Abstract
This case report aimed to present the long-term clinical performance of mineral trioxide aggregate (MTA) pulpotomies in immature permanent teeth. Four patients with complicated crown fractures of five maxillary immature central incisor teeth were treated with pulpotomy using gray MTA. An immature mandibular first molar showing signs of reversible pulpitis that was exposed mechanically during cavity preparation was also treated with MTA pulpotomy. Four of the 6 immature teeth were diagnosed vitally with complete root maturation and with the presence of dentin bridges after 55 months (mean time of follow-ups). MTA pulpotomy was assessed unsuccessfully in two fractured central incisors. Severe discoloration in the crowns was present in all 6 cases. MTA may induce pulp healing with dentin bridge formation and prevent necrosis at long-term periods in most of the pulpotomy cases. However, discoloration following MTA pulpotomy is a significant clinical complication.
Keywords: Immature teeth, mineral trioxide aggregate, pulpotomy
INTRODUCTION
Preserving the vitality of traumatically injured and mechanically exposed immature teeth is one of the major treatment aims in endodontics. Partial pulpotomy (Cvek pulpotomy) and deep (cervical) pulpotomy techniques are the choices of treatment for immature permanent teeth with exposed pulps.1,2 These techniques can maintain pulp vitality and provide continuation of tooth root development in association with the formation of a hard tissue bridge across the exposed pulp surface.3
Calcium hydroxide (CH) materials have long been used as the agents of choice for treating exposed pulp, due to the short-term antimicrobial effect and the stimulation of hard-tissue bridge formation.4 Coagulation necrosis produced by releasing hydroxyl ions from CH materials has been believed to induce bridge formation at the exposed area.4,5 Higher calcium levels and alkalinity provided by CH were also shown to lead to increased bone morphogenetic protein-2 expression and solubilization of bioactive molecule tissue growth factor-β1 from dentin tissue.6,7 TGF-β1 and BMP-2 may play roles in dentin bridge formation.8 Moreover, calcium ions in association with necrotic cell debris may contribute to the formation of dystrophic calcification, to which fibronectin can bind and thereby initiate differentiation of odontoblast-like cells.9
Mineral trioxide aggregate (MTA) has been used as an alternative agent to CH materials in direct pulp capping and pulpotomy treatments. CH is one of the major hydration products during setting reactions of MTA, and CH is soluble from MTA in decreasing rates over time.10 Calcium and OH ion release from MTA may be essential for pulp tissue healing with bridge formation, which is similar to CH materials.8 MTA generally showed better sealing ability as a root-end filling material than conventional zinc-oxide eugenol cements, and it induced the formation of more and thicker dentin bridges than CH.11–14 Clinical reports also demonstrated very successful results such as the maintenance of pulp vitality over longer periods of time and the continuation of root formation with MTA as a pulpotomy agent.15–17 In recent years, the use of MTA has been popular in pulpotomy of permanent teeth showing symptoms of reversible and irreversible pulpitis and in complicated crown fractures of immature teeth and mature teeth.18,19 Contrarily, the high solubility, high price and dis-coloring effect of both gray and white forms are among the disadvantages of MTA, when used as a pulpotomy agent.15,20
The present case report demonstrates long-term clinical performance of MTA pulpotomies in six immature permanent teeth.
CASE REPORT
Diagnosis and treatment procedures
Four patients with complicated crown fractures of 5 maxillary immature central incisor teeth were referred to the Department of Endodontics, Istanbul University, between 2005 and 2006. The patients were between 8 and 10 years old. All 5 teeth were treated with deep pulpotomy using gray MTA (ProRoot MTA; Dentsply Tulsa Dental, Tulsa, OK, USA). Another immature mandibular first molar that was sensitive to cold stimulation and exposed mechanically during cavity preparation was also included in this report. Medical history was non-contributory for all patients.
Vital pulp tissue appeared at the exposure sites in all cases. All teeth responded positively to the electrical pulp testing. Treatment time after the injuries was between days 1 and 22. Table 1 summarizes individual patient data.
Table 1.
Cases and individual data.
| Case No | Patient No. and Gender | Age. | Tooth No. | Days after injury | Pulpotomy Outcome |
|---|---|---|---|---|---|
| 1 | 1-Girl | 9 | 19 | Mechanical exp. | Successful |
| 2 | 2-Boy | 8 | 8 | 22 | Successful |
| 3 | 3-Boy | 10 | 9 | 1 | Unsuccessful |
| 4 | 4-Boy | 10 | 8 | 14 | Successful |
| 5* | 5-Boy | 8 | 8 | 4 | Unsuccessful |
| 6* | 5-Boy | 8 | 9 | 4 | Successful |
Same patient
After completion of dental history records, all teeth were locally anesthetized and a rubber dam was positioned. Exposed pulp tissue was removed to the pulp canal orifice with a sterile diamond round bur in high-speed handpiece with copious saline irrigation. Hemorrhage was controlled first with 2 mL of saline irrigation and then by putting cotton pellets soaked with 5% NaOCl on pulp tissue for 1-minute. MTA was first placed with a spatula-shaped hand instrument and then wet cotton pellets were used to adapt it onto the exposed pulp area. Hemorrhage restarted during first placement of MTA in all cases. Wet cotton pellets were put on MTA; the dentist waited for at least 1-minute to stop hemorrhage and then another piece of new mixed MTA was inserted into the cavity. At layer of MTA at least 3 mm thick was placed over the exposed pulp tissue. The cavity was sealed with a wet cotton pellet and zinc-oxide eugenol cement (Kalzinol, De Trey, Dentsply, Konstanz, Germany). Three days later, the temporary fillings were removed and restored with a composite filling (Supreme, 3M ESPE, Dental Products, MN, USA).
Clinical observations at follow-up
One patient came to our clinic at the year 2006 (10 months after pulpotomy) with signs of acute apical periodontitis, and root canal treatment was performed (Tab. 1). There was severe discoloration in the crown. The remaining 5 patients were recalled at the years 2010 and 2011. Vitality tests and clinical diagnostic tests were applied, and periapical radiographs were also taken at the follow-ups. A periapical lesion around the right central incisor of patient #5 (the patient with 2 fractured incisors, Figures. 1, 2) was diagnosed at the 2010 follow-up radiographs. Root formation of this tooth was incomplete (Case 5, Table 1). No dentin bridge formation could be detected at the radiographs (Figure 2). The tooth exhibited no clinical signs of periapical inflammation. There was severe discoloration in the crowns of both incisors (Figure 3). An apexification procedure was followed using CH for 9 months by renewing it at 1 week, 1 month, 3 months and then every 3 months. At the 9-month visit, the tooth was filled with laterally condensed gutta-percha and a sealer (AH Plus; Dentsply De-Trey, Konstanz, Germany). The radiographic healing was assessed as uncertain at the 2012 follow-up (Figure 4). The tooth was showing no clinical signs or symptoms. All composite restorations on maxillary incisors of this patient were renewed at the 2012 follow-up (Figure 5).
Figure 1.

Preoperative radiograph of Case 5 (right central incisor) and Case 6 (left central incisor).
Figure 2.
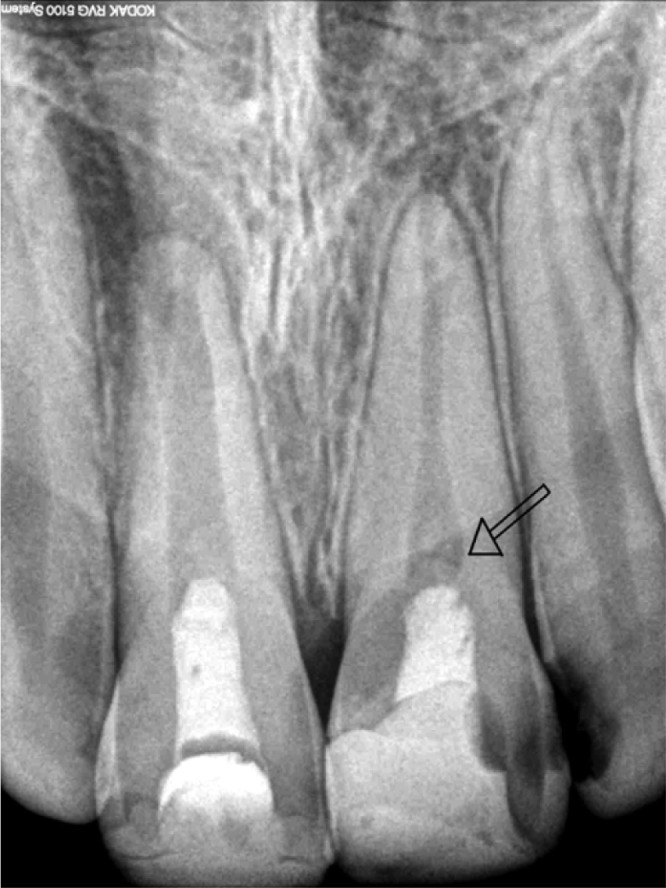
2010 follow-up radiograph of Case 5 and Case 6. Note presence of periapical lesion development around incomplete root formation and absence of dentin bridge formation beneath MTA of Case 5. Also, note complete root formation and evident dentin bridge formation beneath MTA (arrow) in Case 6.
Figure 3.

2012 Control radiograph of Case 5 after apexification and root canal treatment. Note the uncertain healing around Case 5.
Figure 4.
2012 Control radiograph of Case 5 after apexification and root canal treatment. Note the uncertain periapical healing around Case 5.
Figure 5.
Intraoral photograph after renewal of composite restorations of Cases 5 and 6 at 2012.
The remaining 4 teeth (including exposed molar and left central incisor of patient #5) were assessed as vital cases at the 2010 and 2011 follow-ups (mean time of follow-up was 55 months at 2011). There was no pulpal or periapical pain reported by the patients. Teeth did not respond consistently to pulp tests. No signs of periapical inflammatory changes were present clinically or radiographically in any of these cases. There were radiographic signs of apical root completion in these cases. Dentin bridge formations were detected clearly adjacent to MTA in 3 fractured maxillary incisors radiographically (Figures 6–8). There were no radiographic signs of pulp tissue obliteration and internal resorption in all 4 cases. Clinically, severe discoloration on crown segments was observed in all teeth. All composite restorations showed insufficient marginal adaptation and color changes on marginal enamel walls at the follow-ups.
Figure 6.

Preoperative radiograph of Case 2 (right central incisor). Note that the left central incisor had also crown fracture
Figure 8.
Intraoral photograph at 2011 follow-up of Case 2. Note severe discoloration in the right incisor.
DISCUSSION
Four immature teeth (including the molar case) treated with MTA were healthy after a mean time recall 55 months at the year 2011. In the control radiographs of these 4 cases, there was complete formation of root apices and visible dentin bridge formation in three incisor cases. These successful cases may indicate that MTA could induce pulp healing with dentin bridge formation and maintain root development.
There are several MTA pulpotomy case reports involving immature root formation in the literature.15–18 Karabucak et al15 observed that MTA pulpotomy was successful in two immature central incisors after 12 and 18 months of a clinical trial. El Meligy and Avery16 compared CH and MTA pulpotomies in 30 immature permanent teeth for one year. They found that all 15 MTA cases were successful, while 2 CH cases displayed periapical inflammation. Whitherspoon et al17 reported that 5 of 6 immature central maxillary incisors that were treated with MTA pulpotomy due to complicated crown fractures were diagnosed as healed after 13 to 15 months. Barrieshi-Nusair and Qudeimat18 reported that all 7 immature permanent cases treated with MTA pulpotomy were successful after 2 years. According to these clinical reports, MTA pulpotomy has a superior success rate in developing teeth with open apices.
In the present case report, 2 MTA pulpotomy cases were unsuccessful. The primary cause of pulp inflammation after vital pulp treatment is known as bacterial infection.21 Early contamination associated with treatment delay and later contamination with microleakage are the ways for bacteria to cause inflammation and necrosis in complicated crown fractures. There is no time limit for the pulpotomy of fractured immature cases when healthy pulp is clinically present.22 For unsuccessful Cases 3 and 6, the level of pulpotomy may not have been deep enough to reach healthy tissue for recovery. Materials used during pulpotomy, such as NaOCl and MTA, may have put additional pressure on pulp tissue in these cases. Pulpal hemorrhage may cause increased solubility in MTA before setting. The distribution of MTA particles during hemorrhage may also exceed the clean-up capacity of pulp tissue.
In all six cases, gray MTA caused severe discoloration in the tooth crowns. Such a complication following pulpotomy specifically in the anterior teeth should be accounted as a clinical failure of treatment. Discoloration effect of gray MTA as a pulpotomy agent in the crowns was shown and white MTA was developed because of this clinical complication. However, significant tooth discoloration was also reported after the use of white MTA.23 Belobrov and Parashos23 observed that most of the discoloration was inside white MTA and did not penetrate into dentin. They questioned and did not encourage the use of white MTA for vital therapy in the esthetic zone. Lenherr et al24 asserted that the infiltration of blood components into the porosities within MTA may be the prime cause of discoloration. The other possible reasons for tooth discoloration may be bismuth oxide, magnesium oxide and ferric oxide ingredients in MTA powder.25,26
Composite fillings also showed poor marginal adaptation, which may indicate the presence of coronal leakage around the fillings during service. Restorations should be replaced when a possible microleakage is diagnosed clinically, in order to maintain the vitality of pulpotomized cases.
CONCLUSION
MTA may be used as an alternative pulpotomy agent in immature teeth with pulp exposure to stimulate pulp healing with dentin bridge formation and complete root formation. But, discoloration following MTA pulpotomy appears as a major clinical complication.
Figure 7.

2011 follow-up radiograph of Case 2. Note complete root formation and evident dentin bridge formation beneath MTA (arrow).
REFERENCES
- 1.Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1979;4:232–237. doi: 10.1016/S0099-2399(78)80153-8. [DOI] [PubMed] [Google Scholar]
- 2.Çalışkan MK. Success of pulpotomy in the management of hyperplastic pulpitis. Int Endod J. 1993;26:142–148. doi: 10.1111/j.1365-2591.1993.tb00557.x. [DOI] [PubMed] [Google Scholar]
- 3.Cvek M. Endodontic management and the use of calcium hydroxide in traumatized permanent teeth. In: Andreasen JO, Andreasen FM, Andreasen L, editors. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Copenhagen: Blackwell Munksgaard; 2007. p. 605. [Google Scholar]
- 4.Schröder U. Effects of calcium hydroxide-containing pulp capping agents on pulp cell migration proliferation and differentiation. J Dent Res. 1985;64:541–548. doi: 10.1177/002203458506400407. [DOI] [PubMed] [Google Scholar]
- 5.Cvek M, Granath I, Cleaton-Jones P, Austin J. Hard tissue barrier formation in pulpotomized monkey teeth capped with cynoacrylate or calcium hydroxide for 10 and 60 minutes. J Dent Res. 1987;66:1166–1174. doi: 10.1177/00220345870660061501. [DOI] [PubMed] [Google Scholar]
- 6.Graham L, Cooper PR, Casssidy N, Nor JE, Sloan AJ, Smith AJ. The effect of calcium hydroxide on solubilization of bio-active dentin matrix components. Biomaterials. 2006;27:2865–2873. doi: 10.1016/j.biomaterials.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 7.Rashid F, Shiba H, Mizuno N, Mouri Y, Fujita T, Shinohara H, Ogawa T, Kawaguchi H, Kurihara H. The effect of extracellular calcium ion on gene expression of bone-related proteins in human pulp cells. J Endod. 2003;29:104–107. doi: 10.1097/00004770-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Ferracane JL, Cooper PR, Smith AJ. Can interaction of materials with the dentin-pulp complex contribute to dentin regeneration. Odontology. 2010;98:2–14. doi: 10.1007/s10266-009-0116-5. [DOI] [PubMed] [Google Scholar]
- 9.Yoshiba K, Yoshiba N, Nakamura H, Iwaku M, Ozawa H. Immunolocalization of fibronectin during reparative dentinogenesis in human teeth after pulp capping with calcium hydroxide. J Dent Res. 1996;75:1590–1597. doi: 10.1177/00220345960750081101. [DOI] [PubMed] [Google Scholar]
- 10.Chedella SCV, Berzins DW. A differential scanning calorimetry study of the setting reaction of MTA. Int Endod J. 2010;43:509–518. doi: 10.1111/j.1365-2591.2010.01708.x. [DOI] [PubMed] [Google Scholar]
- 11.Gondim E, Jr, Kim S, de Souza-Filho FJ. An investigation of microleakage from root-end fillings in ultrasonic retrograde cavities with or without finishing: a quantative analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:755–760. doi: 10.1016/j.tripleo.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Wu MK, Kontakiotis EG, Wesselink PR. Long-term seal provided by some root-end filling materials. J Endod. 1998;24:557–560. doi: 10.1016/S0099-2399(98)80077-0. [DOI] [PubMed] [Google Scholar]
- 13.Chacko V, Kurikose S. Human pupal response to mineral trioxide aggregate (MTA): a histologic study. J Clin Pediatr Dent. 2006;30:203–209. doi: 10.17796/jcpd.30.3.38h13g5p84651652. [DOI] [PubMed] [Google Scholar]
- 14.Iwamoto CE, Adachi E, Pameijer CH, Barnes D, Romberg EE, Jeffries S. Clinical and histological evaluation of white ProRoot MTA in direct pulp capping. Am J Dent. 2006;19:85–90. [PubMed] [Google Scholar]
- 15.Karabucak B, Li D, Lim J, Iqbal M. Vital pulp therapy with mineral trioxide aggregate. Dent Traumatol. 2005;21:240–243. doi: 10.1111/j.1600-9657.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 16.El Meligy OAS, Avery DR. Comparison of mineral trioxide aggregate and calcium hydroxide as pulptomy agents in young permanent teeth. (Apexogenesis) Pediatric Dent. 2006;28:399–406. [PubMed] [Google Scholar]
- 17.Witherspoon DE, Small JC, Gary ZH. Mineral trioxide aggregate pulpotomies: A case series outcomes assessment. J Am Dent Assoc. 2006;137:610–618. doi: 10.14219/jada.archive.2006.0256. [DOI] [PubMed] [Google Scholar]
- 18.Barrieshi-Nusair K, Qudeimat MA. A prospective clinical study of mineral trioxide aggregate for partial pulpotomy in cariously exposed permanent teeth. J Endod. 2006;32:731–735. doi: 10.1016/j.joen.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009;35:4–8. doi: 10.1111/j.1747-4477.2009.00166.x. [DOI] [PubMed] [Google Scholar]
- 20.Fridland M, Rosado R. MTA solubility: A long-term study. J Endod. 2005;31:376–379. doi: 10.1097/01.don.0000140566.97319.3e. [DOI] [PubMed] [Google Scholar]
- 21.Cox CF, Keall C, Keall H, Ostro E. Biocompability of surface-sealed dental materials against exposed pulps. J Prosthet Dent. 1987;57:1–8. doi: 10.1016/0022-3913(87)90104-1. [DOI] [PubMed] [Google Scholar]
- 22.Çalışkan MK, Savranoğlu S. Delayed partial pulpotomyin a midroot and complicated crown-root-fractured permanent incisor with hyperplastic pulpitis: A case report. J Endod. 2010;36:1250–1253. doi: 10.1016/j.joen.2010.03.036. [DOI] [PubMed] [Google Scholar]
- 23.Belobrov H, Parashos P. Treatment of tooth discoloration after the use of white mineral trioxide aggregate. J Endod. 2011;37:1017–1020. doi: 10.1016/j.joen.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krasti G. Tooth discoloration induced by endodonitc materials: a laboratory study. Int Endod J. 2012;45:942–949. doi: 10.1111/j.1365-2591.2012.02053.x. [DOI] [PubMed] [Google Scholar]
- 25.Steffen R, van Waes H. Understanding mineral trioxide aggregate/Portland cement: a review of literature and background factors. Eur Arch Pediatr Dent. 2009;10:93–97. doi: 10.1007/BF03321608. [DOI] [PubMed] [Google Scholar]
- 26.Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic treatment: A review of the literature. Dent Mater. 2008;24:149–164. doi: 10.1016/j.dental.2007.04.007. [DOI] [PubMed] [Google Scholar]





