Abstract
Sexual minority youth (youth who are attracted to the same sex or endorse a gay/lesbian/bisexual identity) report significantly higher rates of depression and suicidality than heterosexual youth. The minority stress hypothesis contends that the stigma and discrimination experienced by sexual minority youth create a hostile social environment that can lead to chronic stress and mental health problems. The present study used longitudinal mediation models to directly test sexual minority-specific victimization as a potential explanatory mechanism of the mental health disparities of sexual minority youth. One hundred ninety seven adolescents (14–19 years old; 70% female; 29% sexual minority) completed measures of sexual minority-specific victimization, depressive symptoms, and suicidality at two time points six months apart. Compared to heterosexual youth, sexual minority youth reported higher levels of sexual minority-specific victimization, depressive symptoms, and suicidality. Sexual minority-specific victimization significantly mediated the effect of sexual minority status on depressive symptoms and suicidality. The results support the minority stress hypothesis that targeted harassment and victimization are partly responsible for the higher levels of depressive symptoms and suicidality found in sexual minority youth. This research lends support to public policy initiatives that reduce bullying and hate crimes because reducing victimization can have a significant impact on the health and well-being of sexual minority youth.
Keywords: sexual minority youth, victimization, depression, suicidality, minority stress
Introduction
There are significant mental health disparities between sexual minority youth (SMY; youth who are attracted to the same sex, engage in sexual behavior with the same sex, or endorse a gay/lesbian/bisexual identity) and heterosexual youth (Garofalo, Wolf, Wissow, Woods, & Goodman, 1999; Hershberger & D’Augelli, 1995; Remafedi, French, Story, Resnick, & Blum, 1998; Russell & Joyner, 2001). A recent meta-analysis of 24 studies measuring mental health of SMY found that SMY have higher rates of depression and higher rates of suicidality (suicide ideation and suicide attempts) than heterosexual youth (Marshal et al., 2011). Notably, the effect size for the relationship between sexual minority status and suicidality increased as the severity of the suicidality measure increased (e.g., a larger effect size for actual suicide attempts than for having suicidal thoughts). Compared with heterosexual youth, SMY were almost two times as likely to report suicidal ideation, more than three times as likely to report suicide attempts, and more than four times as likely to report a suicide attempt that required medical attention. This finding is particularly troubling because it shows that not only is there a broad and general disparity in the mental health of SMY but the disparity is largest for the most severe mental health outcomes (e.g., attempted suicide). Furthermore, a recent study found that 22% of SMY in the 11th grade attempted suicide in the past 12 months compared to 4% of heterosexual youth (Hatzenbuehler, 2011). Research clearly shows stark disparities between SMY and heterosexual youth on depression and suicidality outcomes.
The disparities, however, are not limited to depression and suicide. A recent report by the Centers for Disease Control and Prevention (CDC) found that SMY, compared to heterosexual youth, have a greater prevalence of health-risk behaviors in 7 out of 10 health behavior categories (violence, attempted suicide, tobacco use, alcohol use, other drug use, sexual behaviors, and weight management; CDC, 2011). There is a clear and pressing need for more research in SMY health disparities, a need reiterated by the Healthy People 2020 initiative (U.S. Department of Health and Human Services, 2012) and a recent report by the Institute of Medicine (IOM) commissioned by the National Institutes of Health (IOM, 2011). In particular, research that identifies explanatory mechanisms of these disparities is needed.
The present research investigates the minority stress hypothesis as an explanatory framework for understanding the depression and suicidality disparities among SMY. The root causes of the disparities in SMY have only just begun to be investigated. The minority stress hypothesis (Meyer, 2003) contends the stigma, prejudice, and discrimination experienced by lesbian, gay, and bisexual individuals create a hostile social environment that can lead to chronic stress and mental health problems. Therefore, most research to date on the cause(s) of the mental health disparities among SMY has focused on victimization based on sexual minority status (i.e., being targeted for bullying and harassment, ranging from verbal slurs to physical abuse, based on one’s actual or perceived sexual identity).
Cross-sectional studies have examined some elements of the minority stress model and results generally support the model. For example, in a recent meta-analysis, SMY were 1.7 times more likely to report being assaulted at school and 2.4 times more likely to report skipping school due to fear (Friedman et al., 2011). Furthermore, victimization based on sexual identity has been found to have a profound impact on the mental health of SMY. SMY who experience higher levels of victimization are 2.6 times more likely to report depression and 5.6 times more likely to attempt suicide than SMY who experience lower levels of victimization (Russell, Ryan, Toomey, Diaz, & Sanchez, 2011); and SMY who experience high levels of victimization engage in more health risk behaviors than SMY who experience lower levels of victimization and heterosexual youth, with the latter two groups not differing significantly (Bontempo & D’Augelli, 2002).
The negative effects of victimization based on sexual minority status are not limited to those youth who actually identify as a sexual minority. Swearer and colleagues (2008) used cross-sectional data and found that boys bullied by being called “gay,” regardless of their actual sexual identity, were more likely to experience psychosocial stress than those bullied for other reasons (Swearer, Turner, Givens, & Pollack, 2008). One longitudinal study found similar results. Specifically, boys who are victimized based on real or perceived sexual identity report higher levels of anxiety and depression even after controlling for anxiety and depression reported a year earlier (Poteat & Espelage, 2007). However neither study measured sexual minority status so they could not determine whether sexual minority-specific victimization disproportionately affected SMY. Taken together, the extant research suggests that it is not sexual minority status that causes mental health and adjustment problems, it is the victimization experienced by being a sexual minority that is responsible for these negative outcomes.
A few studies have tested cross-sectional mediation models of the minority stress hypothesis in youth (14–18 years old) using measures of sexual minority status, victimization and discrimination, and mental health, the findings of which have generally supported the hypothesis. For example Almeida and colleagues (2009) used cross-sectional data to show that the relationship between sexual minority status and emotional distress was explained partially by perceived discrimination (Almeida, Johnson, Corliss, Molnar, & Azrael, 2009). Williams and colleagues (2005) also used cross-sectional data to show that victimization partially explains the relationship between sexual minority status and externalizing behaviors (e.g., aggression, conduct problems, and delinquency; Williams, Connolly, Pepler, & Craig, 2005). Notably, each of these studies used cross-sectional data to test the minority stress hypothesis. We seek to extend their findings by testing the minority stress hypothesis in SMY using a longitudinal model, a sexual minority-specific stress variable, and a heterosexual comparison group, all necessary components to test more completely the major tenets of the minority stress hypothesis.
Overview and Hypotheses
Our study used a six-month longitudinal design to directly test the minority stress hypothesis, specifically that SMY experience greater sexual minority-specific victimization than heterosexual youth and that such victimization is at least partly responsible for elevated levels of depression and suicidality in SMY. We predicted that SMY would report more sexual minority-specific victimization, depressive symptomatology, and suicidality compared to heterosexual youth and that these variables would be positively correlated. We further predicted that greater sexual minority-specific victimization would explain the relationship between sexual minority status and mental health outcomes. To test this prediction, we used a mediation model which is a statistical tool used to identify explanatory mechanisms (e.g., sexual minority-specific victimization) for the effect of a predictor (e.g., sexual minority status) on an outcome (e.g., depressive symptoms / suicidality; see MacKinnon, 2008).
Method
Participants
Participants were 197 adolescents (30% male; 70% female) ranging in age from 14 to 19 (M = 17, SD = 1.36). Represented racial groups included 31% White, 63% African American, 3% other. The ethnicity of the sample was predominately non-Hispanic (90%). Youth were recruited to participate in a longitudinal study of adolescent health and wellness from one adolescent medicine clinic in Pennsylvania and one in Ohio by either provider referral or a screening system in a provider’s waiting room. The two adolescent medicine clinics are large, urban clinics affiliated with academic medical centers that serve adolescents between the ages of 10 and 22 years. They provide primary care health services including routine physical exams and immunizations, family planning services including contraception and testing and treatment for sexually transmitted infections, and consultative care for patients with concerns specific to adolescence. Attraction status was obtained via a clinic-based confidential clinical assessment procedure. All youth were eligible to participate so long as they were between 14–19 (inclusive) and able to read and understand English at the sixth grade level. Otherwise neither the youths’ health status at the time of their clinical visit nor their presenting problem were considered as inclusion or exclusion criteria for recruitment. The long-term recruitment goal of this NIH-funded, IRB-approved longitudinal study is to recruit a sample of 200 same-sex attracted youth and a matched comparison group of opposite-sex attracted youth (final groups will be matched on age, gender, and race). Investigators will accomplish this with an open-cohort design such that a total of 400 adolescent participants will be recruited over 4–5 years (approximately 100 per year), which will accommodate the slower rate of recruitment for same-sex attracted youth due to the lower proportion of sexual minority individuals in the population (2–8%). Results presented in the current article are from the participants recruited in the first two years of enrollment.
Materials and Procedure
Study procedures were approved by the Institutional Review Boards at the University of Pittsburgh and Nationwide Children’s Hospital (Columbus, OH). Parental consent was obtained for all participants who were under 18 years old at the time of study entry. Participants who were 18–19 years old provided their own written consent. Participants completed a battery of questionnaires at wave 1 and again six months later at wave 2.
Sexual minority status
Participants’ sexual minority status was measured at wave 1 by one item that stated “Please choose the description that best fits how you think about yourself.” Response options were: 100% heterosexual (straight), mostly heterosexual (straight), but somewhat attracted to people of your own sex, bisexual – that is, attracted to men and women equally, mostly homosexual (gay), but somewhat attracted to people of the opposite sex, and 100% homosexual (gay). Participants who indicated any category other than 100% heterosexual were classified as a sexual minority. The variable was coded as 0 = 100% heterosexual and 1 = sexual minority.
Sexual minority-specific victimization
Victimization due to actual or perceived sexual minority status was measured at waves 1 and 2 by four items that assessed the frequency during the past 6 months of being teased/bullied, hit/beaten up, treated unfairly, or called bad names because someone thought the participant was gay/lesbian. Responses were scored as 0 = never, 1 = once or twice, 2 = a few times, and 3 = many times. A mean score of the 4 items was computed and used in analyses. The four items had acceptable internal consistency (waves 1 and 2: α = .86).
Depressive symptoms
The CESD (Radloff, 1977) was administered at waves 1 and 2 to assess frequency of depressive symptoms during the past week. The CESD consists of 20 common symptoms of depression scored on a scale of 0 (rarely or none of the time) to 3 (most or all of the time). A mean score of all 20 items was computed and used in analyses. The measure had acceptable internal consistency (wave 1: α = .89; wave 2: α = .84).
Suicidality
Lifetime history of suicidal thoughts and intent were measured at wave 1 by one item: “Have you ever thought about or attempted to kill yourself?” (scored as 0 = never, 1 = it was just a brief or passing thought, 2 = I have had a plan at least once to kill myself but did not try to do it, 3 = I have had a plan at least once to kill myself and really wanted to die, 4 = I have attempted to kill myself, but did not want to die, 5 = I have attempted to kill myself, and really hoped to die). At wave 2 the time frame for the item was changed to “In the past 6 months have you ever thought about or attempted to kill yourself?” (scored on the same scale as the wave 1 item).
Data Analytic Plan
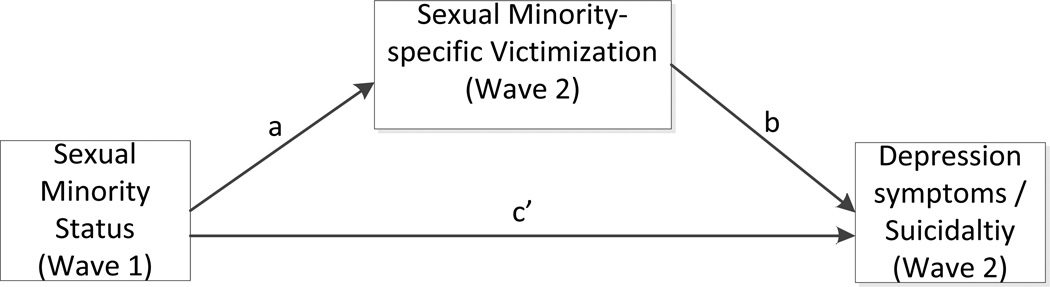
Mediation was tested using the PROCESS macro for SPSS (Hayes, 2012) and following the principles outlined by MacKinnon (2008). According to MacKinnon (2008) a significant effect from the predictor to the mediator (referred to as path a) and a significant effect from the mediator to the outcome (referred to as path b) are required to test for mediation. However, a significant direct effect from the predictor to the outcome (referred to as path c’) is not required (see Figure 1 for a conceptual depiction of paths a, b, and c’). While a direct effect is not required for mediation, it is included in the regression equation testing mediation.
Figure 1.
Conceptual Model for Mediation Analyses
Path a was estimated by regressing sexual minority-specific victimization (and covariates age, race, gender, and wave 1 depressive symptomatology) on sexual minority status. Paths b and c’ were estimated simultaneously by regressing each of the outcomes (depressive symptomatology and suicidality) on sexual minority status and sexual minority-specific victimization (and the covariates). The indirect or mediated effect was estimated by multiplying the unstandardized coefficients for paths a and b; the significance of a*b was determined by computing confidence intervals using bias-corrected bootstrapping as recommended by previous research (MacKinnon, Warsi, & Dwyer, 1995; Shrout & Bolger, 2002).
In the longitudinal mediation models the predictor was sexual minority status at wave 1, the mediator was sexual minority-specific victimization (experienced in the past six months) at wave 2, and the outcomes were depressive symptomatology and suicidality, both measured at wave 2 and both models controlled for wave 1 depressive symptomatology and demographics (sex, age, race). Sexual minority-specific victimization was measured at both waves however victimization at wave 2 was selected as the mediator in all models because it was the most accurate assessment of what happened between waves 1 and 2.
The ideal control variable in the suicidality model would be recent history of suicidality measured at wave 1 as opposed to recent history of depressive symptomatology measured at wave 1. However recent history of suicidality was not measured at wave 1. Instead lifetime history of suicidality was measured at wave 1 and past 6 month history of suicidality was measured at wave 2. Therefore, in the suicidality model, depressive symptomatology at wave 1 was entered as a covariate (just as it was in the mediation model in which depressive symptomatology at wave 2 was the dependent variable). This decision was made because the depression measure at both waves 1 and 2 asked about symptoms in the past week, whereas the suicidality item at wave 1 asked about lifetime history of suicidality. We did not predict that any variable measured in this study, in particular the mediated effect of past 6 month sexual minority-specific victimization, could predict suicidality at wave 2 over and above lifetime history of suicidality because lifetime history (measured at wave 1) would most likely account for the majority of variance of the past 6 month suicidality item (measured at wave 2). However, in an effort to determine the strength of the mediated effect and to inform future research design on how and when to best measure control variables, an exploratory model controlling for lifetime history of suicidality was run in addition to the primary model that controlled for wave 1 depressive symptomatology.
Results
Descriptive Statistics
Of the 197 participants who completed wave 1 measures, 189 completed wave 2. Twenty-nine percent of the sample was classified as sexual minority due to a self-reported status other than 100% heterosexual. Table 1 shows the breakdown of cell sizes by sexual minority status, race, and gender.
Table 1.
Sample Demographics
| Sexual minority | Heterosexual | Total | |
|---|---|---|---|
| Female | 47 (25%) | 87 (45%) | 134 (70%) |
| Male | 8 (4%) | 50 (26%) | 58 (30%) |
| Total | 55 (29%) | 137 (71%) | n = 192 |
| White | 12 (6%) | 53 (28%) | 65 (34%) |
| Racial/ethnic minority | 43 (23%) | 84 (43%) | 127 (66%) |
| Total | 55 (29%) | 137 (71%) | n = 192 |
Notes: All racial/ethnic minorities were collapsed into one minority group for reporting purposes in order to maintain confidentiality and conceal participants’ identities. Five participants did not report all demographic characteristics and have been excluded from the table.
Continuous variables were analyzed for skew and kurtosis. The victimization and suicidality variables were found to have positive skew and positive kurtosis, therefore log transformations were applied to these variables prior to analyses. Table 2 shows the descriptive statistics and difference tests for the primary variables of interest. As predicted, SMY reported higher levels of sexual minority-specific victimization, depressive symptoms, and suicidality. Also as predicted, depressive symptomatology, suicidality, and sexual minority-specific victimization were positively correlated within the sexual minority group; however, only sexual minority-specific victimization and depressive symptomatology were correlated within the heterosexual group (Table 3). Contrary to predictions and previous research, depressive symptomatology and suicidality were not correlated in the heterosexual group, which may be due to the extremely low base rate of suicidality in the heterosexual group.
Table 2.
Descriptive Statistics and Difference Tests for Wave 2 variables
| Measure | Sexual minority M (SD) |
Heterosexual M (SD) |
|
|---|---|---|---|
| SM victimization | .22 (.42) | .10 (.39) | t(181) = 2.29* |
| CESD | .71 (.51) | .55 (.38) | t(177) = 2.41** |
| Suicidality | .46 (1.04) | .10 (.37) | t(179) = 3.35** |
Note: SM victimization = sexual minority-specific victimization, CESD = depressive symptoms. Means are raw scores, not the log transformed variables used in difference tests and other analyses.
p < .05,
p = .001
Table 3.
Correlations among Variables at Wave 2 by Sexual Identity
| Measure | 1 | 2 | 3 |
|---|---|---|---|
| 1. SM victimization | ___ | .25** | .05 |
| 2. CESD | .66*** | ___ | .07 |
| 3. Suicidality | .30* | .53*** | ___ |
Note: Values above the diagonal are correlations within the heterosexual group; values below the diagonal are correlations within the sexual minority group. SM victimization = sexual minority-specific victimization, CESD = depressive symptoms;
p < .05,
p < .01,
p < .001
Mediation Analyses
Table 4 shows the results of the mediation model outlined in Figure 1 for depressive symptoms and suicidality. The requirement that paths a and b be significant was met for both models. Controlling for gender, age, race, and depressive symptomatology at wave 1, sexual minority-specific victimization at wave 2 significantly mediated the effect of sexual minority status on depressive symptomatology at wave 2 (B = .045, 95% CI: .0063, .15).
Table 4.
Mediation Results for Depressive Symptomatology and Suicidality
| Depressive symptomatology | Suicidality | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | B | SE | β | p | |
| Path a | .037 | .017 | .17 | .036 | .039 | .017 | .17 | .028 |
| Path b | 1.21 | .26 | .30 | < .001 | .22 | .11 | .16 | .036 |
| Path c’ | .039 | .060 | .04 | .52 | .058 | .025 | .19 | .019 |
| Indirect effect | .045 | .032 | 95% CI: .0063, .15 | .0086 | .0077 | 95% CI: .0003, .031 | ||
| Total R2 | .39 | < .001 | .11 | .0021 | ||||
Note: Age, race, gender, and wave 1 CESD score were entered as covariates in all above represented relationships.
Similarly, controlling for gender, age, race, and depressive symptomatology at wave 1, sexual minority-specific victimization at wave 2 significantly mediated the effect of sexual minority status on suicidality at wave 2 (B = .0086, 95% CI: .0003, .031). An exploratory model was run in which lifetime history of suicidality (measured at wave 1) replaced wave 1 depressive symptomatology as a covariate. The exploratory model did not meet the requirements for mediation because paths a and b were marginal to non-significant (path a: B = .04, p = .06; path b: B = .14, p = .15). The mediated effect of sexual minority specific-victimization on suicidality at wave 2 controlling for lifetime history of suicidality was significant within a 90% CI (B = .005, 90% CI: .0002, .02) but not significant within a 95% CI (B = .005, 95% CI: −.0007, .02).
Discussion
Recent research and government reports have identified SMY as an at-risk population and documented mental health disparities in this population (IOM, 2011, Marshal et al., 2011). The current project was designed to extend this research by using a longitudinal framework to identify one mechanism that is at least partially responsible for mental health disparities in SMY. Specifically, the present study examined the minority stress model as an explanatory framework for understanding the potential causes of disparities in SMY. The minority stress model proposes that the discrimination and violence, among other things, experienced by sexual minorities lead to negative health outcomes. Results were consistent with previous research in that SMY, compared to heterosexual peers, reported more sexual minority-specific victimization and a higher prevalence of depressive symptoms and suicidality. Longitudinal mediation models supported the minority stress hypothesis and found that elevated levels of sexual minority-specific victimization are partly responsible for the higher prevalence of depressive symptoms and suicidality in SMY.
The mediation model for depressive symptomatology was clear. Controlling for depressive symptoms measured six months prior, sexual minority-specific victimization mediated the relationship between sexual minority status and depressive symptoms 6 months later. The mediation model for suicidality was less clear. Due to a measurement limitation at baseline, recent history of suicidality could not be controlled for in the model. Therefore, two mediation models were run: one controlling for recent history of depressive symptoms and one controlling for lifetime history of suicidality, the former of which was significant while the latter was not. Suicidality is a difficult construct to study in small samples because it has a low base rate, which makes statistical modeling challenging. In addition, there may be only small shifts in rates or severity of suicidality across a six-month time interval that are difficult to capture without conducting a more in-depth clinical interview with participants, which was beyond the scope of this study. However, it is an important construct to study because of its severity; any level of suicidality is dangerous and can ultimately lead to loss of life if gone unrecognized or untreated. Results indicate that sexual minority-specific victimization does partially explain the relationship between sexual minority status and suicidality; however, the strength of the effect is likely smaller than that found for depressive symptoms.
Victimization of youth, particularly in the form of bullying, has become a focus of public health officials in the United States in recent years. Bullying is associated with myriad negative effects including increased absence from school, lower grades, reduced school belonging (a protective factor for suicidality), and risk for sexually transmitted infections (STIs) including HIV (Poteat, Mereish, DiGiovanni, & Koenig, 2011; Russell, Ryan, Toomey, Diaz, & Sanchez, 2011). In its extreme, bullying is frequently cited in media reports as a contributing factor in youth suicide. Our results support the connection between bullying and suicide at least among youth who think about suicide or who survive a suicide attempt. There is no study that has examined victimization among suicide completers. However, research using the Youth Risk Behavior Survey (YRBS) also has found that victimization is a significant predictor of suicide attempts (Shields, Whitaker, Glassman, Franks, & Howard, 2012). Furthermore, meta-analytic results show that the disparity between SMY and heterosexual youth for suicidality increases as the severity of suicidality increases (Marshal et al., 2011). For example, while SMY are about two times more likely to report suicidal ideation, they are over four times more likely to report a suicide attempt that required medical attention. It may be that these severe attempts are driven by feelings of hopelessness that can be triggered or exacerbated by sexual minority-specific victimization.
The specific mechanism(s) that explains how sexual minority-specific victimization leads to increased depressive symptoms and suicidality is beyond the scope of this study. However some recent research has delved more deeply into these relationships. For example, a cross-sectional survey of sexual minority adults found that internalized homonegativity (internalization of negative social attitudes about homosexuality) and rejection sensitivity mediate the relationship between sexual minority-specific victimization and depressive symptoms (Feinstein, Goldfried, & Davila, 2012). Taken together, this research and the present study suggest that, by experiencing sexual minority-specific victimization, SMY develop negative feelings about who they are as a person and learn to expect intolerance and rejection, which can lead to increases in depression and suicidality.
Our project specifically focused on sexual minority-specific victimization because our hypotheses related to explaining the disparities in depression and suicidality between SMY and heterosexual youth. However, it should be noted that both in the present data and in other research, sexual minority-specific victimization is correlated positively with depression in all youth, not just sexual minority youth. Even heterosexual youth are harmed by bullying based on a perceived, but not actual, sexual minority status. While minorities, both sexual minorities and racial/ethnic minorities, frequently are targeted for victimization that puts them at greater risk than non-minority peers, victimization in all youth is an important public health concern.
Some scholars have suggested that the culture in which youth today grow up is quite different from the culture in which previous generations have grown up and that there is a “declining significance of homophobia” experienced by today’s SMY (McCormack, 2012). It further has been suggested that researchers may actually increase destructive behavior patterns in SMY by focusing only on negative outcomes such as depression, suicidality, and substance use (Savin-Williams, 2005). The present study cannot answer the question of whether homophobia has increased or decreased during the past several decades nor can it address whether studying so called destructive behaviors increases or decreases the prevalence of such behaviors. However, it does show that homophobia and bullying still are present in adolescents’ lives today and that such homophobia has negative consequences for adolescent development. Homophobia in schools may be declining and a cultural shift towards increasing acceptance of sexual minorities is evidenced by increasing non-discrimination laws, legislative and popular approval of marriage equality measures, and the presence of student groups designed specifically to support SMY in some school districts (e.g., Gay Straight Alliances). However, there is overwhelming evidence that even in today’s potentially more accepting culture SMY are still at risk for bullying, sexual abuse, depression, suicidality, substance abuse, and school absence due to fear (CDC, 2011; Friedman et al., 2011; IOM, 2011; Marshal et al., 2008; 2011). Researchers should not seek to pathologize SMY, or any other at-risk population, but neither should they neglect the scientific investigation of disparities in SMY because there is a popular, yet unverified, perception that the significance of homophobia is declining in Western culture.
This study is not without limitations. We used a sub-sample of youth from a larger ongoing NIH-funded study with an open enrollment design that will recruit a total of 400 youth over a 4–5 year recruitment period. Although the current subsample represents only half of the total planned enrollment, with less statistical power than we will have when enrollment is completed, the statistically significant findings even after controlling for demographic covariates are notable. The sample size of the present study is currently too small to look at subgroups of SMY. Not all sexual minority subgroups experience the same level of risk. Research has found that SMY who identify as bisexual and “mostly heterosexual” are at greater risk for substance use and depression than youth who identify as “100% heterosexual or “100% homosexual” (Austin et al., 2004; Bostwick, Boyd, Hughes, & McCabe, 2010; Hughes, Szalacha, & McNair, 2010; Marshal et al., 2008; Marshal et al., 2011). Looking at differences between SMY subgroups is important but it requires very large sample sizes to divide any minority group into subgroups. Additionally, SMY who are racial/ethnic minorities may experience different risk factors than SMY who are not racial/ethnic minorities. In the present study, the sample was predominately African American (63%) but it is not known if African American SMY differ in meaningful ways from other racial/ethnic groups of SMY on the variables studied. An advantage of this study over other similar studies is that longitudinal data were collected. While the longitudinal design is certainly a strength, the length of time between measurement points was only 6 months. Future research should look at victimization and mental health in SMY over longer periods of time, and perhaps use individual trajectory modeling methodology (e.g., latent growth curve modeling; Bollen & Curran, 2006) to determine if victimization tends to increase or decrease and if the effects cumulate or dissipate over time.
When studying health disparities in an at-risk population it is easy to pathologize the entire population. However, it must be emphasized that in the present data and in the larger population, the overwhelming majority of SMY are happy, healthy, and well-adjusted with no significant symptoms of depression or history of suicidality. Resilience can be found in every at-risk population. As research closes in on the source or sources of health disparities, it is important to also study the source or sources of resilience in an at-risk population. What protects SMY, even SMY who face continual victimization, from developing mental health problems? Some studies have identified protective factors such as Gay Straight Alliances in schools (Hatzenbuehler, 2011) and family acceptance (Ryan, Russell, Huebner, Diaz, & Sanchez, 2010), but more research is needed in order to understand resiliency in SMY. Future research should focus on resilience factors proven to protect SMY in order to develop programs and interventions to improve the mental health of all SMY (see Haas et al., 2011 for a thorough review of the extant literature and specific suggestions for future research and interventions).
Many studies have identified the health disparities in SMY. This study contributes to this literature by providing strong evidence that sexual minority-specific victimization of SMY is partly responsible for the mental health disparities. These findings suggest that public policy initiatives that reduce bullying and hate crimes against SMY (e.g., stopbullying.gov) could have a significant impact on the health and well-being of this vulnerable population.
Acknowledgments
This research was funded by a grant from the National Institute on Drug Abuse (R01-DA026312; PI: Michael Marshal) and the first author was supported by a grant from the National Institute of Mental Health (T32-MH015169; PI: Gale Richardson).
Biographies
Chad M. Burton, Ph.D., Department of Psychiatry, University of Pittsburgh
Chad Burton is a Postdoctoral Associate at the University of Pittsburgh. He received his doctorate in social psychology from the University of Missouri. His primary research interests include the etiology of mental health and substance use disparities in sexual minority youth and interventions to reduce the disparities.
Michael P. Marshal, Ph.D., Department of Psychiatry, University of Pittsburgh
Michael P. Marshal is a licensed clinical psychologist and an Associate Professor of Psychiatry and Pediatrics at the University of Pittsburgh. He received his doctorate in clinical psychology from Arizona State University. His major research interests include substance use and mental health disparities among lesbian, gay, bisexual, and transgender adolescents and identifying associated risk and protective factors.
Deena J. Chisolm, Ph.D., Department of Pediatrics, The Ohio State University
Deena Chisolm is an Associate Professor in the Ohio State University College of Medicine Department of Pediatrics and a Principal Investigator in the Research Institute at Nationwide Children’s Hospital. She received her doctorate public health from the Ohio State University. Her major research interests include adolescent health, health literacy, and health disparities.
Gina S. Sucato, M.D., M.P.H., Department of Pediatrics, University of Pittsburgh
Gina S. Sucato, MD, MPH is an Assistant Professor at the University of Pittsburgh School of Medicine. She is board certified in general pediatrics and adolescent medicine. Her research interests cover a variety of aspects of adolescent reproductive health.
Mark S. Friedman, Ph.D., M.P.H., Graduate School of Public Health, University of Pittsburgh
Mark S. Friedman is an Assistant Professor of Public Health and Pediatrics at the University of Pittsburgh where he also received his doctorate in social work. His primary research interests include multiples forms of abuse perpetrated against sexual minority youth and translation of evidence-based interventions into real-world settings.
Footnotes
Contributions
CB conducted all data analyses and wrote most of the content contained in the manuscript. MM is the principal investigator on the project from which the data were derived. MM assisted with data analysis and manuscript preparation. DC is a co-investigator on the larger project from which the data were derived and director of one of the recruitment sites. DC assisted with participant recruitment and manuscript preparation. GS is the director of one of the recruitment sites, assisted in recruitment, and manuscript preparation. MF: assisted with hypothesis development and manuscript preparation.
All authors made significant contributions to the research presented in this article.
References
- Almeida J, Johnson RM, Corliss HL, Molnar BE, Azrael D. Emotional distress among LGBT youth: The influence of perceived discrimination based on sexual orientation. Journal of Youth and Adolescence. 2009;38:1001–1014. doi: 10.1007/s10964-009-9397-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin SB, Ziyadeh N, Fisher LB, Kahn JA, Colditz GA, Frazier AL. Sexual orientation and tobacco use in a cohort study of US adolescent girls and boys. Archives of Pediatrics and Adolescent Medicine. 2004;158:317–322. doi: 10.1001/archpedi.158.4.317. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: John Wiley and Sons; 2006. [Google Scholar]
- Bontempo DE, D'Augelli AR. Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths' health risk behavior. Journal of Adolescent Health. 2002;30:364–374. doi: 10.1016/s1054-139x(01)00415-3. [DOI] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, McCabe SE. Dimensions of Sexual Orientation and the Prevalence of Mood and Anxiety Disorders in the United States. American Journal of Public Health. 2010;100:468–475. doi: 10.2105/AJPH.2008.152942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention) Morbidity and Mortality Weekly Report: Sexual identity, sex of sexual contacts, and health-risk behaviors among students in grades 9–12: Youth risk behavior, surveillance, selected sites, United States, 2001–2009, Early release. 2011;Vol. 60 [PubMed] [Google Scholar]
- Feinstein BA, Goldfried MR, Davila J. The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of Consulting and Clinical Psychology. 2012;80:917–927. doi: 10.1037/a0029425. [DOI] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Guadamuz TE, Wei C, Wong CF, Saewyc EM, Stall R. A meta-analysis of disparities in childhood sexual abuse, parental physical abuse, and peer victimization among sexual minority and sexual nonminority individuals. American Journal of Public Health. 2011;101:1481–1494. doi: 10.2105/AJPH.2009.190009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Wolf C, Wissow LS, Woods ER, Goodman E. Sexual orientation and risk of suicide attempts among a representative sample of youth. Archives of Pediatrics and Adolescent Medicine. 1999;153:487–493. doi: 10.1001/archpedi.153.5.487. [DOI] [PubMed] [Google Scholar]
- Haas A, Eliason M, Mays VM, Mathy RM, Cochran SD, D’Augelli AR, Silverman MM, Fisher PW, Hughes TL, et al. Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: Review and recommendations. Journal of Homosexuality. 2011;58:10–51. doi: 10.1080/00918369.2011.534038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, bisexual youth. Pediatrics. 2011;127:896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf. [Google Scholar]
- Hershberger SL, D’Augelli AR. The impact of victimization on the mental health and suicidality of lesbian, gay, bisexual youths. Developmental Psychology. 1995;31:65–74. [Google Scholar]
- Hughes T, Szalacha LA, McNair R. Substance abuse and mental health disparities: Comparisons across sexual identity groups in a national sample of young Australian women. Social Science and Medicine. 2010;71(4):824–831. doi: 10.1016/j.socscimed.2010.05.009. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Erlbaum; 2008. [Google Scholar]
- MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behavioral Research. 1995;30:42–62. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, Thoma BC, Murray PJ, D’Augelli A, Brent DA. Suicidality and Depression Disparities between Sexual Minority and Heterosexual Youth: A Meta-Analytic Review. Journal of Adolescent Health. 2011;49:115–123. doi: 10.1016/j.jadohealth.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, Bukstein OG, Morse JQ. Sexual orientation and adolescent substance use: A meta-analysis and methodological review. Addiction. 2008;103(4):546–556. doi: 10.1111/j.1360-0443.2008.02149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack M. The declining significance of homophobia: How teenage boys are redefining masculinity and heterosexuality. New York: Oxford; 2012. [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat VP, Espelage DL. Predicting psychosocial consequences of homophobic victimization in middle school students. Journal of Early Adolescence. 2007;27:175–191. [Google Scholar]
- Poteat VP, Mereish EH, DiGiovanni CD, Koenig BW. The effects of general and homophobic victimization on adolescents’ psychosocial and educational concerns: The importance of intersecting identities and parent support. Journal of Counseling Psychology. 2011;58:597–609. doi: 10.1037/a0025095. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: Results of a population-based study. American Journal of Public Health. 1998;88:57–60. doi: 10.2105/ajph.88.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Joyner K. Adolescent sexual orientation and suicide risk: Evidence from a national study. American Journal of Public Health. 2001;91:1276–1281. doi: 10.2105/ajph.91.8.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Ryan C, Toomey RB, Diaz RM, Sanchez J. Lesbian, gay, bisexual, and transgender adolescent school victimization: Implications for young adult health and adjustment. Journal of School Health. 2011;81:223–230. doi: 10.1111/j.1746-1561.2011.00583.x. [DOI] [PubMed] [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT adults. Journal of Child and Adolescent Psychiatric Nursing. 2010;23:205–213. doi: 10.1111/j.1744-6171.2010.00246.x. [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC. The new gay teenager. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Shields JP, Whitaker K, Glassman J, Franks HM, Howard K. Impact of victimization on risk of suicide among lesbian, gay, bisexual high school students in San Francisco. Journal of Adolescent Health. 2012;50:418–420. doi: 10.1016/j.jadohealth.2011.07.009. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Swearer SM, Turner RK, Givens JE, Pollack WS. “You’re so gay!”: Do different forms of bullying matter for adolescent males? School Psychology Review. 2008;37:160–173. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2020. 2012 Retrieved 01/06/2012 from http://www.hhs.gov/ash/oah/resources-and-publications/healthy-people-2020.html.
- Williams T, Connolly J, Pepler D, Craig W. Peer victimization, social support, and psychosocial adjustment of sexual minority adolescents. Journal of Youth and Adolescence. 2005;34:471–482. [Google Scholar]