Abstract
Purpose
People frequently present to voice clinics with complaints of irritating laryngeal sensations. Clinicians attempt to reduce the irritating sensations and their common sequela, coughing and throat clearing, by advocating for techniques that remove the irritation with less harm to the vocal fold tissue. Despite the prevalence of patients with these complaints, it is not known if the less harmful techniques recommended by clinicians are effective at clearing irritating laryngeal sensations or that irritating laryngeal sensations are, in fact, more frequent in people with voice disorders than people without voice disorders.
Method
Assessments of participant reported laryngeal sensation, pre- and post- clearing task, were obtained from 22 people with and 24 people without a voice disorder. Six clearing tasks were used to preliminarily evaluate the differing effects of tasks believed to be deleterious and ameliorative.
Results
People with and without voice disorders reported pre-clear laryngeal sensation at a similar rate. Post-clear sensation was less likely to be completely or partially removed in people with voice disorders than in the non-voice disordered group. Hard throat clear and swallow with water were the most effective techniques at removing laryngeal sensation.
Conclusions
The findings provide initial evidence for some of the clinical practices common to treating patients with voice disorders and chronic clearing such as advocating for swallowing a sip of water as a replacement behavior instead of coughing or throat clearing. However, the findings raise questions about other practices such as associating irritating laryngeal sensation with a voice disorder.
Keywords: voice, larynx, sensation, throat clear, cough
INTRODUCTION
People with voice disorders frequently present to speech-language pathology and otolaryngology clinics with complaints of irritating laryngeal sensations. These sensations range from burning or pain to an irritating tickle. In response to these patient complaints, SLPs and ENTs discuss the type of sensation, location of sensation, and possible causes of the sensation with the patient. One reason that we spend time discussing laryngeal sensation is to ascertain the cause of the sensation and the underlying cause of the larger laryngeal pathology. For example, a burning sensation in the throat is often associated with laryngeal-pharyngeal reflux while soreness in the throat may be associated with muscle tension dysphonia. Another reason that we spend time discussing the sensations, and the focus of this study, is that very often the sensations are the stated cause of patients chronically clearing their throat and coughing1.
Patients who habitually clear their throat report doing so because of a sensation of something in their throat that they must dislodge prior to speaking1. There are approximately 4,800,000 people with voice disorders who use habitual clearing behaviors making laryngeal sensations and associated clearing widespread problems among people with voice disorders1–4. These clearing behaviors are believed to cause vocal fold swelling or more serious vocal fold pathologies and are considered one of the most prevalent forms of vocal abuse4. Given that the clearing behaviors are believed to be harmful to vocal fold mucosa, SLPs and ENTs attempt to reduce the irritating laryngeal sensations and reduce the clearing behaviors that are believed to be harmful to vocal fold tissue5. Despite the significant portion of practice spent on these issues, there is little scientific evidence to suggest appropriate methods of evaluating and treating irritating laryngeal sensations or habitual clearing.
Discussion of the role of irritating laryngeal sensations and the reduction of their associated clearing and coughing behaviors is important because sixty-eight percent of people with hyperfunctional voice disorders use abusive clearing behaviors4. Although it is difficult to distinguish the precise role the clearing behaviors have, a combination of these three candidates are likely: a causal role, a reactive role, and a maintaining role, as the result of a lesion. Clinical assumptions regarding the causal role of clearing behaviors in specific voice disorders have abounded4,6,7. The following causal model is the basis for current therapeutic techniques: Throat clearing and coughing cause or contribute to specific voice disorders for two main reasons. The first reason is the mechanical force with which the laryngeal anatomy, primarily the vocal folds and arytenoid cartilages, contact8,9. The second reason is the amplitude and high velocity of the vocal fold mucosa during the behaviors that cause mechanical stress and shear. Large amplitudes of vibration and high velocity of the vocal fold mucosa, as well as vigorous contact of the vocal folds, is reported to cause vocal fold nodules, polyps, and cysts7. Laryngeal pathology that influences laryngeal sensation could cause a reactive cough. Coughing may have a role in maintaining a voice disorder or impeding treatment of a voice disorder. The effect of coughing and throat clearing on the vocal fold mucosa diminishes the impact of behavioral voice therapy and surgical interventions. Thus, reducing coughing and clearing should reduce the severity of the related vocal pathology, decrease the reoccurrence of the pathology and therefore improve voice quality6.
The prevalence of voice disorders associated with the presumably deleterious clearing behaviors accentuates the need to reduce the reportedly harmful clearing behaviors10. Beyond advising the patient not to clear their throat or cough non-productively, clinicians offer alternative, presumable ameliorative, behaviors to replace the throat clearing and coughing2,5. Reducing the frequency of coughing and throat clearing by substituting these behaviors with less harmful behaviors presumably breaks the habitual loop created by coughing and throat clearing. The concept is that coughing and throat clearing are believed to create a loop by irritating the laryngeal mucosa and activating mucus production which leads the person to feel the need to cough or clear again. Thus, when coughing and clearing are replaced by behaviors that are less irritating the loop is broken and the replacement behavior will be needed less and less often.
The main alternative behaviors commonly offered to patients are soft throat clearing, silent coughing, swallowing hard, and swallowing hard with a fluid bolus5–7. Soft throat clear is a variation on the typical throat clear accomplished at a lower intensity level. The decreased intensity of the soft throat clear is thought to require less subglottal pressure than the hard throat clear, which would reduce the mechanical force exerted on the vocal folds and decrease the number of cycles the vocal folds would come into contact. The silent cough, unlike the soft throat clear is not associated with vocal fold contact. To perform the silent cough the patient is asked to inhale and then to forcibly exhale, resulting in an exaggerated /h/ sound. The forceful exhale of the silent cough is thought to be sufficient to move the irritating mucus. The hard swallow is an attempt to mediate the sensation through the removal of mucus if present without the forceful tissue contact associated with coughing and hard throat clearing. The hard swallow is believed to relieve sensation via the swallowing of the offending mucus and the contact of the laryngeal tissues during the swallow. The hard swallow is similar to the effortful swallow used in dysphagia therapy. The hard swallow with a fluid bolus adds upon the hard swallow by including a thin liquid bolus, typically water, in an attempt to utilize the fluid to carry the mucus posteriorly and provide a wash of some tissue to reduce sensation. These four techniques have been utilized in clinical practice with anecdotally reported success despite the lack of published efficacy for these alternative tasks.
For these alternative behaviors to be viable replacements for the habituated clearing behaviors they must be equally effective in reducing irritating laryngeal sensation. While comparisons between the harmful behaviors of coughing and throat clearing1,4 and the less harmful behaviors which are advocated by clinicians as substitutes have not been conducted, there is literature to support the general use of these techniques. This approach was used as part of a treatment program in a study evaluating the efficacy of speech pathology management of chronic cough11. Vertigan found that patients in the treatment group had a significant reduction in cough in comparison to a control group who received healthy living education11. The treatment program was also found to significantly improve vocal quality12. Knowing this, it is important to understand the efficacy of the individual components of the treatment program such as identifying the optimal alternative clearing behavior.
PURPOSE
This study sought to evaluate the efficacy of reducing laryngeal sensation by hard coughing, hard throat clearing, silent coughing, soft throat clearing, dry swallowing, and swallowing a fluid bolus of water in people with and without voice disorders. The specific research questions were:
Are the ameliorative clearing tasks (silent cough, soft throat clear, dry swallow, or swallow with a fluid bolus of water) advocated for in therapy, as effective as the deleterious, habitual clearing tasks (hard cough, hard throat clear) in reducing or removing laryngeal sensation?
Are people with voice disorders less likely to experience reduction or removal of laryngeal sensation from clearing than people without voice disorders?
METHOD
Participants
Forty-six people, 22 with and 24 without voice disorders, participated in this study. There were fifteen females without voice disorders, nine males without voice disorders, thirteen females with voice disorders, and nine males with voice disorders who participated. The average age for the participants were: 40.5, 37.9, 40.3, and 40.7 for vocally-normal females, vocally-normal males, females with a voice disorders, and males with a voice disorder, respectively. The age ranges were: 27–59, 30–59, 24–60, and 27–59 for vocally-normal females, vocally-normal males, females with a voice disorder, and males with a voice disorder, respectively. People were categorized as being with or without a voice disorder based on voice quality of life survey14, perceptual judgment of voice quality, participant interview, self-categorization and endoscopy with stroboscopy completed by an SLP who specializes in voice disorders. The diagnoses of people with voice disorders are characterized in Table 1. Those who did not fall into a voice disorder category described in Table 1 were considered vocally normal. Participation in the study was accepted through an informed consent form. The data for this study was recorded at Charlotte Eye, Ear, Nose and Throat Associates specialized voice center in Charlotte, NC. The speech-language pathologists involved with data collection were specifically trained in voice. The data collection, storage, and use were in accordance with human subjects regulations.
Table 1.
Type of voice disorder and number of participants with each disorder for all persons included in this study.
| Patient ID | Type of Disorder | V-RQOL Score |
|---|---|---|
| 1 | Right polyp, Left reactive nodule, Left bowing | 16 |
| 2 | Muscle tension dysphonia, Left bowing | 24 |
| 3 | Left polyp, Right reactive nodule, Bilateral generalized edema | 29 |
| 4 | Left recurrent paralysis, Bilateral generalized edema | 25 |
| 5 | Bilateral muscle tension dysphonia, erythema, and edema | 13 |
| 6 | Nodules, Erythema, Prominent Vascularization | 24 |
| 7 | Left bowing, Laryngopharyngeal Reflux | 15 |
| 8 | Glottal insufficiency, Left bowing | 15 |
| 9 | Bilateral diffuse edema and varices, Anterior glottal gap | 36 |
| 10 | Bilateral edema medially | 30 |
| 11 | Bilateral polypoid degeneration | 23 |
| 12 | Right bowing, Mild tremor, Intermittent medial glottal gap | 28 |
| 13 | Left pseudosulcus, Mild glottal Insufficiency | 14 |
| 14 | Bilateral edema, erythema, and muscle tension dysphonia, Pseudosulcus | 10* |
| 15 | Right cyst, Left reactive nodule, bilateral prominent vascularization, anterior glottal gap | 19 |
| 16 | Mild bilateral edema and erythema | 15 |
| 17 | Left hemorrhage, Cyst with a polyp underneath, Bilateral glottal gap | 12 |
| 18 | Post-op nodule removal, Bilateral irregular leading edges, Glottal gap, Adynamic segments | 23 |
| 19 | Post-op right polyp removal, Anterior erythema | 18 |
| 20 | Bilateral polypoid lesions | 45 |
| 21 | Pedunculated ventricular cyst extending to impede vocal fold contact | 12 |
| 22 | Bilateral bowing, Anterior gap, Muscle tension dysphonia | 11 |
Instrumentation and Procedures
Participants underwent a series of twelve clearing behavior trials with each behavior assessed twice. The clearing behaviors were elicited in a standardized order with the first behavior balanced across groups (people with and without voice disorders). The order was: soft throat clear, hard throat clear, silent cough, hard cough, swallow, and swallow with a fluid bolus of water. This standardized order was chosen to prevent differences in participant response due to an order effect. That is, this method allows for the evaluation of all participants having undergone the same clearing task prior to the one elicited so that there is not a differing response across participants due to the prior task. The same clinician provided verbal instructions and an example of each task for all of the participants. For example, instructions for the swallow with a fluid bolus of water were “take a sip of water from a water bottle”. The amount of water was not standardized across participants. If the participant did not produce the instructed task, that trial was discarded and the task was elicited again until the participant produced the correct task.
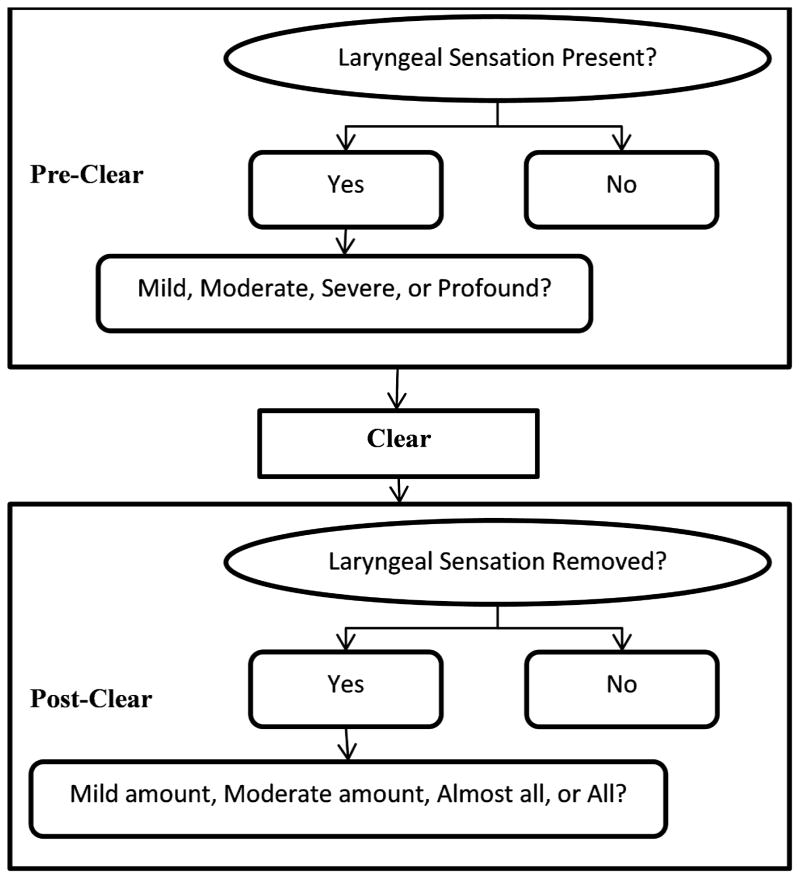
Immediately prior to each clearing behavior the participant was asked to judge the level of their irritating laryngeal sensation on the two-level scale of “Yes, I feel as though I have an irritating laryngeal sensation” or “No, I don’t feel as though I have an irritating laryngeal sensation”. If the participant reported the presence of an irritating laryngeal sensation, they were asked to quantify the sensation as being: mild sensation, moderate sensation, severe sensation or profound sensation. After each clearing behavior trial, the participants were asked to report how much of the sensation was changed by the clearing behavior on a 2-point scale of “No change in laryngeal sensation” or “The clearing behavior changed my laryngeal sensation”. If there was at least some resolution of sensation reported, the participants were asked to judge the magnitude of sensation relieved as: mild, moderate, almost all, or all. This protocol is characterized in Figure 1.
Figure 1.
Schematic of the method for data capture.
Analysis
Statistically significant differences in the report of pre- and post-clearing laryngeal sensations between people with and without voice disorders were calculated using generalized linear mixed models (GLMMs), which account for with-subject correlation among repeated measurements15, and Pearson’s, Mantel-Haenszel (M-H), or Fisher’s chi-square tests (as appropriate) for subjects’ non-repeated measurements. GLMM analyses involving change in sensation also accounted for the specific task used (e.g. hard cough, hard throat clear, etc.). Statistical analyses were performed using SAS v9.2 (Cary, NC), and p-values < 0.05 were considered statistically significant. Comparisons between subjects with and without voice disorders involved 1-sided hypothesis testing, while comparisons across the various tasks all involved 2-sided hypothesis testing.
RESULTS
Pre-clear laryngeal sensation presence
Of all participants on all clears, 281/598 (47%) reported no laryngeal sensation while 317/598 (53%) reported laryngeal sensation. On all clears, people with voice disorders and vocally-normal participants reported a similar rate of laryngeal sensation (T[36df] = 0.72, p=0.24) according to the results of the generalized linear mixed model (GLMM) (Table 2). When the same comparison was completed for first clears only, the rates of pre-clear laryngeal sensations were also similar for people with voice disorders and vocally-normal participants (Fisher exact test, p=0.55).
Table 2.
Reports of pre-clear sensation presence for all clears and first clears from persons with and without voice disorders.
| Yes – Laryngeal Sensation Present | No – Laryngeal Sensation Absent | % | Statistical Significance* | ||
|---|---|---|---|---|---|
| All Clears | Patients (n=22) | 162 | 124 | 57% | p=0.24 |
| Controls (n=24) | 155 | 157 | 50% | ||
| First Clears | Patients (n=22) | 15 | 7 | 68% | P=0.55 |
| Controls (n=24) | 17 | 7 | 71% |
Note. In All Clears, statistical significance was tested with a generalized linear mixed model. In First Clears, statistical significance was tested with a Fisher’s Exact test.
Pre-clear laryngeal sensation severity
On all clears, after accounting for within-subject correlation, no significant differences in pre-clear laryngeal sensation severity were noted between people with or without voice disorders (T[37df] = 0.74, p=0.23) (Table 3). On first clears, people with and without voice disorders also did not have statistically significant between group differences (Fisher’s exact test, p=0.87).
Table 3.
Reports of pre-clear sensation severity for all clears and first clears from persons with and without voice disorders.
| None | Mild | Moderate | Severe | Statistical Significance* | ||
|---|---|---|---|---|---|---|
| All Clears | Patients | 43% | 48% | 8% | 1% | p=0.74 |
| Controls | 50% | 45% | 4% | 1% | ||
| First Clears | Patients | 36% | 27% | 27% | 9% | P=0.87 |
| Controls | 29% | 42% | 25% | 4% |
Note. In All Clears, statistical significance was tested with a generalized linear mixed model. In First Clears, statistical significance was tested with a Fisher’s Exact test.
Post-clear change in laryngeal sensation
On all clears among subjects reporting some pre-clear sensation, the GLMM that accounted for within-subject correlation indicated that subjects without voice disorders exhibited a greater attenuation in their sensation than did subjects with voice disorders (T(32 DF) = 2.39, p = 0.011) (Table 4). On first clears, sensation attenuation was significantly greater among people without voice disorders than people with voice disorders (Fisher’s exact test, p=0.05).
Table 4.
Reports of post-clear sensation removal for all clears and first clears from persons with and without voice disorders who reported pre-clear sensation.
| No Change | Mild Change | Moderate Change | Almost Complete Removal | Complete Removal | Statistical Significance* | ||
|---|---|---|---|---|---|---|---|
| All Clears | Patients | 40% | 17% | 14% | 13% | 16% | p=0.011 |
| Controls | 30% | 17% | 10% | 14% | 30% | ||
| First Clears | Patients | 40% | 20% | 27% | 0% | 13% | P=0.05 |
| Controls | 6% | 6% | 35% | 12% | 41% |
Notes. In All Clears, statistical significance was tested with a generalized linear mixed model. In First Clears, statistical significance was tested with a Fisher’s Exact test.
Post-clear elimination of laryngeal sensation
On all clears, people without voice disorders reported that the clear completely removed the sensation in 47/155 (30%) trials, while people with voice disorders reported that the clear completely removed the sensation in 26 out of 162 (16%) trials, a difference that remained significant in the GLMMs that accounted for repeated measures within subjects and task classification (T[32df] = 2.31, p=0.01). On first clears, 7 out of 17 (41%) people without voice disorders reported that the clear completely removed the sensation; while 2 out of 15 (13%) people with voice disorders reported that the clear completely removed the sensation (Fisher Exact Test p=0.07).
Post-clear task-specific change
Overall in people who reported pre-clear laryngeal sensation, no change was reported more frequently after hard cough (44%) and silent cough (53%) than after other clearing techniques. Complete sensation removal was more commonly reported after “hard throat clear” (40%) and “swallow with water” (41%) than after other clearing techniques (“hard cough”=17%, “silent cough”=9%, “soft throat clear”=14%, “swallow”=17%), with the GLMM analysis indicating significant differences in complete sensation removal across the various tasks (F[5,300] = 5.0, p<0.001) (Table 5).
Table 5.
Post-clear sensation removal for all clears by type of clear from persons with and without voice disorders who reported pre-clear sensation.
| Clearing Task | Patients | Controls | ||||
|---|---|---|---|---|---|---|
| Removed | Reduced | No Change | Removed | Reduced | No Change | |
| Hard Cough | 8% | 40% | 52% | 24% | 38% | 38% |
| Hard Throat Clear | 25% | 42% | 33% | 54% | 36% | 11% |
| Silent Cough | 7% | 47% | 47% | 12% | 28% | 60% |
| Soft Throat Clear | 9% | 45% | 45% | 18% | 50% | 32% |
| Swallow | 3% | 52% | 45% | 33% | 42% | 25% |
| Swallow with Water | 45% | 38% | 17% | 35% | 45% | 20% |
Task-specific differences were identified for people with and without voice disorders People with voice disorders were less likely than people without voice disorders to report any sensation removal after a hard throat clear (70% vs. 60%, T[34df]=1.65, p=0.054). Swallowing with a fluid bolus of water was the clearing technique that had the highest number of positive reports (81%) of some or all sensation removal for people with voice disorders. The hard throat clear was the technique that had the highest number of positive reports (90%) of some or all sensation removal for people without voice disorders. People with and without voice disorders reported nearly the same level of effectiveness for silent coughs, hard coughs, and swallowing with a fluid bolus of water. Table 6 displays the clearing techniques in order of most effective to least effective at removing some laryngeal sensation (columns 2 & 3) and removing all laryngeal sensation (columns 4 & 5) for people with and without voice disorders.
Table 6.
Hierarchy of clearing techniques by sensation removal and reducti on for persons with and without voice disorders. This table displays the clearing techniques in order of most helpful to remove at least some laryngeal sensation (columns 2 & 3) and most helpful to remove all laryngeal sensation (columns 4 & 5) for persons with and without voice disorders. Across all participants hard throat clear and swallow with a fluid bolus were statistically significantly better than the other techniques for removing or reducing the irritating laryngeal sensation.
| Removes at least Some Sensation in Patients | Removes at least Some Sensation in Controls | Removes All Sensation in Patients | Removes All Sensation in Controls | |
|---|---|---|---|---|
| Most Effective | Swallow with a Fluid Bolus | Hard Throat Clear | Swallow with a Fluid Bolus | Hard Throat Clear |
| Hard Throat Clear | Swallow with Fluid Bolus | Hard Throat Clear | Swallow with Fluid Bolus | |
| Swallow | Swallow | Soft Throat Clear | Swallow | |
| Soft Throat Clear | Soft Throat Clear | Hard Cough | Hard Cough | |
| Silent Cough | Hard Cough | Silent Cough | Soft Throat Clear | |
| Least Effective | Hard Cough | Silent Cough | Swallow | Silent Cough |
DISCUSSION
The type of clearing behavior that produced the most positive responses was different between people with and without voice disorders. People with voice disorders responded best to swallowing with a fluid bolus of water which may indicate that washing the tissue around the larynx with water is helpful or that the clearing behaviors that involved vocal fold movement and contact were somewhat irritating themselves. People without voice disorders preferred the hard throat clear to relieve laryngeal sensations. This difference in the preferred clearing alternative may be further evidence of people with voice disorders having a different underlying reason for their irritating laryngeal sensation than people without voice disorders. Interestingly, coughing, the clearing behavior believed to be most effective at clearing laryngeal sensations, was not the behavior that people with or without voice disorders judged to be most effective in clearing the irritating laryngeal sensation.
While anecdotal reports from clinicians who work with patients with voice disorders suggest that laryngeal sensation and the associated habitual clearing behaviors are common patient complaints, the data for this study suggest that the presence of laryngeal sensation may not be unique to people with voice disorders. Our finding that approximately 50% of people with and without voice disorders reported experiencing irritating laryngeal sensation suggests that patient report of laryngeal sensation is not a useful measure for assessing laryngeal sensation issues specific to people with voice disorders. A better understanding of the specific laryngeal sensations and ways to measure these sensations in people with voice disorders is needed to advance our treatment of these patients and reach our treatment goals of reducing the irritating laryngeal sensations and consequentially the coughing and throat clearing. People with voice disorders were less likely than people without voice disorders to note a positive change in sensation level post-clearing. This suggests that people with voice disorders are not achieving removal of the negative sensation from using the clearing behaviors. This finding implies that while a similar amount of people with and without voice disorders have irritating laryngeal sensations, the sensations may be from differing causes. One possible cause of the difference is that for some people with voice disorders the trigger of chronic coughing could be the result of a sensory neuropathic disorder16. Another possible cause may be that the laryngeal sensation is caused by a vocal fold mass2. An alternative rationale for the difference in sensation removal in people with voice disorders is that their laryngeal mucus is different than in people without voice disorders and thus harder to dispel. Research that supports this reasoning comes from a recent finding that although the incidence of mucus aggregation in people with (100%) and without voice disorders (97%) is similar, dysphonic speakers have more severely thick mucus and significantly more mucus pooling than normophonic speakers17,18.
Limitations
There are five main limitations of this study. First, the study asked the participants to perform and judge unfamiliar and somewhat odd tasks. This is true especially of the vocally-normal participants who are novices at silent coughs and judging laryngeal sensation. Second, this study had a relatively small sample size which precludes generalizations about the population at large. Third, this was a subjective study of laryngeal sensation. The current study relied on participants’ judgments as used in clinical practice. A further study of this mechanism is underway that includes quantification of laryngeal sensation. Fourth, clearing behaviors are generally believed to relieve irritating laryngeal sensation; however there is the possibility of the behaviors to cause such sensations. This study did not account for the clearing behaviors causing laryngeal sensation. Lastly, while vocally-normal participants were screened for voice disorder, the main criterion for inclusion in the study was self-associating with either a voice disordered or non-voice disordered group. In the absence of visible laryngeal pathology and a perceptible auditory voice disorder, people who self-identified as vocally-normal were considered vocally-normal in this study. Future studies should consider a thorough medical work-up of people self-identifying as vocally-normal.
CONCLUSIONS
The findings from this study provide evidence for the clinical practices and phenomenon common to treating patients with voice disorders and chronic clearing. One such practice substantiated by this study is advocating the use of swallowing with a fluid bolus of water as a behavioral substitute for non-productive, potentially mucosa-harming throat clearing and coughing. A clinical phenomenon confirmed by this study was the persistence of irritating laryngeal sensation in people with voice disorders after any type of clearing. The results of this study lay the foundation for further research into the cause of irritating laryngeal sensations in people with voice disorders and the best method for quelling those sensations. Future studies should investigate whether there are differences dependent on the type of voice disorder in the reporting of laryngeal sensation and efficacy of the clearing behaviors.
The clinically-based hypothesis of a difference in laryngeal sensation between people with and without voice disorders was not substantiated by the findings of this study. Approximately half of people with and without voice disorders reported mildly irritating laryngeal sensation pre-clear. Furthermore, clearing did eliminate the laryngeal sensation more often in people without voice disorders than people with voice disorders. The best two clearing techniques to eliminate at least some of the laryngeal sensation were hard throat clear and swallow with water; however, there were differences for people with and without voice disorders. People with voice disorders reported the most benefit from swallowing with a fluid bolus of water, while people without voice disorders reported the most benefit from a hard throat clear.
Acknowledgments
This project was supported by an R03 grant (R03 DC00843) funded by the National Center for Deafness and Other Communication Disorders at the National Institutes of Health. This publication was supported by the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, NIH/NCRR Grant number UL1 RR029880. The authors express their appreciation to Dr. Dimitar Deliyski whose encouragement supported this project.
Footnotes
Portions of this study have been presented at the 39th Symposium of the Voice Foundation, Philadelphia, PA, June 2010 and the Convention of the American Speech-Language-Hearing Association, Philadelphia, PA, November 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Colton RH, Casper JK. Understanding voice problems: a physiological perspective for diagnosis and treatment. Baltimore, MD: Williams and Wilkins Press; 1996. [Google Scholar]
- 2.Boone DR, McFarlane SC, Von Berg SL. The Voice and Voice Therapy 7th Edition. Boston, Massachusetts: Pearson Education Inc; 2005. [Google Scholar]
- 3.Brodnitz F. Vocal Rehabilitation. Rochester, MN: American Academy of Ophthalmology and Otolaryngology; 1971. [Google Scholar]
- 4.Stemple JC, Glaze LE, Klaben BG. Clinical Voice Pathology: Theory and Management. 3. San Diego, California: Singular; 2000. [Google Scholar]
- 5.Zwitman DH, Calcaterra TC. The “silent cough” method for vocal hyperfunction. J Speech Hear Disord. 1973;38:119–125. doi: 10.1044/jshd.3801.119. [DOI] [PubMed] [Google Scholar]
- 6.Stemple JC. Voice Therapy: Clinical Studies. Clifton Park, New Jersey: Delmar Learning; 2000. [Google Scholar]
- 7.Titze IR. Principles of Voice Production. Englewood Cliffs, New Jersey: Prentice-Hall Inc; 1994. [Google Scholar]
- 8.Hess MM, Verdolini K, Bierhals W, Mansmann U, Gross M. Endolaryngeal contact pressures. J Voice. 1998;12 (1):50–67. doi: 10.1016/s0892-1997(98)80075-1. [DOI] [PubMed] [Google Scholar]
- 9.Jiang JJ, Shah AG, Hess MM, Verdolini K, Banzali FM, Hanson DG. Vocal fold impact stress analysis. J Voice. 2001;15 (1):4–14. doi: 10.1016/S0892-1997(01)00002-9. [DOI] [PubMed] [Google Scholar]
- 10.Vertigan AE, Theodoros DG, Gibson PG, Winkworth AL. Voice and upper airway symptoms in people with chronic cough and paradoxical vocal fold movement. J Voice. 2007;21 (3):361–383. doi: 10.1016/j.jvoice.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Vertigan AE, Theodoros DG, Gibson PG, Winkworth AL. Efficacy of speech pathology management for chronic cough: a randomised placebo controlled trial of treatment efficacy. Thorax. 2006;61:1065–1068. doi: 10.1136/thx.2006.064337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vertigan AE, Theodoros DG, Winkworth AL, Gibson PG. A comparison of two approaches to the treatment of chronic cough: perceptual, acoustic, and electroglottographic outcomes. J Voice. 2008;22 (5):581–589. doi: 10.1016/j.jvoice.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Behrman A. Abstract: Efficacy of voice therapy for vocal fold nodules. NIH CRISP database. 2003 Feb 7; < http://crisp.cit.nih.gov/>.
- 14.Hogikyan ND, Sethuraman G. Validation of an instrument to measure voice-related quality of life (V-RQOL) J Voice. 1999;13(4):557–69. doi: 10.1016/s0892-1997(99)80010-1. [DOI] [PubMed] [Google Scholar]
- 15.McCulloch CE, Searle SR. Generalized, Linear, and Mixed Models. New York: John Wiley & Sons, Inc; 2001. [Google Scholar]
- 16.Vertigan AE, Gibson PG. Chronic refractory cough as a sensory neuropathy: evidence from a reinterpretation of cough triggers. J Voice. 2010;25 (5):596–601. doi: 10.1016/j.jvoice.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Bonilha H, Aikman A, Hines K, Deliyski D. Vocal fold mucus aggregation in vocally normal speakers. Logopedics Phoniatrics Vocology. 2008;33:136–142. doi: 10.1080/14015430701875588. [DOI] [PubMed] [Google Scholar]
- 18.Bonilha HS, White L, Kuckhahn K, Deliyski D. Mucus aggregation in persons with voice disorders. Journal of Communication Disorders. doi: 10.1016/j.jcomdis.2012.03.001. in revision. [DOI] [PMC free article] [PubMed] [Google Scholar]