Abstract
The purpose of this study was to test the impact of two variables on post-binge eating negative emotion in a combined sample of women with anorexia nervosa (AN; n = 47) and bulimia nervosa (BN; n = 121). Participants completed two weeks of an ecological momentary assessment protocol during which they provided multiple daily ratings of overall negative affect and guilt and reported eating disorder behaviors including binge eating and self-induced vomiting. The results indicate that both overall negative affect and guilt exhibited a statistically significantly decrease in the hour immediately following binge eating episodes. The decrease in guilt, but not overall negative affect, was moderated by eating disorder diagnosis and the tendency to engage in self-induced vomiting. Specifically, individuals with BN reported a greater reduction in guilt than those with AN, and individuals who did not typically engage in self-induced vomiting reported more decreases in guilt than those who typically engaged in self-induced vomiting. This study extends the existing literature on the relationship between negative affect and eating disorder behaviors, suggesting guilt as a potentially relevant facet of negative affect in the maintenance of binge eating. In addition, the findings indicate that two individual differences, eating disorder diagnosis and self-induced vomiting, may influence the trajectory of guilt following binge eating episodes.
Keywords: anorexia nervosa, bulimia nervosa, negative affect, guilt, ecological momentary assessment
1. Introduction
Binge eating is characterized by two key features: (1) eating within a discrete period of time an amount of food that is much more than what most others would eat under similar circumstances; and (2) a subjective experience of loss of control over eating (APA, 2000). It occurs across eating disorder diagnoses, in individuals with other psychiatric diagnoses, and in non-clinical populations (e.g., Hudson et al., 2007; McElroy et al., 2011). Binge eating is a core diagnostic feature of binge eating disorder and bulimia nervosa (BN) and may also be present in anorexia nervosa (AN). Binge eating in AN and BN is often accompanied by compensatory behaviors (e.g., self-induced vomiting, misuse of laxatives/diuretics, dietary restriction, excessive exercise) in an attempt to prevent weight gain, and these compensatory behaviors are thought to be associated with the body weight and shape concerns (i.e., fear of weight gain in AN and overvaluation of weight/shape in AN and BN) that characterize these disorders (Fairburn, 2008).
Given that many individuals with AN and BN exhibit a consistent pattern of binge eating despite the presumably distressing nature of the behavior and its consequences in eating disorder populations, researchers have sought to understand the processes underlying the maintenance of binge eating. In particular, affect regulation models have received substantial attention in empirical studies testing the idea that binge eating is maintained via negative reinforcement (i.e., reduction of aversive affective states). For instance, both Heatherton and Baumeister’s (1991) Escape Theory and the recently proposed emotional dysregulation model of AN (Haynos and Fruzzetti, 2011) suggest that binge eating results in temporary reductions in negative affect. Consistent with these theories, an extensive body of research indicates that binge eating is more likely to occur during states of elevated negative affect (e.g., Crosby et al., 2009; Engelberg et al., 2007; Hilbert and Tuschen-Caffier, 2007; Smyth et al., 2007). In addition, the two largest studies assessing momentary affective states in the natural environment in AN (i.e., Engel at al., 2010) and BN (i.e., Smyth et al., 2007) indicate that negative affect decreases over the four hours following binge eating episodes. However, a recent meta-analysis of negative affect immediately pre- and post-binge eating in BN suggested that negative affect may increase after episodes of binge eating (Haedt-Matt and Keel, 2011). It is possible that there are individual differences that moderate affective changes following binge eating episodes. Specifically, some individuals with eating disorders may tend to experience a reduction in negative affect following binge eating while others do not, making it difficult to broadly characterize the function of binge eating in individuals with eating disorders.
The objective of this study was to test two individual difference variables that may account for variability in post-binge eating negative affect using data drawn from two ecological momentary assessment (EMA) studies, which have been described previously (Engel et al., 2010; Smyth et al., 2007). Specifically, two theoretically relevant moderators of post-binge eating changes in negative affect were examined: (a) eating disorder diagnosis (AN and BN) and (b) propensity to engage in compensatory self-induced vomiting. Additionally, we sought to extend the existing literate on affect and binge eating by comparing overall negative affect and the specific facet of guilt, both of which are of particular conceptual relevance to binge eating (e.g., Sanftner and Crowther, 1998). While negative affect is a broad construct comprised of several distinct affective states, guilt, a specific facet of negative affect, is a complex emotion that is elicited by a cognitive process of self-evaluation that is driven by the belief that one could have prevented a negative outcome by exerting greater behavioral control (Schmader and Lickel, 2006; Tilghman-Osborne et al., 2010). Given that binge eating is a behavior that is defined in large part by loss of control, guilt may be of central importance to emotional experiences following binge eating. In contrast, negative affect includes guilt and other more basic emotions (e.g., sadness, fear) for which cognitive processes are less central (Lewis, 2008). As such, the affective impact of binge eating may be stronger for emotions that depend more heavily on self-evaluative processes (e.g., guilt). Thus, compared to the broader construct of negative affect, the facet of guilt may be more specifically influenced by binge eating.
2. Method
2.1. Participants
Participants came from two EMA studies, one in women with AN (data collected in Fargo, Minneapolis, Chicago; Engel et al., 2010) and one in women with BN (data collected in Fargo; Smyth et al., 2007). Demographics and information regarding the severity of illness and psychosocial functioning are displayed in Table 1. Participants were required to be female and at least 18 years of age and meet Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA, 2000) criteria for BN, full-threshold AN, or sub-threshold AN (meeting all AN criteria except: (1) Criteria B-D, but BMI 17.6–18.5, (2) Criteria A-C, but no amenorrhea, or (3) Criteria A and D, but no body image disturbance and intense fear of gaining weight or becoming fat). Only participants who reported engaging in binge eating and had at least one affect rating within one hour post-binge eating episode while enrolled in the study procedures were included in the present study. This requirement resulted in 121 women with BN, which represents 92.4% of the original sample of 131 participants. For AN, 47 women were included (15 restricting type1, 32 binge eating-purging type), which represents 39.8% of the original sample of 118 individuals. A total of 27 of these 47 (57.4%) individuals with AN met full DSM-IV criteria, and the remaining met sub-threshold criteria. Additional details about co-occurring diagnoses, treatment history, and symptom severity have been reported elsewhere (Engel et al., 2010; Smyth et al., 2007).
Table 1.
Participant Demographics
| Anorexia Nervosa (n = 47)
|
Bulimia Nervosa (n = 120–121†)
|
||||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Age (years) | 25.68 | 8.27 | 25.21 | 7.55 | |
| BMI (kg/m2)a | 16.99 | 0.95 | 24.00 | 5.21 | |
| EDE Global | 3.08 | 1.20 | 3.27 | 1.13 | |
| EDE Restraint | 3.15 | 1.49 | 3.00 | 1.56 | |
| EDE Eating Concern | 2.57 | 1.30 | 2.28 | 1.38 | |
| EDE Shape Concern | 3.34 | 1.53 | 3.78 | 1.32 | |
| EDE Weight Concerna | 3.26 | 1.59 | 4.00 | 1.39 | |
|
| |||||
| n | % | n | % | ||
|
| |||||
| Ethnicity (Caucasian) | 45 | 95.74 | 116 | 96.67 | |
| Marital Status (single/never married) | 31 | 65.96 | 79 | 65.83 | |
| Education (any post-secondary) | 42 | 89.36 | 106 | 88.33 | |
Note. BMI = Body Mass Index; EDE = Eating Disorder Examination interview.
Demographic information (except for BMI) is missing for one participant.
Diagnostic groups differed significantly in BMI (t(165) = 9.15, p<.001) and EDE Weight Concern (t(166) = 2.97, p<.01).
All other diagnostic comparisons were non-significant (p>.05).
2.2. Measures
2.2.1. Diagnostic Interview
Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition-Eating Disorder Module (SCID-I/P). The SCID-I/P (First et al., 1995) is a semi-structured interview that assesses DSM-IV Axis I disorders and was used to make eating disorder and other Axis I diagnoses. The interview was administered by trained assessors. In the AN sample, a subsample of 30 interviews were rated by an independent assessor for reliability and yielded a kappa coefficient of .929. In the BN sample, a subsample of 25 randomly selected interviews was independently rated and yielded a kappa coefficient of 1.00.
Eating Disorders Examination (EDE). The EDE (Fairburn and Cooper, 1995) is a structured interview that provides an index of eating pathology in the form of a global score and four subscales (restraint, eating concern, shape concern, and weight concern). In addition, the frequency of binge eating and purging are assessed over the previous 3 months. The EDE has demonstrated good reliability and validity (Berg et al., 2012; Fairburn, 2008). In the AN sample, 25% of interviews were recorded and rated by a second independent assessor, finding intraclass correlation coefficients for the EDE subscales ranging from .894 to .997. In the BN sample, 20% of interviews were rated by a second assessor, with intraclass correlation coefficients ranging from .65 to .98.
2.2.2. EMA Measures
Positive and Negative Affect Schedule (PANAS). This measure (Watson et al., 1988; Watson and Clark, 1994) assesses positive affect and negative affect broadly, and a subset of eight negative affect items from the full PANAS-X (afraid, ashamed, disgusted, distressed, nervous, dissatisfied with self, sad, and angry at self) served as a measure of momentary negative affect. These items were selected from several of the lower order emotion scales due to their high factor loadings (Watson and Clark, 1994) and conceptual relevance to eating disorders. Participants rated the extent to which they currently felt each of these emotions on a 5-point scale, ranging from 1 (“not at all”) to 5 (“extremely”). Items were summed for a total score representing overall negative affect. Among the eight items assessing negative affect were three items from the guilt facet of negative affect (ashamed, dissatisfied with self, and angry at self). The sum score of these items was the measure of momentary guilt. The guilt facet of the PANAS-X contains a total of six items; only the three listed were administered in this study. The coefficient alpha of the eight items comprising the negative affect scale was .91, and the coefficient alpha of the three items comprising the guilt facet was .84.
Eating Disorder Checklist. At each EMA recording (schedule described below), participants indicated whether they engaged in eating disorder behaviors including binge eating and self-induced vomiting using a checklist presented via palmtop computers. Definitions of binge eating (“an amount of food that you consider excessive, or an amount of food that other people would consider excessive, with an associated loss of control or the feeling of being compelled to eat”) and examples of what constituted objectively large amounts of food were provided to participants. Thus, binge eating as assessed in this study included only objective binge eating episodes (i.e., loss of control while eating an objectively large amount of food) and not subjective binge eating episodes (i.e., loss of control while eating an amount of food that is not objectively large).
2.3. Procedure
Participants in both studies attended two assessment visits and completed two weeks of an EMA protocol. These studies were approved by local Institutional Review Boards. Participants were recruited through advertisements at clinical, community, and campus locations. Individuals interested in participating were screened over the telephone to determine their eligibility. Eligible individuals participated in an informational meeting during which they received information about the studies and provided written informed consent. Over the course of two assessment visits, participants completed a battery of assessments including semi-structured interviews, self-report questionnaires, and screenings to ensure medical stability.
At the end of their first assessment visit, participants were instructed on the use of the palmtop computers to make EMA recordings. They then completed practice ratings over the next two days. At their second assessment visit, they received feedback regarding compliance rates and further instruction, when necessary. Participants then completed the EMA protocol over the next two weeks. Participants were compensated $200 for completing the two-week assessment period with an additional $50 bonus for reaching specific compliance targets.
The EMA assessment protocol for the two studies included signal contingent recording, interval contingent recording, and event contingent recording (Wheeler and Reis, 1991). For signal contingent recordings, the palmtop computers alerted participants to complete EMA ratings at six semi-random times of the day that were within 20 minutes of six “anchor” times (8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m.). For event contingent recordings, participants made EMA ratings immediately following the occurrence of specific behaviors (e.g., binge eating and self-induced vomiting), which were identified by the researchers and provided to participants through a list attached to the palmtop computer. If participants reported a binge eating episode at a signal or event contingent recording, they also indicated how much time (in minutes) had passed since the binge eating episode occurred. The PANAS and Eating Disorder Checklist were included in all of these recordings. For interval contingent recordings, participants provided EMA PANAS ratings at the end of each day.
2.4. Statistical Analyses
Mixed effects models were used to evaluate the two potential moderators. These models include fixed effects to test for relationships between variables of interest and random effects to estimate variation attributable to sampling error (Singer and Willett, 2003). This analysis takes into consideration the dependency of EMA data arising from repeated measurement. PANAS negative affect and the guilt facet were the dependent variables in two separate analyses. Although these two constructs overlap (i.e., the items assessing guilt are subsumed within the assessment of overall negative affect), separate analyses with these two variables were conducted because guilt is a conceptually distinct, specific facet of negative affect. Time since the occurrence of a binge eating episode was the independent variable in both analyses, with the post-binge eating period restricted to a maximum of one hour. Binge eating episodes were located in time using data participants provided in the moment regarding how much time had passed between the occurrence of the episode and the affect rating they were making. Finally, eating disorder diagnosis (AN or BN) and whether self-induced vomiting occurred within an hour of the binge eating episode were the two dichotomous moderator variables.
Negative affect scores (and the specific guilt facet), eating disorder diagnosis, and the occurrence of self-induced vomiting were centered on their respective grand means. Centering the occurrence of self-induced vomiting on each individual’s mean (i.e., person-centering rather than grand mean-centering) would have allowed a within-person comparison of negative affect and guilt following binge eating on occasions with and without self-induced vomiting; however, the results of a descriptive analysis of the tendency to engage in self-induced vomiting in the hour following binge eating revealed a bimodal distribution, with individuals either consistently engaging in or not engaging in self-induced vomiting. As a result, this approach was not utilized. Instead, centering on the grand mean allowed for a comparison of individuals who tend to engage in self-induced vomiting within an hour after binge eating with those who do not, making it a person- rather than situation-level comparison.
Models included a random intercept (allowing individuals to vary about their own average level of negative affect) and fixed effects to assess the relationship between time, diagnosis, self-induced vomiting, and negative affect, including all two-way interactions (time x diagnosis; time x self-induced vomiting; diagnosis x self-induced vomiting) and the three-way interaction (time x diagnosis x self-induced vomiting). Estimates in the models were evaluated with statistical significance set at p < .05. Analyses were conducted using SPSS Version 19.0.
3. Results
A total of 1336 PANAS ratings were completed within 1-hour after binge eating episodes. These ratings occurred following a total of 1033 separate binge eating episodes. The bulk of the PANAS ratings (72.9%) and binge eating episodes (75.0%) were reported by individuals with BN. A total of 51.1% of individuals with AN and 82.6% of individuals with BN reported inducing vomiting within one hour of at least one binge eating episode.
3.1 Post-Binge Eating Changes in Negative Affect
The first model examined the effect of time on PANAS negative affect in an unconditional growth model, which indicated the presence of a main effect of time (t(1143.28) = −4.35, p < .001). Negative affect decreased during the first hour after binge eating by approximately 2.46 points (95% confidence interval: 1.35–3.57), decreasing from an estimated mean of 25.75 at the time of binge eating to 23.29 one hour later.
Next, the effects of time, diagnosis, self-induced vomiting and their interactions were entered simultaneously. The three-way interaction was not significant (t(1051.77) = 1.46, p = .144), so it was removed. The results of the remaining model indicated that time and diagnosis did not interact to predict negative affect; individuals with AN and BN experienced similar patterns of negative affect following episodes of binge eating (Table 2). Similarly, time and self-induced vomiting did not interact to predict negative affect, indicating that the tendency to engage in self-induced vomiting was not related to specific negative affect patterns during the 1-hour interval after binge eating episodes. There were also no main effects of time, self-induced vomiting, or diagnosis and no self-induced vomiting by diagnosis interaction.
Table 2.
Linear Mixed Model Results of PANAS Negative Affect and Guilt
| Parameter | Negative Affect
|
Guilt
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | df | p | Estimate | SE | t | df | p | |
| Intercept | 25.63 | 0.64 | 40.23 | 237.03 | <.001 | 10.94 | 0.26 | 41.84 | 247.64 | <.001 |
| Time | −2.27 | 0.58 | −3.90 | 1165.54 | <.001 | −0.84 | 0.25 | −3.32 | 1192.71 | <.001 |
| SIV | −0.58 | 0.61 | −0.96 | 1086.18 | .340 | −0.40 | 0.27 | −1.48 | 1122.36 | .138 |
| Dx | −1.89 | 1.43 | −1.33 | 241.40 | .186 | −0.08 | 0.59 | −0.14 | 252.80 | .888 |
| Time x SIV | 1.30 | 1.11 | 1.17 | 1090.20 | .242 | 1.09 | 0.49 | 2.23 | 1122.98 | .026 |
| Time x Dx | −2.47 | 1.29 | −1.92 | 1116.99 | .056 | −1.32 | 0.56 | −2.33 | 1157.11 | .020 |
| SIV x Dx | 0.87 | 0.73 | 1.20 | 987.97 | .231 | 0.37 | 0.32 | 1.14 | 1029.44 | .253 |
Note. SIV = self-induced vomiting (coded 0 for absent and 1 for present); Dx = diagnosis (coded 0 for anorexia nervosa and 1 for bulimia nervosa); significance evaluated at a p-value of .05, represented by bolded type.
3.2 Post-Binge Eating Changes in Guilt
The second mixed model evaluated the guilt facet of PANAS negative affect. The results of the unconditional growth model indicated that there was a main effect of time (t(1177.90) = −3.85, p < .001) such that individuals experienced a decrease in guilt in the hour after binge eating. Guilt decreased during that hour by approximately 0.96 points (95% confidence interval: 0.47–1.44), decreasing from an estimated mean of 11.01 at the time of binge eating to 10.05 one hour later.
Next, time, diagnosis, self-induced vomiting and their interactions were entered simultaneously. Because the three-way interaction was again not significant (t(1086.38) = 0.93, p = .355), it was removed. The parameter estimates in the resulting model were very similar to those in the model using overall negative affect; however, the interaction parameters that pertained to the two potential moderators were statistically significant (Table 2) and are depicted in Figure 1. Specifically, the interaction of time and diagnosis indicated that individuals with BN experienced a significantly greater decrease in their levels of guilt in the hour following binge eating episodes compared to individuals with AN. The interaction of time and self-induced vomiting was also significant. An examination of the interaction suggested that individuals who tended not to engage in self-induced vomiting experienced more of a decrease in their levels of guilt than individuals who tended to engage in self-induced vomiting. There were no main effects of time, self-induced vomiting, or diagnosis and no self-induced vomiting by diagnosis interaction. In order to quantify the effect size of the significant interactions, pseudo-R2 statistics were calculated (Singer and Willett, 2003) and indicated that the time by diagnosis interaction accounted for 1.02% of the residual variance, and the time by self-induced vomiting interaction accounted for 0.74% of the residual variance.
Figure 1.
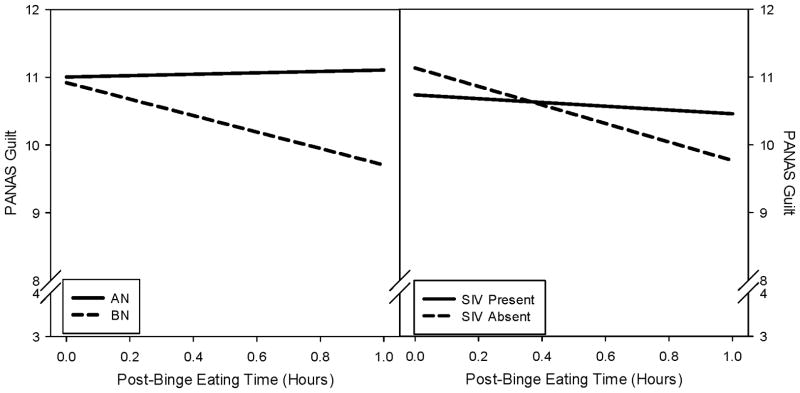
These figures display guilt during the 1-hour post-binge eating period as a function of eating disorder diagnosis (AN: anorexia nervosa; BN: bulimia nervosa) and tendency to engage in self-induced vomiting (SIV).
4. Discussion
This study aimed to test two potential moderators of post-binge eating negative affect trajectories in order to identify individual differences that might account for variability in these trajectories. The results indicate that both overall negative affect and the guilt facet of negative affect decreased during the hour following binge eating episodes; however, changes in guilt, and not overall negative affect, were moderated by eating disorder diagnosis and the tendency to engage in self-induced vomiting. Specifically, individuals with BN experienced a decrease in guilt in the hour following binge eating episodes whereas individuals with AN did not. In addition, individuals who tended not to engage in self-induced vomiting in the hour following binge eating episodes experienced a decrease in guilt whereas those who did engage in self-induced vomiting did not. These findings suggest that both ED diagnosis and the tendency to engage in self-induced vomiting are associated with post-binge eating changes in guilt, but not the broader construct of negative affect.
The differences found between AN and BN in momentary guilt trajectories following binge eating are consistent with research suggesting that individuals with BN report more emotional reactivity than individuals with AN (Forbush and Watson, 2006), although it should be noted that the similar pattern for broad negative affect was not found. In the present study, binge eating was more strongly linked to reductions in guilt in BN than AN, which suggests that binge eating may function differently in terms of regulating guilt in these diagnostic groups. It is possible that binge eating is more reinforcing to individuals with BN, whereas restrictive eating behaviors are more reinforcing to individuals with AN (Kaye et al., 2010). It is possible that by virtue of being low weight, individuals with AN, regardless of subtype, find the specific stimulus of food to be less rewarding than do individuals with BN. Unfortunately, this study lacked adequate statistical power to test for differences between AN subtypes; future studies should investigate whether post-binge guilt trajectories differ between AN subtypes. A number of other factors may account for this finding. Among these factors may be various qualities of binge eating episodes. For instance, the amount or types of food eaten may affect the magnitude of guilt experienced and/or the extent to which the guilt is reduced. These factors may vary by eating disorder diagnosis (e.g., size of binge eating episodes and their macronutrient composition may differ across diagnoses) and should therefore be the subject of future investigations.
Some authors have posited that self-induced vomiting serves to reduce negative affect produced from binge eating (Haedt-Matt and Keel, 2011; Schupak-Neuberg and Nemeroff, 1993). This study indicates that individuals who tend to engage in self-induced vomiting during the hour following binge eating do not experience as great a reduction in guilt as do individuals who do not induce vomiting during the first hour. There are several possible explanations for this finding. It is possible that individuals who induce vomiting in the hour following binge eating do so because they experience less of a reduction in guilt related to the binge eating episode; self-induced vomiting may be an additional attempt to decrease persistent guilt. Alternatively, it may be that those who engage in self-induced vomiting in the hour after binge eating actually increase guilt as a result of vomiting, a behavior that is often emotionally aversive and may be experienced as an additional loss of control. Yet another possibility is that the tendency to engage in self-induced vomiting is simply a marker of greater eating disorder severity, which may limit guilt reduction following binge eating.
The findings of this study highlight the utility of investigating facets of overall negative affect, which is a relatively broad construct comprised of a number of specific emotional states (e.g., guilt). Guilt was also investigated in this study in light of the empirical and theoretical relevance of this state and related emotions to eating disorder psychopathology (e.g., Sanftner and Crowther, 1998). Guilt is a self-conscious emotion (Tracy and Robins, 2004) involving a judgment of having failed to prevent a negative event from occurring, that requires a cognitive process, contrasting it with more basic emotions like sadness and fear, for which cognitive processes are less central (Lewis, 2008) and the emotions less self-conscious. If the process of binge eating is associated with decreased self-awareness through the narrowing of attention to the immediate external environment, as posited by Heatherton and Baumeister (1991), emotions like guilt that rely on a self-evaluative process may be impacted by binge eating more than other more basic emotions.
This study is one of only a few investigations examining the relationship between momentary affective states and eating disorder behaviors in a combined AN/BN sample. The findings provide support for the distinction between AN and BN with respect to the experience of guilt during the first post-binge eating hour; however, it is unknown what aspect of this diagnostic difference is responsible for the different guilt trajectories observed. Additional factors that were not assessed in this study may influence the relationship between binge eating, self-induced vomiting, and guilt. For instance, duration of illness information was not available, and it is possible that the function of binge eating changes over the course of illness. In addition, due to low variability in the probability of engaging in self-induced vomiting within the hour after binge eating episodes, this variable was investigated at the individual difference level. As a result, intra-individual variability in self-induced vomiting was statistically treated as error. Future studies should investigate intra-individual variability in addition to the other relevant covariates. In addition, it was somewhat unexpected that 15 individuals with ANr (20.5% of the total ANr sample) reported objective binge eating episodes at least once during the two weeks of EMA. All participants were provided with detailed instructions regarding the definition of such episodes, but it is unknown how strictly participants followed these instructions. Another limitation of the current study is the possibility of reactivity to the EMA procedure (i.e., participants could alter their behavior due to the increased self-monitoring required by EMA). Although previous research indicates that such reactivity is minimal among those with eating disorders (Stein and Corte, 2003), it is unknown whether EMA procedures affect guilt uniquely. The shortened version of the PANAS negative affect and guilt facet scales also represent a potential limitation of this study, as they may not assess the constructs of interest as completely as the full scales. Finally, while the ethnic diversity of the sample reflects the geographic regions from which it was drawn, the limited ethnic diversity may reduce generalizability.
In sum, this study identified two factors that may account for differences in post-binge eating changes in guilt: eating disorder diagnosis and the tendency to engage in self-induced vomiting. The description of such moderators aids in the understanding of the function of binge eating and how it might differ among individuals with eating disorders. It appears that some individuals, by virtue of the constellation of symptoms that comprise their eating disorders and the behaviors that tend to accompany their binge eating episodes, experience different trajectories of guilt after binge eating. Knowledge of factors that distinguish individuals by the processes implicated in the maintenance of their disorders will ultimately help target specific interventions to specific processes. Future research should continue to investigate the functional nature of eating disorder behaviors (e.g., binge eating, purging, etc.) with regard to emotion. Given inconsistencies in the literature regarding the potentially negatively reinforcing functions of binge eating (e.g., Haedt-Matt and Keel, 2011, Smyth et al., 2007), careful consideration should be given to methodological issues that would facilitate the detection and explication of these functional relationships.
Acknowledgments
Role of the funding source
This research was supported by the following sources: R01 MH059674; T32 MH082761.
Footnotes
AN restricting type is not characterized by the regular occurrence of episodes of binge eating or purging, although they may occasionally occur (APA, 2000).
Contributors
Drs. De Young, Lavender, and Wonderlich led the manuscript development. Dr. Crosby assisted with statistical analyses and managed the databases. Drs. Wonderlich, Crosby, Engel, Mitchell, Crow, Peterson, and Le Grange designed the study. All authors contributed to and approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kyle P. De Young, University of North Dakota
Jason M. Lavender, Neuropsychiatric Research Institute and University of North Dakota School of Medicine and Health Sciences
Stephen A. Wonderlich, Neuropsychiatric Research Institute and University of North Dakota School of Medicine and Health Sciences
Ross D. Crosby, Neuropsychiatric Research Institute and University of North Dakota School of Medicine and Health Sciences
Scott G. Engel, Neuropsychiatric Research Institute and University of North Dakota School of Medicine and Health Sciences
James E. Mitchell, Neuropsychiatric Research Institute and University of North Dakota School of Medicine and Health Sciences
Scott Crow, University of Minnesota.
Carol B. Peterson, University of Minnesota
Daniel Le Grange, The University of Chicago.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington DC: APA Press; 2000. Text Revision. [Google Scholar]
- Armey MF, Crowther JH, Miller IW. Changes in ecological momentary assessment reported affect associated with episodes of nonsuicidal self-injury. Behavior Therapy. 2011;42:579–88. doi: 10.1016/j.beth.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. International Journal of Eating Disorders. 2012;45:428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47:181–88. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel SG, Crosby RD, Wonderlich SA, Crow S, Le Grange D, Mitchell JE, et al. Ecological momentary assessment of eating disorder behavior and affect in samples of AN and BN participants. Presented at the 16th Annual Meeting of the Eating Disorders Research Society; Boston. October 2010. [Google Scholar]
- Engelberg MJ, Steiger H, Gauvin L, Wonderlich SA. Binge antecedents in bulimic syndromes: An examination of dissociation and negative affect. International Journal of Eating Disorders. 2007;40:531–6. doi: 10.1002/eat.20399. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008. [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. 12. New York: Guilford; 1995. pp. 317–360. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCIDI/P) New York: Biometrics; 1995. [Google Scholar]
- Forbush K, Watson D. Emotional inhibition and personality traits: A comparison of women with anorexia, bulimia, and normal controls. Annals of Clinical Psychiatry. 2006;18:115–21. doi: 10.1080/10401230600614637. [DOI] [PubMed] [Google Scholar]
- Grilo CM. Recent research of relationships among eating disorders and personality disorders. Current Psychiatry Reports. 2002;4:18–24. doi: 10.1007/s11920-002-0007-8. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–81. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia Nervosa as a disorder of emotion dysregulation: Evidence and treatment implications. Clinical Psychology: Science and Practice. 2011;18:183–202. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: A naturalistic comparison of binge eating disorder and bulimia nervosa. International Journal of Eating Disorders. 2007;60:521–30. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiology and Behavior. 2008;94:121–35. doi: 10.1016/j.physbeh.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Wagner A, Fudge JL, Paulus M. Neurocircuitry of eating disorders. In: Adan RAH, Kaye WH, editors. Behavioral neurobiology of eating disorders. Berlin: Spinger-Verlag; 2010. pp. 37–57. [Google Scholar]
- Lewis M. Self-conscious emotions: Embarrassment, pride, shame, and guilt. In: Lewis M, Haviland-Jones JM, Feldman Barrett L, editors. Handbook of emotions. New York: The Guilford Press; 2008. pp. 742–56. [Google Scholar]
- McElroy SL, Frye MA, Hellemann G, Altshuler L, Leverich GS, Suppes T, et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. Journal of Affective Disorders. 2011;128:191–8. doi: 10.1016/j.jad.2010.06.037. [DOI] [PubMed] [Google Scholar]
- O’Brien KM, Vincent NK. Psychiatric comorbidity in anorexia and bulimia nervosa: Nature, prevalence, and causal relationships. Clinical Psychology Review. 2003;23:57–74. doi: 10.1016/s0272-7358(02)00201-5. [DOI] [PubMed] [Google Scholar]
- Safer D, Telch C, Chen E. Dialectical behavior therapy for binge eating and bulimia. New York NY: Guilford Press; 2009. [Google Scholar]
- Sanftner JL, Crowther JH. Variability in self-esteem, moods, shame, and guilt in women who binge. International Journal of Eating Disorders. 1998;23:391–7. doi: 10.1002/(sici)1098-108x(199805)23:4<391::aid-eat6>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Schmader T, Lickel B. The approach and avoidance function of guilt and shame emotions: Comparing reactions to self-caused and other-caused wrongdoing. Motivation and Emotion. 2006;30:43–56. [Google Scholar]
- Schupak-Neuberg E, Nemeroff CJ. Disturbance in identity and self-regulation in bulimia nervosa: Implications for a metaphorical perspective of “body as self. International Journal of Eating Disorders. 1993;13:335–47. doi: 10.1002/1098-108x(199305)13:4<335::aid-eat2260130402>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willet JB. Modeling change and event occurrence. Oxford: University Press; 2003. Applied longitudinal data analysis. [Google Scholar]
- Smyth J, Wonderlich SA, Heron K, Sliwinski M, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress predict binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–38. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stein KF, Corte CM. Ecological momentary assessment of eating-disordered behaviors. International Journal of Eating Disorders. 2003;34:349–60. doi: 10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]
- Steiner H, Lock J. Anorexia nervosa and bulimia nervosa in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:352–9. doi: 10.1097/00004583-199804000-00011. [DOI] [PubMed] [Google Scholar]
- Tilghman-Osborne C, Cole DA, Felton JW. Definition and measurement of guilt: Implications for clinical research and practice. Clinical Psychology Review. 2010;30:536–46. doi: 10.1016/j.cpr.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy JL, Robins RW. Putting the self into self-conscious emotions: A theoretical model. Psychological Inquiry. 2004;15:103–25. [Google Scholar]
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule – Expanded form. The University of Iowa; 1994. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins types and uses. Journal of Personality. 1991;59:339–54. [Google Scholar]
- Wonderlich SA, Engel SG, Peterson CB, Robinson MD, Crosby RD, Mitchell JE, et al. Examining the conceptual model of Integrative Cognitive-Affective Therapy for BN: Two assessment studies. International Journal of Eating Disorders. 2008;41:748–54. doi: 10.1002/eat.20551. [DOI] [PubMed] [Google Scholar]


