Abstract
Self-management is critical to achieving diabetes treatment goals. Mobile phones and Bluetooth® can supportself-management and lifestyle changes for chronic diseases such as diabetes. A mobile health (mHealth) research platform—the Few Touch Application (FTA)—is a tool designed to support the self-management of diabetes. The FTA consists of a mobile phone-based diabetes diary, which can be updated both manually from user input and automatically by wireless data transfer, and which provides personalized decision support for the achievement of personal health goals. Studies and applications (apps) based on FTAs have included: (1) automatic transfer of blood glucose (BG) data; (2) short message service (SMS)-based education for type 1diabetes (T1DM); (3) a diabetes diary for type 2 diabetes (T2DM); (4) integrating a patient diabetes diary with health care (HC) providers; (5) a diabetes diary for T1DM; (6) a food picture diary for T1DM; (7) physical activity monitoring for T2DM; (8) nutrition information for T2DM; (9) context sensitivity in mobile self-help tools; and (10) modeling of BG using mobile phones.
We have analyzed the performance of these 10 FTA-based apps to identify lessons for designing the most effective mHealth apps. From each of the 10 apps of FTA, respectively, we conclude: (1) automatic BG data transfer is easy to use and provides reassurance; (2) SMS-based education facilitates parent-child communication in T1DM; (3) the T2DM mobile phone diary encourages reflection; (4) the mobile phone diary enhances discussion between patients and HC professionals; (5) the T1DM mobile phone diary is useful and motivational; (6) the T1DM mobile phone picture diary is useful in identifying treatment obstacles; (7) the step counter with automatic data transfer promotes motivation and increases physical activity in T2DM; (8) food information on a phone for T2DM should not be at a detailed level; (9) context sensitivity has good prospects and is possible to implement on today’s phones; and (10) BG modeling on mobile phones is promising for motivated T1DM users.
We expect that the following elements will be important in future FTA designs: (A) automatic data transfer when possible; (B) motivational and visual user interfaces; (C) apps with considerable health benefits in relation to the effort required; (D) dynamic usage, e.g., both personal and together with HC personnel, long-/short-term perspective; and (E) inclusion of context sensitivity in apps. We conclude that mHealth apps will empower patients to take a more active role in managing their own health.
Keywords: blood glucose, diabetes, mobile health, self-management, type 1 diabetes, type 2 diabetes
Introduction
It is estimated that 366 million people worldwide have diabetes mellitus, comprising both type 1 (T1DM) and type 2 diabetes (T2DM).1 Lifestyle factors and blood glucose (BG) management are important in reducing long-term diabetes complications.2,3 Both personal suffering and enormous costs are associated with insufficient self-management. In 2011, diabetes caused 4.6 million deaths in the adult population, and the number of people with T2DM is increasing in every country.1 Health care expenditures to treat and prevent diabetes and its complications exceeded $465 billion (2011), indicating an opportunity and growing need to develop cost-effective support tools and interventions for diabetes self-management.
Personal health applications (PHAs) developed for use on mobile information and communication technology (ICT) platforms offer potential to address this need. While much of the current evidence pertains to PHAs deployed on stationary desktop computers and televisions, a growing number of research publications indicate a trend toward development of mobile PHAs for diabetes self-management support.4
Advances in ICT provide a variety of options for developing hardware and software deployment platforms for new test and sensor technologies. However, many of these products have not been optimized for usability or evaluated for their effectiveness in motivating or changing users’ self-management behaviors. Mobile phones provide a promising foundation for developing cost-effective diabetes PHAs that can be incorporated into daily routines.5–7 However, there are few published studies addressing which specific elements of mobile diabetes applications (apps) offer the greatest potential to benefit users effectively.
Since 2001, our research group has developed mobile PHAs for diabetes. We have involved end users in the designs and performed research on the effects of the systems. This article describes the program of research involving the Few Touch Application (FTA), a mobile PHA, to illustrate functionalities and findings related to various approaches. The core component is a mobile phone-based diabetes diary that is updated both by manual user input and automatically by wireless data transfer. It also provides personalized decision support by giving feedback on users’ performance related to their personal health goals.
The objective of this article is to describe opportunities for developing and leveraging mobile health (mHealth) interventions in diabetes treatment and self-management based on various feature sets. Lessons learned and design implications are derived from multiple studies of patient user experiences and design preferences, as well as clinician, developer, and researcher experience. Directions for future research and development by our research team are also discussed.
Methods
Throughout our research, we have actively engaged representative end users in all phases of PHA develop-ment and evaluation. The overall aim has been to search for strategies for utilizing mobile ICT to improve patients’ self-management abilities. This aim led us to use the following design methods and foci.
Design Methods
Leverage existing societal trends in ICT adoption and incorporate the relevant technologies (e.g., mobile phones, glucose meters) into the PHA designs.
Focus on the most important chronic disease self-management parameters—for this patient group: diet, physical activity, BG, and medications.
Optimize the PHA for usability.
Apply techniques proven effective at improving self-reported health status and clinical outcomes.
Design solutions that are possible to implement on a large scale and that have the potential to be cost-effective for society.
Evaluation Methods
Our research is based on user-centered methods that incorporate focus groups, interviews, usability testing, questionnaires, paper prototyping, functional software and hardware prototyping, and iterative design and development cycles, described more in detail elsewhere.8
Results
We have developed 10 different feature sets (Table 1) for the FTA suite for mobile phones with Bluetooth® and touch-sensitive screens (also called smartphones). Diabetes mHealth PHA lessons learned and design implications derived from our research experiences with each of the 10 FTA feature sets are presented here.
Table 1.
Summary of Aims, Lessons Learned, and Design Implications from the Presented Mobile Diabetes Application Feature Sets
| Set | Study aim | Lesson learned | Design implication |
|---|---|---|---|
| 1 | Explore the effects of automatic transfer of blood glucose data from children with T1DM to their parents as SMSs. | Parents of children with T1DM felt reassured receiving blood glucose measures as SMS messages but also asked for access to their children’s insulin use measures. | Blood glucose meters should automatically transfer data to the users’ and/or caregivers’ mobile phones for support purposes, e.g., generating graphical trending displays. |
| 2 | To evaluate tools and methods to enhance access to information and educational services for people with diabetes. | General diabetes-related information received by SMS offers potential to facilitate parent-child communication, and the parents valued the pop-up reminder effect. | Parents should be able to tailor the frequency and the type of information received as text messages to their mobile phones. |
| 3 | Generate knowledge about how a mobile tool can be designed for supporting lifestyle changes among people with T2DM. | An always-available diary as a mobile phone app can challenge T2DM users to think about how to improve their situation and encourage them to adopt lifestyle changes. | A T2DM diary should enable the user to capture and analyze blood glucose, physical activity, and nutritional data, in addition to motivating users to achieve personal aims. |
| 4 | To research if/how a mobile patient diabetes diary can be integrated with the HC service and how it affects patients’ self-management and other health factors. | Patients use the mobile-phone-based diary to show and discuss their data with their doctors and nurses. | Educational needs related to use of touch-sensitive mobile phones have to be clarified and provided as an option for those who are new to this technology. |
| 5 | To further explore the needs of people with T1DM with regards to benefiting from a mobile-phone-based diabetes diary, including interaction with hospital personnel. | A mobile diabetes diary, especially the blood glucose function, is useful for many users with T1DM and should preferably be available on their own mobile phone. | Special efforts must be focused on making a phone-based diary useful and motivational for users with T1DM. For example, the personal goals function that worked fairly well for T2DM users was rarely used by T1DM users. |
| 6 | Investigate whether and potentially how a mobile-phone-based food picture diary can improve communication between adolescents with T1DM and their medical providers. | Short, intensive learning periods where adolescents take pictures of what they eat seem to be a good way to identify obstacles in reaching the treatment goals for this group. | Plan for how to use a food picture diary for shorter periods in case some users are reluctant to use it on a long-term basis. |
| 7 | To research how an easy-to-use system for monitoring and managing physical activity within T2DM could be designed and to document users’ feedback on using it. | An automatic step-counter-based system seems to be motivating to monitor physical activity but should optionally be succeeded by a more advanced system. | Tools for physical activity monitoring within T2DM should be as integrated as closely as possible with the users’ daily tools and outfits. |
| 8 | To research preferences for presentation of food information on a mobile phone screen for T2DM users. | It is appealing to look up food information, which should include practical tips, carbohydrate content, suggestions for alternative foods, comparison based on nutritional content, and/or ways of preparing the food. | Nutritional information on mobile phones should be easy to read, i.e., information that is easy to access, but approximate information is better than information that is harder to access but more precise. |
| 9 | Research how to make mobile diabetes diaries more “aware” of their environment and make the self-help system adapt to patients’ needs. | Users respond positively to context-sensitive functionalities for enhancing the usability of mobile self-management tools. | Today’s mobile phones support context-sensitive app development; to improve usability and convenience, this should be a stronger focus in future systems. |
| 10 | To explore the potential for implementing statistical models in mobile diabetes diaries to help the user understand patterns in the blood glucose. | For a motivated group of T1DM patients, analysis of data from a mobile-phone-based diary using period finding and scale-space trends was found to be promising. | A predictive model of blood glucose requires fine resolution of the input, in particular food. Finding innovative solutions for nutritional recording that does not require too much extra effort by users should be a focus of future research. |
Automatic Transfer of Blood Glucose Data
Children with T1DM and their parents face numerous challenges in BG monitoring and regulation. They often need help while home alone, at school, during leisure activities, while visiting friends, on overnight visits, and during weekend trips without parents.
We designed a system to transfer readings automatically >from a child’s BG monitor to their parent’s mobile phone.9 Using a custom-made Bluetooth adapter [a similar adapter called “Polytel”10 is now available (Polymap Wireless, LLC, Tucson, AZ)], the system was designed to transfer BG readings automatically from a BG monitor—the OneTouch® Ultra® (LifeScan, Inc., Milpitas, CA)—to a mobile phone after measurements had been taken. The child’s mobile phone was programmed to send the measurement results automatically via short message service (SMS) to the parents’ mobile phone; see Figure 1.
Figure 1.

The wireless system for automatic transfer of BG data.
The mobile phone sent the SMS message without intervention from the user as long as the phone was within Bluetooth range (10 m) of the BG monitor at the time of the BG reading. The system was tested among 15 children (aged 9–15 years) with T1DM and their parents. Parental suggestions for further developments included similar alerts of irregular insulin dosages and automatically generated dietary and insulin dosage advice. The results have been reported in detail elsewhere.11
Short Message Service-Based Education for Type 1 Diabetes
We tested the feasibility of using an automated SMS system for educating parents of children with T1DM about the disease.12 An object-oriented database server (Zope) was used to administer 74 different SMS messages with facts related to T1DM. The messages were classified into seven relevant categories: diabetes definitions, BG, insulin, nutrition, physical activity, illness, and rights at school. Users could choose message types by sending a keyword as a SMS request to the server.
Eleven parents of children with T1DM received messages for 11 weeks. Most reported an enormous need for information, especially when their children were first diagnosed. We assessed user satisfaction and perceived strengths and weaknesses of the SMS system through interviews. The parents were positive about the system and said that they would like to continue using it. They especially liked the pop-up reminder effect of SMS messages in busy everyday life. Some commented that the messages were intrusive, arriving too often and at inconvenient times. They also noted the potential of the messages to facilitate communication with their adolescent children. The inability to store or print the messages was seen as a significant design weakness.
Mobile Phone-Based Diabetes Diary for Type 2 Diabetes
A mobile phone-based system for supporting lifestyle changes among people with T2DM was designed and tested with a cohort of 12 patients.13 The mobile system comprises a BG monitor connected to a Bluetooth adapter, a tailored step counter, an eating habit registration system, and an educational system with practical tips. Step counter and glucose meter data are transferred from these sensor devices to the smart phone automatically, and nutritional intakes are entered manually using a touch-screen interface that is also used to access all components of the system (see Figure 2).
Figure 2.
The main menu for the T2DM version of the FTA.
Findings from a 6-month field study indicated good system usability and user acceptance.13 The diary also challenges patients to think about how they can improve their situation, because it provides them a way to capture and analyze relevant personal information about their disease. Furthermore, it provides users with feedback on how they perform in relation to their own personal aims or general recommendations regarding nutrition habits, physical activity, and BG levels—the three main basic elements that influence personal diabetes management. The prospects for this and similar apps are good because mobile phone platforms and the mobile Web are developing quickly and already provide the required capabilities.
Integrating a Patient Diabetes Diary with Health Care Providers
From our study involving diabetes nurses and from research on preferences for receiving BG data directly from patients’ mobile diaries into electronic health record systems, we found that three of four hospitals were positive to this.14 The fourth hospital had some reservations, commenting that the BG data itself were not very useful without additional information on factors that affect the measurements, such as food and activity. In general, the nurses preferred to receive the data presented as a data log (date, time, measure). They said that this was faster to read because they were used to traditional paper-based logs but that data presented as pie charts and graphs could also be useful. In most of our other studies,13,15 both T1DM and T2DM users reported that they showed and discussed their data on the FTA with their HC providers. In focus group meetings after use of the FTA over several months, comments like these were reported: “It is an easy system to show to my diabetes doctor and diabetes nurse—especially the BG graph” (T1DM), and “I showed the system to my general practitioner, and he thought it was very nice” (T2DM). Further, there have been some challenges due to the touch-sensitive mobile phone, which causes usability problems for some of the users.
The diabetes diary (FTA) is currently being studied in a randomized controlled trial among people with T2DM (approximately 150 patients). One of the objectives of the study is to find out how the app can be integrated specifically in the primary HC service. The study16 is part of the European Union project RENEWING HEALTH.17
Mobile Phone-Based Diabetes Diary for Type 1 Diabetes
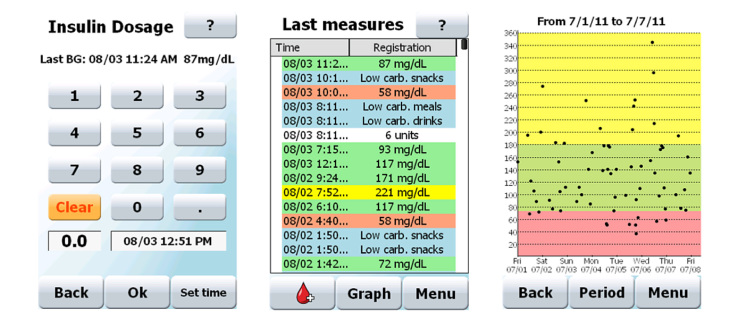
A mobile phone app for T1DM has been developed based on the FTA concept described earlier.13 In addition to the version for T2DM patients, this T1DM version of FTA comprises a function for easy recording of insulin injections together with nutrition, options for commenting on all data, and an improved feedback screen where the user sees BG, insulin injections, and food intake in relation to each other. For examples of screenshots, see Figure 3.
Figure 3.
Examples of input/output screens for the T1DM app; insulin input, list of recordings, and graphical glucose plot.
A study has been completed wherein 30 T1DM patients used the app for 3–6 months. Most of the users reported that the tool was feasible and useful to use on a daily basis. The BG function was the most popular, and many users recorded food intake, but the personal goal-setting function was seldom used. Generally, the T1DM patients expected much greater functionality from a mobile tool like this than the T2DM patients did, even though the T2DM group was using a version of the app that had less functionality. Specialist and diabetes nurses were positive to their patients using this tool. However, the potential for such apps is dependent on how HC personnel can be engaged in interacting with the system and how the system and the personnel’s efforts can be reimbursed.
Food Picture Diary for People with Type 1 Diabetes
Due to the major impact of food on BG levels, an approximate recording of nutrition intake may not be sufficient to understand the reason for unwanted glucose excursions. This is especially relevant for young people with T1DM, where BG values generally vary more than what is normal. Thus, a more detailed method for food recording might be helpful in the process of analyzing challenging situations.
Based on the previously described FTA, a module for using the mobile phone’s built-in camera has been designed for easy capture of food and drink intake. This module also automatically incorporates the last relevant BG readings, insulin injections, and physical activity as part of the picture taken; see Figure 4. Users themselves and/or their caregivers may then gain an improved overview of the situation from this aggregated feedback, both on the phone and on a personal computer.
Figure 4.
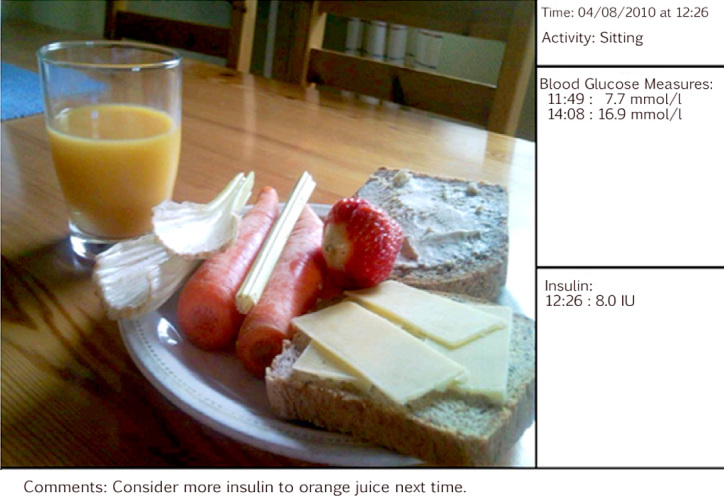
Example of a photographed meal with accumulated data: physical activity, BG values, insulin, and user’s comment.
Eleven adolescents used this tool in interaction with their medical doctor over a period of 3 months. The patients reported an increased understanding of their diabetes treatment. Earlier reports on taking pictures of each meal indicated that this was a tedious and interruptive action among adults with T1DM.18 Therefore, this study was based on 3 days’ data as an alternative way of using such apps. Short, intensive learning periods as a way to identify obstacles in reaching the treatment goals seemed to be well adapted to the adolescent group.
Physical Activity Monitoring for Type 2 Diabetes
The study of the automated BG monitoring module revealed that automatic data transfer functionalities were critical to usability and patient acceptance of the system.11 Therefore, the physical activity module was designed with similar automatic data transfer (Bluetooth) from the patient’s step counter to the diabetes diary on the mobile phone.19 Transfer was done automatically every evening (10 p.m.). The user could also transfer data on demand by pushing the only button on the step counter. The step counter was designed to have no LCD (liquid crystal display), since all interaction was to be done from the mobile phone app; see Figure 5.
Figure 5.
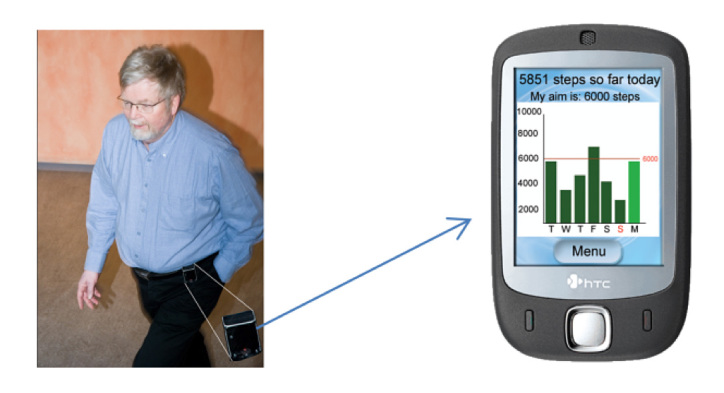
System for automatic transfer of step counts from sensor to phone.
The 15 T2DM users involved in the design process wanted the functions of a step counter to be as automatic and easy to use as possible. Furthermore, they said that tools for self-help should be integrated with their daily tools and outfits, which was not fully achieved for our study,13 since the step counter was perceived as rather large and bulky. Most of the users liked the simplicity and motivational feedback from the step counter system, but some expressed a need for a system that could record activities other than step-like movements.
Nutrition Information for Type 2 Diabetes
Feedback from a 6-month test among 12 T2DM patients13 revealed that food information was the most attractive category for users to look up on the mobile FTA system. Future wishes were enriched information about foods and meals. The information should be easily available so that it can give useful information to enable better decisions on food choices and improve understanding about nutritional aspects in relation to the users’ BG levels.
To understand the users’ needs in detail, paper proto-typing sessions were arranged. These revealed needs for more practical tips and information about food; the information should be easy to read and should include carbohydrate data. Users wanted the food-specific information to include suggestions for alternative foods, comparison based on nutritional content, ways of preparing the food, and energy content in relation to recommended energy intake from protein, fat, and carbohydrate. Relevant literature20,21 describes the use of food information on handheld devices and the difficulties in finding food items a user wants—even though, or because, the database contains several thousand food items. Especially for people with T2DM, it seems to be more important to get approximate ideas of how much impact a food item has on the BG level than to record very precise amounts of carbohydrate.
Context Sensitivity in Mobile Self-Help Tools
Usability is critical in the design of self-help systems for people with diseases that require considerable attention 24/7. Such systems should ideally become a natural part of the patient’s life and should be as unobtrusive as possible. We therefore researched how to make the mobile phone platform more “aware” of or sensitive to its environment, as well as how to make the self-help system adapt to the patients’ needs. For example, the system should be able to sense the patient’s context and be “smart” enough to tell when it is best for the various disease-management components to interact with the patient.
An engineering approach was used for system design, resulting in a prototype that uses data from a step counter and the mobile phone’s calendar, microphone, camera, battery, and system clock as sources of context information.22 Physical activity data are used to detect whether the patient is stationary (sitting or standing), walking, or moving fast; calendar data reveal whether the patient is currently busy with planned events, etc. The use of such context data is also essential in controlling the actions to be taken by the system, exemplified by the ambient noise level acquired from the microphone, which is used both to adapt the phone’s volume to the surrounding noise levels and to determine whether the interaction with the self-help system should be initiated at all.
A survey among 11 people with T2DM showed that context-sensitive functionalities was a feature that they wanted, and user tests demonstrated that the framework was useful in creating an environment that could improve usability of mobile self-help apps.22 Although the work was based mostly on improvised techniques for sensing the context of use, the potential can be considered promising. Increasing availability and openness of embedded sensors in mobile devices will eventually result in more accurate and adaptive apps that are aware of their context of use, e.g., the RingDimmer app.23
Modeling of Blood Glucose using Mobile Phones
We have demonstrated that it is possible to gather patient data on BG and related physiological parameters, as well as how to provide visualization of statistically generated feedback. The data are often not used much beyond immediate investigation, and providing patients with data-driven feedback may be beneficial in understanding patterns in BG. A study involving 30 T1DM patients was arranged to gather data on BG, exercise, diet, and insulin to understand the quality of the data that can be expected in realistic settings and which types of feedback could be considered. We found that the module for approximate food records meant that predictive modeling was not directly possible. However, useful feedback can be provided by detecting significant periodicities and displaying them to the user as evolution of the BG over a typical day. Pattern recognition techniques can be used to find patterns that reliably predict low or high BG and can provide important learning points for the user.
Mobile phone-gathered data from T2DM patients have provided important insight into the problem, demonstrating that scale-space techniques are an important way to assess the data retrospectively.24 Finding live scale-space trends can be useful in that they show current long- or short-term trends in BG and can motivate the user in maintaining a long-term decreasing trend if that is desirable.15
Analyses of the Findings
For the 10 studies and feature sets, Table 2 sums up the main design functions and the main arguments for considering such functions in mHealth apps.
Table 2.
Main Design Functions and Arguments for the 10 Presented Feature Sets
| Set | Main design function | Main arguments |
|---|---|---|
| 1 | Automatic BG data transfer | Easy to use, reassuring |
| 2 | Educational SMS | Facilitates communication |
| 3 | Mobile T2DM diary | Encourages reflection |
| 4 | Diary integration with HC providers | Enhances discussions |
| 5 | Mobile T1DM diary | Useful, motivational, own phone |
| 6 | Mobile picture diary | Way of detecting treatment obstacles |
| 7 | Automatic step counter | Motivating, increase physical activity |
| 8 | Food information on phone | Attractive, approximate information sufficient |
| 9 | Context sensitivity | Positive prospects, phones support it |
| 10 | Mobile BG modeling | Promising for motivated T1DM users |
All studies involve either research on a specific version of a mobile phone-based diary or a component or feature of such a diary. The users in the various studies have been generally positive to one or more components of the designs, and we consider the following elements of great importance in future designs:
Automatic data transfer when possible;
Motivational and visual user interfaces;
Applications should provide considerable health benefits in relation to the effort required; and
Dynamic usage, e.g., both personal and together with HC personnel, long-/short-term perspective, etc.
Another important but more challenging element is the inclusion of context sensitivity in apps. This is especially relevant because patients as user groups are already loaded with devices and/or routines to handle, and context sensitivity should be used in efforts to improve usability. Usability can also be increased by making it possible to run apps on a user-chosen mobile phone and to integrate apps with current tools and routines.
Discussion
For the 10 apps described, we have actively engaged end users and/or referred to user data in all phases of the design and evaluation. This seems to have been one of the overall success factors in being able to design and test relevant mobile apps in everyday life settings. Making health systems that are part of the user’s daily life is argued to be important by, for example, Krishna and colleagues,25 who state that technologies that are already a part of people’s daily lives, such as mobile phones and SMSs, have potential to affect self-management and improve people’s health.
Mature, Immature, and Future Features
We have presented summaries of our design research across a portfolio of FTA feature sets. All have been evaluated and well received by representative patients; many offer strong commercialization potential and market appeal (feature sets 1–7). It is important for further usage that mHealth apps are made available for the various mobile platforms. The feature sets 8–10 are still in the developmental process, involving more uncertainty and higher risks in connection with both technical and medical feasibility, and we encourage the research community to help us explore such possibilities. We believe that the integration of mobile apps with existing diabetes equipment and mobile phones is especially important in future development. Mobile health apps are currently being developed and used for many chronic diseases.26 It is also important to focus on how to make services that are cost-effective. Furthermore, we encourage reviews of mobile apps across different chronic diseases to gain knowledge from various disease fields to help design sound future features.
Interaction with Health Care Sector
A recent review by Holtz and Lauckner27 identified 21 articles describing studies of mobile phone use for diabetes management where interaction with health providers was sparsely reported. To establish new systems like mobile apps as services available to patients, the HC sector must be involved in one way or another. It is of utter importance that HC providers open up for implementing such modern communication tools to facilitate the self-management potential reported in our studies. Our aim is to integrate and find ways to utilize the mobile and patient-operated disease-management apps in various HC settings. If we and others succeed with this, the outcome may be new ways of delivering HC to people living with chronic conditions. Consequently, the traditional role of a patient as a passive recipient of care will hopefully be changed drastically to that of an active participant in the management of his or her disease(s).
Limitations and Barriers
A limitation of participatory design processes, thus also for our studies, is the selection bias, i.e., that it may be difficult to find representative users for the patient group in general. The Hawthorne effect is also a factor to be considered in such studies. The presented portfolio of feature sets are all based on the same mobile platform. Using only one platform provides a momentum resulting from greater knowledge by focusing on fewer technologies, reuse of common components, and more stability for the apps. This is however also a limitation—not representing the most desired situation, where end users prefer to download apps to their own chosen type of mobile phone. In the preface of Diabetes Spectrum’s special section devoted to technology in 2008, Hirsch28 provides examples of several barriers that impede patients from using and benefiting from new diabetes technology. However, this should not discourage us from implementing such technology in diabetes treatment but should rather stimulate a variety of designs to meet the different needs of end users.
Conclusions
Utilizing mobile ICT for self-management has been addressed by our research group and others for some years now. The current developments indicate that we are closer than ever to the goal where useful apps will eventually reach end users. We want to underline the importance of reviewing existing possibilities when designing apps. Our hope is that this article will help to demonstrate some possibilities and that the presented lessons learned and the design implications will be helpful for various actors working with diabetes technology. We highlight the importance of engaging representative end users in all phases of design and implementation. Further development of sound and motivating apps and mobile systems is needed. The tools and possibilities for doing this are very good.
Acknowledgments
We want to thank all the participants in the cohorts, our colleagues and health care professionals involved in the projects and studies, and especially the nurses and the endocrinologist Ragnar M. Joakimsen at the Department of Endocrinology at the University Hospital of North Norway. We also want to thank our former colleague Geir Østengen and the system developers Niklas Andersson, Ragnhild Varmedal, Thomas Samuelsen, and Daniel Hallgren for the great efforts they have devoted to the applications and studies presented.
Glossary
- (app)
application
- (BG)
blood glucose
- (FTA)
Few Touch Application
- (HC)
health care
- (ICT)
information and communication technology
- (mHealth)
mobile health
- (PHA)
personal health application
- (SMS)
short message service
- (T1DM)
type 1 diabetes mellitus
- (T2DM)
type 2 diabetes mellitus
Funding
This work was supported in part by the Research Program for Telemedicine of Helse Nord RHF, Norway; the Centre for Research Driven Innovation: Tromsø Telemedicine Laboratory (Norwegian Research Council Grant No. 174934); the Norwegian health and rehabilitation foundation (Helse og Rehabilitering); the Norwegian Centre for Integrated Care and Telemedicine; the University Hospital of North Norway; the University of Tromsø; and Novo Nordic Norway.
References
- 1.The Global Burden. International Diabetes Federation. http://www.idf.org/diabetesatlas/5e/the-global-burden Accessed March 19, 2012.
- 2.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 3.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tatara N, Arsand E, Nilsen H, Hartvigsen G. A Review of Mobile Terminal-Based Applications for Self-Management of Patients with Diabetes. Presented at: 2009 International Conference on eHealth, Telemedicine, and Social Medicine (eTELEMED 2009); February 1–7, 2009; Cancun, Mexico. Norwegian Centre for Telemedicine, University Hospital of North Norway. [Google Scholar]
- 5.Jensen KL, Larsen LB. Evaluating the usefulness of mobile services based on captured usage data from longitudinal field trials. Presented at: the 4th International Conference on Mobile Technology, Applications, and Systems and the 1st International Symposium on Computer Human Interaction in Mobile Technology, Mobility Conference 2007; September 10–12, 2007; Singapore. [Google Scholar]
- 6.Fogg BJ, Eckles D, Bogost I, Consolvo S, Holmen E, Spasojevic M, Ulm J, Tanguay S, Walker S, White S. Mobile Persuasion: 20 Perspectives of the Future of Behavior Change. Palo Alto (CA): Stanford Captology Media; 2007. [Google Scholar]
- 7.Tufano JT, Karras BT. Mobile eHealth interventions for obesity: a timely opportunity to leverage convergence trends. J Med Internet Res. 2005;7(5):e58. doi: 10.2196/jmir.7.5.e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arsand E, Demiris G. User-centered methods for designing patient-centric self-help tools. Inform Health Soc Care. 2008;33(3):158–169. doi: 10.1080/17538150802457562. [DOI] [PubMed] [Google Scholar]
- 9.Årsand E, Andersson N, Hartvigsen G. No-Touch Wireless Transfer of Blood Glucose Sensor Data. Presented at: COGIS ‘ 07; COGnitive systems with Interactive Sensors; November 26–27, 2007; Stanford University, Stanford, CA. [Google Scholar]
- 10.Polytel® Wireless Glucose Meter Accessory (GMA) The Polytel® System. Polymap Wireless. http://www.polymapwireless.com/Products/PolytelGMA.aspx Accessed March 21, 2012.
- 11.Gammon D, Arsand E, Walseth OA, Andersson N, Jenssen M, Taylor T. Parent-child interaction using a mobile and wireless system for blood glucose monitoring. J Med Internet Res. 2005;7(5):e57. doi: 10.2196/jmir.7.5.e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. J Telemed Telecare. 2006;12(Suppl 1):55–56. doi: 10.1258/135763306777978515. [DOI] [PubMed] [Google Scholar]
- 13.Arsand E, Tatara N, Østengen G, Hartvigsen G. Mobile phone-based self-management tools for type 2 diabetes: the few touch application. J Diabetes Sci Technol. 2010;4(2):328–336. doi: 10.1177/193229681000400213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Årsand E, Walseth OA, Skipenes E. Blood glucose data into Electronic Health Care Records for diabetes management. Presented at: the second HelsIT Conference at the Healtcare Informatics Week; September 20–24, 2004; Trondheim, Norway. www.ub.uit.no/munin/bitstream/10037/2762/4/thesis.pdf. [Google Scholar]
- 15.Skrøvseth SO, Årsand E, Godtliebsen F, Joakimsen RM. Model Driven Mobile Care for Patients with Type 1 Diabetes. Studies in Health Technology and Informatics. 2012;180:1045–1049. [PubMed] [Google Scholar]
- 16.Self-management in Type 2 Diabetes Patients Using the Few Touch Application. ClinicalTrials.gov. U.S. National Institutes of Health. http://clinicaltrials.gov/ct2/show/NCT01315756.
- 17. Project admin. RENEWING HEALTH. http://www.renewinghealth.eu/ Accessed March 24, 2012.
- 18.Arsand E, Tufano JT, Ralston JD, Hjortdahl P. Designing mobile dietary management support technologies for people with diabetes. J Telemed Telecare. 2008;14(7):329–332. doi: 10.1258/jtt.2008.007001. [DOI] [PubMed] [Google Scholar]
- 19.Arsand E, Olsen OA, Varmedal R, Mortensen W, Hartvigsen G. A system for monitoring physical activity data among people with type 2 diabetes. Stud Health Technol Inform. 2008;136:113–118. [PubMed] [Google Scholar]
- 20.Yon BA, Johnson RK, Harvey-Berino J, Gold BC, Howard AB. Personal digital assistants are comparable to traditional diaries for dietary self-monitoring during a weight loss program. J Behav Med. 2007;30(2):165–175. doi: 10.1007/s10865-006-9092-1. Epub 2007 Jan 10. [DOI] [PubMed] [Google Scholar]
- 21.Ma Y, Olendzki BC, Chiriboga D, Rosal M, Sinagra E, Crawford S, Hafner AR, Pagoto SL, Magner RP, Ockene IS. PDA-assisted low glycemic index dietary intervention for type II diabetes: a pilot study. Eur J Clin Nutr. 2006;60(10):1235–1243. doi: 10.1038/sj.ejcn.1602443. Epub 2006 May 17. [DOI] [PubMed] [Google Scholar]
- 22.Chomutare TF. A context-sensitive framework for mobile terminals for assisting Type 2 diabetes patients. Munin. http://munin.uit.no/handle/10037/1632 Acessed April 20, 2012.
- 23.RingDimmer. Android Apps on Google Play. https://play.google.com/store/apps/details?id=com.michaelpardo.ringdimmer Accessed March 26, 2012.
- 24.Skrøvseth SO, Godtliebsen F. Scale space methods for analysis of type 2 diabetes patients’ blood glucose values. Comput Math Methods Med. 2011 doi: 10.1155/2011/672039. 2011:672039. Epub 2011 Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 26.Blake H. Mobile phone technology in chronic disease management. Nurs Stand. 2008;23(12):43–46. doi: 10.7748/ns2008.11.23.12.43.c6728. [DOI] [PubMed] [Google Scholar]
- 27.Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health. 2012;18(3):175–184. doi: 10.1089/tmj.2011.0119. Epub 2012 Feb 22. [DOI] [PubMed] [Google Scholar]
- 28.Hirsch IB. Diabetes Technology Update: Practical Information for Clinicians. Diabetes Spectrum. 2008;21(2):71–72. [Google Scholar]