Abstract
Few recent estimates of childhood asthma incidence exist in the literature, although the importance of incidence surveillance for understanding asthma risk factors has been recognized. Asthma prevalence, morbidity, and mortality reports have repeatedly shown that low-income children are disproportionately impacted by the disease. The aim of this study was to demonstrate the utility of Medicaid claims data for providing statewide estimates of asthma incidence. Medicaid analytic extract (MAX) data for Texas children aged 0–17 years enrolled in Medicaid between 2004 and 2007 were used to estimate incidence overall and by age group, gender, race, and county of residence. A ≥13-month period of continuous enrollment was required in order to distinguish incident from prevalent cases identified in the claims data. The age-adjusted incidence of asthma was 4.26/100 person-years during 2005–2007, higher than reported in other populations. Incidence rates decreased with age, were higher for males than females, differed by race, and tended to be higher in rural than urban areas. This study demonstrates the utility of Medicaid analytic extract data for estimating asthma incidence and describes the methodology required for a population with unstable enrollment.
Keywords: asthma, child, incidence, Medicaid
Nearly 10% of children in the United States had asthma in 2009 (1). Asthma is a leading cause of illness and hospitalizations among children, with significant impacts on health and quality of life. Direct and indirect costs of asthma are substantial, from increased medical care to missed school days (1, 2). Low-income children are disproportionately impacted, accounting for 37% of the US population but 58% of prevalent asthma cases (3). Medicaid-enrolled children have higher risk of asthma-related morbidity, complications, and hospitalization than do privately insured children (4–6).
Although asthma prevalence and morbidity are well described, estimates of childhood asthma incidence are rare. Rudd and Moorman (7) estimated annual asthma incidence in US children ranging from 5.7/1,000 in 1980 to 10.1/1,000 in 1995. A recent Canadian study reported incidence in 2004–2005 ranging from 31.3/1,000 person-years for children under 5 to 5.6/1,000 person-years in children aged 10–14 years (8). Others have reported incidence rates in children ranging from 8.4/1,000 person-years to 24.6/1,000 person-years (9, 10).
Medicaid provides health and long-term-care coverage to nearly 60 million low-income and disabled Americans, including 30% of US children, and is funded jointly by state and federal governments (11). Broad federal guidelines mandate that states cover certain benefits like hospital and physician services, but other benefits are optional, including prescription drug coverage. States set eligibility criteria and cost-sharing requirements, within federal standards (12).
Medicaid claims data have been used to describe asthma prevalence, morbidity, and health-care utilization patterns (13–22). Although 2 studies estimated asthma incidence using claims data (8, 23), we found none that used Medicaid data to estimate national- or state-level incidence. Thus, we conducted this investigation to demonstrate the utility of Medicaid claims data for estimating asthma incidence among Texas children enrolled in Medicaid, a population of over 2.5 million (24).
MATERIALS AND METHODS
We used Medicaid analytic extract (MAX) files produced by the Centers for Medicare and Medicaid Services specifically for research. MAX files contain annual, person-level data on Medicaid eligibility and health-care utilization reported by the states. The files contain final adjudicated claims by date of service and have undergone quality checks and corrections (25, 26). We obtained enrollment (“personal summary”), inpatient and outpatient medical claims, and pharmacy claims files from the Centers for Medicare and Medicaid Services for Texas beneficiaries aged 0–17 years enrolled in Medicaid for any length of time between 2004 and 2007. Claims submitted only to reflect capitated payments were not included in the Centers for Medicare and Medicaid Services files.
Identification of study population
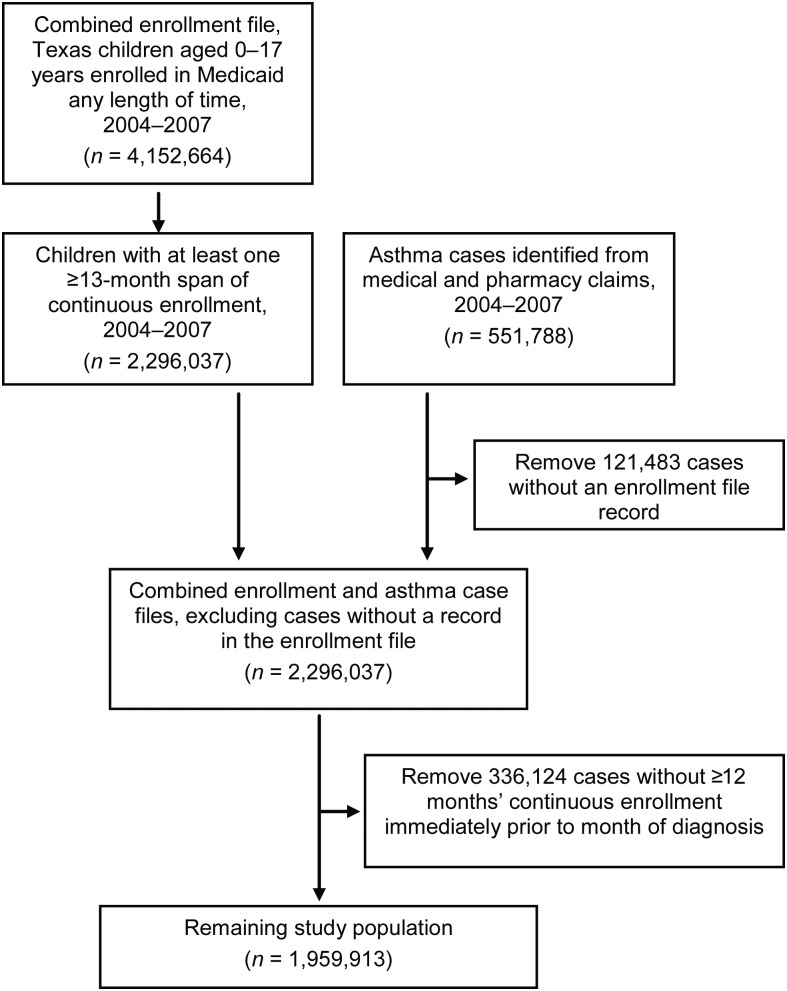
The personal summary files contained indicators that were used to determine which months each child was enrolled and eligible for the full scope of Medicaid benefits, until his/her 18th birthday. Even if enrolled, children were considered ineligible during any year they had private insurance coverage, as this could result in incomplete claims history. Children with only premium (i.e., capitated) payment claims during the year were also considered ineligible to eliminate follow-up time during which no medical or pharmacy claims would be found in the MAX files. Once eligible, months were determined for each child, and the 4 personal summary files were combined into a single enrollment file (Figure 1).
Figure 1.
Description of the process used to identify the study population and cases from the original MAX files containing enrollment and claims records for Texas Medicaid-enrolled children aged 0–17 years, 2004–2007. The numbers of children with at least one ≥13-month enrollment span, in the combined enrollment and case file and in the remaining study population, represent the number of ≥13-month enrollment spans; a child could have more than one enrollment span during the 4-year study period. MAX, Medicaid analytic extract.
The beginning and ending months for each child's period(s) of enrollment were derived from the combined, 4-year enrollment file. Children were included in the study population if they had one or more continuous ≥13-month span of enrollment between 2004 and 2007, allowing for a single 1-month enrollment gap during the 4-year period. This continuous enrollment span provided a “wash-out” period that enabled us to distinguish incident from prevalent cases.
Identification of asthma cases
We combined all medical and pharmacy claims for the 4-year period and defined cases as children with a primary diagnosis of asthma (International Classification of Diseases, Ninth Revision, code 493.xx) on one or more outpatient or inpatient records or 4 or more asthma medication (27) dispensing events (30-day supply) during a 365-day period. For a medication prescription with more than 30 days' supply, we divided days by 30 and rounded up to calculate the number of 30-day dispensing events. For each case, the earliest of either date of service for the first asthma medical claim or prescribed date of the first asthma prescription dispensed was kept as the date of diagnosis.
Analysis
Records from the enrollment and case files were joined, and cases without an enrollment record (i.e., did not have a ≥13-month span of continuous enrollment between 2004 and 2007) were excluded. We also excluded cases that were in the enrollment file but not enrolled continuously in the 12-month period prior to diagnosis, as we could not determine whether these were incident or prevalent cases. For the remaining study population, person-months were calculated beginning with the 13th month of follow-up (the first month in which a subject could become an incident case). Follow-up ended on the earliest of 1) the last month of the enrollment span, 2) the month of asthma diagnosis, or 3) December 31, 2007. Hence, person-months of follow-up ranged from 1 to 36. Personal summary and claims files from 2004 were not used in the analysis other than to provide a wash-out period for children in the 2005 files.
Asthma incidence rates were calculated for Texas overall and by age group (1–4, 5–9, 10–14, and 15–17 years), gender, race (white, black, Hispanic, Asian, American Indian), and county (n = 254) between 2005 and 2007. Rates (other than by age group) were age adjusted on the basis of the proportion in the age group in the 2000 US Census (28) and reported as cases/100 person-years. Age and county of residence reflected values at first enrollment. Incidence rates were calculated by dividing the number of incident cases in 2005–2007 by person-months of follow-up for the study population during the same period. County rates were statistically different from the Texas rate if the 95% confidence interval for the county rate did not include the statewide point estimate. Incidence rates for counties with fewer than 16 asthma cases (n = 36) were not calculated because of unstable rates.
Analyses were performed by using SAS, version 9.2, software (SAS Institute, Inc., Cary, North Carolina). A map of county-specific incidence rates was generated with ArcGIS, version 10 (Esri, Redlands, California). The study was approved by the Centers for Medicare and Medicaid Services Privacy Board and the University of Texas Health Science Center Committee for the Protection of Human Subjects.
RESULTS
The 2004–2007 MAX enrollment files included 4,152,664 Texas children aged 0–17 years. After exclusion of children without a ≥13-month continuous enrollment span between 2004 and 2007, the remaining sample included 2,164,463 children free of asthma at baseline and 2,467,757 person-years of follow-up. The study population was evenly distributed between males and females, and over half were under the age of 5 years (Table 1). Sixty-five percent were Hispanic, and approximately 16% each were white and black.
Table 1.
Age-adjusted Incidence Ratesa of Childhood Asthma Among Texas Medicaid-enrolled Children Aged 1–17 Years, 2005–2007
| Person-Years | % | No. of Asthma Casesb | % | Incidence Rate/ 100 Person-Years | 95% CI | |
|---|---|---|---|---|---|---|
| Total | 2,467,757 | 129,588 | 4.26 | 4.23, 4.30 | ||
| Age group, years | ||||||
| 1–4 | 1,304,611 | 52.9 | 85,390 | 65.9 | 6.55 | 6.50, 6.59 |
| 5–9 | 603,279 | 24.4 | 26,131 | 20.2 | 4.33 | 4.28, 4.38 |
| 10–14 | 487,355 | 19.7 | 15,949 | 12.3 | 3.27 | 3.22, 3.32 |
| 15–17 | 72,512 | 2.9 | 2,118 | 1.6 | 2.92 | 2.80, 3.05 |
| Gender | ||||||
| Female | 1,235,010 | 50.0 | 58,722 | 45.3 | 3.95 | 3.90, 3.99 |
| Male | 1,232,706 | 50.0 | 70,864 | 54.7 | 4.57 | 4.52, 4.62 |
| Race | ||||||
| White | 406,837 | 16.5 | 23,079 | 17.8 | 4.78 | 4.69, 4.86 |
| Black | 390,526 | 15.8 | 20,617 | 15.9 | 4.45 | 4.37, 4.52 |
| American Indian | 7,465 | 0.3 | 409 | 0.3 | 3.84 | 3.33, 4.36 |
| Asian | 29,990 | 1.2 | 1,407 | 1.1 | 3.54 | 3.29, 3.79 |
| Hispanic | 1,608,753 | 65.2 | 82,612 | 63.7 | 4.18 | 4.14, 4.22 |
| Unknown | 24,187 | 1.0 | 1,464 | 1.1 | ||
| Race/gender | ||||||
| White/male | 203,965 | 8.3 | 12,489 | 9.7 | 4.92 | 4.80, 5.03 |
| Black/male | 193,951 | 7.9 | 11,479 | 9.0 | 4.89 | 4.78, 5.01 |
| American Indian/male | 3,866 | 0.2 | 251 | 0.2 | 4.27 | 3.63, 4.91 |
| Asian/male | 14,741 | 0.6 | 794 | 0.6 | 3.82 | 3.47, 4.17 |
| Hispanic/male | 807,900 | 32.9 | 44,915 | 35.1 | 4.52 | 4.46, 4.57 |
| White/female | 202,865 | 8.3 | 10,590 | 8.3 | 4.62 | 4.50, 4.74 |
| Black/female | 196,573 | 8.0 | 9,137 | 7.1 | 4.00 | 3.90, 4.10 |
| American Indian/female | 3,598 | 0.1 | 158 | 0.1 | 3.42 | 2.58, 4.26 |
| Asian/female | 14,882 | 0.6 | 613 | 0.5 | 3.25 | 2.90, 3.61 |
| Hispanic/female | 814,428 | 33.2 | 37,697 | 29.4 | 3.84 | 3.79, 3.89 |
Abbreviation: CI, confidence interval.
a Per 100 person-years. Age-adjusted to the proportion of the 2000 US Census population in each age category, with the exception of rates presented by age group.
b Cells with 10 or fewer cases are not displayed per Centers for Medicare and Medicaid Services stipulation.
We identified 129,588 incident asthma cases between 2005 and 2007 (Table 1). Most cases (75%) were identified from an outpatient record, and 91% of these also had at least one subsequent asthma medication claim. Fewer than 1% were identified through inpatient records. The remaining 25% received their diagnosis on the date they filled the first of 4 prescriptions, and of these, over 40% had a subsequent outpatient record. Overall age-adjusted asthma incidence in this population was 4.26 cases (95% confidence interval (CI): 4.23, 4.30) per 100 person-years. Incidence was higher in males than females and decreased with age. White children and black children had the highest incidence, while rates were lowest among Asians. Incidence rates for white males and black males approached 5 cases per 100 person-years.
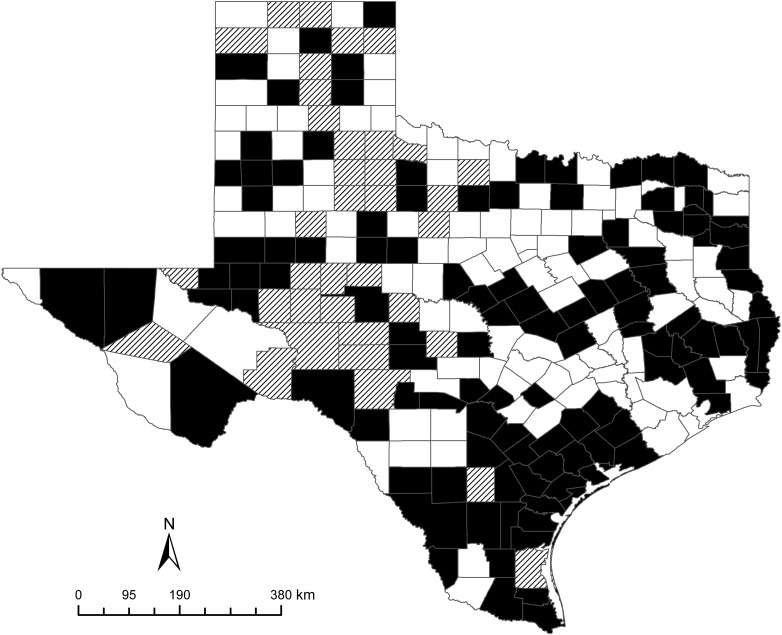
County-specific incidence rates were generally higher in southern border counties and lower in larger metropolitan areas (Figure 2). Counties including Houston, Dallas, Fort Worth, Austin, and El Paso had incidence rates significantly below the statewide rate, from 3.08 (95% CI: 2.90, 3.27) to 3.95 (95% CI: 3.84, 4.06) per 100 person-years. Of the state's largest population centers, only Bexar County, which includes San Antonio, surpassed the state average with an incidence rate of 5.19 (95% CI: 5.06, 5.32) per 100 person-years. The 36 counties with fewer than 16 cases had total population sizes from 67 to 8,854, with between 2 and 474 children enrolled in Medicaid (24, 28).
Figure 2.
County-specific asthma incidence per 100 person-years among Medicaid-enrolled children in Texas, aged 1–17 years, 2005–2007. Counties shaded in black are those with incidence above the statewide incidence rate, while those shaded in white were below the state rate. Counties with hash marks had fewer than 16 cases, and therefore incidence rates were not calculated.
DISCUSSION
Forty percent of Texas children are enrolled in Medicaid, and the cost of asthma-related treatment for these children exceeded $242 million in 2004 (29). On the basis of our analysis, Medicaid-enrolled children in Texas were newly diagnosed with asthma at a rate of 4.26/100 person-years between 2005 and 2007. Our estimates are higher than previously reported in the United States (7) and Canada (8) but not unexpected among low-income children. Incidence rates were higher for males and decreased with age, consistent with other reports (8, 9). As in the Canadian study, we found that incidence rates were higher for males than females in the youngest age groups but similar in children aged 15–17 years (males = 2.8%, females = 3.0%). The median age at diagnosis was 4.9 years, consistent with clinical experience that most children with asthma will develop symptoms by the age of 5 years (30).
A higher incidence among whites than blacks was unexpected, as most prevalence studies report the reverse. Some (31, 32) but not all (33, 34) have shown a lessened effect of race on childhood asthma prevalence after adjustment for socioeconomic status. Our results may reflect lower health-care utilization among blacks, who generally have fewer primary care visits and more emergency room visits and inpatient hospital stays than whites (5, 19, 35, 36). Although we identified few cases through inpatient claims, lower primary care visit rates could result in underestimated incidence among blacks.
The primary strengths of our study are the large sample size and 3-year timeframe that allowed estimation of stable rates by age group, gender, race/ethnicity, and county. We applied methodology previously used in cancer research (37–45) to estimate rates of newly occurring asthma, using a data source with both medical and pharmacy claims. The date of onset was determined directly from claims data and was not subject to recall bias. Requiring a ≥13-month continuous enrollment period without evidence of asthma decreased the likelihood of classifying prevalent cases as incident cases, particularly for a disease with seasonal morbidity patterns (46).
Weaknesses of the study include the lack of a “gold standard” for measuring asthma incidence, making it difficult to validate this method. Our results are not generalizable to the general population in Texas, as they represent low-income children with health insurance benefits. Incidence rate estimates across states using this methodology and data source may not be directly comparable because of differences in Medicaid eligibility, benefits, and coverage. The Medicaid population is fluid, resulting in variable lengths of follow-up and potential selection bias. Nearly 11% of children were enrolled for only 13 months, while 15% were enrolled for the entire 3-year period.
The inclusion of beneficiaries from capitated managed-care (health maintenance organization) plans and fee-for-service plans may have introduced bias into our estimates. Although claims reporting for health maintenance organization plans improved over time, data completeness and quality likely differed between the 2 types of plans (47). Most children in the 9 major metropolitan areas of Texas are required to enroll in a capitated program, whereas a fee-for-service program covers the rest of the state. It is unclear whether underreporting of health maintenance organization claims may have contributed to lower incidence rates in urban areas or to what extent statewide rates were underestimated. Lower asthma prevalence in urban areas has been reported among other Medicaid populations and may be partially attributable to higher smoking rates in rural areas (48). We should note that pharmacy claims in Texas are paid on a fee-for-service basis. Although use of both medical and pharmacy records is the method preferred by the Centers for Medicare and Medicaid Services for identifying asthma cases, relying on pharmacy records alone can also provide reliable estimates (16).
The Centers for Disease Control and Prevention has called for a greater emphasis on tracking incidence in US asthma surveillance programs, while acknowledging the inherent challenges and limited data sources (49, 50). In this unique study, we estimated population-based asthma incidence using statewide Medicaid claims data, a rich source for studying diseases disproportionately impacting low-income children. Our results indicate that Medicaid-enrolled children are at greater risk of being given an asthma diagnosis than those in the general population. Knowledge of asthma incidence patterns is critical to understanding associated risk factors, and we hope that this novel approach will be applied to other Medicaid populations to increase understanding of this disabling and costly disease.
ACKNOWLEDGMENTS
Author affiliation: Division of Epidemiology, Human Genetics, and Environmental Sciences, University of Texas School of Public Health, Houston, Texas (Judy K. Wendt, Elaine Symanski, Xianglin L. Du).
This project was supported by the National Institute for Occupational Safety and Health-funded Southwest Center for Occupational and Environmental Health Education and Research Center (grant T42OH008421).
The authors thank Gerrie Barosso, Jeanne Moorman, and Dr. Beth Benedict for their invaluable assistance with this project.
Conflict of interest: none declared.
REFERENCES
- 1.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. Natl Health Stat Report. 2011;12(32):1–14. [PubMed] [Google Scholar]
- 2.Selgrade MK, Lemanske RF, Jr, Gilmour MI, et al. Induction of asthma and the environment: what we know and need to know. Environ Health Perspect. 2006;114(4):615–619. doi: 10.1289/ehp.8376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markus AR, Lyon M, Rosenbaum S. Changing Policy: The Elements for Improving Childhood Asthma Outcomes. Washington, DC: Department of Health Policy, the George Washington University School of Public Health and Health Services; 2010. [Google Scholar]
- 4.Bai Y, Hillemeier MM, Lengerich EJ. Racial/ethnic disparities in symptom severity among children hospitalized with asthma. J Health Care Poor Underserved. 2007;18(1):54–61. doi: 10.1353/hpu.2007.0001. [DOI] [PubMed] [Google Scholar]
- 5.Ortega AN, Belanger KD, Paltiel AD, et al. Use of health services by insurance status among children with asthma. Med Care. 2001;39(10):1065–1074. doi: 10.1097/00005650-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Lozano P, Sullivan SD, Smith DH, et al. The economic burden of asthma in US children: estimates from the National Medical Expenditure Survey. J Allergy Clin Immunol. 1999;104(5):957–963. doi: 10.1016/s0091-6749(99)70075-8. [DOI] [PubMed] [Google Scholar]
- 7.Rudd RA, Moorman JE. Asthma incidence: data from the National Health Interview Survey, 1980–1996. J Asthma. 2007;44(1):65–70. doi: 10.1080/02770900601125896. [DOI] [PubMed] [Google Scholar]
- 8.Gershon AS, Guan J, Wang C, et al. Trends in asthma prevalence and incidence in Ontario, Canada, 1996–2005: a population study. Am J Epidemiol. 2010;172(6):728–736. doi: 10.1093/aje/kwq189. [DOI] [PubMed] [Google Scholar]
- 9.Simpson CR, Sheikh A. Trends in the epidemiology of asthma in England: a national study of 333,294 patients. J R Soc Med. 2010;103(3):98–106. doi: 10.1258/jrsm.2009.090348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gilliland FD, Berhane K, Islam T, et al. Obesity and the risk of newly diagnosed asthma in school-age children. Am J Epidemiol. 2003;158(5):406–415. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- 11.The Henry J. Kaiser Family Foundation. Washington, DC: The Henry J. Kaiser Family Foundation; 2010. Medicaid: a primer. (http://www.kff.org/medicaid/upload/7334-04.pdf. ). (Accessed January 12, 2012) [Google Scholar]
- 12.Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Baltimore, MD: Centers for Medicare and Medicaid Services; 2012. Medicaid information by topic. (http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/By-Topic.html. ). (Accessed January 12, 2012) [Google Scholar]
- 13.Piecoro LT, Potoski M, Talbert JC, et al. Asthma prevalence, cost, and adherence with expert guidelines on the utilization of health care services and costs in a state Medicaid population. Health Serv Res. 2001;36(2):357–371. [PMC free article] [PubMed] [Google Scholar]
- 14.Smith MJ, Rascati KL, Barner JC. A descriptive analysis of asthma-related medical services and prescription utilization among recipients in a Medicaid program. J Asthma. 2005;42(6):447–453. doi: 10.1081/JAS-67954. [DOI] [PubMed] [Google Scholar]
- 15.Buescher PA, Jones-Vessey K. Using Medicaid data to estimate state- and county-level prevalence of asthma among low-income children. Matern Child Health J. 1999;3(4):211–216. doi: 10.1023/a:1022377405914. [DOI] [PubMed] [Google Scholar]
- 16.Dombkowski KJ, Wasilevich EA, Lyon-Callo SK. Pediatric asthma surveillance using Medicaid claims. Public Health Rep. 2005;120(5):515–524. doi: 10.1177/003335490512000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pawar V, Smith MJ. Asthma-related healthcare services utilization by African-Americans enrolled in West Virginia Medicaid. Respir Med. 2006;100(9):1579–1587. doi: 10.1016/j.rmed.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Roberts EM. Racial and ethnic disparities in childhood asthma diagnosis: the role of clinical findings. J Natl Med Assoc. 2002;94(4):215–223. [PMC free article] [PubMed] [Google Scholar]
- 19.Shields AE, Comstock C, Weiss KB. Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics. 2004:496–504. doi: 10.1542/peds.113.3.496. 113(3 pt 1) [DOI] [PubMed] [Google Scholar]
- 20.Dombkowski KJ, Cabana MD, Cohn LM, et al. Geographic variation of asthma quality measures within and between health plans. Am J Manag Care. 2005;11(12):765–772. [PubMed] [Google Scholar]
- 21.Stevenson MD, Heaton PC, Moomaw CJ, et al. Inhaled corticosteroid use in asthmatic children receiving Ohio Medicaid: trend analysis, 1997–2001. Ann Allergy Asthma Immunol. 2008;100(6):538–544. doi: 10.1016/S1081-1206(10)60049-X. [DOI] [PubMed] [Google Scholar]
- 22.Wilson SE, Leonard A, Moomaw C, et al. Underuse of controller medications among children with persistent asthma in the Ohio Medicaid population: evolving differences with new medications. Ambul Pediatr. 2005;5(2):83–89. doi: 10.1367/A04-154R.1. [DOI] [PubMed] [Google Scholar]
- 23.Siwik JP, Johnson CC, Havstad SL, et al. Airway hyperresponsiveness to methacholine at age 6 to 8 years in nonasthmatic patients is not related to increased health-care utilization for asthma in the ensuing 5 years: a longitudinal study of a birth cohort. Chest. 2005;128(4):2420–2426. doi: 10.1378/chest.128.4.2420. [DOI] [PubMed] [Google Scholar]
- 24.Texas Health and Human Services Commission. Austin, TX: Texas Health and Human Services Commission; 2011. Final count—Medicaid enrollment by month. (http://www.hhsc.state.tx.us/research/MedicaidEnrollment/ME-Monthly.asp. ). (Accessed October 6, 2010) [Google Scholar]
- 25.Centers for Medicare and Medicaid Services, US Department of Health and Human Services. Baltimore, MD: Centers for Medicare and Medicaid Services; 2011. Medicaid Analytic eXtract (MAX) general information. (https://www.cms.gov/MedicaidDataSourcesGenInfo/07_MAXGeneralInformation.asp. ). (Accessed October 19, 2011) [Google Scholar]
- 26.Hennessy S, Leonard CE, Palumbo CM, et al. Quality of Medicaid and Medicare data obtained through Centers for Medicare and Medicaid Services (CMS) Med Care. 2007;45(12):1216–1220. doi: 10.1097/MLR.0b013e318148435a. [DOI] [PubMed] [Google Scholar]
- 27.National Committee for Quality Assurance. HEDIS. Washington, DC: National Committee for Quality Assurance; 2011; 2011. NDC lists: use of appropriate medications for people with asthma (ASM) (http://www.ncqa.org/tabid/1274/Default.aspx. ). (Accessed January 27, 2011) [Google Scholar]
- 28.Bureau of the Census, US Department of Commerce. Census. Washington, DC: Bureau of the Census; 2011; 2000. summary file 3. (http://factfinder.census.gov/servlet/DatasetMainPageServlet?_ds_name=DEC_2000_SF3_U&_program=DEC&_lang=en. ). (Accessed June 17, 2011) [Google Scholar]
- 29.Agency for Healthcare Research and Quality. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Asthma care quality improvement: a resource guide for state action. (http://www.ahrq.gov/qual/asthmacare/asthmatab1_4.htm. ). (Accessed October 6, 2010) [Google Scholar]
- 30.Kemp JP, Kemp JA. Management of asthma in children. Am Fam Physician. 2001;63(7):1341–1348. [PubMed] [Google Scholar]
- 31.Akinbami LJ, LaFleur BJ, Schoendorf KC. Racial and income disparities in childhood asthma in the United States. Ambul Pediatr. 2002;2(5):382–387. doi: 10.1367/1539-4409(2002)002<0382:raidic>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 32.Aligne CA, Auinger P, Byrd RS, et al. Risk factors for pediatric asthma. Contributions of poverty, race, and urban residence. Am J Respir Crit Care Med. 2000;162(3 pt 1):873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- 33.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9(2):154–160. doi: 10.1097/aci.0b013e3283292207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moorman JE, Zahran H, Truman BI, et al. Current asthma prevalence—United States, 2006–2008. Centers for Disease Control and Prevention (CDC) MMWR Surveill Summ. 2011;60(suppl 01):84–86. [PubMed] [Google Scholar]
- 35.Nash DR, Childs GE, Kelleher KJ. A cohort study of resource use by Medicaid children with asthma. Pediatrics. 1999;104(2 pt 1):310–312. doi: 10.1542/peds.104.2.310. [DOI] [PubMed] [Google Scholar]
- 36.Lozano P, Connell FA, Koepsell TD. Use of health services by African-American children with asthma on Medicaid. JAMA. 1995;274(6):469–473. [PubMed] [Google Scholar]
- 37.Gold HT, Do HT. Evaluation of three algorithms to identify incident breast cancer in Medicare claims data. Health Serv Res. 2007;42(5):2056–2069. doi: 10.1111/j.1475-6773.2007.00705.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nattinger AB, Laud PW, Bajorunaite R, et al. An algorithm for the use of Medicare claims data to identify women with incident breast cancer. Health Serv Res. 2004;39(6 pt 1):1733–1749. doi: 10.1111/j.1475-6773.2004.00315.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koroukian SM, Cooper GS, Rimm AA. Ability of Medicaid claims data to identify incident cases of breast cancer in the Ohio Medicaid population. Health Serv Res. 2003;38(3):947–960. doi: 10.1111/1475-6773.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang PS, Walker AM, Tsuang MT, et al. Finding incident breast cancer cases through US claims data and a state cancer registry. Cancer Causes Control. 2001;12(3):257–265. doi: 10.1023/a:1011204704153. [DOI] [PubMed] [Google Scholar]
- 41.Cooper GS, Yuan Z, Jethva RN, et al. Use of Medicare claims data to measure county-level variation in breast carcinoma incidence and mammography rates. Cancer Detect Prev. 2002;26(3):197–202. doi: 10.1016/s0361-090x(02)00056-9. [DOI] [PubMed] [Google Scholar]
- 42.Freeman JL, Zhang D, Freeman DH, et al. An approach to identifying incident breast cancer cases using Medicare claims data. J Clin Epidemiol. 2000;53(6):605–614. doi: 10.1016/s0895-4356(99)00173-0. [DOI] [PubMed] [Google Scholar]
- 43.Cooper GS, Yuan Z, Stange KC, et al. Use of Medicare claims data to measure county-level variations in the incidence of colorectal carcinoma. Cancer. 1998;83(4):673–678. doi: 10.1002/(sici)1097-0142(19980815)83:4<673::aid-cncr7>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 44.Cooper GS, Yuan Z, Jethva RN, et al. Determination of county-level prostate carcinoma incidence and detection rates with Medicare claims data. Cancer. 2001;92(1):102–109. doi: 10.1002/1097-0142(20010701)92:1<102::aid-cncr1297>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 45.Ramsey SD, Scoggins JF, Blough DK, et al. Sensitivity of administrative claims to identify incident cases of lung cancer: a comparison of 3 health plans. J Manag Care Pharm. 2009;15(8):659–668. doi: 10.18553/jmcp.2009.15.8.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gergen PJ, Mitchell H, Lynn H. Understanding the seasonal pattern of childhood asthma: results from the National Cooperative Inner-City Asthma Study (NCICAS) J Pediatr. 2002;141(5):631–636. doi: 10.1067/mpd.2002.127510. [DOI] [PubMed] [Google Scholar]
- 47.Texas External Quality Review Organization. Validating Encounter Data: Texas Medicaid Managed Care and Children's Health Insurance Program Managed Care Organization Medical Record Review, Fiscal Year 2006. Gainesville, FL: Texas External Quality Review Organization; 2008; [Google Scholar]
- 48.Valet RS, Gebretsadik T, Carroll KN, et al. High asthma prevalence and increased morbidity among rural children in a Medicaid cohort. Ann Allergy Asthma Immunol. 2011;106(6):467–473. doi: 10.1016/j.anai.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Akinbami LJ, Moorman JE, Garbe PL, et al. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(suppl 3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 50.Redd SC. Asthma in the United States: burden and current theories. Environ Health Perspect. 2002;110(suppl 4):557–560. doi: 10.1289/ehp.02110s4557. [DOI] [PMC free article] [PubMed] [Google Scholar]