Abstract
Objective:
Glass carbomer cement represents a new generation of dental material, which mineralizes gradually into fluorapatite. The aim of this study was to evaluate the microleakage and marginal integrity of newly developed glass carbomer cement with and without protective surface coating (SC) in primary molars.
Methods:
Standardized cavities were prepared on extracted human primary molars, and the teeth were randomly assigned into the following groups (n = 10/each): (1) conventional glass ionomer cement (GIC) without SC; (2) GIC with SC; (3) glass carbomer cement without SC; (4) glass carbomer cement with SC; and (5) compomer without SC. Following thermocycling (5 ± 2°C–55 ± 2°C, dwell time 15 s, 2000×), the specimens were immersed in 0.5% basic fuchsin solution, sectioned, and digitally photographed. Microleakage was evaluated quantitatively by using open-source image analysis toolkit (ImageJ), and the data were analyzed statistically by using Kruskal-Wallis and Conover’s Multiple Comparison tests (P=.05).
Results:
The greatest amount of dye leakage was observed in the uncoated glass carbomer specimens, followed by the uncoated glass ionomer group (P<.05). There was no significant difference between the microleakage values of coated glass ionomer, coated glass carbomer, and the compomer (P>.05). The following statistical ranking was observed among microleakage of the test materials: uncoated glass carbomer > uncoated glass ionomer > coated glass ionomer ≈ coated glass carbomer ≈ compomer. Uncoated glass carbomer exhibited severe internal ice crack-like lines.
Conclusion:
The use of the new glass carbomer cement without SC results in severe microleakage and catastrophic internal cracks.
Keywords: Glass ionomer cement, glass carbomer, image analysis, microleakage, primary teeth, sealant
INTRODUCTION
The conventional glass ionomer cement (GIC) has been advocated as a restorative material because of its ability to chemically bond to tooth structures1,2 and release fluoride.3,4 With additional benefits of biocompatibility,5 antibacterial effects,4,6 and the ability to remineralize hydroxyapatite crystals,7,8 conventional GIC has been well accepted in pediatric patients with high caries risk activity.4,9 However, conventional GICs also have a number of drawbacks that limit their indication for permanent restoration in primary teeth. In particular, GICs are advisable only in non-to-moderate stress bearing areas.10 As such, class II conventional GIC restorations show significantly shorter longevity in primary molars compared to those restored with resin-modified GICs and compomers.11 Marginal deficiencies, wear, and secondary caries are other considerations that jeopardize the long-term performance of GIC restorations in primary teeth.12,13
Resin-modified GIC and high-viscosity GICs have been developed in an attempt to overcome the inherent physical shortcomings of conventional GIC. Today, both restorative materials have been established in pediatric practice, and their favorable longevity as a permanent restoration in primary teeth have been demonstrated in several clinical studies.14,16 Recently, glass carbomer cement, a GIC-based restorative material, has been introduced with claims of improved physical characteristics. This new material contains nanosized powder particles and fluorapatite as secondary filler. The reactive glass is treated with dialkyl siloxanes described in the European Patent 20040748628. The rationale for the addition of fluorapatite into the powder is based on previous work by Van Duinen et al,17 who demonstrated the in vivo chemical transformation of glass ionomer into a fluorapatite-like material in primary teeth. The liquid of glass carbomer is polyacrylic acid. Similar to high-viscosity GICs, incorporation of nanosized filler particles into the glass carbomer cement may improve its compressive strength and wear resistance. As a final step, the manufacturer stipulates photopolymerization of this new material by using a number of light-curing sources with a high output range. Presumably, the initial setting of the glass carbomer with such units may increase the compressive strength of the material. Being a glassionomer based restorative, application of a surface protection may also aid in the improvement of surface characteristics and sealing properties of the glass carbomer cement.
Because there is no published data on the clinical use of glass carbomer cements, laboratory testing of the material may provide valuable insights into the physical properties of the material, particularly in primary teeth. Consequently, the aim of this study was to evaluate the microleakage and marginal integrity of the newly developed glass carbomer cement with and without protective surface coating in primary molars. The null hypothesis tested was 2-fold: (1) the microleakage and marginal integrity of glass carbomer cement was not influenced by the application of protective surface coating (SC), and (2) there was no difference between the sealing efficiency of glass carbomer cement, conventional GIC, and polyacid-modified resin composite in primary molars.
MATERIALS AND METHODS
Specimen preparation
Non-carious human primary molars, extracted for orthodontic reasons, were used in the present study. Following surface debridement with a hand-scaling instrument and cleaning with a rubber cup and slurry of pumice, the teeth were examined at 20 X magnification under a dissecting microscope to discard those with any visible structural defects, cracks, or carious lesions. Selected teeth (n = 50) were stored at 4°C in 0.9% w/v NaCl for a maximum of 1 month. One operator prepared standardized class I cavities with an ISO #014 cylindrical diamond bur in a high-speed handpiece under copious water spray. No bevels were added at the preparation margins.
The teeth were randomly assigned into 5 groups (n = 10/each) with regard to filling material and/or presence of an SC:
Group 1: Conventional GIC (Ionofil U, VOCO, Cuxhaven, Germany) without an SC.
Group 2: Conventional GIC (Ionofil U, VOCO, Cuxhaven, Germany) with an SC (Heliobond, Ivoclar Vivadent, Schaan, Liechtenstein).
Group 3: Glass carbomer cement (Glass Carbomer Products, Leiden, Netherlands) without an SC.
Group 4: Glass carbomer cement (Glass Carbomer Products, Leiden, Netherlands) with an SC (Glass Carbomer Surface Gloss, Glass Carbomer Products, Leiden, Netherlands).
Group 5: Compomer (Dyract Extra, Dentsply, Konstanz, Germany) without an SC.
All the materials were handled and applied by 1 calibrated operator in strict accordance with the manufacturer’s instructions. For the glass carbomer cement, photopolymerization of the surface gloss was accomplished using Elipar S10 LED Curing Light (3M ESPE, Seefeld, Germany), which is one of the proprietary high-energy light curing units recommended by the manufacturer. Heliobond and Dyract Extra were light cured using a quartz-tungsten-halogen curing unit (Optilux 501, Kerr; Danbury, CT, USA). After completion of restorative procedures, samples were stored in distilled water at 37°C for 24 h, and then subjected to thermocycling (2000×, in 5 ± 2°C to 55 ± 2°C with a dwell time of 15 s and a transfer time of 10 s).
Microleakage test and image analysis
The root apices were sealed with a sticky wax to prevent dye penetration. The samples were coated with 2 consecutive layers of nail varnish up to 1 mm from the restoration margins. Then, samples were immersed in 0.5% basic fuchsine solution (Wako Pure Chemical Industry, Osaka, Japan) for 24 h. Thereafter, samples were rinsed thoroughly under tap water, air dried, and embedded in a phenolic ring with epoxy resin (Struers, Copenhagen, Denmark). Three parallel longitudinal sections were made through the restorations18 using a low-speed, water-cooled diamond saw (Isomet, Buehler, Lake Bluff, IL, U.S.A.) in the buccolingual direction.
For each specimen, the dye penetration along the buccal and lingual margins on each of the 3 sectioned surfaces was digitally photographed at 20× (1280 × 1024 resolution) under a stereomicro-scope (Olympus, Tokyo, Japan) and transferred to a Macintosh PowerPC Workstation. On each section, the staining along the buccal and lingual restoration interfaces was measured separately (in mm) using image analysis software (Image J V1.34 for MacOSX, National Institutes of Health, Bethesda, Maryland). The microleakage value for each section was obtained by calculating the mean dye penetration along the buccal and lingual restoration margins.19 Finally, the microleakage of each tooth specimen was recorded by calculating the mean microleakage values of the 3 sections.
Statistical Analysis
Statistical comparisons of the dye penetration values were made using Kruskal-Wallis and Conover’s multiple comparison tests at P=.05.
RESULTS
The microleakage values of the test groups are presented in Table 1. All test materials exhibited dye penetration along the tooth-restoration interface. The greatest amount of dye leakage was observed in uncoated glass carbomer specimens (Conover’s multiple comparison test, P<.05). This was followed by the uncoated glass ionomer group (Table 1, P<.05). The dye penetration values of the coated glass ionomer were greater than those of the coated glass carbomer and compomer (Table 1). However, there was no significant difference between the latter 3 groups (P>.05). The following statistical ranking was observed among microleakage values of the test materials (Conover’s multiple comparison test, P=.05): uncoated glass carbomer > uncoated glass ionomer > coated glass ionomer ≈ coated glass carbomer ≈ compomer.
Table 1.
Microleakage values (mm) obtained in the study.
| Group No | Test Material | Surface Coating | Median | IQR | Minimum | Maximum |
|---|---|---|---|---|---|---|
| 1 | GIC | − | 0,50a | 0,38 | 0,00 | 1,00 |
| 2 | GIC | + | 0,35b | 0,45 | 0,00 | 1,00 |
| 3 | GC | − | 1,00c | 0,40 | 0,30 | 1,00 |
| 4 | GC | + | 0,25b | 0,78 | 0,00 | 1,00 |
| 5 | COMP | − | 0,20b | 0,60 | 0,00 | 1,00 |
Values with same superscript letters are not significantly different at P=.05 (Conover’s Multiple Comparisons test).
GIC: Glass ionomer cement; GC: Glass carbomer; COMP: Compomer; IQR: Interquartile range.
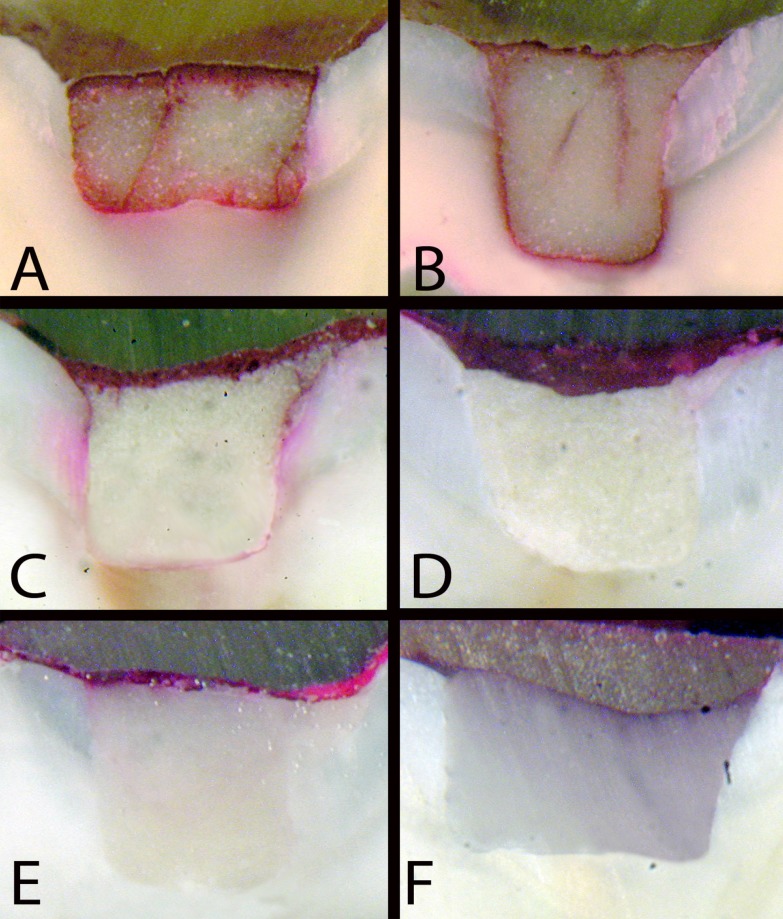
Representative micrographs depicting microleakage along the tooth-restoration interface are presented in Figure 1. All the specimens of uncoated glass carbomer exhibited oblique and vertical ice crack-like lines that extend from the restoration surface toward the cavity floor (Figures 1A and 1B). Depending on the level of sectioning, some of those lines are presented as internal cracks. In some specimens, the crack ends at the occlusal surface even exhibited minute amounts of material loss (Figure 1A). Surface cracks were also evident in uncoated GIC specimens (Figure 1C), but to a lesser extent.
Figure 1.
Examples of microleakage in the test groups. A and B: glass carbomer (GC) without surface protection (SP); C: glass ionomer cement (GIC) without SP; D: GIC with SP; E: GC with SP; F: compomer. Note the presence of ice crack-like lines in uncoated specimens of glass carbomer (A and B), and surface cracks in uncoated GIC (C).
DISCUSSION
Conventional GICs are moisture-sensitive restorative materials. During the setting stage, both water uptake and water loss can compromise the physical properties and marginal sealing of the restoration.20 Thus, following the placement of GIC, surface protection must be provided to maintain the water balance of restorations for the first 24 h.20 Among several surface coating agents tested to date (e.g., cocoa butter, waterproof varnish, and even nail varnish),21,23 light-polymerized resin adhesives have shown to provide an effective surface protection and improve marginal sealing.24,26 Heliobond is a mixture of bisphenol A-glycidyl methacrylate (Bis-GMA), triethylene glycoldimethacry-late (TEG-DMA), and photoinitiator and was used in the present study as a resin-based SC agent in the conventional GIC groups. As for the glass carbomer product, the manufacturer provides a patented carbon-silicon fluid (referred to as “Surface Gloss”) to moisten the surface of the filling during modeling and to seal the restoration surface.
The present results indicate that the absence of surface protection results in significant reductions in the marginal sealing efficiency of both the conventional GIC and the glass carbomer cement, with the latter yielding the greatest amount of microleakage among the test groups. These results necessitate rejection of the 2-fold null hypothesis that sealing properties of glass carbomer cement would not be influenced by the absence of surface protection and that all test materials would exhibit a similar level of resistance against microleakage. Despite the lack of statistical significance, it should be noted that the sealed versions of both the conventional GIC and the glass carbomer cement showed higher values of dye penetration than the compomer material, which was only tested in an unsealed state as per the manufacturer’s instructions. As with other resin-based filling materials, it can be assumed that surface protection would significantly increase the marginal sealing of the compomer.27
In the present study, the marginal integrity of the glass ionomer and glass carbomer restorations was differentially affected in the absence of surface protection. Compared with the glass carbomer cement, the unsealed glass ionomer specimens exhibited minor surface cracks in the marginal and central regions of the restorations. In the glass carbomer group, catastrophic internal and surface crack lines, resembling ice cracks, were evident in all specimens. In addition to the microleakage along the cavity walls and the pulpal floor, dye penetration was also evident within the crack lines, suggesting the severity of the loss of integrity. Similar crack patterns, referred to as “fracture lines” have been recently reported in a laboratory study investigating the microleakage of glassionomer-based sealant materials.28 In that study, the surface gloss was applied over the newly placed glass carbomer sealant, but thereafter, a special carving instrument was used to remove the excess material, which also might have removed some or most of the surface sealant before photopolymerization. Because the authors did not report placement of an additional layer of surface gloss after shaping and contouring, it is possible that the glass carbomer sealant, in its semi-sealed state, behaved like it did herein in its uncoated state. In the present study, the surface gloss was applied after the shaping/contouring step, and none of those specimens showed ice-crack lines within the hardened material.
The relationship between marginal leakage in restorations and the type of restorative materials has been extensively studied in both laboratory and clinical studies. In the absence of definitive clinical data, laboratory microleakage studies are a well-accepted method of screening the marginal sealing efficiency, and as a measure by which the performance of a restorative material can be predicted. Among different methods employed, measurement of dye penetration on sections of restored teeth is the most commonly used technique.18 In the present study, 3 sections were made through each restoration to increase the reliability of measurements.18 This technique was combined with an image analysis in order to obtain quantitative results instead of a conventional subjective scoring. A relative merit of this objective approach compared with a subjective scoring system was to discard the need for scoring by separate evaluators and for consensus scoring in borderline cases as well as statistical procedures with regard to interexaminer reliability.19
In the coated restorations, the surface gloss used with the glass carbomer cement was more effective in its sealing ability as compared to the resin-based surface coating applied to the conventional GIC. Although the manufacturer does not provide detailed information regarding how the surface gloss acts, it is evident that its proprietary formulation provides some chemical interaction with the glass carbomer cement leading to better sealing properties on glass carbomer compared to that of the non-specific Heliobond sealant on the glass ionomer. While both restorative materials have common ingredients (e.g., glass), it is also interesting to observe the inferior sealing characteristics of the glass carbomer in its un-sealed state, particularly in comparison with the uncoated GIC. Although a dye-penetration setup alone cannot explain the exact reasons for this finding, it may be speculated that the absence of the wetting effect of the glass carbomer surface gloss coupled with the dehydrating effect of the high-energy light-curing unit may have resulted in a rapid deterioration of the material surface and tooth-material interface, leading to increased levels of leakage. In this regard, further studies are also required to elucidate the physical changes in glass carbomer cement, especially when the protective surface gloss is lost over time. Unlike the latter 2 materials, a hydrophobic polymer network is formed immediately after photopolymerization of the compomer, which maintains the surface integrity and provides adequate resistance against leakage in the absence of surface protection.
CONCLUSIONS
Within the limitations of this in vitro study, the following conclusions were drawn:
Surface protection should be added to glass carbomer restorations in primary teeth.
Sealed glass carbomer cement yields similar sealing efficiency as with the sealed conventional GIC and unsealed compomer.
REFERENCES
- 1.Smith DC. Polyacrylic acid-based cements-adhesion to enamel and dentin. Oper Dent. 1992;(Suppl 5):177–183. [PubMed] [Google Scholar]
- 2.Erickson RL, Glasspoole EA. Bonding to tooth structure: a comparison of glassionomer and composite-resin systems. J Esthet Dent. 1994;6:227–244. doi: 10.1111/j.1708-8240.1994.tb00864.x. [DOI] [PubMed] [Google Scholar]
- 3.Nikolaos K, Vassiliki T, Christine T, Eirini T. The early fluoride release pattern of an aged glass ionomer treated with fluoride. Eur J Prosthodont Restor Dent. 2007;15:135–141. [PubMed] [Google Scholar]
- 4.Davidovich E, Weiss E, Fuks AB, Beyth N. Surface antibacterial properties of glass ionomer cements used in atraumatic restorative treatment. J Am Dent Assoc. 2007;138:1347–1352. doi: 10.14219/jada.archive.2007.0051. [DOI] [PubMed] [Google Scholar]
- 5.Modena KC, Casas-Apayco LC, Atta MT, Costa CA, Hebling J, Sipert CR, Navarro MF, Santos CF. Cytotoxicity and biocompatibility of direct and indirect pulp capping materials. J Appl Oral Sci. 2009;17:544–554. doi: 10.1590/S1678-77572009000600002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hallgren A, Oliveby A, Twetman S. Caries associated micro-flora in plaque from orthodontic appliances retained with glassionomer cement. Scand J Dent Res. 1992;100:140–143. doi: 10.1111/j.1600-0722.1992.tb01729.x. [DOI] [PubMed] [Google Scholar]
- 7.Valk JW, Davidson CL. The relevance of controlled fluoride release with bonded orthodontic appliances. J Dent. 1987;15:257–260. doi: 10.1016/0300-5712(87)90049-2. [DOI] [PubMed] [Google Scholar]
- 8.Bynum AM, Donly KJ. Enamel de/remineralization on teeth adjacent to fluoride releasing materials without dentifrice exposure. ASDC J Dent Child. 1999;66:89–92. [PubMed] [Google Scholar]
- 9.Rutar J, McAllan L, Tyas MJ. Three-year clinical performance of glass ionomer cement in primary molars. Int J Paediatr Dent. 2002;12:146–147. doi: 10.1046/j.1365-263x.2002.00339.x. [DOI] [PubMed] [Google Scholar]
- 10.Tyas MJ, Burrow MF. Adhesive restorative materials: a review. Aust Dent J. 2004;49:112–121. doi: 10.1111/j.1834-7819.2004.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 11.Qvist V, Poulsen A, Teglers PT, Mjör IA. The longevity of different restorations in primary teeth. Int J Paediatr Den. 2010;20:1–7. doi: 10.1111/j.1365-263X.2009.01017.x. [DOI] [PubMed] [Google Scholar]
- 12.Hickel R, Kaaden C, Paschos E, Buerkle V, García-Godoy F, Manhart J. Longevity of occlusally-stressed restorations in posterior primary teeth. Am J Dent. 2005;18:198–211. [PubMed] [Google Scholar]
- 13.Hübel S, Mejàre I. Conventional versus resin-modified glassionomer cement for Class II restorations in primary molars. A 3-year clinical study. Int J Paediatr Dent. 2003;13:2–8. doi: 10.1046/j.1365-263x.2003.00416.x. [DOI] [PubMed] [Google Scholar]
- 14.Qvist V, Manscher E, Teglers PT. Resin-modified and conventional glass ionomer restorations in primary teeth: 8-year results. J Dent. 2004;2:285–294. doi: 10.1016/j.jdent.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Qvist V, Laurberg L, Poulsen A, Teglers PT. Class II restorations in primary teeth: 7-year study on three resin-modified glass ionomer cements and a compomer. Euro J Oral Sci. 2004;112:188–196. doi: 10.1111/j.1600-0722.2004.00117.x. [DOI] [PubMed] [Google Scholar]
- 16.Faccin ES, Ferreira SH, Kramer PF, Ardenghi TM, Feldens CA. Clinical performance of ART restorations in primary teeth: a survival analysis. J Clin Pediatr Dent. 2009;33:295–298. doi: 10.17796/jcpd.33.4.001283522r230h70. [DOI] [PubMed] [Google Scholar]
- 17.Van Duinen RN, Davidson CL, De Gee AJ, Feilzer AJ. In situ transformation of glassionomer into an enamel-like material. Am J Dent. 2004;17:223–227. [PubMed] [Google Scholar]
- 18.Raskin A, Tassery H, D’hoore W, Gonthier S, Vreven J, Degrange M, Dejaou J. Influence of the number of specimens on reliability of in vitro microleakage evaluations. Am J Dent. 2003;6:207–210. [PubMed] [Google Scholar]
- 19.Cehreli ZC, Gungor HC. Quantitative microleakage evaluation of fissure sealants applied with or without a bonding agent: results after four-year water storage in vitro. J Adhes Dent. 2008;10:379–384. [PubMed] [Google Scholar]
- 20.Mount GJ, Makinson OF. Glassionomer restorative cements: clinical implications of the setting reaction. Oper Dent. 1982;7:134–141. [PubMed] [Google Scholar]
- 21.Asmussen E. Opacity of glassionomer cements. Acta Odontol Scand. 1983;41:155–7. doi: 10.3109/00016358309162317. [DOI] [PubMed] [Google Scholar]
- 22.Earl MS, Hume WR, Mount GJ. Effect of varnishes and other surface treatments on water movement across the glassionomer cement surface. Aust Dent J. 1985;30:298–301. doi: 10.1111/j.1834-7819.1985.tb02513.x. [DOI] [PubMed] [Google Scholar]
- 23.Rodrigues Garcia RC, De Goes MF, Del Bel Cury AA. Influence of protecting agents on the solubility of glass ionomers. Am J Dent. 1995;8:294–296. [PubMed] [Google Scholar]
- 24.Hotta M, Hirukawa H, Yamamoto K. Effect of coating materials on restorative glassionomer cement surface. Oper Dent. 1992;17:57–61. [PubMed] [Google Scholar]
- 25.Watson T, Banerjee A. Effectiveness of glassionomer surface protection treatments: a scanning optical microscope study. Eur J Prosthodont Restor Dent. 1993;2:85–90. [PubMed] [Google Scholar]
- 26.Using glass ionomers Council on Dental Materials, Instruments, and Equipment. J Am Dent Assoc. 1990;121:181–188. [PubMed] [Google Scholar]
- 27.Guelmann M, Bonnin S, Primosch RE, Söderholm KJ. Microleakage and wall adaptation of conservative restorations. Am J Dent. 2002;15:407–411. [PubMed] [Google Scholar]
- 28.Chen X, Cuijpers V, Fan M, Frencken JE. Marginal leakage of two newer glassionomer-based sealant materials assessed using micro-CT. J Dent. 2010;38:731–735. doi: 10.1016/j.jdent.2010.05.018. [DOI] [PubMed] [Google Scholar]