To the Editor—Clostridium difficile infection (CDI) is a nosocomial infection that poses a challenge to infection control procedures, often from delays in testing [1]. A nurse-driven protocol may result in earlier identification and isolation of infected patients, leading to decreased transmission. It is a common “urban legend” among nursing staff that they can identify patients with CDI by the odor of their stool alone. Based on studies that used gas chromatography, this is biologically plausible—in 2004, Probert et al demonstrated the presence of unique volatile organic compounds (VOCs) in stool from patients with CDI [2]. Similarly, Garner et al demonstrated in 2007 that derived discriminant scores from VOC data had 100% predictive accuracy in distinguishing stool from patients who were asymptomatic, had ulcerative colitis, had Campylobacter jejuni infection, or had CDI [3].
In 2002, Johansen et al found that nurses on the wards were 84% sensitive and 77% specific in diagnosing CDI by stool odor [4]. Similarly, in 2007 Burdette et al found that nurses were 55% sensitive and 83% specific in diagnosing CDI [5]. A limitation of both studies, as pointed out in an accompanying commentary [6], is that the nurses were not blinded to any patient characteristics. Thus, one could not conclude that stool odor was the sole factor informing their assessments. We hypothesized that nurses can detect the presence of C. difficile in stool by odor alone in a controlled, laboratory setting.
Nurses were recruited from inpatient wards at our hospital. Our microbiology laboratory randomly set aside 5 positive and 5 negative stool samples based on results from 2-step testing (glutamate dehydrogenase/toxin enzyme immunoassay followed by polymerase chain reaction for discordant results) for C. difficile toxin (CDTOX) from patients with liquid stool. We asked nurses about their work experience and whether they believed they could detect C. difficile by odor. They were instructed to sniff each sample and record whether CDTOX positive stool was present. Fisher exact and Mann-Whitney tests were used to assess statistical significance.
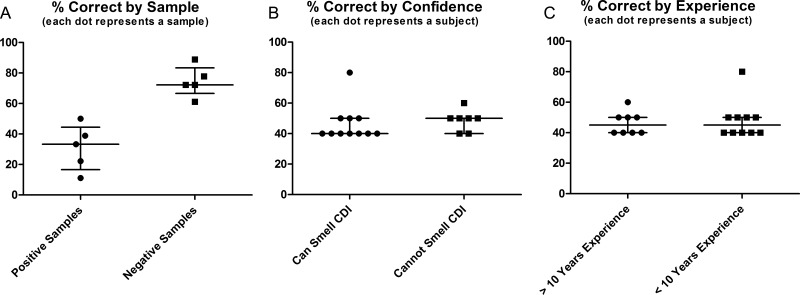
Eighteen nurses participated. Experience ranged from 1 to 30 years (8 with >10 years of experience). Eleven felt confident in their sniffing ability (61%). The median percentage correct was 45% (range, 40%–80%). CDTOX-positive samples elicited a lower percentage of correct answers than CDTOX-negative samples (Figure 1A; median, 31% vs 74%; P = .0119). No single individual performed better than chance (mean sensitivity/specificity = 0.26/0.69). Those with confidence in sniffing did not perform better than others (Figure 1B; median, 40% vs 50%; P = .2471) and more experienced nurses were no different from less experienced nurses (Figure 1C; both 45%; P = .8887).
Figure 1.
The percentage of correct responses, based on smell, regarding the presence of toxigenic Clostridium difficile in stool depending on sample type (A), confidence level (B), and experience (C); lines are at the median and interquartile range. Abbreviation: CDI, Clostridium difficile infection.
In this controlled laboratory setting, our nurses were unable to identify stool samples with C. difficile by odor, but CDTOX-negative samples elicited more correct answers than CDTOX-positive samples. More experience with nursing and confidence in sniffing ability did not improve performance. It is likely that our findings differ from prior studies owing to their inadequate blinding of nurses to patient and stool characteristics.
Notes
Acknowledgments. We thank the nursing staff from the University Hospital for their participation in this study. Parts of this work were presented at IDWeek 2012 on 18 October 2012 in San Diego, CA (poster number 326).
Financial support. This work was supported by the Department of Internal Medicine, University of Michigan Health Systems.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31:431–55. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 2.Probert CS, Jones PR, Ratcliffe NM. A novel method for rapidly diagnosing the causes of diarrhoea. Gut. 2004;53:58–61. doi: 10.1136/gut.53.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garner CE, Smith S, de Lacy Costello B, et al. Volatile organic compounds from feces and their potential for diagnosis of gastrointestinal disease. FASEB J. 2007;21:1675–88. doi: 10.1096/fj.06-6927com. [DOI] [PubMed] [Google Scholar]
- 4.Johansen A, Vasishta S, Edison P, Hosein I. Clostridium difficile associated diarrhoea: how good are nurses at identifying the disease? Age Ageing. 2002;31:487–8. doi: 10.1093/ageing/31.6.487-a. [DOI] [PubMed] [Google Scholar]
- 5.Burdette SD, Bernstein JM. Does the nose know? The odiferous diagnosis of Clostridium difficile–associated diarrhea. Clin Infect Dis. 2007;44:1142. doi: 10.1086/513033. [DOI] [PubMed] [Google Scholar]
- 6.Wilcox MH. Diagnosis of Clostridium difficile-associated diarrhea and odor. Clin Infect Dis. 2007;45:1110. doi: 10.1086/521944. [DOI] [PubMed] [Google Scholar]