20 estimated that the fraction of the total surface area irradiated by a Blanket to be 6% for a term infant and 9% for a preterm infant compared with 33% for overhead banks. Tayman recently compared overhead and underneath LED devices with identical irradiances (30 μW cm−2 nm) in infants ≥35 weeks.21 The results demonstrated that the overhead units were more effective in reducing TSB levels and had a shorter duration of PT. They theorized that the overhead unit illuminated a larger surface area resulting in better efficacy. Our findings would support the concept of an overhead PT system being more effective than a system below the infant given similar irradiance levels.
In evaluating therapies, it is important to consider clinical and neurodevelopmental outcomes beyond discharge especially in this vulnerable population. The NICHD Neonatal Research Network PT trial provided an opportunity to explore the possibility that different PT lights may have divergent effects. However, our findings here should be interpreted with caution because the assignment of PT devices was not randomized, which introduced a potential for bias and created device groups of different sizes, and a large number of comparisons were performed. It is reassuring to know that for death or neurodevelopmental impairment (primary outcome of the NICHD PT trial) and almost all of the other outcomes, there were no significant differences in risk among the PT devices. However, the wide CIs for this and other outcomes do not exclude the possibility of important differences in the long-term effects of these commonly used devices.
There were a few differences that deserve some discussion. Infants treated with Blankets were at lower risk for PDA and PDA or death compared with those treated with the other PT devices. There was also a decreased risk of NEC with Blankets compared with Spots, however, this was not found for the combined outcome of NEC or death. Could there be different physiological effects for an ELBW infant lying on their back on a biliblanket vs an overhead PT light? There have been trials showing a hemodynamic effect from PT. In a small randomized trial, chest shielding during PT reduced the frequency of PDA and length of hospital stay,22 but in another trial this effect was not found.23 Benders et al24,25 has shown hemodynamic changes in term and premature infants while on PT, which resolved when PT was stopped. Pezzati et al26 and Yao et al27 have shown changes to the postprandial mesenteric blood flow with conventional PT. Pezzatti et al did not find these blood flow changes with fiber-optic PT. The recent NICHD PT trial did not show a difference in the RR of PDA or death (RR (95% CI) 0.95, (0.88, 1.02)), PDA (RR (95% CI) 0.93 (0.86, 1.02)) or NEC (RR (95% CI) 0.9 (0.70, 1.14)) between the aggressive and conservative groups despite a very significant difference in the duration of PT treatment (88 vs 35 h, P<0.001).15 These results in a large randomized trial would argue against a causal association between PT and PDA or NEC.
An important outcome associated with bilirubin encephalopathy is hearing loss. We could detect no difference between the device groups in the prevalence of severe hearing loss or severe hearing loss and death. However, hearing loss was an infrequent outcome limiting our power to detect associations.
The only outcomes at 18 to 22 months corrected age that differed among the PT device groups were MDI <85 and death or MDI <85. The results suggest that infants treated with Banks had an increased risk for either of these outcomes compared with the other three device types. In addition, Blankets had a decreased risk for MDI <85 compared with LEDs but not for the composite outcome of death or MDI <85. We do not have a plausible biological theory to explain these findings. These differences were not hypothesized before the study and due to the large number of comparisons performed could be because of chance.
PT is administered to the great majority of ELBW infants. This study represents the largest sample of ELBW infants treated with PT and analyzed to assess the performance of the devices and the outcomes of the infants. LED lights were the most efficient at reducing the absolute TSB in the first 24±12 h of treatment but were similar to Spots in the other performance measures. Our findings indicate short-term differences in the efficacy of the devices used to administer this therapy and the possibility of important differences at 18 to 22 months. Different PT devices being developed or used in treating high-risk infants deserve rigorous testing in randomized trials that include both short- and long-term follow-up assessments.
Acknowledgments
This work was supported by grants from the National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, which provided oversight for study conduct.
Appendix
Acknowledgements
The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) provided grant support for the Neonatal Research Network’s (NRN’s) Phototherapy Trial (2002 to 2005).
Data collected at participating sites of the NICHD NRN were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed and analyzed the data for this study. On behalf of the NRN, Dr Abhik Das (DCC Principal Investigator), Dr Qing Yao, Dr Dennis Wallace and Ms Sarah Kandefer (DCC Statisticians) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis.
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study:
NRN Steering Committee Chairs—Alan Jobe, MD PhD, University of Cincinnati (2001 to 2006); Michael S Caplan, MD, University of Chicago, Pritzker School of Medicine (2006 to present).
Alpert Medical School of Brown University and Women and Infants Hospital of Rhode Island (U10 HD27904)—Abbot R Laptook, MD; Angelita Hensman, BSN RNC; Lucy Noel RN.
Case Western Reserve University Rainbow Babies and Children’s Hospital (U10 HD21364, M01 RR80)—Avroy A Fanaroff, MD; Michele C Walsh, MD MS; Deanne Wilson-Costello, MD; Nancy S Newman, RN; Bonnie S Siner, RN.
Cincinnati Children’s Hospital Medical Center, University Hospital and Good Samaritan Hospital (U10 HD27853, M01 RR8084)—Edward F Donovan, MD; Kurt Schibler, MD; Jean Steichen, MD; Barb Alexander, RN; Cathy Grisby, BSN CCRC; Marcia Mersmann, RN; Holly Mincey, RN; Jody Shively, RN; Teresa Gratton, PA.
Duke University School of Medicine University Hospital, Alamance Regional Medical Center and Durham Regional Hospital (U10 HD40492, M01 RR30)—Ronald N Goldberg, MD; C Michael Cotten, MD MHS; Ricki F Goldstein, MD; Kathy J Auten, MSHS; Melody B Lohmeyer, RN MSN.
Emory University Children’s Healthcare of Atlanta, Grady Memorial Hospital and Emory University Hospital Midtown (U10 HD27851, M01 RR39)—Barbara J Stoll, MD; Ira Adams-Chapman, MD; Ellen C Hale, RN BS CCRC.
Eunice Kennedy Shriver National Institute of Child Health and Human Development—Linda L Wright, MD; Elizabeth M McClure, MEd.
Indiana University Indiana University Hospital, Methodist Hospital, Riley Hospital for Children and Wishard Health Services (U10 HD27856, M01 RR750)—Brenda B Poindexter, MD MS; James A Lemons, MD; Anna M Dusick, MD; Diana D Appel, RN BSN; Dianne E Herron, RN; Lucy C Miller, RN BSN CCRC; Leslie Dawn Richard, BSN CCRC.
RTI International (U10 HD36790)—W Kenneth Poole, PhD; Betty Hastings; Elizabeth N McClure, MEd; Jamie E Newman, PhD MPH; Rebecca L Perritt, MS; Carolyn M Petrie Huitema, MS; Kristin M Zaterka-Baxter, RN BSN.
Stanford University Lucile Packard Children’s Hospital (U10 HD27880, M01 RR70)—Susan R Hintz, MD MS; M Bethany Ball, BS CCRC.
University of Alabama at Birmingham Health System and Children’s Hospital of Alabama (U10 HD34216, M01 RR32)—Waldemar A Carlo, MD; Namasivayam Ambalavanan, MD; Myriam Peralta-Carcelen, MD MPH; Monica V Collins, RN BSN MaEd; Shirley S Cosby, RN BSN; Vivien A Phillips, RN BSN.
University of California—San Diego Medical Center and Sharp Mary Birch Hospital for Women (U10 HD40461)—Neil N Finer, MD; Yvonne E Vaucher, MD MPH; Maynard R Rasmussen MD; David Kaegi, MD; Kathy Arnell, RNC; Clarence Demetrio, RN; Martha G Fuller, RN MSN; Chris Henderson, RCP CRTT; Wade Rich, BSHS RRT.
University of Miami Holtz Children’s Hospital (U10 HD21397, M01 RR16587)—Charles R Bauer, MD; Shahnaz Duara, MD; Silvia Hiriart-Fajardo, MD; Ruth Everett-Thomas, RN BSN; Amy Mur Worth, RN MS; Silvia Frade Eguaras, MS.
University of Rochester Medical Center Golisano Children’s Hospital (U10 HD40521, M01 RR44)—Ronnie Guillet, MD PhD; Gary J Myers, MD; Linda J Reubens, RN CCRC; Diane Hust, MS RN CS; Rosemary L Jensen; Erica Burnell, RN.
University of Texas Southwestern Medical Center at Dallas Parkland Health and Hospital System and Children’s Medical Center Dallas (U10 HD40689, M01 RR633)—Walid A Salhab, MD; Pablo J Sanchez, MD; Charles R Rosenfeld, MD; Roy J Heyne, MD; Jackie Hickman, RN; Gay Hensley, RN; Nancy A Miller, RN; Janet Morgan, RN.
University of Texas Health Science Center at Houston Medical School, Children’s Memorial Hermann Hospital and Lyndon Baines Johnson General Hospital/Harris County Hospital District.
(U10 HD21373, KL2 RR24149, UL1 RR24148)—Kathleen Kennedy, MD MPH; Pamela J Bradt, MD MPH; Patricia W Evans, MD; Laura L Whiteley, MD; Esther G Akpa, RN BSN; Patty A Cluff, RN; Anna E Lis, RN BSN; Claudia I Franco, RNC MSN; Maegan Currence, RN; Nora I. Alaniz, BS; Patti L Pierce Tate, RCP; Sharon L Wright, MT(ASCP).
Wake Forest University Baptist Medical Center, Brenner Children’s Hospital, and Forsyth Medical Center (U10 HD40498, M01 RR7122)—Lisa K Washburn, MD; Nancy J Peters, RN CCRP; Barbara G Jackson, RN BSN.
Wayne State University Hutzel Women’s Hospital and Children’s Hospital of Michigan (U10 HD21385)—Seetha Shankaran, MD; Yvette Johnson, MD; Athina Pappas, MD; Rebecca Bara, RN BSN; Geraldine Muran, RN BSN; Deborah Kennedy, RN BSN.
Yale University Yale-New Haven Children’s Hospital (U10 HD27871, M01 RR6022)—Richard A. Ehrenkranz, MD; Patricia Gettner, RN; Harris C Jacobs, MD; Christine Butler, MD; Patricia Cervone, RN; Monica Konstantino, RN BSN; Elaine Romano, MSN.
Footnotes
Conflict of interest
Natus Medical loaned light-emitting diode phototherapy lights to each center. These lights were used at the discretion of the attending neonatologist in treating infants in either treatment group. The lights were returned to Natus Medical or purchased at a prorated price after the study. Natus Medical has no role in the study design, data collection, data analysis or manuscript preparation or revision.
References
- 1.Cremer RJ, Perryman PW, Richards DH. Influence of light on the hyperbilirubinemia of infants. Lancet. 1958;271:1094–1097. doi: 10.1016/s0140-6736(58)91849-x. [DOI] [PubMed] [Google Scholar]
- 2.Vreman HJ, Wong RJ, Stevenson DK, Route RK, Reader SD, Fejer MM, et al. Light-emitting diodes: a novel light source for phototherapy. Pediatr Res. 1998;44(5):804–809. doi: 10.1203/00006450-199811000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Seidman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK, et al. A prospective randomized controlled study of phototherapy using blue and blue-green light-emitting devices, and conventional halogen-quartz phototherapy. J Perinatology. 2003;23:123–127. doi: 10.1038/sj.jp.7210862. [DOI] [PubMed] [Google Scholar]
- 4.Tan KL. Comparison of the efficacy of fiberoptic and conventional phototherapy for neonatal hyperbilirubinemia. J Pediatr. 1994;125:607–612. doi: 10.1016/s0022-3476(94)70019-2. [DOI] [PubMed] [Google Scholar]
- 5.Romagnoli C, Zecca E, Papacci P, Vento G, Girlando P, Latella C. Which phototherapy system is most effective in lowering serum bilirubin in very preterm infants? Fetal Diagn Ther. 2006;21:204–209. doi: 10.1159/000089304. [DOI] [PubMed] [Google Scholar]
- 6.Costello SA, Nyikal J, Yu VYH, McCloud P. Biliblanket phototherapy system versus conventional phototherapy: a randomized controlled trial in preterm infants. J Paediatr Child Health. 1995;31:11–13. doi: 10.1111/j.1440-1754.1995.tb02903.x. [DOI] [PubMed] [Google Scholar]
- 7.Donzelli GP, Moroni M, Rapisardi G, Agati G, Fusi F. Fiberoptic phototherapy in the management of jaundice in low birthweight infants. Acta Pediatr. 1996;85:366–370. doi: 10.1111/j.1651-2227.1996.tb14034.x. [DOI] [PubMed] [Google Scholar]
- 8.Dani C, Martelli E, Reali MF, Bertini G, Panin G, Rubaltelli F. Fiberoptic and conventional phototherapy effects on the skin of premature infants. J Pediatr. 2001;138(3):438–440. doi: 10.1067/mpd.2001.111329. [DOI] [PubMed] [Google Scholar]
- 9.Van Kaam AHLC, van Beek RHT, Vergunstvan Keulen JG, van der Heijden J, Lutz-Dettinger N, Hop W, et al. Fiber optic versus conventional phototherapy for hyperbilirubinemia in preterm infants. Eur J Pediatr. 1998;157:132–137. doi: 10.1007/s004310050785. [DOI] [PubMed] [Google Scholar]
- 10.Bertini G, Perugi S, Elia S, Pratesi S, Dani C, Rubaltelli FF. Transepidermal water loss and cerebral hemodynamics in preterm infants: conventional versus LED phototherapy. Eur J Pediatr. 2008;167:37–42. doi: 10.1007/s00431-007-0421-3. [DOI] [PubMed] [Google Scholar]
- 11.Martins BMR, de Carvalho M, Moreira ME, Lopes JMA. Efficacy of new microprocessed phototherapy system with five high density light emitting diodes (Super LED) J Pediatr (Rio J) 2007;83:253–258. doi: 10.2223/JPED.1637. [DOI] [PubMed] [Google Scholar]
- 12.Seidman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK, et al. A new blue light-emitting phototherapy device: a prospective randomized controlled study. J Pediatr. 2000;136(6):771–774. [PubMed] [Google Scholar]
- 13.Maisels MJ, Kring EA, DeRidder J. Randomized controlled trial of light-emitting diode phototherapy. J Perinatol. 2007;27:565–567. doi: 10.1038/sj.jp.7211789. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan M, Gold V, Hammerman C, Hochman A, Goldschmidt D, Vreman HJ, et al. Phototherapy and photo-oxidation in premature neonates. Biol Neonate. 2005;87:44–50. doi: 10.1159/000081085. [DOI] [PubMed] [Google Scholar]
- 15.Morris BH, Oh W, Tyson JE, Stevenson DK, Phelps DL, O’Shea TM, et al. Aggressive vs conservative phototherapy for infants with extremely low birth weight. N Engl J Med. 2008;359:1885–1896. doi: 10.1056/NEJMoa0803024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bayley N. Bayley Scales of Infant Development II. The Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- 17.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Invited Editorial Note. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 18.Landry RJ, Scheidt PC, Hammond RW. Ambient light and phototherapy conditions of eight neonatal care units: a summary report. Pediatrics. 1985;75:434–436. [PubMed] [Google Scholar]
- 19.Hart G, Cameron R. The importance of irradiance and area in neonatal phototherapy. Arch Dis Child Fetal Neonatal Ed. 2005;90:F437–F440. doi: 10.1136/adc.2004.068015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dicken P, Grant LJ, Jones S. An evaluation of the characteristics and performance of neonatal phototherapy equipment. Physiol Meas. 2000;21:493–503. doi: 10.1088/0967-3334/21/4/306. [DOI] [PubMed] [Google Scholar]
- 21.Tayman C, Tatli MM, Aydemir S, Karadag A. Overhead is superior to underneath light-emitting diode phototherapy in the treatment of neonatal jaundice: a comparative study. J Paediatr Child Health. 2010;46:234–237. doi: 10.1111/j.1440-1754.2009.01676.x. [DOI] [PubMed] [Google Scholar]
- 22.Rosenfeld W, Sadhev S, Brunot V, Jhaveri R, Zabaleta I, Evans HE. Phototherapy effect on the incidence of patent ductus arteriosus in premature infants: prevention with chest shielding. Pediatrics. 1986;78:10–14. [PubMed] [Google Scholar]
- 23.Travadi J, Simmer K, Ramsay J, Doherty D, Hagan R. Patent ductus arteriosus in extremely preterm infants receiving phototherapy: does shielding the chest make a difference? A randomized, controlled trial. Acta Paediatr. 2006;95:1418–1423. doi: 10.1080/08035250600771458. [DOI] [PubMed] [Google Scholar]
- 24.Benders MJ, van Bel F, van de Bor M. Haemodynamic consequences of phototherapy in term infants. Eur J Pediatr. 1999;158:323–328. doi: 10.1007/s004310051082. [DOI] [PubMed] [Google Scholar]
- 25.Benders MJ, van Bel F, van de Bor M. Cardiac output and ductal reopening during phototherapy in preterm infants. Acta Paediatr. 1999;88:1014–1019. doi: 10.1080/08035259950168540. [DOI] [PubMed] [Google Scholar]
- 26.Pezzati M, Biagiotti R, Vangi V, Lombardi E, Wiechmann L, Rubaltelli FF. Changes in mesenteric blood flow response to feeding: Conventional versus fiber-optic phototherapy. Pediatrics. 2000;105:350–353. doi: 10.1542/peds.105.2.350. [DOI] [PubMed] [Google Scholar]
- 27.Yao AC, Martinussen M, Johansen OJ, Brubakk AM. Phototherapy-associated changes in mesenteric blood flow response to feeding in term neonates. J Pediatr. 1994;124:309–312. doi: 10.1016/s0022-3476(94)70325-6. [DOI] [PubMed] [Google Scholar]