Abstract
Diabetes self-management (DSM) training helps prevent diabetic complications. eHealth approaches may improve its optimal use. The aims were to determine a) acceptability of e-HealthyStrides© (an interactive, Internet-based, patient-driven, diabetes self-management support and social networking program) among Morehouse Community Physicians’ Network diabetics; b) efficacy for DSM behavior change c) success factors for use of e-HealthyStrides©. Baseline characteristics of pilot study participants are reported. Of those approached, 13.8% agreed to participate. Among participants, 96% were Black, 77% female; age 56±9.2 years; education: 44% college or higher and 15% less than 12th grade; 92.5% with home computers. Over half (51%) failed the Diabetes Knowledge Test. Nearly half (47%) were at goal A1C; 24% at goal blood pressure; 3% at goal LDL cholesterol level. Median (SD) Diabetes Empowerment Scale score = 3.93 (0.72) but managing psychosocial aspects = 3.89 (0.89) scored lower than other domains. There was low overall confidence for DSM behaviors. Assistance with healthy eating was the most frequently requested service. Requestors were more obese with worse A1C than others. Chronic care delivery scored average with high scores for counseling and problem solving but low scores for care coordination and follow up.
Keywords: Self-management skills, diabetes mellitus, ehealth, psychosocial, empowerment, chronic illness care, consumer health information technologies, health coach, Internet-based, interactive health technologies, African Americans, primary care
Diabetes is a complex chronic disease that affects one in 10 Americans. African Americans and other minorities bear a disproportionate burden of the disease and its adverse outcomes.1 Diabetes care is expensive and the condition leads to serious complications including kidney failure, myocardial Infarction, stroke, blindness and limb amputation.2–3 There is now strong evidence regarding the benefits of aggressive glycemic control in reducing the risk for and delaying the progression of diabetes complications.4–6 However, aggressive glycemic control requires a lifelong adherence to complex lifestyle management involving routine blood glucose monitoring, self-adjustment of medications, nutrition management and a physically active lifestyle. In order to increase diabetes self-management motivation and skills, current research emphasizes patient education and close ongoing support from a health care team.7 As a result, diabetes self-management education (DSME) has been recognized as a valuable resource that enables patients to actively participate in managing their own care.8 The Institute of Medicine defines self-management as the task that individuals must undertake to live with one or more chronic conditions.9[p.57] These tasks include having the confidence to deal with medical, behavioral, and emotional management of their conditions. Self-management is the foundation for achieving optimum glucose control necessary to avoid the complications of diabetes through increasing knowledge and awareness and learning effective behavioral techniques to manage diabetes.38,39
Data on the reach of self-management education programs reveals broad variation in attendance at DSME programs. A Maine survey of Medicaid and privately insured patients10,11 revealed that only 24% of insured and newly diagnosed diabetics were attending DSME programs and only 3% of all diabetics participated in DSME programs each year. The top reasons for non-attendance broadly classified, related to patient perception, difficulties with class time or content, psychosocial/patient behavioral issues, issues related to the structure and timing of the educational content or those related to the providers. Patients reported challenges with transportation, insurance, or being overwhelmed with fear or the stress of their lives that caused them to prioritize diabetes care lower. Others didn’t perceive a need for DSME programs because they felt diabetes was a disease of old people. The educational content was considered by some to be difficult to understand or too much for one time; not specifically targeted to the individual patient’s context; or too long. Suggestions were made to expand the format of delivery to alternatives such as the Internet or peer-to-peer learning. Referring provider issues revolved around lack of information among providers about DSME programs and their value; administrative burden of the referral process was sometimes daunting and time pressures of a typical encounter that limit opportunities for discussions about self-management.
Systematic reviews of studies on the effectiveness of diabetes self management education programs12–16 indicate that programs have variable effects on outcomes and in different populations. Suggestions to improve effectiveness of DSME programs include providing education in more formats including the use of the Internet; providing avenues for peer-to-peer interactions and using an empowerment rather than a didactic approach with direct involvement of the health care team for accountability. However, studies that reported use of the Internet for DSME reported poor uptake and high attrition especially for programs with follow-up greater than six months.
Persistence of effects of DSME also vary. These behaviors are often difficult for individuals with diabetes to maintain over time. A large study (The Diabetes Attitudes, Wishes, and Needs—DAWN—Study) of more than 5,000 patients with type 1 and type 2 diabetes and almost 4,000 providers from 13 countries asked about diabetes self-management and related psychosocial issues.17 The results showed that only 46% of patients with type 1 and 39% of patients with type 2 reported achieving success in two-thirds of their self-management behaviors. Suggested approaches to improve persistence revolved around understanding psychosocial variables in the individual, reminders during visits with health care providers and improvement of peer-to-peer interactions and family/community support as well as frequent contact with the educational content.
Given the general reluctance of patients with diabetes to attend diabetes classes and group sessions, Internet-based and other eHealth approaches to diabetes self-management education (DSME) have great potential to meet the requirements for successful diabetes self-management education programs at a relatively low cost, to wit: content that is delivered in context; uses an empowerment approach; involves frequent contact and a supportive environment. However, low participation rates and high levels of attrition are often observed with ehealth programs.18–22 These rates are of concern since studies with a higher utilization tend to have better behavior change outcomes.20 Reasons advanced for poor patient acceptance include poor usability, insufficient training on how to use the technology, physical and environmental constraints (difficulty manipulating the computer mouse due to arthritis or poor vision) and low self-efficacy. The psychosocial predictors of use of such eHealth programs specifically for diabetic African American patients are an area of on-going enquiry that we hope our data will extend.
The Morehouse Community Physicians’ Network (CPN) is a practice-based research network of small independent medical practices that provide care to predominant minority and/or underserved patients.23 Patients in the CPN often have multiple co-morbidities, including a high prevalence of poorly controlled diabetes and hypertension. 24 The reach and effectiveness of DSME in the CPN and similar practices is unknown. We believed that DSME reach would be lower than the recommended goal of 60% for Healthy People 2010,25 so we undertook the e-HealthyStrides© project to test the efficacy of an online interactive program to improve self-management skills among the diabetic patients in our CPN practices. The e-HealthyStrides© application integrates peer-to-peer social networking as well as feedback and counseling from a health coach located at the participants’ primary care practice with round-the-clock availability to encourage frequent use.
We hypothesized that e-HealthyStrides©, an integrated system designed to empower and engage patients and their care team by providing diabetes knowledge, linked to patient-driven results of blood glucose, exercise, and blood pressure monitoring would aid in improving self-management skills attainment, persistence, and reach among adult African American patients with diabetes.
Our specific aims were to determine whether a) diabetic patients in CPN practices would accept and use e-HealthyStrides© to improve DSME; b) patients who used e-HealthyStrides© for DSME would attain 3 of 7 self-management skills they had not attained at baseline, persist in the attainment of those goals; c) patients who used e-HealthyStrides©, would demonstrate improvements in their diabetes outcomes (hemoglobin A1c, blood pressure, lipids) attitudes and knowledge; d) identify success factors for use of e-HealthyStrides© to improve diabetes self-management skills.
In this report, we provide the baseline characteristics of diabetics who volunteered for the program.
Methods
This is a report of the baseline socio-demographic and psychosocial characteristics of participants in the e-HealthyStrides© program.
Program description
We developed an interactive, Internet-based, patient-driven, diabetes self-management support and social networking forum to engage diabetic patients, their physicians and a health coach in the practice, in order to create an environment supportive of improvement in diabetes self-care skills and outcomes. The e-HealthyStrides© application is accessible at https://www.ehealthystrides.org. It consists of an integrated diabetes curriculum and pages for uploading and viewing self-monitored graphic and color-coded parameters such as blood pressure, body mass index, number of steps walked, and blood glucose. The application also included a structured instrument used by the patient to identify and set self-management goals,26 based on the American Association of Diabetes Educators (AADE) seven self-care behaviors (AADE7) goals. In consultation with the health coach, steps required to attain and track these goals were routinely monitored by the patient and shared with the health coach during monthly scheduled calls. The discussion forum was accessible from the e-HealthyStrides© sign on page for conversations among participants from each practice and their health coach and physician. All access was password-protected. Data entered through the e-HealthyStrides© application was stored on the Microsoft© Healthvault™ and all participants in the study received free Microsoft© Healthvault™ accounts as part of the study.
Inclusion/recruitment of patients and practices
Physician practices that belonged to the Morehouse School of Medicine Community Physicians’ Network (CPN) who had electronic medical records and were interested in participating in the study were invited to participate.
A lead physician at each participating site was identified to champion the project. This physician identified an employee in the practice, usually a medical assistant, for training as a health coach.
The physicians and health coaches were oriented to the study processes and the e-HealthyStrides© web application and discussion forum. The health coaches were trained and certified using a program designed by the American Association for Diabetes Educators for staff at the point of care of diabetes. Additional training was provided for the coaches on the use of the structured goal setting and counseling tool, and technical training for web access in order to assist study participants. Each coach was provided with a laptop computer for the duration of the study to facilitate their work. Computers with privacy screens were provided in a suitable location at each practice to facilitate use and access of e-HealthyStrides© for those patients who did not have access to a home computer.
All diabetic patients in each practice were identified using the International Classification of Diseases version 1027 codes for diabetes mellitus. Letters of invitation were sent to all identified patients. Patients who called to opt out did not receive any further contact. The health coach approached others to solicit their participation. Those who agreed were enrolled consecutively by the health coach at each practice. Patients were included if they were diabetic, over the age of 21 and willing and able to use the Internet for the duration of the study. Participants were excluded if they were precluded from doing so by any insurmountable physical impairment. Eligible participants were mailed a packet with study protocol and informed consent prior to attending a training and orientation day at Morehouse School of Medicine. Participants were enrolled at the training/enrollment day after they reviewed and provided signed informed consent, approved by the Morehouse School of Medicine Institutional Review Board.
Study procedures
The participant orientation process was a four-to-five hour, hands-on process, which occurred at a computer laboratory at the main campus of the Morehouse School of Medicine. It was conducted by the authors (PIP, FO) and health coaches from each practice. Once enrolled, all participants (with or without assistance) created email accounts, usernames and passwords, specific to the e-HealthyStrides© application. They were guided through the access and use of e-HealthyStrides© including how to create updated medication lists, how to access their personal e-HealthyStrides© webpage from home; how to use their monitors: sphygmomanometer, glucometers, and pedometers to record and upload information to the Microsoft© Healthvault™ database and how to view the data. They were oriented to the curriculum and associated quizzes, use of the discussion forum and how to keep the usernames and passwords safe.
All participants completed several surveys at enrollment: The Diabetes Empowerment Scale (DES),28–29 Diabetes Knowledge Test (DKT),30–31 Patient Assessment of Chronic Illness Care (PACIC),32 Consumer Health Information Technology survey (CHITs, a locally developed instrument), and the American Association of Diabetes Educators seven self-care behaviors (AADE7).26
At the end of the orientation visit, each participant was provided with a sphygmomanometer, glucometer, and pedometer, all of which were universal serial bus (USB) port enabled to directly interface with the e-HealthyStrides© and up load all monitored data onto each participant’s Microsoft© Healthvault™ account. Participants were encouraged to access all parts of e-HealthyStrides© as often as they could. Incentives were provided for completion of quizzes at the end of each chapter of the curriculum. Participants were encouraged to upload their data at least once a week for those with home access to a computer and once every three weeks for those needing to go to the physicians’ office to upload data. All participants were required to set a self-management behavioral goal and arrange a follow-up call with their health coach for accountability. Coaches were expected to contact each participant at least once per month to review their progress in attainment of their chosen self-management behavioral goal.
Weekly training calls were set up to enable participants to receive on-going help with any difficulties they could be encountering in the early phase of the study. Study personnel and health coaches were available for support of the participants. The study was set up to last for 12 months.
Data sources
The data reviewed in this report included responses to surveys (PACIC, DES, DKT, AADE7, CHITs, and an extract of clinical data from the patients’ medical records).
Data management
Survey responses were all coded by individual participant identification numbers and exported to excel spreadsheets. Subsequently, data were audited for accuracy and appropriateness and exported to STATA®11 for further data analysis. (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP). Medical record data extract was obtainable from 1 of 3 electronic health record systems. Only clinical data for consented participants was used in this analysis.
Scoring criteria
Questionnaires were scored according to guidelines provided by the developers.26,28–32 Scoring was based on completed items or questions. Each item received a score ranging from 1 to 5. An item checked strongly agree received five points; agree, four points; neutral, three points; disagree, two points; and strongly disagree received one point. The PACIC questionnaire (Ques.) has five subscales.32
The Diabetes Knowledge Test was scored out of 23 for diabetics who used insulin and out of 14 (the first 14 questions) for those who did not use insulin.30,31
The Diabetes Empowerment Scale (DES): The Diabetes Empowerment Scale, a 30-item psychosocial self-efficacy scale developed specifically for empowerment-based DSME, contains three subscales addressing patients’ management of the psychosocial aspects of diabetes care, dissatisfaction and readiness to change, and readiness to set and achieve diabetes-related goals. The three subscales were calculated as recommended.28–29
Consumer Health Information Technology Survey (CHITs): The Consumer Health Information Technology survey was locally developed to assess ease or comfort with computer/Internet use, access to a computer at home and to assess attitudes towards consumer health information technologies.
Responses to CHITs questions were coded as follows: Ques 10, 19, 22–27, 32, 33 (1 = strongly agree to 5 = strongly disagree); Ques 12, 20 (Rescaled from 1 = unable 6 = perfectly able); Ques 31 (1 = excellent to 5 = poor). The resulting value is the average score for that subscale.
Statistical analysis
This report presents a descriptive analysis of the baseline socio-demographic and psychosocial characteristics of participants in the e-HealthyStrides© program. Univariate statistics were generated in STATA for psychosocial, demographic and clinical factors obtained from all data sources. Categorical data was summarized using frequencies and percentages, and continuous data summarized using mean (standard deviation). Output from the univariate analysis was used to generate bar graphs and tables included in this report. Further exploratory analysis to assess effect of psycho-social and demographic variables on clinical outcomes will be described in the future.
The research was reviewed and approved by the Morehouse School of Medicine Institutional Review Board.
Results
Seven of the 10 primary care CPN practices with electronic medical records were approached for participation; five agreed and were initially recruited for participation. Of the two that declined participation; one did not have the staff available at the practice to serve as health coach and the other was already involved in another diabetes study. Of the five practices that agreed to participate; two were unable to continue due to one practice moving locations and the other lacking the support of a health coach to carry out significant portions of the proposed study. This report concern the three practices that participated. We sent out 447 invitations for practice #1; and 119 (26.62%) declined participation; 484 invitations for practice #2 with 173 (35.74%) declining participation; 128 invitations for practice #3 with 60 (46.88%) declining participation. Of 1,059 diabetics, 352 (33.2%) declined participation. Seven hundred and seven (66.8%) diabetics did not respond to coaches, but 206 (19.5%) responded, met inclusion criteria, and were scheduled for training and 146 (13.8%) were successfully trained on the use of e-HealthyStrides©. Figure 10 shows participant flow. We were unable to collect any information about participants who refused to take part in the study. A total of 10 (0.94%) participants dropped out early (four from practice #1; one from practice #2 and five from practice #3. Of this number, six were female; one withdrew due to worsening of her health; and two withdrew because their diabetes was medication-related and had resolved. One participant withdrew because she had experienced a lot of stressful life events and could not cope with being in the study as well. No reasons were provided by the other six participants.
Figure 10.
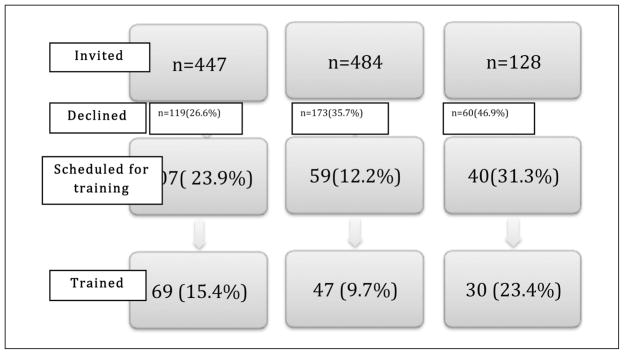
Flow chart of study participants from each practice.
Participant Characteristics
Baseline assessment revealed the following about the participants in e-HealthyStrides© as shown in Table 1: The majority of the participants were female (77%) and Black (~96%). Review of educational attainment showed that only 16% of participants had high school education or less. Nineteen percent of this group had a post-graduate degree and average age was 56±9.2 years. The majority (n=102; 68%) rated their health as average or good, while 32% rated their health poor or below average. Table 2 shows some clinical characteristics of our study population. Fifty-three percent were not at goal for diabetes control reflected in their glycosylated hemoglobin; only 24% had blood pressure controlled and 25% had evidence of significant microalbuminuria, an indication of early diabetic nephropathy. Goal attainment for lipids ranged from 3–56%. Sixty-one respondents (51%) did not attain a passing score on the Diabetes Knowledge Test.
Table 1.
DEMOGRAPHIC CHARACTERISTICS
| Demographic Characteristics | N =141 (%) |
|---|---|
| Gender (Female) | 108 (77%) |
| Ethnicity | |
| Black | 135 (95.7%) |
| Hispanic | 1 (0.71%) |
| White | 2 (1.42%) |
| Other | 3 (2.13%) |
| Education | |
| High school or less | 21 (15.45%) |
| Tech school | 55 (40.44%) |
| College | 34 (25%) |
| Post-grad degree | 26 (19.12%) |
| Diabetes Knowledge test (Pass) | 59 (49.17%) |
| Own a computer? (Yes) | 124 (92.5%) |
| Anxious about ability to use internet? (Yes) | 45 (34.09%) |
| Self rating of ability to use computer? | (n=96) |
| Unable | 12 (9.16%) |
| Less than average | 39 (29.77%) |
| Average | 16 (12.21%) |
| Above average | 64 (48.85%) |
| Self rating of ability to use CHITs | (n=106) |
| Unable | 18 (18.75%) |
| Less than average | 16 (16.67%) |
| Average | 16 (16.67%) |
| Above average | 46 (47.92%) |
CHITs = Consumer Health Information Technologies
Table 2.
clinical characteristcs of the study population
| Characteristic | N (%) |
|---|---|
| Gender (Female) | 54 (79%) |
| HbA1c (At goal) | 32 (47%) |
| Hypertension(At goal) | 16 (24%) |
| Micro albumin/Creatinine (Normal) | 51 (75%) |
| HDL cholesterol (At goal) | 38 (56%) |
| LDL cholesterol (At goal) | 2 (3%) |
| Triglycerides (At goal) | 8 (12%) |
HbA1c = Glycosylated hemoglobin. At Goal <7%
Controlled hypertension in diabetic <135/80 mmHg
Normal Micro albumin/Creatinine <30
HDL cholesterol = High density lipoprotein cholesterol
- At goal females ≥50 mg/dL
- At goal males ≥40 mg/dL
LDL cholesterol = Low density lipoprotein cholesterol.
- At goal for diabetics ≤100 mg/dL
Access and Attitudes to CHITs and Internet resources for health
Ninety-two percent of respondents owned or had access to a computer at home. Regarding self-rated ability to use the computer, 9% reported inability to use computers, and 48% rated themselves as above average with using computers. Similarly, about 35% of respondents considered their ability to use consumer health information technologies (CHITs) to be below average and 48% considered theirs to be above average. Responses from participants suggested that only a minority (n=11; 12%) would feel comfortable asking their physician for help if they experienced difficulties with using CHITs or Internet resources for health; 28 (31.5%) would ask family for help. Forty-eight participants (51%) would stop using the Internet for health or CHITs if they encountered any difficulties. This was reflected in the low scores on a composite score examining overall attitudes towards use of CHITs Internet resources for health as shown in Figure 1.
Figure 1.
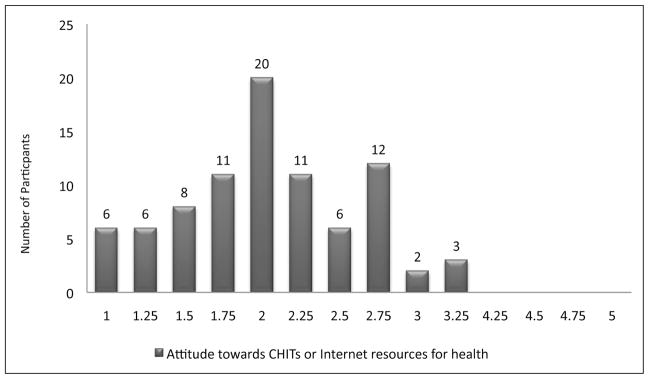
1 = Poorest attitude
5 = Best attitude
Attitudes towards diabetes
As shown in Figure 2–4, overall, median score for diabetes empowerment was 3.93±0.72 (range 1–5). Examination of the subscales of the Diabetes Empowerment Scale (DES) revealed the following: The respondents scored high for assessing dissatisfaction and readiness to change (median 4±0.69); and for setting and achieving goals (median 4±0.77); and somewhat lower on managing psychosocial aspects of diabetes (median 3.89±0.89).
Figure 2.
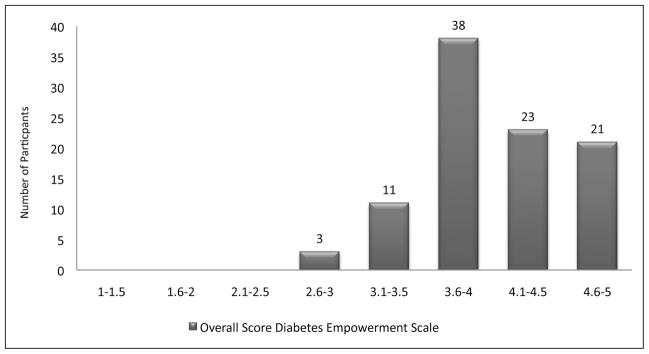
Median (SD) = 3.93 (0.72)
1 = Lowest score for diabetes empowerment
5 = Highest lscore for diabetes empowerment
Figure 4.
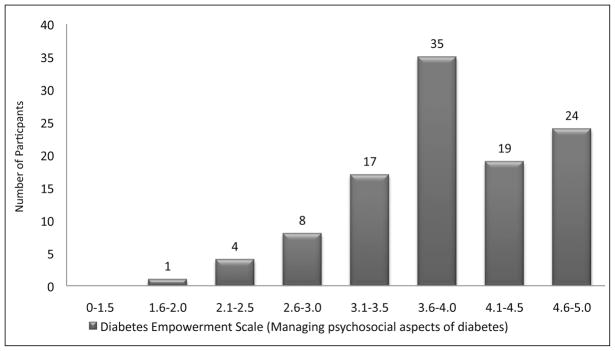
Median (SD) = 3.89 (0.89)
1 = Lowest level of confidence with managing psychosocial aspects of diabetes
5 = Highest level of confidence with managing psychosocial aspects of diabetes
Patient Assessment of Chronic Illness Care (PACIC)
Overall, respondents rated their physicians’ practices average (3.3±1.1) for chronic illness care as shown in Figure 5. The highest scores were in the domains of problem solving/contextual counseling (Figure 6); (median 4±1.3) and delivery system design (Figure 7) (median 3.67±1.1). The lowest score was in the domain of follow-up and care coordination as shown in Figure 8 (median 3±1.2).
Figure 5.
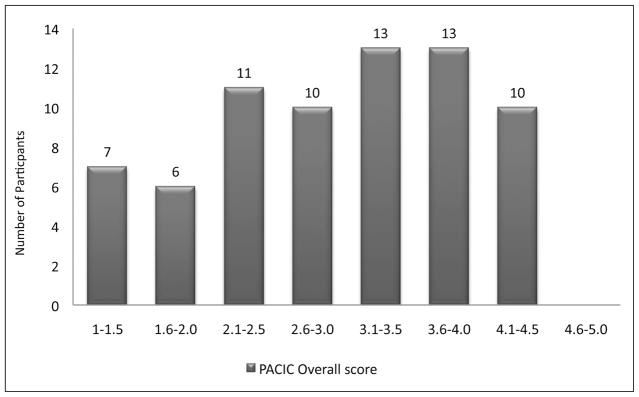
Median (SD) = 3.3 (1.1)
1 = Lowest score for patient assessment of chronic illness care at the practice
5 = Highest score for patient assessment of chronic illness care at the practice
Figure 6.
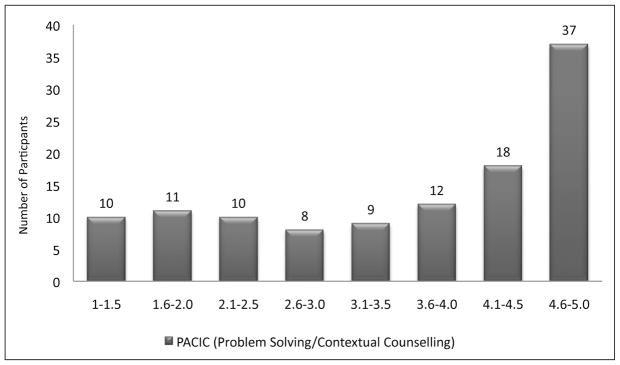
Median (SD) = 4 (1.27)
1 = Lowest score for practice support for contextual counseling and problem solving
5 = Highest score for practice support for contextual counseling and problem solving
Figure 7.
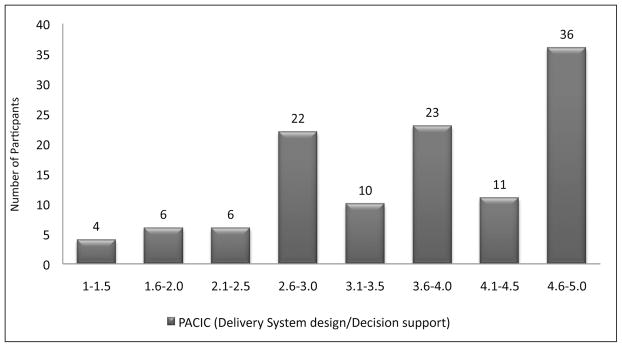
Median (SD) = 3.67 (1.09)
1 = Lowest score for delivery system design/decision support
5 = Highest score for delivery system design/decision support
Figure 8.
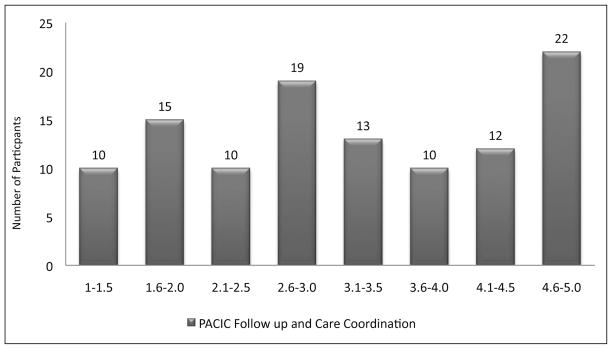
Median (SD) = 3 (1.2)
1 = Lowest score for practice in the area of follow up and care coordination
5 = Highest score for practice in the area of follow up and care coordination
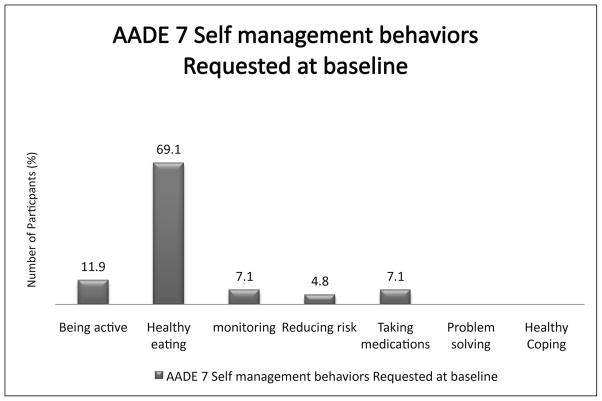
AADE7 self-management behaviors at baseline
Participants expressed low levels of confidence related to all self management behaviors at baseline, with all scores below 4 (Figure 9). The lowest confidence was expressed for monitoring (mean score 3.33±.58) followed by healthy eating (3.41±.57). Among the seven self-care behaviors essential for successful and effective diabetes self-management,26 assistance with healthy eating was most frequently requested (69% of participants). We examined relationships among baseline glycosylated hemoglobin, blood pressure, lipids and self management skills requested at baseline and found that diabetes control (HbA1c), blood pressure (SBP, DBP), lipids and body mass index (BMI) at baseline varied depending on the skills requested; those requesting assistance with healthy eating (mean HbA1c 7.9±1.9) and those requesting assistance with taking medication (mean HbA1c 8.8±2.05) were the least controlled compared with those requesting assistance with being active (HbA1c 6.68±1.1); and monitoring (HbA1c 6.4±.25). Similarly, those requesting assistance with healthy eating (mean BMI 39.8±8.4) and taking medication (mean BMI 40.4±3.5) were more obese than those requesting assistance with being active (BMI 32.50±4.46) and monitoring (BMI 29.18±5.28).
Figure 9.
Discussion
The discussion of findings in this report of the baseline socio-demographic and psychosocial characteristics of participants in the e-HealthyStrides© program must begin with the acknowledgment that only 13.8% of all diabetic patients in the practices agreed to participate in this study. Participants strongly tended to be Black and middle-aged, with diverse educational attainment and good access to computers at home. Despite these resources, a slim majority failed the diabetes knowledge test and in spite of high computer ownership, their self-assurance with Internet use was divided evenly, with one half reporting confidence with using the Internet and consumer health information technologies (CHITs) and the other half reporting an inability or low confidence with using the CHITs.
Overall diabetes control was low, as were control rates for hypertension and lipids. Overall empowerment scores were above average, but scores for managing psychosocial aspects of diabetes were lower than others. Participants’ perception of chronic illness care delivery at their physician’s practice was average but they scored the level of follow-up and care coordination low compared with support for contextual counseling and problem-solving. Their overall confidence related to self-management behaviors relevant to successful diabetes management was low. The most frequent requests for assistance were for developing healthy eating habits; those participants requesting this skill were more obese with worse diabetes control than others. Study participants scored the delivery of chronic illness care as average overall with high scores for contextual counseling and problem-solving but low scores for care coordination and follow up.
These findings are important and significant as they clearly define the study population for future inference and generalizability and they provide information that would guide further program development activities.
Our results confirm that this population has a need for self-management skills training based on their confidence levels with self-management skills and inadequate diabetes control. Furthermore, specific areas of need have been highlighted: skills for healthy eating, support for managing psychosocial aspects of diabetes, and resources for follow-up and care coordination at the practice will be emphasized in the program implementation phase. The need for managing psychosocial aspects of diabetes is not usually reported in studies of clinical outcomes of DSME. However, the impact of psychosocial factors on coping and living with chronic diseases in the population in general is known and we speculate that it would have even greater effects on outcomes in minority and underserved populations. As designed, the e-HealthyStrides© program will provide support for managing psychosocial aspects of diabetes by encouraging peer-to-peer interactions on the discussion forum with rich discussions around issues of mutual concern among this population of diabetics.
The participants in this program were similar in their demographic characteristics to the general primary care population of African American diabetics in the Atlanta area.33–34 However, access to computers at home and the Internet appear to be greater in this group (over 90%) than previously reported in the general population of African Americans.35 Fifty percent of African Americans have Internet access; of those, 93% access the Internet using their computers versus 76% who access the Internet using mobile phones. In our study, 93% reported owning a computer with Internet access however, almost 40% reported below average ability to use the Internet. This is notable since a report on expanding the impact and reach of consumer ehealth tools released by the department of health and human services36 identified factors such as access, health literacy, ability to use the Internet in a meaningful way (“meaningful use”) and behavior related to health information seeking as vital to successful use of ehealth tools such as e-HealthyStrides©. It is a matter of some concern that about half of our study participants expressed discomfort with using the Internet or CHITs and indicated that they would stop using them if they encountered any difficulties. This could lead to attrition and thereby affect the results of our study. The reasons for discomfort with ehealth programs include issues related to self-efficacy with using the program, ease of program use as well as the attitude of the participant to the program. Specific elements in the design of e-HealthyStrides© and our program implementation are geared towards addressing these concerns. We anticipate that the combination of frequent training calls, a familiar health coach, an engaged physician and a detailed interactive training session at the beginning of the study will reduce the likelihood that these negatives will lead to high attrition or failure of uptake of the program. This is supported by Ciminino et al.,37 who demonstrated that participants with low health literacy and inability to use computers were able to persist with use of an ehealth program after a brief training session.
Implications of characteristics of our study population for program participation and drop-out
The characteristics of our population (female, educated, positive outlook towards their health) are among those that have been reported to increase likelihood of remaining with the studies on the Internet.20,22 Our study also addresses an area of need in that it provides information related specifically to patient psychosocial characteristics associated with engagement in Internet programs for diabetes self-management education. Future analysis of qualitative data from focus groups should provide additional information about the patients who used this program, whether successfully or not.
Implications for care coordination and the medical home
This study has identified important gaps that have implications for the ability to effectively coordinate chronic illness care of such vulnerable populations. Future research will evaluate the e-HealthyStrides© application among CPN practices, as a model to improve care coordination and a more patient-centered approach to chronic illness care all of which will help primary care practices to meet requirements for the primary care medical home.
Limitations
In this baseline report of psychosocial and clinical characteristics of e-HealthyStrides©, we had a limited sample of participants for whom clinical data were available. In spite of this limitation, we established that this cohort of participants had similar clinical characteristics to other diabetics. However, we may have been limited in our ability to assess relationships between psychosocial variables and our clinical outcome variables.
Figure 3.
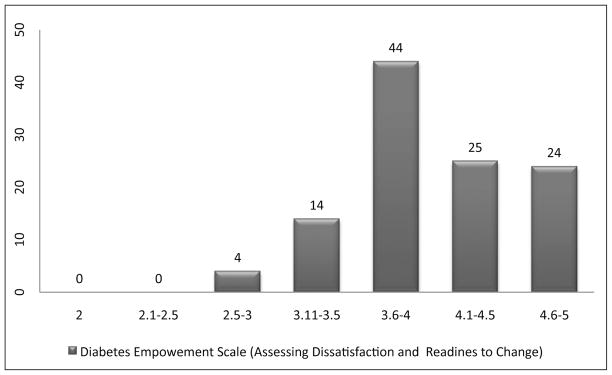
Median (SD) = 4 (0.69)
1 = Lowest level of dissatisfaction and readiness to change
5 = Highest level of dissatisfaction and readiness to change
Acknowledgments
Supported by Grants from Microsoft© Healthvault™ Be Well fund; NIH: #3U54RR026137- S3 2R25RR017694-06A1; 5U54RR022814 and 5P20RR11104 from the National Center for Research Resources, NCRR; CPN physicians: Dr. Janet Bivens, Dr. Kingsley Agbeyegbe, and Dr. Patricia Glenn and all CPN patients.
Notes
- 1.Centers for Disease Control and Prevention (CDC) National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta, GA: CDC; 2011. [Google Scholar]
- 2.Xu J, Kochanek KD, Murphy SL, et al. National Vital Statistics Reports. 19. Vol. 58. Hyattsville, MD: National Center for Health Statistics; 2010. May 20, Deaths: final data for 2007. [PubMed] [Google Scholar]
- 3.American Diabetes Association website. Available at: http://www.diabetes.org/diabetes-basics/diabetes-statistics/
- 4.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993 Sep 30;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 5.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005 Dec 22;353:2643–53. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):837–53. [PubMed] [Google Scholar]
- 7.American Diabetes Association. Third-party reimbursement for diabetes care, self-management education, and supplies. Diabetes Care. 2006 Jan;29(Suppl 1):S68–9. doi: 10.2337/diacare.29.1.68. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. 2004 referenced in a presentation by Kate Lorig. Auburn, Maine: Jun 15, 2006. [Google Scholar]
- 9.Adams K, Corrigan JM, editors. Institute of Medicine. Priority areas for national action: transforming health care quality. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 10.Maine Center for Disease Control and Prevention. Maine Behavioral Risk Factor Surveillance System (BRFSS) 2000–2004. Augusta, ME: Maine Center for Disease Control and Prevention; Division of Public Health Systems; 2010. Available at: http://www.maine.gov/dhhs/boh/phs/odrvs/brfss/index.shtml. [Google Scholar]
- 11.Joly B, O’Rourke K. Diabetes assessment: a systems approach: Maine Diabetes Health System final summary report. Augusta, ME: Maine Department of Health and Human Services; 2004. [Google Scholar]
- 12.Norris SL, Engelgau MM, Naranyan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001 Mar;24(3):561–87. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 13.Gary TL, Genkinger JM, Guallar E, et al. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003 May-Jun;29(3):488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- 14.Deakin T, McShane CE, Cade JE, et al. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005 Apr 18;(2):CD003417. doi: 10.1002/14651858.CD003417.pub2. [DOI] [PubMed] [Google Scholar]
- 15.Renders CM, Valk GD, Griffin SJ, et al. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001 Oct;24(10):1821–33. doi: 10.2337/diacare.24.10.1821. [DOI] [PubMed] [Google Scholar]
- 16.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002 Jul;25(7):1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 17.Peyrot M, Rubin RR, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes, and Needs (DAWN) Study. Diabet Med. 2005 Oct;22(10):1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 18.Norman GJ, Zabinski MF, Adams MA, et al. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007 Oct;33(4):336–45. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eysenbach G. The law of attrition. J Med Internet Res. 2005 Mar 31;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Im EO, Chee W. Methodological issues in the recruitment of ethnic minority subjects to research via the Internet: a discussion paper. Int J Nurs Stud. 2005 Nov;42(8):923–9. doi: 10.1016/j.ijnurstu.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 21.Verheijden MW, Jans MP, Hildebrandt VH, et al. Rates and determinants of repeated participation in a web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res. 2007 Jan 22;9(1):e1. doi: 10.2196/jmir.9.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robroek SJ, van Lenthe FJ, van Empelen P, et al. Determinants of participation in worksite health promotion programmes: a systematic review. Int J Behav Nutr Phys Act. 2009 May 20;6:26. doi: 10.1186/1479-5868-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ofili E, Igho-Pemu P, Lapu-Bula R, et al. The Community Physicians Network (CPN): an academic community partnership to eliminate healthcare disparities. Ethn Dis. 2005 Autumn;15(4 Suppl 5):S5-124–7. [PubMed] [Google Scholar]
- 24.Igho-Pemu P, Quarshie A, Oduwole A, et al. Morehouse Community Physicians Network(CPN) hypertension registry: patterns of care and opportunities for targeted medical education. Etn Dis. 2005 Autumn;15(4 Suppl 5):S5-120–3. [PubMed] [Google Scholar]
- 25.National Center for Health Statistics. Healthy People 2000 final review. Hyattsville, MD: U.S. Department of Health and Human Services; 2001. Available at: http://www.cdc.gov/nchs/data/hp2000/hp2k01.pdf. [Google Scholar]
- 26.AADE. AADE7 self-care behaviors. Diabetes Educ. 2008 May-Jun;34(3):445–9. doi: 10.1177/0145721708316625. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization (WHO) International Classification of Diseases (ICD) 10th revision, clinical modification ICD-10 CM. Geneva, Switzerland: WHO; 2011. Available at: http://www.who.int/classifications/icd/en/ [Google Scholar]
- 28.Anderson RM, Funnell MM, Fitzgerald JT, et al. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000 Jun;23(6):739–43. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- 29.Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995 Jul;18(7):943–9. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 30.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998 May;21(5):706–10. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 31.University of Michigan Health System. Diabetes research and training center: Michigan diabetes research training center materials for health professionals. Ann Arbor, MI: University of Michigan Health System; 2000. [Google Scholar]
- 32.Glasgow RE, Wagner EH, Schaefer J, et al. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005 May;43(5):436–44. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 33.Phillips LS, Hertzberg VS, Cook CB, et al. The Improving Primary Care of African Americans with Diabetes (IPCAAD) project: rationale and design. Control Clin Trials. 2002 Oct;23(5):554–69. doi: 10.1016/s0197-2456(02)00230-1. [DOI] [PubMed] [Google Scholar]
- 34.el-Kebbi IM, Ziemer DC, Gallina DL, et al. Diabetes in urban African-Americans. XV. Identification of barriers to provider adherence to management protocols. Diabetes Care. 1999 Oct;22(10):1617–20. doi: 10.2337/diacare.22.10.1617. [DOI] [PubMed] [Google Scholar]
- 35.Fox S. Health topics. Washington, DC: Pew Research Center; 2011. Available at: www.pewInternet.org/reports/2011/healthtopics. [Google Scholar]
- 36.Office of Disease Prevention and Health Promotion. Expanding the reach and impact of consumer e-Health tools. Washington, DC: U.S. Department of Health and Human Services; 2006. Available at http://www.health.gov/communication/ehealth/ehealthtools/summary.htm. [Google Scholar]
- 37.Cimino JJ, Li J, Mendonca EA, et al. An evaluation of patient access to their electronic medical records via the World Wide Web. Proc AMIA Symp. 2000:151–5. [PMC free article] [PubMed]
- 38.Vinicor F, Cohen SJ, Mazzuca SA, et al. DIABEDS: a randomized trial of the effects of physician and/or patient education on diabetes patient outcomes. J Chronic Dis. 1987;40(4):345–56. doi: 10.1016/0021-9681(87)90050-6. [DOI] [PubMed] [Google Scholar]
- 39.Brown SA. Effects of educational interventions in diabetes care: a meta-analysis of findings. Nurs Res. 1988 Jul-Aug;37(4):223–30. [PubMed] [Google Scholar]