Abstract
Hospital readmission is an important contributor to total medical expenditures and is an emerging indicator of quality of care. Diabetes, similar to other chronic medical conditions, is associated with increased risk of hospital readmission. Risk factors include previous hospitalization, extremes in age, and socioeconomic barriers. Preliminary studies suggest that acute and/or chronic glycemic control may be of importance when diabetes is the primary diagnosis or when it is a comorbidity. Very limited evidence from prospective randomized controlled trials aimed at improving glycemic control is available. However, whether one concludes that inpatient or outpatient glycemic control is partly responsible for reduced hospitalizations, attention to glycemic control in the hospital may facilitate sustained glycemic control post-discharge. Limited prospective and retrospective evidence suggest that the involvement of a diabetes specialist team may improve readmission rates, but attention to more generalized comprehensive approaches may also be worthwhile. Prospective interventional studies targeting interventions for improving glycemic control are needed to determine whether glycemic control impacts readmission rates.
Keywords: glycemic control, hemoglobin A1c, hospital, inpatient, readmission, rehospitalization
Introduction
A significant proportion of hospital costs are attributable to a small percentage of patients, particularly those with chronic medical conditions.1,2 These costs are, in large part, due to repeated hospitalizations for the same condition.3 Approximately 20% of all hospitalized Medicare patients are readmitted within 30 days, and 34% are readmitted within 90 days of discharge.4 Prevention of unplanned hospital readmission has therefore received increasing attention as one way of reducing hospital costs. For example, the Medicare Payment Advisory Commission has recommended reduced reimbursement rates for patients having early rehospitalizations for congestive heart failure (CHF).5
The purpose of this article is to identify predictors of unplanned hospital readmissions and to describe the role of the diagnosis of diabetes and glycemic control. Then the paper will describe general measures and diabetes-specific interventions to prevent readmission.
Role of Chronic Medical Conditions
A large Medicare study revealed that the most common conditions that require rehospitalization within 30 days of discharge are CHF, pneumonia, and chronic obstructive pulmonary disease and that medical patients are more likely to require readmission than surgical patients.4 Readmission is difficult to compare across studies because it is defined nonuniformly in terms of the reason for readmission (index condition versus any reason), duration of follow-up, planned versus unplanned, and preventable versus not preventable.6 Algorithms for identifying patients at risk of readmission have been published.7,8 Variables such as increasing age, low socioeconomic status, increased geographic distance, and previous admission in the past 3 years were identified as being predictive of readmission.8 Comorbid medical conditions that were associated with readmission included chronic obstructive pulmonary disease, alcoholism, diabetes, chronic renal failure, liver disease, anemia, acute coronary syndrome, CHF, peripheral vascular disease, and malignancy. Overall, the predictive capacity for these models is limited with a receiver operator curve of 0.658 to 0.68,7 indicating that other factors that may be difficult to measure play a substantial role. Other factors that have been implicated include severity of illness, dependence, low mobility, and low level of care after discharge.9,10
Role of Diabetes Diagnosis
The estimated cost of diabetes in 2007 was $174 billion, with the largest expenditure being inpatient care.11 The cost of a patient with diabetes was estimated at 2.3 times that of a patient without diabetes. In elderly patients with diabetes, it has been reported that 56% of Medicare costs are accounted for by 10% of patients, and these costs are, in large part, due to hospitalization.12 Complications of diabetes were associated with increased expenses.
Predictors of hospital readmission are shown in Table 1. In a large study of hospital utilization in five states, 30% of hospitalized patients with diabetes were readmitted within the 1 year study period, accounting for 50% of all hospital stays among patients with diabetes.13 Rehospitalizations occurred disproportionately among socioeconomically disadvantaged groups, including Hispanics and African Americans, those living in lower-income zip codes, and those without private insurance. Racial/ethnic disparities in readmissions were also reported elsewhere, particularly for microvascular complications.18
Table 1.
Predictors of Readmission among Inpatient Diabetes Cohorts
| General hospitalized diabetes cohorts | ||||
|---|---|---|---|---|
| Reference number | Number | Significant predictors | Follow-up | Relationship(all predictors in model)a |
| 13 | 648,748 | African American versus Caucasian Hispanic versus Caucasian Medicare versus private Medicaid versus private Low versus high income Medium versus high income |
Multiple admissions within 1 calendar year | OR 1.15 (1.13–1.17) OR 1.20 (1.18–1.23) OR 1.48 (1.45–1.50) OR 1.63 (1.60–1.66) OR 1.03 (1.01–1.04) OR 1.03 (1.01–1.05) |
| 14 | 482 | Hospital length of stay Family history of atherosclerosis Dependent for basic needs Systolic blood pressure >130 mmHg CHF Atrial fibrillation Basal glucose Creatinine clearance Hemoglobin |
1 year | OR 1.03 (1.00–1.07) OR 0.23 (0.11–0.485) OR 2.57 (1.17–5.68) OR 0.40 (0.24–0.67) OR 1.75 (1.07–2.89) OR 1.75 (1.01–3.02) OR 1.004 (1.001–1.007) OR 0.99 (0.98–0.99) OR 0.76 (0.68–0.85) |
| DKA cohorts | ||||
|---|---|---|---|---|
| Reference number | Number | Significant predictors | Follow-up | Relationship |
| 15 | 168 | Hispanic versus African American | Up to 3 years | OR 3.67 (1.66–8.10) |
| 16 | 152 | Polysubstance abuse | Up to 5 years | OR 19.5 (2.5–15.3) |
| 17 | 92 | (In children) Behavioral problems Young age at diagnosis Low socioeconomic status |
Up to 10 years | All were significant predictors |
OR, odds ratio.
Furthermore, disadvantaged patients were more likely to be admitted for acute complications of their diabetes, as opposed to chronic complications.13 This is of importance because acute complications are potentially more easily prevented. Among minority patients admitted with diabetic ketoacidosis (DKA), Hispanic patients were particularly likely to be readmitted (58% versus 27% of African Americans).16 Another factor that is associated with high risk of readmission for DKA is recreational drug abuse, and this is frequently overlooked.17
Socioeconomic disparities were particularly prominent in children.13 Adolescents may be particularly prone to recurrent admissions for DKA.19 In a longitudinal study of newly diagnosed patients with type 1 diabetes, risk factors for recurrent DKA include elevated hemoglobin A1c (HbA1c), behavioral problems, young age at diagnosis, and low socioeconomic status.18
In patients with diabetes, comorbidities that were predictors of readmission following hospitalization on internal medicine services at a single center include a history of CHF, renal dysfunction, anemia, and atrial fibrillation.20 As a comorbidity itself, diabetes is associated with increased readmission following hospitalization for CHF,21,22 renal transplant,23cardiac surgery,24–26 and coronary artery bypass surgery with preexisting left ventricular dysfunction27 (Table 2).
Table 2.
Cohorts in which Diabetes Is Tested as a Predictor of Readmission
| Reference number | Number | Population | Follow-up | Relationshipa |
|---|---|---|---|---|
| 22 | 1129 | CHF | 6 months | OR 1.62 (1.23–2.14) |
| 23 | 5791 | CHF | 2–3 months | OR 5.54 (4.94–6.20) |
| 24 | 366 | Renal transplant | Up to 14 years | 10.89 versus 18.28 months (p = .047) |
| 25 | 1665 | Cardiac surgery, readmission for CHF | 1 month | Adjusted OR 1.18 (0.87–1.60) |
| 26 | 7493 | Cardiac surgery | Up to 10 years | Cox HR 1.3 (1.20–1.41) |
| 27 | 2574 | Cardiac surgery | 1 month | OR 1.64 (1.25–2.14) |
| 28 | 900 | Cardiac surgery | 48 months | OR 2.56 (1.81–3.63) |
Cox HR, Cox prandial hazard ratio; OR, odds ratio.
Role of Glycemic Control
There are few studies indicating whether there is a relationship between glycemic control and hospital admission (Table 3). In one study, very poor glycemic control (HbA1c > 10%) but not moderate to poor glycemic control (HbA1c 8–9% or 9–10%) was associated with increased odds for diabetes-related hospitalization (odds ratio 2.13, 95% confidence interval 1.36–3.33 versus HbA1c < 7.0%).28 Likewise, there are few studies investigating a relationship between glycemic control and hospital readmission. A small study of hospitalized internal medicine patients with diabetes showed that patients who were readmitted within 1 year had higher plasma glucose levels at the index admission.20 Early post-renal transplant hyperglycemia in patients without known diabetes was associated with increased risk of readmission for infectious complications.15
Table 3.
Hyperglycemia as a Predictor of Readmission
| Reference number | Number | Population | Follow-up | Measure of glycemia | Relationshipa |
|---|---|---|---|---|---|
| 14 | 482 | Diabetes (internal medicine units) | 1 year | Basal glucose | OR 1.004 (1.001–1.007) adjusted |
| 29 | 1931 | Non-diabetic renal transplant (readmit for infection) | Up to 22 years | 2 glucoses > 126 mg/dl in early post-transplant period | Cox HR 2.93 (1.55–5.56) |
| 30 | 748 | CHF (readmit for CHF) | 30–90 days | Time-weighted in-hospital capillary blood glucose, HbA1c | Glucose: OR 3.3 (p = .03) HbA1c: OR 5.5 (p = .04) adjusted |
| 31 | 969 | Community-acquired pneumonia | 30 day | Admission glucose | No association (summary data not reported) |
| 32 | 2366 | Community-acquired pneumonia | 90 day | Admission glucose | Adjusted OR versus 72–110 mg/dl: 110–140 mg/dl, 0.74 (0.53–1.04) 140–200 mg/dl, 0.85 (0.58–1.25) 200–360 mg/dl, 0.92 (0.48–1.76) |
Cox HR, Cox prandial hazard ratio; OR, odds ratio.
Given the high risk of readmission in patients with CHF, Dungan and coauthors33 used a centralized information warehouse to investigate whether readmission for CHF may be related to glycemic control. Data showed that higher HbA1c and higher time-weighted mean glucose were both associated with increased frequency of CHF readmission. It is not immediately obvious why improved glycemic control either in the hospital or beyond would reduce readmissions for other conditions. The most intriguing explanation is modification of the comorbidity through glycemic control. In the case of CHF, hyperglycemia (and insulin resistance) has been hypothesized to play a role in the development of diabetic cardiomyopathy, in part, via inefficient myocardial fuel metabolism.34 Limited evidence suggests that improvement in glycemic control may improve cardiac function by as early as 3 weeks, at least early in the course of CHF.29 Furthermore, severe hyperglycemia is known to induce shifts in fluids and electrolytes that may be of particular relevance in patients with CHF. In a more generalized view, hyperglycemia may lead to impaired immune function30 and, in particular, has been associated with postoperative infection,35,36 a common cause of hospital readmission among surgical patients.
Another possibility is that good glycemic control is simply a predictor of adherence to medical and dietary therapies in general, better self-care behaviors, and fewer socioeconomic barriers that are important for many chronic disease states. However, this does not necessarily explain why inpatient glycemic control would predict readmissions, unless inpatient control is heavily influenced by preadmission glycemic control, and interventions in the hospital to rectify hyperglycemia are either not implemented or are ineffective. Dungan and colleagues33 found that HbA1c was only modestly correlated with inpatient time-weighted glycemic control, although this correlation was statistically significant (R-value 0.47, p < .0001).
By extension, it is unclear whether attention to inpatient glycemic control can reduce readmissions. In the CHF cohort, inpatient glycemic control was associated with later (30–90 day) but not early (<30 day) readmissions, and both HbA1c and inpatient glycemic control were predictors. Admission glucose was not associated with readmission. These observations suggest that any benefit acquired from glycemic control requires time to develop. This is further illustrated by studies of patients hospitalized with community-acquired pneumonia, where admission glucose alone was not a predictor of 30-day37 or 90-day38 hospital readmission. It is unknown whether an assessment of glycemia over a more extended period would have shown a relationship. However, whether one concludes that inpatient or outpatient glycemic control is partly responsible for reduced hospitalizations, attention to glycemic control in the hospital may facilitate sustained glycemic control post-discharge.
Prevention of Readmission
General Measures
A more generalized approach to reducing readmissions in patients with diabetes seems reasonable for three reasons. (1) There are very few published data for interventions targeted at prevention of readmission in patients with diabetes. (2) Comorbidities are common in patients with diabetes, which may not be the primary reason for admission. (3) Important predictors of readmission may be common to multiple diseases, including socioeconomic, psychosocial, and educational disparities. Appropriate targeting of interventions to high-risk groups would potentially optimize the cost-to-benefit ratio.
Various approaches have been employed in generalized inpatient populations. One potentially cost-effective approach is a phone call to patients following discharge, but this has shown limited effectiveness.31,39 There were no studies specifically targeted to telephone follow-up of hospitalized patients with diabetes. However, barriers to obtaining prescriptions are common among hospitalized patients with diabetes.32 Thus early identification of post-discharge problems while they are still manageable could potentially reduce the need for readmission.
Methods specifically intended to encourage hospital follow-up have also received interest because half of Medicare patients who are readmitted within 30 days did not have an outpatient encounter following discharge.4 In patients with diabetes, a direct referral from inpatient staff significantly increases the odds of keeping a follow-up visit.40 However, other barriers to hospital follow-up are common among patients with diabetes, including lack of transportation, expense, and lack of health insurance.41
There is evidence for a small benefit from individualized discharge planning for decreasing readmissions in undifferentiated hospitalized patients.42 Successful programs utilize multiple approaches, such as a nurse discharge advocate, prearranged follow-up appointments, medication reconciliation, patient education, and communication with the primary care provider.43,44
Diabetes-Specific Measures
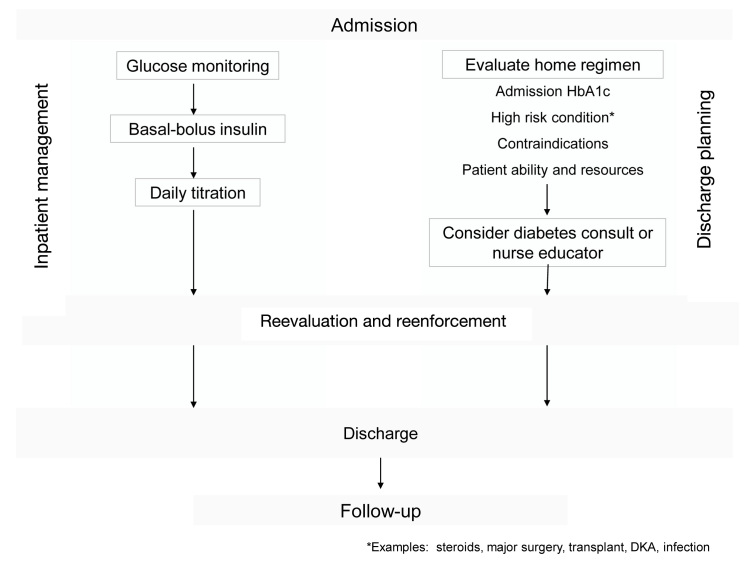
Although the evidence is still limited, diabetes-specific measures may play a role in reducing unnecessary readmissions. In general, these measures are best implemented closer to admission, not at discharge (Figure 1). There are several key points that warrant emphasis.
Figure 1.
An expanded view of inpatient diabetes management encompasses two early parallel therapeutic tracks, addressing inpatient glucose stabilization and management as well as diabetes-specific discharge planning, both of which require ongoing reevaluation and reinforcement.
Reinforcement by Example
The inpatient setting could be viewed as an ideal environment for reinforcing the importance of glycemic control and diabetes self-care habits following discharge. It is unclear whether interventions to improve glycemic control in the hospital actually reduce the frequency of readmission. However, assuming this to be true, strategies for glycemic control would need to be implemented early in the hospital course in order to achieve optimal outcomes at discharge since effective glycemic control takes several days to implement.45,46
Choosing a Discharge Regimen
The default approach to discharge therapy is often to restart the previous home diabetes regimen without regard to its effectiveness. Establishing a discharge regimen is further complicated by guidelines that recommend discontinuation of noninsulin diabetes therapies at admission,47 which can add to confusion and lapses in care of diabetes at discharge.48 Computerized support tools and medication reconciliation procedures may help to avoid omissions of discharge medications. However, the ideal discharge regimen should be implemented with knowledge of the pre-hospital and in-hospital glycemic control, and the needs and capabilities of the individual patient. At a minimum, a recent HbA1c should be available or ordered at the time of admission in order to inform discharge treatment decisions for all patients with diabetes.47
Acknowledging the Diagnosis of Diabetes
One study demonstrated a significant association between failure to record the diagnosis of diabetes in hospital discharge data and 30-day readmissions.49 It is unclear whether such omissions are related to inadequate glycemic control or to a more global problem of poor transitions in care. Diabetes is not typically the primary indication for admission, and it is likely that competing medical priorities could eclipse glycemic management in the hospital and at discharge. Documenting the diagnosis on the problem list is the first step toward ensuring that proper attention is received during hospitalization and at discharge. Electronic medical records may decrease the impact of this problem over time.
Provider Responsibility
Diabetes is often considered an outpatient problem that should be relegated to the primary physician or endocrinologist. Unfortunately, the outpatient provider is typically also dealing with competing priorities and may not have adequate data or educational resources that may be available in the hospital. Effective hand-offs to the provider in the outpatient setting help to minimize confusion.50
Inpatient Glycemic Management Teams
Limited data in some,51 but not all,52 studies suggest that the involvement of a diabetes specialist team reduces readmissions. Results may depend upon the individual components of the program and attention to discharge needs. Inpatient diabetes management teams generally incorporate some component of diabetes education. Education is ideally delivered over multiple visits, and therefore, early identification of patient needs and appropriate consultation is desirable.53 Where certified diabetes educators are unavailable, diabetes nurse champions can be trained on each unit to facilitate education efforts. In the outpatient setting, nursing education has resulted in improved HbA1c and adherence to medication and glucose monitoring, so the potential benefits are not limited to readmission.54–56
While diabetes education in the hospital generally focuses on survival skills,47 more detailed self-management education is typically deferred to the outpatient arena. Further study is needed in hospitalized patients, but more advanced self-management education may be useful on an individualized basis. In the case of CHF, self-management education has been associated with improved readmissions,57 so such a relationship in patients with diabetes would not be unprecedented.
Post-Discharge Support
Following discharge, negative attitudes toward insulin are common and contribute to a high rate of nonadherence to insulin post-discharge, particularly in the absence of contact with a diabetes educator.58 In a nonrandomized interventional study, indigent patients with ketosis-prone diabetes who participated in an outpatient diabetes treatment program that included free access to insulin, 24 h per day voicemail–pager access to a staff, and frequent phone calls and scheduled visits were less likely to be readmitted with DKA than those who did not participate (16% versus 43%, p = .001).59 More research is clearly needed in this respect.
Conclusions
Diabetes, like other chronic medical conditions, is associated with increased risk of hospital readmission. However, diabetes is not always the main priority for providers in the inpatient setting, and opportunities for optimization of care may be missed without a systematic approach. Preliminary studies suggest that acute and chronic glycemic control may be of importance when diabetes is the primary diagnosis or whether it is a comorbidity. Prospective interventional studies targeting interventions for improving glycemic control in the hospital and after discharge are needed to determine whether glycemic control impacts the frequency of readmissions. In the meantime, efforts to reduce readmissions should be multifactorial and encompass both general and diabetes-specific measures.
Glossary
- (CHF)
congestive heart failure
- (DKA)
diabetic ketoacidosis
- (HbA1c)
hemoglobin A1c
Disclosures
Kathleen M. Dungan has received research support from Novo Nordisk and has served as a consultant with Eli Lilly and Pfizer.
References
- 1.Calver J, Brameld KJ, Preen DB, Alexia SJ, Boldy DP, McCaul KA. High-cost users of hospital beds in Western Australia: a population-based record linkage study. Med J Aust. 2006;184(8):393–397. doi: 10.5694/j.1326-5377.2006.tb00289.x. [DOI] [PubMed] [Google Scholar]
- 2.Johansen H, Nair C, Bond J. Who goes to the hospital? An investi-gation of high users of hospital days. Health Rep. 1994;6(2):253–277. [PubMed] [Google Scholar]
- 3.Zook CJ, Moore FD. High-cost users of medical care. N Engl J Med. 1980;302(18):996–1002. doi: 10.1056/NEJM198005013021804. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Epstein AM. Revisiting readmissions--changing the incentives for shared accountability. N Engl J Med. 2009;360(14):1457–1459. doi: 10.1056/NEJMe0901006. [DOI] [PubMed] [Google Scholar]
- 6.Rumball-Smith J, Hider P. The validity of readmission rate as a marker of the quality of hospital care, and a recommendation for its definition. N Z Med J. 2009;122(1289):63–70. [PubMed] [Google Scholar]
- 7.Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ. 2006;333(7563):327. doi: 10.1136/bmj.38870.657917.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howell S, Coory M, Martin J, Duckett S. Using routine inpatient data to identify patients at risk of hospital readmission. BMC Health Serv Res. 2009;9:96. doi: 10.1186/1472-6963-9-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shipton S. Risk factors associated with multiple hospital readmissions. Home Care Provid. 1996;1(2):83–85. doi: 10.1016/s1084-628x(96)90234-8. [DOI] [PubMed] [Google Scholar]
- 10.Jacob L, Poletick EB. Systematic review: predictors of successful transition to community-based care for adults with chronic care needs. Care Manag J. 2008;9(4):154–165. doi: 10.1891/1521-0987.9.4.154. [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 12.Krop JS, Powe NR, Weller WE, Shaffer TJ, Saudek CD, Anderson GF. Patterns of expenditures and use of services among older adults with diabetes. Implications for the transition to capitated managed care. Diabetes Care. 1998;21(5):747–752. doi: 10.2337/diacare.21.5.747. [DOI] [PubMed] [Google Scholar]
- 13.Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421–1426. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- 14.Hosseini MS, Nemati E, Pourfarziani V, Taheri S, Nourbala MH, Einollahi B. Early hyperglycemia after allogenic kidney transplanta-tion: does it induce infections. Ann Transplant. 2007;12(4):23–26. [PubMed] [Google Scholar]
- 15.Nyenwe E, Loganathan , Blum , Ezuteh , Erani , Palace , Ogugua C. Admissions for diabetic ketoacidosis in ethnic minority groups in a city hospital. Metabolism. 2007;56(2):172–178. doi: 10.1016/j.metabol.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Isidro ML, Jorge S. Recreational drug abuse in patients hospitalized for diabetic ketosis or diabetic ketoacidosis. Acta Diabetol. 2010 doi: 10.1007/s00592-010-0243-z. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Kovacs M, Charron-Prochownik D, Obrosky DS. A longitudinal study of biomedical and psychosocial predictors of multiple hospitalizations among young people with insulin-dependent diabetes mellitus. Diabet Med. 1995;12(2):142–148. doi: 10.1111/j.1464-5491.1995.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 18.Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: the case of diabetes. Am J Public Health. 2005;95(9):1561–1567. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skinner TC. Recurrent diabetic ketoacidosis: causes, prevention and management. Horm Res. 2002;57(Suppl 1):78–80. doi: 10.1159/000053320. [DOI] [PubMed] [Google Scholar]
- 20.Montero Pérez-Barquero M, Martínez Fernández R, de Los Mártires Almingol I, Michán Doña A, Conthe Gutiérrez P. DICAMI Study. Prognostic factors in patients admitted with type 2 diabetes in Internal Medicine Services: hospital mortality and readmission in one year (DICAMI study) Rev Clin Esp. 2007;207(7):322–330. doi: 10.1157/13107943. [DOI] [PubMed] [Google Scholar]
- 21.Krumholz HM, Chen Y, Wang Y, Vaccarino V, Radford MJ, Horwitz RI. Predictors of readmission among elderly survivors of admission with heart failure. Am Heart J. 2000;139((1 Pt 1)):72–77. doi: 10.1016/s0002-8703(00)90311-9. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg BH, Abraham WT, Albert NM, Chiswell K, Clare R, Stough WG, Gheorghiade M, O’Connor CM, Sun JL, Yancy CW, Young JB, Fonarow GC. Influence of diabetes on characteristics and outcomes in patients hospitalized with heart failure: a report from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) Am Heart J. 2007;154(2):277.e1–277.e8. doi: 10.1016/j.ahj.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Ramezani M, Ghoddousi K, Hashemi M, Khoddami-Vishte HR, Fatemi-Zadeh S, Saadat SH, Khedmat H, Naderi M. Diabetes as the cause of end-stage renal disease affects the pattern of post kidney transplant rehospitalizations. Transplant Proc. 2007;39(4):966–969. doi: 10.1016/j.transproceed.2007.03.074. [DOI] [PubMed] [Google Scholar]
- 24.D’Agostino RS, Jacobson J, Clarkson M, Svensson LG, Williamson C, Shahian DM. Readmission after cardiac operations: prevalence, patterns, and predisposing factors. J Thorac Cardiovasc Surg. 1999;118(5):823–832. doi: 10.1016/s0022-5223(99)70051-6. [DOI] [PubMed] [Google Scholar]
- 25.Steuer J, Blomqvist P, Granath F, Rydh B, Ekbom A, de Faire U, Ståhle E. Hospital readmission after coronary artery bypass grafting: are women doing worse? Ann Thorac Surg. 2002;73(5):1380–1386. doi: 10.1016/s0003-4975(02)03467-7. [DOI] [PubMed] [Google Scholar]
- 26.Ferraris VA, Ferraris SP, Harmon RC, Evans BD. Risk factors for early hospital readmission after cardiac operations. J Thorac Cardiovasc Surg. 2001;122(2):278–286. doi: 10.1067/mtc.2001.114776. [DOI] [PubMed] [Google Scholar]
- 27.Whang W, Bigger JT., Jr Diabetes and outcomes of coronary artery bypass graft surgery in patients with severe left ventricular dysfunction: results from the CABG Patch Trial database. The CABG Patch Trial Investigators and Coordinators. J Am Coll Cardiol. 2000;36(4):1166–1172. doi: 10.1016/s0735-1097(00)00823-8. [DOI] [PubMed] [Google Scholar]
- 28.Menzin J, Korn JR, Cohen J, Lobo F, Zhang B, Friedman M, Neumann PJ. Relationship between glycemic control and diabetes-related hospital costs in patients with type 1 or type 2 diabetes mellitus. J Manag Care Pharm. 2010;16(4):264–275. doi: 10.18553/jmcp.2010.16.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Von Bibra H, Hansen A, Dounis V, Bystedt T, Malmberg K, Rydén L. Augmented metabolic control improves myocardial diastolic function and perfusion in patients with non-insulin dependent diabetes. Heart. 2004;90(12):1483–1484. doi: 10.1136/hrt.2003.020842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turina M, Fry DE, Polk HC., Jr Acute hyperglycemia and the innate immune system: clinical, cellular, and molecular aspects. Crit Care Med. 2005;33(7):1624–1633. doi: 10.1097/01.ccm.0000170106.61978.d8. [DOI] [PubMed] [Google Scholar]
- 31.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;4 doi: 10.1002/14651858.CD004510.pub3. CD004510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kimmel B, Sullivan MM, Rushakoff RJ. Survey on transition from inpatient to outpatient for patients on insulin: what really goes on at home? Endocr Pract. 2010;16(5):785–791. doi: 10.4158/EP10013.OR. [DOI] [PubMed] [Google Scholar]
- 33.Dungan KM, Osei K, Nagaraja HN, Schuster DP, Binkley P. Relationship between glycemic control and readmission rates in patients hospitalized with congestive heart failure during implementation of hospital-wide initiatives. Endocr Pract. 2010;16(6):945–951. doi: 10.4158/EP10093.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aneja A, Tang WH, Bansilal S, Garcia MJ, Farkouh ME. Diabetic cardiomyopathy: insights into pathogenesis diagnostic challenges, and therapeutic options. Am J Med. 2008;121(9):748–757. doi: 10.1016/j.amjmed.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 35.Ramos M, Khalpey Z, Lipsitz S, Steinberg J, Panizales MT, Zinner M, Rogers SO. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591. doi: 10.1097/SLA.0b013e31818990d1. [DOI] [PubMed] [Google Scholar]
- 36.Furnary AP, Wu Y, Bookin SO. Effect of hyperglycemia and continuous intravenous insulin infusions on outcomes of cardiac surgical procedures: the Portland Diabetic Project. Endocr Pract. 2004;10(Suppl 2):21–33. doi: 10.4158/EP.10.S2.21. [DOI] [PubMed] [Google Scholar]
- 37.Godar DA, Kumar DR, Schmelzer KM, Talsness SR, Liang H, Schmelzer JR, Mazza JJ, Yale SH. The impact of serum glucose on clinical outcomes in patients hospitalized with community-acquired pneumonia. WMJ. 2011;110(1):14–20. [PubMed] [Google Scholar]
- 38.Eurich DT, Gamble JM, Marrie TJ, Majumdar SR. Dysglycaemia and 90 day and 1 year risks of death or readmission in patients hospitalised for community-acquired pneumonia. Diabetologia. 2010;53(3):497–503. doi: 10.1007/s00125-009-1598-y. [DOI] [PubMed] [Google Scholar]
- 39.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S–30S. doi: 10.1016/s0002-9343(01)00966-4. [DOI] [PubMed] [Google Scholar]
- 40.Wheeler K, Crawford R, McAdams D, Benel S, Dunbar VG, Caudle JM, George C, El-Kebbi I, Gallina DL, Ziemer DC, Cook CB. Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow-up. Arch Intern Med. 2004;164(4):447–453. doi: 10.1001/archinte.164.4.447. [DOI] [PubMed] [Google Scholar]
- 41.Wheeler K, Crawford R, McAdams D, Robinson R, Dunbar VG, Cook CB. Inpatient to outpatient transfer of diabetes care: perceptions of barriers to postdischarge followup in urban African American patients. Ethn Dis. 2007;17(2):238–243. [PubMed] [Google Scholar]
- 42.Shepperd S, McClaran J, Phillips CO, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;1 doi: 10.1002/14651858.CD000313.pub3. CD000313. [DOI] [PubMed] [Google Scholar]
- 43.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O’Donnell JK, Paasche-Orlow MK, Manasseh C, Martin S, Culpepper L. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dedhia P, Kravet S, Bulger J, Hinson T, Sridharan A, Kolodner K, Wright S, Howell E. A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc. 2009;57(9):1540–1546. doi: 10.1111/j.1532-5415.2009.02430.x. [DOI] [PubMed] [Google Scholar]
- 45.Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, Puig A, Mejia R. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial) Diabetes Care. 2007;30(9):2181–2186. doi: 10.2337/dc07-0295. [DOI] [PubMed] [Google Scholar]
- 46.Umpierrez GE, Hor T, Smiley D, Temponi A, Umpierrez D, Ceron M, Munoz C, Newton C, Peng L, Baldwin D. Comparison of inpatient insulin regimens with detemir plus aspart versus neutral protamine Hagedorn plus regular in medical patients with type 2 diabetes. J Clin Endocrinol Metab. 2009;94(2):564–569. doi: 10.1210/jc.2008-1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE. American Association of Clinical Endocrinologists; American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–1131. doi: 10.2337/dc09-9029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lipska KJ, Wang Y, Kosiborod M, Masoudi FA, Havranek EP, Krumholz HM, Inzucchi SE. Discontinuation of antihyperglycemic therapy and clinical outcomes after acute myocardial infarction in older patients with diabetes. Circ Cardiovasc Qual Outcomes. 2010;3(3):236–242. doi: 10.1161/CIRCOUTCOMES.109.887620. [DOI] [PubMed] [Google Scholar]
- 49.Robbins JM, Webb DA. Diagnosing diabetes and preventing rehospi-talizations: the urban diabetes study. Med Care. 2006;44(3):292–296. doi: 10.1097/01.mlr.0000199639.20342.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440. doi: 10.1002/jhm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koproski J, Pretto Z, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20(10):1553–1555. doi: 10.2337/diacare.20.10.1553. [DOI] [PubMed] [Google Scholar]
- 52.Davies M, Dixon S, Currie CJ, Davis RE, Peters JR. Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial. Diabet Med. 2001;18(4):301–307. doi: 10.1046/j.1464-5491.2001.00470.x. [DOI] [PubMed] [Google Scholar]
- 53.Cook CB, Seifert KM, Hull BP, Hovan MJ, Charles JC, Miller-Cage V, Boyle ME, Harris JK, Magallanez JM, Littman SD. Inpatient to outpatient transfer of diabetes care: planing for an effective hospital discharge. Endocr Pract. 2009;15(3):263–269. doi: 10.4158/EP.15.3.263. [DOI] [PubMed] [Google Scholar]
- 54.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24(2):202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 55.Kim HS, Oh JA. Adherence to diabetes control recommendations: impact of nurse telephone calls. J Adv Nurs. 2003;44(3):256–261. doi: 10.1046/j.1365-2648.2003.02800.x. [DOI] [PubMed] [Google Scholar]
- 56.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108(1):20–27. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 57.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. doi: 10.1186/1471-2261-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lerman I, Díaz JP, Ibarguengoitia ME, Pérez FJ, Villa AR, Velasco ML, Cruz RG, Rodrigo JA. Nonadherence to insulin therapy in low-income, type 2 diabetic patients. Endocr Pract. 2009;15(1):41–46. doi: 10.4158/EP.15.1.41. [DOI] [PubMed] [Google Scholar]
- 59.Maldonado MR, D’Amico S, Rodriguez L, Iyer D, Balasubramanyam A. Improved outcomes in indigent patients with ketosis-prone diabetes: effect of a dedicated diabetes treatment unit. Endocr Pract. 2003;9(1):26–32. doi: 10.4158/EP.9.1.26. [DOI] [PubMed] [Google Scholar]