Abstract
Background:
Epidemiological data pertaining to maternal mortality is valuable in each set up to design interventional programs to favourably reduce the ratio. This study was done to evaluate the maternal mortality rate in our hospital, to assess the epidemiological aspects and causes of maternal mortality, and to suggest recommendations for improvement.
Methods:
This was a 10 year retrospective study. Epidemiological data was collected from the hospital register and maternal mortality ratio, epidemiological factors and causes affecting maternal mortality were assessed.
Results:
A total of 120 maternal deaths occurred. Most maternal deaths occurred in the age group of 20–24 years, multiparous women (56.66%), women from rural areas (69.16%), illiterate women (65%), unbooked patients (83.33%), and patients of low socioeconomic status (83.33%). Direct causes accounted for 72.5% of maternal deaths where as 27.5% of maternal deaths were due to indirect causes.
Conclusion:
There is a wide scope for improvement as a large proportion of the observed deaths are preventable.
Keywords: Maternal mortality ratio, maternal mortality, prevention
INTRODUCTION
According to the World Health Organization (WHO), “A maternal death is defined as death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to or aggravated by pregnancy or its management” (ICD-10). Almost half a million women die every year from complications during pregnancy and childbirth. About 99% of these women are from developing world with over 90% concentrated in Africa and Asia. The current maternal mortality ratio (MMR) in India is 212/100,000 live births.[1] The tragedy is that these deaths are largely preventable. The progress in maternal health has been uneven, inequitable, and unsatisfactory. The risk of a woman dying as a result of pregnancy and childbirth during her lifetime is about 1 in 6 in Afghanistan compared with 1 in 30,000 in Northern Europe.[2]
United Nation (UN) report card on Millennium Development Goal-5 concluded that little progress had been made in sub-Saharan Africa where half of all maternal deaths take place. The progress shown by the South Asian countries including India which accounts for 25% of all maternal deaths is also not impressive.[3]
Most of the evidence for maternal mortality is obtained through hospital data and community based reports, which are situated mostly in urban areas, whereas most of the maternal deaths are from rural areas. This study was done to assess maternal mortality in a tertiary medical college hospital situated in semi urban part of western Maharashtra where large numbers of patients are referred from rural parts of western Maharashtra and North Karnataka. This study was done to assess the local causes of maternal mortality and suggest remedial measures to reduce the same.
Aims and objectives
To calculate the maternal mortality rate in our hospital.
To assess the epidemiological aspects of maternal mortality.
To assess the causes of maternal mortality.
To suggest ways to reduce the MMR.
METHODS
Our Hospital is a semi-urban, tertiary care center; situated in the southernmost part of Western Maharashtra. It gets a large number of referrals from maternity homes, Primary health centers from rural parts of western Maharashtra, and also from North Karnataka. The present study was a retrospective study, conducted in the department of Obstetrics and Gynecology of this hospital. Data regarding maternal mortality was collected from maternal mortality Register after obtaining permission from the Medical Superintendent of the hospital. The details of maternal deaths from January 2001 to December 2010 were collected and analyzed with respect to following epidemiological parameters.
Locality wise distribution of maternal deaths.
Literacy wise distribution of maternal deaths.
Gravidity wise distribution of maternal deaths.
Maternal deaths according to receipt of antenatal care.
Distribution of maternal deaths according to socioeconomic status.
Causes of maternal deaths.
Descriptive data was tabulated as absolute figures and percentages.
The details of number of live births from January 2001 to December 2010 were collected from labor ward register.
Maternal mortality rate for the study period was calculated by using the formula-
![]()
Mean maternal mortality ratio for the study period was calculated by calculating the mean of yearly MMR of the entire study period.
RESULTS
During the study period, January 2001 to December 2010, there were a total of 39704 live births and 120 maternal deaths. The mean maternal mortality rate in the study period was 302.23/100000 live births.
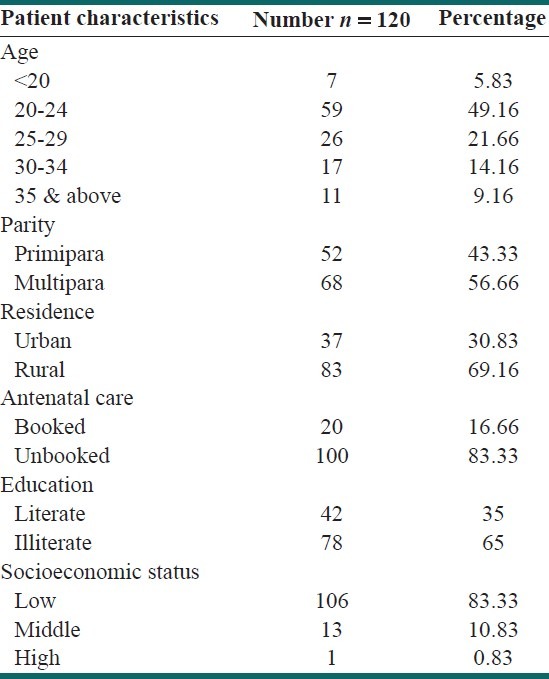
The epidemiological characteristics of maternal deaths are shown in Table 1. Maximum maternal deaths (49.16%) were reported in the age group of 20 to 24 years. More deaths were reported in multiparous women (56.66%) as compared to Primiparas. (43.33%), More maternal deaths were reported in women from rural areas (69.16%) as compared to women from urban areas (30.83%).Maximum maternal deaths were reported in unbooked patients (83.33%) as compared to booked patients (16.66%). Sixty-five percent of maternal deaths were reported in illiterate women. Most maternal deaths (83.33%) were reported in women with low socioeconomic status.
Table 1.
Epidemiological characteristics of maternal deaths (n = 120)
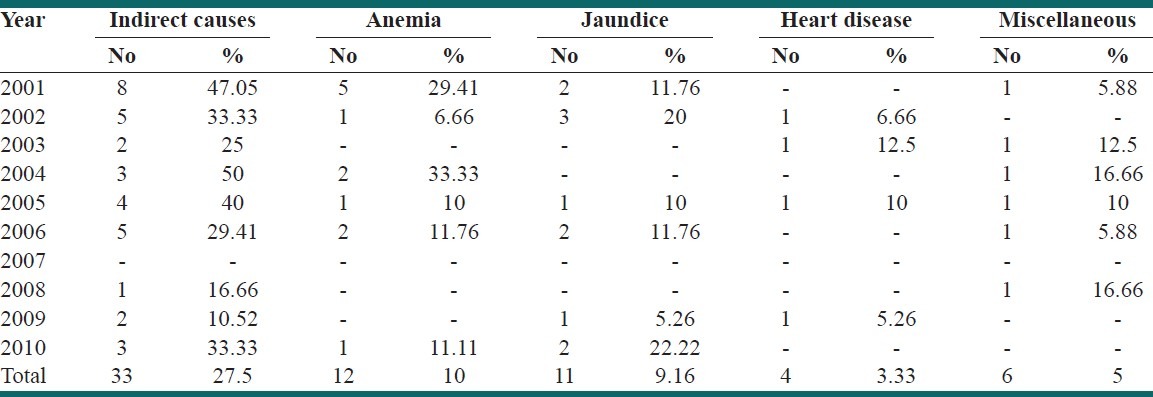
In the study period, 72.5% of maternal deaths were due to direct causes. Year-wise distribution of direct causes of maternal deaths is shown in Table 2. The classical triad of hemorrhage (26.66%), eclampsia (26.66%), and sepsis (18.33%) was the major direct causes of maternal deaths, whereas only one maternal death (0.83%) was due to obstructed labor. In the study period, 27.5% of maternal deaths were due to indirect causes. Anemia, jaundice, and heart disease accounted for 10%, 9.16%, and 3.33% of maternal deaths respectively and miscellaneous cause like acute gastroenteritis accounted for 5% of maternal deaths as shown in Table 3.
Table 2.
Year-wise distribution of direct causes of maternal deaths
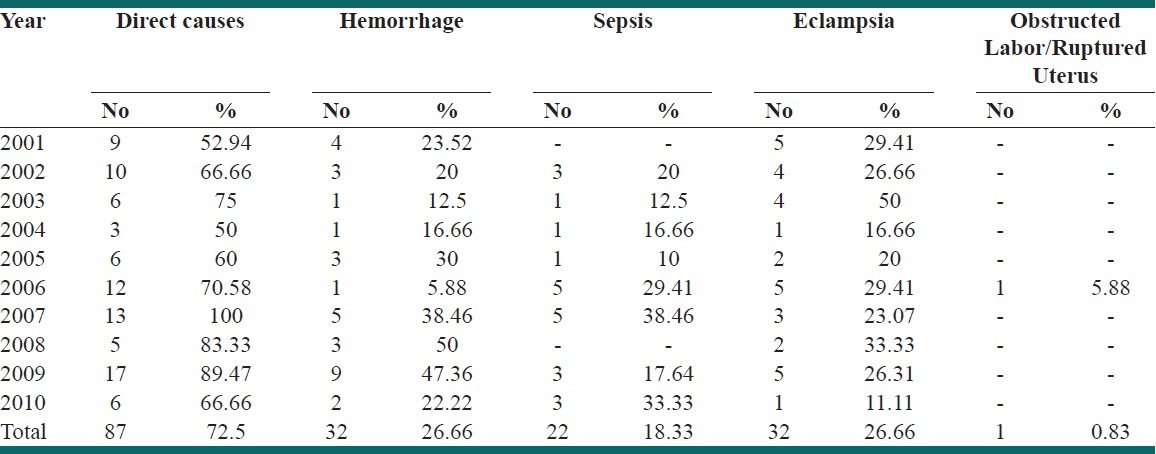
Table 3.
Indirect causes of maternal deaths
DISCUSSION
Maternal mortality is an index of reproductive health of the society. High incidence of maternal deaths reflects poor quality of maternal services, late referral and low socioeconomic status of the community. The mean Maternal mortality rate in the study period was 302.23/100000 births. The current maternal mortality ratio (MMR) in India is 212/100,000 live births.[1] Various studies done in India in the last 15 years have shown wide variation in MMR ranging from 47/100000 to 625/100000 births.[4–9] Madhu Jain has reported a very high MMR of 2270/100000.[5] This study has comparatively high MMR, which could be due to the fact, that our hospital is a tertiary care hospital and receives a lot of complicated referrals from rural areas of southern Maharashtra and also from North Karnataka at a very late stage.
In our study, 70% of maternal deaths were in the age group of 20 to 29 years, as highest numbers of births are reported in this age group. Similarly, 56.66% of maternal deaths were reported in multiparous patients. More maternal deaths were reported in women from rural areas (69.16%), unbooked patients (83.33%), illiterate women (65%), and women belonging to low socioeconomic status. (83.33%) All our findings were similar to studies by Jain,[5] Jadhav,[6] Pal,[7] Onakewhor.[8]
In our study, 72.5% of maternal deaths were due to direct causes. Hemorrhage (26.66%), eclampsia (26.66%), and sepsis (18.33%) were the major direct causes of maternal deaths. Our findings were consistent with studies by Jain,[5] Jadhav,[6] Pal,[7] Onakewhor,[8] and Shah.[9]
Even today large number of maternal deaths is due to the classical triad of hemorrhage, sepsis, and eclampsia. All these are preventable causes of maternal mortality provided the treatment is instituted in time. Unfortunately, in many cases, patients were referred very late, in critical condition, unaccompanied by health care worker. Many patients had to travel a distance of 70 to 80 kilometers in a private vehicle to reach our tertiary center. Most of these deaths are preventable if patients are given appropriate treatment at periphery and timely referred to higher centers. Training of medical officers and staff nurses working in rural areas by programs like basic emergency obstetrics care (BEMOC) and skilled attendant at birth (SAB) training gives a ray of hope of reducing maternal mortality.
Indirect causes accounted for 27.5% of maternal deaths in our study. Anemia, jaundice, and heart disease were responsible for 10%, 9.16%, and 3.33% of maternal deaths, respectively. These findings were consistent with studies by Jain,[5] Jadhav,[6] Pal,[7] and Onakewhor.[8]
Maternal deaths can be prevented by improving the health care facilities in rural areas by ensuring round the clock availability of certain basic drugs like injection magnesium sulfate, tablet misoprostol as most maternal deaths in rural areas are still due to eclampsia and post partum hemorrhage. Early detection of high risk pregnancies and referring them to a tertiary center at the earliest can reduce the complications of high risk pregnancies. National Rural Health Mission (NRHM) can play a major role in reducing maternal mortality by advocating institutional deliveries and timely referral of high risk cases. Although we have not actually evaluated the impact of aforementioned educational programs on maternal mortality, it would be interesting to direct future studies in this regard.
CONCLUSIONS
Even today most maternal deaths are seen in patients from rural areas, unbooked, illiterate patients and patients from low socioeconomic status. Hemorrhage, Eclampsia and sepsis are the major causes of maternal deaths. Improvement in primary health care in rural areas and proper implementation of NRHM programs and up gradation of hospitals in rural areas can definitely bring down the number of maternal deaths.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Special Bulletin on Maternal Mortality in India 2007-09: Sample registration system, Office of Registrar General, India. 2011 Jun [Google Scholar]
- 2.Ronsmans C, Graham WJ Lancet Maternal Survival Series steering group. Maternal mortality: Who, when, where and why. Lancet. 2006;368:1189–200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- 3.The Millennium Development Goals Report 2009. New York: United Nations; 2009. [Google Scholar]
- 4.Puri A, Yadav I, Jain N. Maternal mortality in an urban Tertiary care hospital of north India. J Obstet Gynaecol India. 2011;61:280–5. [Google Scholar]
- 5.Jain M, Maharahaje S. Maternal mortality: A retrospective analysis of ten years in a tertiary hospital. Indian J Prev Soc Med. 2003;34:103–11. [Google Scholar]
- 6.Jadhav AJ, Rote PG. Maternal mortality–changing trends. J Obstet Gynaecol India. 2007;57:398–400. [Google Scholar]
- 7.Pal A, Ray P, Hazra S, Mondal TK. Review of changing trends in maternal mortality in a rural medical college in west Bengal. J Obstet Gynecol India. 2005;55:521–4. [Google Scholar]
- 8.Onakewhor JU, Gharoro EP. Changing trends in maternal mortality in a developing country. Niger J Clin Pract. 2008;11:111–20. [PubMed] [Google Scholar]
- 9.Shah RJ, Ali I, Banday A, Fazili A, Khan I. Analysis of maternal mortality in a small teaching hospital attached to tertiary care hospital. Indian J Community Med. 2008;33:260–2. doi: 10.4103/0970-0218.43234. [DOI] [PMC free article] [PubMed] [Google Scholar]


