Abstract
Objective:
This study aimed to compare the cephalometric characteristics of obstructive sleep apnea (OSA) patients with those of healthy subjects and to determine possible relationships between cephalometric measurements of OSA patients and control subjects.
Methods:
Standardized lateral cephalograms of 16 OSA patients and 16 healthy controls were obtained. Airway dimensions and dentofacial parameters were measured using a cephalometric analysis program (Dolphin Imaging Cephalometric and Tracing Software, Chatsworth, CA, USA). All statistical analyses were conducted using SPSS version 17.0.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were calculated for all measurements, and the Mann–Whitney U test was used to evaluate intergroup differences.
Results:
Midface length was significantly shorter and upper lip E-plane length was significantly longer in the OSA group than in the controls (P<.05). SNA, SNB, and mandibular plane angles (GoGn-SN), anterior and posterior facial heights, and posteroanterior face height ratio were similar in both groups. Maxillary length was slightly longer in the OSA group, whereas the mandibular length showed a slight increase in the control group (P<.05). The axial inclination of the lower incisor to its respective plane was normal, whereas the upper incisor was significantly protrusive (P<.05) in the OSA group. Distance between the hyoid and mandible was significantly greater in the OSA group than in the controls, indicating that the hyoid bone was positioned more downward in the OSA group (P<.05).
Conclusions:
In this study, the patients with OSA demonstrated significant differences in several craniofacial measurements. OSA patients showed reduced midface length and inferiorly placed hyoid bone and tended to have smaller airway dimensions.
Keywords: Cephalometry, obsrtructive sleep apnea, airway
INTRODUCTION
Sleep induces an unnatural and unusual increase in upper-airway resistance in about 2–5% of the adult population; this condition is known as obstructive sleep apnea (OSA).1,2 OSA is characterized by frequent episodes of airway obstruction associated with a reduced diameter of the upper airway, which is vulnerable to further narrowing and collapse.3 Acute and repeated effects of apnea and hypopnea include oxygen desaturation, reduction in intrathoracic pressure, withered executive function and central nervous system arousals, and excessive daytime sleepiness.4
The causes of OSA include factors related to the upper airway anatomy, for instance, narrow airway space, relative mandibular retrognathia, increased tongue volume, and enlargement of palatine or adenoidal tissue.3,5,6 Severity of OSA may be assessed subjectively by the patient or his/her spouse and objectively by nocturnal polysomnography or imaging techniques.7 However, polysomnography has the disadvantage of being time consuming and complicated.8
Lateral cephalography is useful to analyze skeletal and soft tissue characteristics of patients with OSA and has the advantage of being available in most dental clinics, easy to perform, and less expensive than a polysomnographic examination.9,10 Skeletal differences between OSA patients and control groups have been observed in the sagittal and vertical planes.11–14 Moreover, a tendency toward shorter dimension of the cranial base and maxillary length, maxillo-mandibular retrognathia, and increased anterior lower facial height and mandibular plane angle have been reported.15–17 Although several studies have analyzed these skeletal differences, there is still much debate on this subject, particularly on the positions of the mandible and hyoid bone and length of the soft palate.
The conflicting results obtained by these studies suggest the need for well-designed controlled studies to clearly evaluate the cephalometric characteristics of OSA patients. The present study aimed to compare the cephalometric characteristics of OSA patients with healthy subjects and determine possible relationships between cephalometric measurements of OSA patients and control subjects. The null hypothesis to be tested stated that no difference exists in craniofacial morphology between patients with OSA and the healthy population.
MATERIALS AND METHODS
This study included 16 OSA patients (11 men and 5 women; mean age, 51.5 ± 11.01 years) and 16 healthy subjects (10 men and 6 women; mean age, 48.06 ± 9.74 years).
Subjects diagnosed with OSA on the basis of polysomnography performed at the Suleyman Demirel University, Faculty of Medicine, were referred to the Suleyman Demirel University, Faculty of Dentistry, Department of Oral Diagnosis and Radiology. The patients with OSA was classified according to Apnoea + Hypopnoea Index (AHI = average number of apnoeas+ hypopnoeas/hour during sleep). The control group were consisted of the patients who participated in the study and had AHI<10. Two of the 16 subjects, who have been determined to have OSA, had mild (AHI = 10–30), 11 had moderate (AHI = 31–50), 3 had severe (AHI > 50) OSA. Informed consent was obtained from all the patients, and standardized lateral cephalograms of the patients were obtained.
The exclusion criteria for the OSA patients were as follows:
Having less than 10 teeth in each jaw.
Having temporomandibular disorders.
Having severe periodontitis.
Standardized lateral cephalograms of 16 healthy subjects, who did not snore, have any history of respiratory disorders, or have daytime somnolence, were retrospectively obtained from the archives of the Suleyman Demirel University, Faculty of Dentistry, Department of Oral Diagnosis and Radiology.
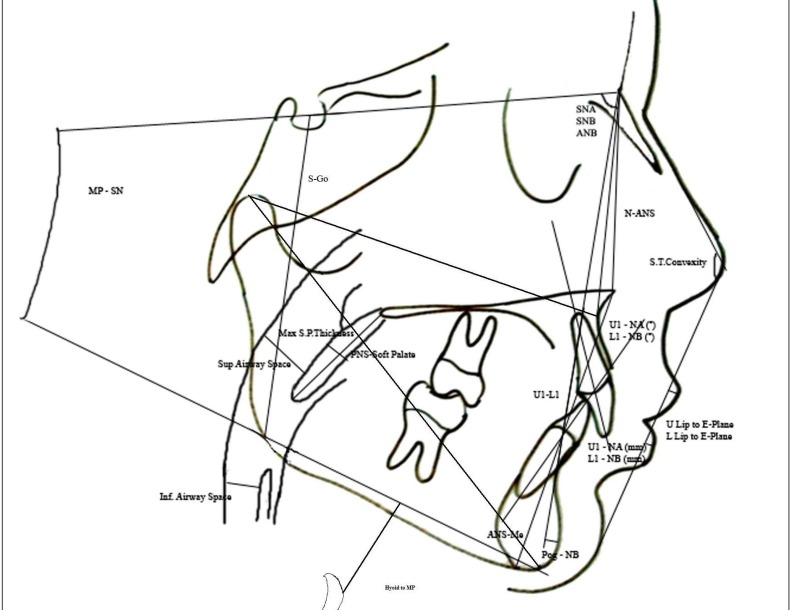
Airway dimensions and dentofacial parameters were measured using a cephalometric analysis program (Dolphin Imaging Cephalometric and Tracing Software, Chatsworth, CA, USA). A total of 22 measurements were performed on the lateral cephalograms (Figure 1). Cephalometric landmarks were marked and digitized by one of the authors (A.Y.G). In 10 subjects, all of the measurements were repeated 2 weeks later to determine the measurement error, which was 0.994 or greater for all parameters.
Figure 1.
Measurements on lateral cephalometric films.
Statistical method
All statistical analyses were conducted using SPSS version 17.0.0 (SPSS Inc., Chicago, IL, USA). Significance for all statistical tests was predetermined at P<.05. Descriptive statistics were calculated for all measurements, and the Mann–Whitney U test was used to evaluate intergroup differences.
RESULTS
In the OSA group, the age of the patients varied from 32 to 74 years, with a mean age of 51.5 ± 11.01 years. The age range in the control group was 33–63 years, with a mean age of 48.6 ± 9.74 years. Age, snoring time, accompanying pathology, and Epworth sleep scale findings of the OSA patients are presented in Table 1. Of the 16 patients, 7 had nasal septum deviation, and the frequency of occurrence of deviation on the right and left sides was almost equal (4/3). Of the 16 patients, 6 had concha nasalis hypertrophy and 4 had uvula hypertrophy. Nasal polyps or high tonsils were not present in any of the patients.
Table 1.
Age, snoring time, accompanying pathology and Epworth sleep scale findings of the OSA patients.
| No | Age | Snoring Time (Years) | Accompaying Patology | Epworth Sleep Scale | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Septum Deviation | Conca H. | Nasal P. | H. Tonsilla | Uvula H. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
| 1 | 53 | 3,5 | Left | Lower Right | 1 | 3 | 0 | 0 | 1 | 0 | 1 | 0 | |||
| 2 | 66 | 2,5 | Left | x | 1 | 2 | 1 | 0 | 2 | 0 | 1 | 0 | |||
| 3 | 48 | 20 | x | x | 3 | 3 | 3 | 3 | 2 | 1 | 2 | 1 | |||
| 4 | 43 | 2,5 | Lower Right | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| 5 | 58 | 12 | x | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| 6 | 69 | 20 | Left | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | ||||
| 7 | 50 | 12 | Left | Lower Bilateral | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | |||
| 8 | 50 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| 9 | 73 | 10 | x | x | 2 | 2 | 3 | 0 | 3 | 1 | 3 | 0 | |||
| 10 | 46 | 3 | Right | Lower Left | 2 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 11 | 52 | 7,5 | x | 3 | 3 | 0 | 2 | 2 | 0 | 3 | 0 | ||||
| 12 | 32 | 5 | x | x | 2 | 2 | 0 | 0 | 1 | 0 | 2 | 0 | |||
| 13 | 52 | 1 | x | x | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 14 | 50 | 20 | x | 3 | 1 | 3 | 2 | 1 | 1 | 3 | 0 | ||||
| 15 | 35 | 5 | Right | 2 | 1 | 0 | 2 | 2 | 0 | 2 | 0 | ||||
| 16 | 47 | 5 | Right | 1 | 0 | 0 | 2 | 3 | 0 | 0 | 0 | ||||
The results of the descriptive statistics and intergroup comparison of cephalometric variables are presented in Table 2. Radiographs of the OSA patients and control group subjects showed very similar facial characteristics. Midface length was significantly shorter and upper lip E-plane length was significantly longer in the OSA group than in the control group (P<.05). SNA, SNB, and mandibular plane angles (GoGn-SN), anterior and posterior facial heights, and posteroanterior face height ratio were similar in both groups (P>.05). Maxillary length was slightly longer in the OSA group, whereas the mandibular length was found to be slightly increased in the control group (P<.05).
Table 2.
Comparison of the cephalometric variables (Mann Withney U test; *P<.05).
| Parameters | Patients with OSA | Healthy Individuals | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean | SD | Lower | Upper | Mean | SD | Lower | Upper | P | |
|
| |||||||||
| Maxilla-Mandible | |||||||||
| ANB (º) | 1,39 | 3,41 | −5,50 | 5,80 | 3,83 | 2,44 | −1,40 | 7,70 | |
| SNA (º) | 80,93 | 3,84 | 71,40 | 85,60 | 82,29 | 3,77 | 77,40 | 89,00 | |
| SNB (º) | 79,55 | 4,59 | 67,40 | 90,00 | 78,46 | 4,02 | 70,50 | 86,00 | |
| mandibular body | 89,20 | 6,26 | 26,90 | 100,50 | 88,33 | 6,77 | 67,10 | 98,10 | |
| maxillary length | 53,10 | 4,82 | 44,80 | 63,70 | 55,42 | 5,08 | 46,00 | 63,10 | |
| midface length | 88,39 | 5,35 | 79,6 | 97,6 | 93,32 | 5,91 | 83,4 | 106,9 | * |
| GoGn-SN | 32,66 | 7,36 | 21,60 | 50,40 | 34,11 | 5,27 | 25,20 | 46,00 | |
| Lower Lip to E-Plane (mm) | −6,97 | 2,58 | −10,30 | 3,70 | −2,49 | 3,51 | −8,10 | 5,10 | |
| Upper Lip to E-Plane (mm) | −6,66 | 2,63 | −9,90 | −0,80 | −4,40 | 3,08 | −8,70 | 2,50 | * |
| Anterior Face Height (NaMe) (mm) | 134,64 | 11,06 | 119,9 | 159,2 | 138,83 | 9,06 | 123,00 | 157,30 | |
| Posterior Face Height (SGo) (mm) | 87,33 | 8,82 | 69.1 | 97,30 | 90,25 | 7,17 | 78,70 | 104,00 | |
| P-A Face Height (S-Go/N-Me) (%) | 64,98 | 5,70 | 51,40 | 74,10 | 65,03 | 3,32 | 57,70 | 71,20 | |
| Dental | |||||||||
| Interincisal Angle (U1-L1) (º) | 125,89 | 8,16 | 112,30 | 141,60 | 132,85 | 9,88 | 117,60 | 150,10 | |
| U1 - NA (mm) | 4,68 | 3,49 | −2,80 | 8,50 | 3,18 | 3,29 | −2,00 | 10,30 | |
| L1 - NB (mm) | 2,89 | 4,67 | −6,10 | 9,60 | 5,36 | 3,46 | 0,30 | 12,90 | |
| U1 - NA (º) | 23,03 | 6,16 | 11,40 | 31,50 | 17,10 | 7,35 | 6,00 | 29,30 | * |
| L1 - NB (º) | 25,18 | 7,16 | 14,80 | 38,00 | 24,98 | 7,06 | 15,10 | 39,60 | |
| Pog - NB (mm) | 2,87 | 2,16 | −1,00 | 7,50 | 2,39 | 2,60 | −2,30 | 6,70 | |
| Airway | |||||||||
| PNS to Soft Palate (mm) | 42,71 | 5,14 | 34,40 | 52,00 | 41,66 | 5,47 | 34,50 | 56,80 | |
| Max Soft Palate Thickness (mm) | 9,84 | 2,02 | 6,70 | 13,30 | 9,24 | 1,95 | 6,90 | 14,70 | |
| Inferior Airway Space IAS (mm) | 7,12 | 2,81 | 3,90 | 14,30 | 8,26 | 2,71 | 2,80 | 13,60 | |
| Sup Airway Space SPAS (mm) | 10,67 | 3,27 | 5,90 | 17,70 | 11,26 | 4,00 | 5,20 | 19,90 | |
| Hyoid to Mandible | 25,87 | 7,33 | 15,50 | 37,20 | 19,75 | 6,57 | 9,30 | 31,20 | * |
Dental examination showed that there were no differences between the position of the teeth in the OSA and control groups. The axial inclination of the lower incisor to its respective plane was normal, whereas the upper incisor was significantly protrusive (P<.05).
The distance between the hyoid and mandible was significantly greater in the OSA group than in the control group; this finding indicated that the hyoid bone was positioned more downward in the OSA group (P<.05). All of the airway measurements were smaller in the OSA group than in the control group; however, the difference in middle airway space length was significant in the OSA group (P<.05).
DISCUSSION
Recent studies have reported skeletal differences between OSA patients and control groups in the sagittal and vertical planes.11–14 Battagel et al18 stated that these anatomical differences place the entire facial complex closer to the cervical spine and thus contribute to the reduction of space available for the airway in both sleep-disordered breathing groups.
This study failed to demonstrate any differences in the positional relationships of the mandible and maxilla between the OSA and control groups in both the vertical and sagittal dimensions; this finding was in contrast to that of another study.15 Mandibular retrognathia has been reported by some authors,19–22 whereas other studies have found no evidence of mandibular retrognathia.9,23,24
OSA patients had reduced midface length, and this finding supported that of Tangugsorn et al15 Reduced midface length may cause a reduction of space available for the airway.
The upper incisors were more protrusive in the OSA patients than in the control group. However, other studies did not find any such difference.9,18 Protrusion of the upper incisors may be attributed to oral breathing resulting from obstruction of the upper airways. Although the upper incisors were more protrusive, we found that the upper lips were more retrusive to the E-plane in the OSA group. This could be due to the reduction in midface length. Protrusion of the upper incisors may not be able to compensate for the reduction in midface length.
In OSA patients, the hyoid bone was more inferiorly placed. This finding was consistent with those of previous investigations.11,18,22,24–27 Determining the position of the hyoid bone is important because of its relationship with tongue position. Lower position of the hyoid causes more of the tongue mass to be concentrated in the hypopharyngeal area and may therefore be a poor prognostic indicator for the successful use of mandibular advancement splints.18,28,29 Arya et al6 stated that the hyoid bone plays an important role in maintaining the upper airway dimensions. Lower position of the hyoid with a lower tongue posture may increase the mandibular load because of the requirement of extra energy to elevate the tongue; this, in turn, may aggravate apnea by resulting in the open-mouth posture during sleep.6,30
In the present study, the airways tended to be smaller in the OSA patients than in the control group; however, this difference was insignificant in the upper and lower airway spaces. Enciso et al31 found significantly smaller lateral dimension in OSA patients, however they found no significant differences in mean airway length, average cross-sectional airway and total volume of the airways. On the other hand another study showed increased airway length with elliptical in shape.32 Ivanhoe et al33 stated that the narrower dimensions of the upper airway in OSA patients than in normal people may be due to structural differences in the craniofacial structures that support the airway.
Airway collapse often occurs when patients sleep on their back and the base of the tongue abuts the posterior pharyngeal wall and soft palate.34 Elongated soft palate or excessive tissue in the soft palate is one of the most common cause of snoring and OSA.34 In the present study, we found no significant differences in soft palate length between the OSA and control groups. This finding was consistent with those of other studies.15,24,25,35 However, in some studies, soft palate length was significantly shorter in the OSA patients than in the controls.18,26 In our study, soft palate thickness showed no significant difference between the OSA patients and controls. In contrast, Battagel et al18 showed a significant increase in soft palate thickness in OSA patients.
On the basis of these results, the null hypothesis was rejected. Significant differences existed in the craniofacial morphology of patients with OSA and the healthy population.
CONCLUSIONS
Significant differences existed in the craniofacial morphology of patients with OSA and the healthy population.
OSA patients showed reduced midface length and inferiorly placed hyoid bone and tended to have smaller airway dimensions.
Positional relationships of the maxilla and mandible to the cranial base and to each other are similar between the OSA patients and healthy subjects.
REFERENCES
- 1.Kim J, In K, Kim J, You S, Kang K, Shim J, Lee S, Lee J, Lee S, Park C, Shin C. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004;170:1108–1113. doi: 10.1164/rccm.200404-519OC. [DOI] [PubMed] [Google Scholar]
- 2.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.Sunitha C, Kumar SA. Obstructive sleep apnea and its management. Indian J Dent Res. 2010;21:119–124. doi: 10.4103/0970-9290.62806. [DOI] [PubMed] [Google Scholar]
- 4.Sunitha C, Aravindkumar S. Obstructive sleep apnea: clinical and diagnostic features. Indian J Dent Res. 2009;20:487–491. doi: 10.4103/0970-9290.59457. [DOI] [PubMed] [Google Scholar]
- 5.Meyer JB, Jr, Knudson RC. The sleep apnea syndrome. Part I: Diagnosis. J Prosthet Dent. 1989;62:675–679. doi: 10.1016/0022-3913(89)90591-x. [DOI] [PubMed] [Google Scholar]
- 6.Arya D, Tripathi A, Singh SV, Tripathi S, Nagar A, Mishra A. A pilot study to evaluate posttreatment cephalometric changes in subjects with OSA. J Prosthet Dent. 2010;103:170–177. doi: 10.1016/S0022-3913(10)60024-8. [DOI] [PubMed] [Google Scholar]
- 7.Clark GT, Blumenfeld I, Yoffe N, Peled E, Lavie P. A crossover study comparing the efficacy of continuous positive airway pressure with anterior mandibular positioning devices on patients with obstructive sleep apnea. Chest. 1996;109:1477–1483. doi: 10.1378/chest.109.6.1477. [DOI] [PubMed] [Google Scholar]
- 8.Practice parameters for the indications for polysomnography and related procedures. Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Sleep. 1997;20:406–422. [PubMed] [Google Scholar]
- 9.Battagel JM, L'Estrange PR. The cephalometric morphology of patients with obstructive sleep apnoea (OSA) Eur J Orthod. 1996;18:557–569. doi: 10.1093/ejo/18.6.557. [DOI] [PubMed] [Google Scholar]
- 10.Bacon WH, Turlot JC, Krieger J, Stierle JL. Cephalometric evaluation of pharyngeal obstructive factors in patients with sleep apneas syndrome. Angle Orthod. 1990;60:115–122. doi: 10.1043/0003-3219(1990)060<0115:CEOPOF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Pracharktam N, Hans MG, Strohl KP, Redline S. Upright and supine cephalometric evaluation of obstructive sleep apnea syndrome and snoring subjects. Angle Orthod. 1994;64:63–73. doi: 10.1043/0003-3219(1994)064<0063:UASCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Svanholt P, Petri N, Wildschiodtz G, Sonnesen L, Kjaer I. Associations between craniofacial morphology, head posture, and cervical vertebral body fusions in men with sleep apnea. Am J Orthod Dentofacial Orthop. 2009;135:702 e701–709. doi: 10.1016/j.ajodo.2009.02.011. discussion 702–703. [DOI] [PubMed] [Google Scholar]
- 13.Seto BH, Gotsopoulos H, Sims MR, Cistulli PA. Maxillary morphology in obstructive sleep apnoea syndrome. Eur J Orthod. 2001;23:703–714. doi: 10.1093/ejo/23.6.703. [DOI] [PubMed] [Google Scholar]
- 14.Sonnesen L, Petri N, Kjaer I, Svanholt P. Cervical column morphology in adult patients with obstructive sleep apnoea. Eur J Orthod. 2008;30:521–526. doi: 10.1093/ejo/cjn028. [DOI] [PubMed] [Google Scholar]
- 15.Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T. Obstructive sleep apnoea: a cephalometric study. Part I. Cervico-craniofacial skeletal morphology. Eur J Orthod. 1995;17:45–56. doi: 10.1093/ejo/17.1.45. [DOI] [PubMed] [Google Scholar]
- 16.Tangugsorn V, Krogstad O, Espeland L, Lyberg T. Obstructive sleep apnea (OSA): a cephalometric analysis of severe and non-severe OSA patients. Part I: Multiple comparison of cephalometric variables. Int J Adult Orthodon Orthognath Surg. 2000;15:139–152. [PubMed] [Google Scholar]
- 17.Enache AM, Nimigean VR, Mihălţan F, Didilescu AC, Munteanu I, Nimigean V. Assessment of sagittal and vertical skeletal patterns in Romanian patients with obstructive sleep apnea. Rom J Morphol Embryol. 2010;51:505–508. [PubMed] [Google Scholar]
- 18.Battagel JM, Johal A, Kotecha B. A cephalometric comparison of subjects with snoring and obstructive sleep apnoea. Eur J Orthod. 2000;22:353–365. doi: 10.1093/ejo/22.4.353. [DOI] [PubMed] [Google Scholar]
- 19.Hochban W, Brandenburg U. Morphology of the viscerocranium in obstructive sleep apnoea syndrome--cephalometric evaluation of 400 patients. J Craniomaxillofac Surg. 1994;22:205–213. doi: 10.1016/s1010-5182(05)80559-1. [DOI] [PubMed] [Google Scholar]
- 20.Jamieson A, Guilleminault C, Partinen M, Quera-Salva MA. Obstructive sleep apneic patients have craniomandibular abnormalities. Sleep. 1986;9:469–477. doi: 10.1093/sleep/9.4.469. [DOI] [PubMed] [Google Scholar]
- 21.Series F, St Pierre S, Carrier G. Effects of surgical correction of nasal obstruction in the treatment of obstructive sleep apnea. Am Rev Respir Dis. 1992;146:1261–1265. doi: 10.1164/ajrccm/146.5_Pt_1.1261. [DOI] [PubMed] [Google Scholar]
- 22.Andersson L, Brattstrom V. Cephalometric analysis of permanently snoring patients with and without obstructive sleep apnea syndrome. Int J Oral Maxillofac Surg. 1991;20:159–162. doi: 10.1016/s0901-5027(05)80007-4. [DOI] [PubMed] [Google Scholar]
- 23.deBerry-Borowiecki B, Kukwa A, Blanks RH. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988;98:226–234. doi: 10.1288/00005537-198802000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Zucconi M, Ferini-Strambi L, Palazzi S, Orena C, Zonta S, Smirne S. Habitual snoring with and without obstructive sleep apnoea: the importance of cephalometric variables. Thorax. 1992;47:157–161. doi: 10.1136/thx.47.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maltais F, Carrier G, Cormier Y, Series F. Cephalometric measurements in snorers, non-snorers, and patients with sleep apnoea. Thorax. 1991;46:419–423. doi: 10.1136/thx.46.6.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frohberg U, Naples RJ, Jones DL. Cephalometric comparison of characteristics in chronically snoring patients with and without sleep apnea syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:28–33. doi: 10.1016/s1079-2104(95)80012-3. [DOI] [PubMed] [Google Scholar]
- 27.Ozbek MM, Miyamoto K, Lowe AA, Fleetham JA. Natural head posture, upper airway morphology and obstructive sleep apnoea severity in adults. Eur J Orthod. 1998;20:133–143. doi: 10.1093/ejo/20.2.133. [DOI] [PubMed] [Google Scholar]
- 28.Lyberg T, Krogstad O, Djupesland G. Cephalometric analysis in patients with obstructive sleep apnoea syndrome: II. Soft tissue morphology. J Laryngol Otol. 1989;103:293–297. doi: 10.1017/s0022215100108746. [DOI] [PubMed] [Google Scholar]
- 29.Mayer G, Meier-Ewert K. Cephalometric predictors for orthopaedic mandibular advancement in obstructive sleep apnoea. Eur J Orthod. 1995;17:35–43. doi: 10.1093/ejo/17.1.35. [DOI] [PubMed] [Google Scholar]
- 30.Caballero P, Alvarez-Sala R, García-Río F, Prados C, Hernán MA, Villamor J, Alvarez-Sala JL. CT in the evaluation of the upper airway in healthy subjects and in patients with obstructive sleep apnea syndrome. Chest. 1998;113:111–116. doi: 10.1378/chest.113.1.111. [DOI] [PubMed] [Google Scholar]
- 31.Enciso R, Nguyen M, Shigeta Y, Ogawa T, Clark GT. Comparison of cone-beam CT parameters and sleep questionnaires in sleep apnea patients and control subjects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:285–293. doi: 10.1016/j.tripleo.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abramson Z, Susarla S, August M, Troulis M, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy in patients with obstructive sleep apnea. J Oral Maxillofac Surg. 2010;68:354–362. doi: 10.1016/j.joms.2009.09.087. [DOI] [PubMed] [Google Scholar]
- 33.Ivanhoe JR, Cibirka RM, Lefebvre CA, Parr GR. Dental considerations in upper airway sleep disorders: A review of the literature. J Prosthet Dent. 1999;82:685–698. doi: 10.1016/s0022-3913(99)70010-7. [DOI] [PubMed] [Google Scholar]
- 34.Ephros HD, Madani M, Yalamanchili SC. Surgical treatment of snoring & obstructive sleep apnoea. Indian J Med Res. 2010;131:267–276. [PubMed] [Google Scholar]
- 35.Pracharktam N, Nelson S, Hans MG, Broadbent BH, Red-line S, Rosenberg C, Strohl KP. Cephalometric assessment in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996;109:410–419. doi: 10.1016/s0889-5406(96)70123-3. [DOI] [PubMed] [Google Scholar]