Abstract
Emerging research has revealed that subjective social status (SSS), or how people perceive their position in the social hierarchy, is significantly associated with multiple health outcomes. Yet few studies have examined how this association is affected by the person or group to whom respondents are comparing themselves. While previous studies have used distal referent groups when assessing SSS, scholars have suggested that individuals may prefer to make comparisons to those who share similar characteristics to themselves. Overall, there has been little empirical analysis assessing the health impact of comparing oneself to one referent group over another. Using a diverse, national U.S. sample (n=3,644), this study explores whether the relationship between SSS and self-rated health is sensitive to the referent used for social comparison. Data are from respondents who completed the Styles mail surveys and who have assessed their SSS against four referents: others in American society, others of the same race or ethnicity, neighbors, and parents at the same age. Self-rated health was the dependent variable, while we controlled for household income, education, home ownership, race/ethnicity, and other covariates. In logistic regression models, SSS using each of the four referents was significantly associated with self-rated health, but the model using the referent of others in American society had the strongest association with self-rated health and was the most parsimonious. Findings validate previous studies which typically have used a more distal referent such as others in American society in exploring the SSS-health relationship. However, future work should explore whether this referent is salient to diverse population groups when making social comparisons. Researchers may also want to consider using SSS as an additional status measure since it may capture more subtle differences in the status hierarchy than traditional economic measures.
Introduction
Social status is a multidimensional concept whose measurement has been the topic of much debate. Scholars have suggested that social status indicators are comprised of different types of measures, some assessing actual economic resources and others capturing prestige-related characteristics (Krieger, Williams, & Moss, 1997; Oakes & Rossi, 2003; Wilkinson, 1997). Health status has been found to be strongly associated with economic measures such as household income or wealth as well as with rank-related indicators such as occupational prestige (Lynch & Kaplan, 2000; Wilkinson, 1997). More recently, a growing number of studies has also indicated that subjective social status (SSS)—how people perceive their position in the social hierarchy—is significantly associated with health status, independently of objective economic indicators (Adler, Epel, Castellazzo, & Ichovics, 2000; Ostrove, Adler, Kupperman, & Washington, 2000).
The association between SSS and health has been quite consistent when the outcome is a global self-rated health measure. Self-related health is considered a robust indicator of physical health status and a strong predictor of subsequent mortality (Idler & Benyamini, 1997; Singh-Manoux, Martikainen, Ferrie, Zins, Marmot, & Goldberg, 2006), although several validation studies have found racial/ethnic differences in self-rated health perceptions among various cultural groups both within the U.S. (Borrell & Dallo, 2007; McGee., Liao, Cao, & Cooper, 1999; Ren & Amick, 1996) and in other countries (Agyemang, Denktas, Buijnzeels, & Foets, 2006; Jylhä, Guralnik, Ferruci, Jokela, & Heikkinen, 1998). While some questions have emerged regarding the use of self-rated health as a health indicator across cultures, higher SSS has been consistently found to be significantly associated with better self-rated health in several different population sub-groups, including White healthy women (Adler et al., 2000), White and Chinese-American pregnant women (Ostrove et al., 2000), British civil servants (Singh-Manoux, Adler, & Marmot, 2003), Hispanic adults in Texas (Franzini & Fernandez-Esquer, 2006), rural Chinese residents (Yip & Adler, 2005), and Taiwanese senior citizens (Hu, Adler, Goldman, Weinstein, & Seeman, 2005). In some cases, SSS has been shown to have a stronger association with health than objective social status (OSS) measures. In a national sample of American adults, a multivariable analysis of cross-sectional data showed that SSS was a stronger independent predictor of self-rated health than traditional economic indicators (Operario, Adler, & Williams, 2004), while the longitudinal Whitehall-II study of British civil servants found that SSS was a better predictor of health status over time than income or education (Singh-Manoux, Marmot, & Adler, 2005).
SSS and self-rated health
It has been suggested that SSS captures the averaging of standard status indicators. While the measure is associated with psychological factors such as negative affect, it is thought that these factors mediate, rather than confound, the relationship between SSS and health (Operario, Adler, & Williams, 2004; Singh-Manoux, Adler, & Marmot, 2003). Similarly, the measure of self-rated health is correlated with psychological factors, yet it is still considered a strong indicator of subsequent morbidity and mortality. Although SSS and self-rated health are both subjective measures, previous research has concluded that their association is not driven by common method bias.
Since psychological factors are hypothesized as being significant mediators in the pathway of how SSS may affect one’s health status, research has begun to explore the mechanisms underlying this relationship. Discussions on the psychological processes involved in the social status-health relationship have tended to focus on the relative deprivation perceived by people who are lower on the social hierarchy (Baum, Garofalo, & Yalli, 1999; Wilkinson, 1999) which may affect health via stress-related processes (Kubzansky & Kawachi, 2000; Wilkinson, 1999). Evidence suggests that the negative psychological effects associated with low social status—such as chronic stress, anxiety, and negative emotions—can lead to the adoption of harmful coping behaviors such as smoking and drug use and can trigger a number of harmful physiological changes that can increase the risk of coronary heart disease, depression, the common cold, and a number of other conditions (Adler et al., 2000; Baum, Garofalo, & Yalli, 1999; Schnittker & McLeod, 2005).
However, it remains unclear whether the relationship between SSS and health status is consistent across populations, specifically among racial/ethnic minority groups. Relevant studies with large samples either have ignored race/ethnicity entirely or controlled for it in analyses. The few studies that have focused on racial/ethnic differences in the relationship between SSS and health have been with small samples and have generally yielded insignificant results for Blacks and mixed results for Hispanics. In models adjusting for OSS indicators, no significant relationship was found between SSS and self-rated health among Black and Hispanic pregnant women (Ostrove et al., 2000) or Black men (Adler, Singh-Manoux, Schwartz, Stewart, Matthews, & Marmot, 2008). However, Franzini & Fernandez-Esquer (2006) did find that SSS was significantly associated with self-rated health among low-income Hispanic adults in Texas.
Referent group sensitivity
There is also scant research empirically documenting the extent to which the relationship between SSS and health might be sensitive to the referent group used for social comparison. Most public health studies examining SSS have used a more distal referent when asking respondents how they rate themselves within the social hierarchy. Typically, research has explored the relationship between SSS and health by using the referent group of others “in [our] society” (Ostrove et al., 2000; Singh-Manoux, Adler, & Marmot, 2003) or by asking respondents to indicate the occupational group (e.g., manager, foreman) or social class (e.g., lower class, working class, middle class) of which they consider themselves to be a member (MacLeod, Smith, Metcalfe, & Hart, 2005; Veenstra, 2005). While most public health studies examining SSS have used a more distal referent group for SSS measures, social psychologists have suggested that referent choice may be situational and comprise of more proximal referents. According to this line of research, referent choice is likely to vary with the respondents’ personal characteristics, including group identification, demographic characteristics, and performance-related abilities (Wood & Taylor, 1991). Specifically, individuals in low status groups, such as racial/ethnic minorities, may be more likely to make comparisons with referents in their own group or to other low status groups (Leach & Smith, 2006; Suls & Wills, 1991), although the evidence in this area has not been entirely consistent (Guimond, 2006; Kulik & Ambrose, 1992; Leach & Smith, 2006). People may also prefer to make temporal comparisons, evaluating their present circumstances to themselves or others in the past (Guimond, 2006; Suls & Wills, 1991).
Referent salience is important because SSS ratings by racial/ethnic group appear to be differentially sensitive to the referent group used in the comparison. In a multiethnic sample, Blacks and Hispanics were both more likely than Whites to perceive their income level to be lower than their friends and relatives, while only Blacks were more likely than Whites to consider their incomes lower than the national norm and those with the same education (Stiles & Kaplan, 2004). Among Cherokee and White Appalachian youth, Whites surprisingly rated their SSS lower than Cherokee youth when compared to the national norm, but when the referent was their peer group, White youth rated their peer SSS higher than Cherokee youth did (Brown, Adler, Worthman, Copeland, Costello, & Angold, 2008).
With few exceptions, there has been little empirical analysis assessing the health impact of comparing oneself to one referent group over another. Siahpush, Borland, Taylor, Singh, Ansari, & Serraglio (2006) reported that, after adjusting for objective economic measures, SSS with the referent group of “others in your local area” was significantly associated with smoking status among Australians in a metropolitan sample. Analyses from a national Canadian survey found that SSS with the referent group “parents at the same age” was not significantly related to self-rated health, yet using the more distal referent of “other Canadians” for social comparison yielded a significant association between SSS and health in adjusted models (Dunn, Veenstra, & Ross, 2006). However, for the temporal comparison, this Canadian study asked whether, in general, “people your age are financially better off…as their parents at the same age” rather than specifically asking respondents about their own status compared to their own parents, a measurement limitation the authors note as possibly affecting their findings (Dunn, Veenstra, & Ross, 2006). In their study of low-income Hispanic adults, Franzini & Fernandez-Esquer (2006) asked participants to whom they were comparing themselves when they responded to their SSS survey question. Nearly half the sample reported using the referent group of Mexicans in the U.S., while others compared themselves to people in the U.S./Anglos and to Mexicans in Mexico. While SSS was significantly related to self-rated health in this study, analyses assessing the relationship between SSS comparisons to alternative referent groups and health status were not reported (Franzini & Fernandez-Esquer, 2006).
In this paper, we aim to provide a greater understanding of whether the relationship between SSS and self-rated health is sensitive to the referent group used for social comparison as well as to the race/ethnicity of the respondent. We surveyed a national sample of American adults who provided their SSS ratings, by comparing themselves to the following referent groups: others in American society, others of their same race/ethnicity, their neighbors, and their parents when they were their age. We assessed the relationship between SSS with these alternative reference groups and self-rated health and hypothesized that the magnitude of the relationship between SSS and self-rated health would be strongest when respondents used more proximal referents, e.g., others of the same race/ethnicity or neighbors. Additionally, we hypothesized that there would be significant racial/ethnic differences in the relationship between SSS and self-rated health, particularly when using the distal referent group of others in American society.
Methods
Data collection
Data for this study are from the ConsumerStyles and HealthStyles annual surveys conducted by Porter Novelli using the Synovate, Inc. consumer mail panel. In May-June 2007, a stratified random sample of 20,000 individuals was selected from the panel and mailed the ConsumerStyles survey. The sample was stratified on region, household income, population density, age, and household size and oversampled for low income and minority participants. A total of 11,758 people completed the 2007 ConsumerStyles survey, yielding an overall response rate of 58.8%, which is consistent with response rates of other national mail panel surveys (Weber et al., 2007; Wolff et al., 2010). In July-August 2007, the HealthStyles survey was administered to half of the households that returned the ConsumerStyles surveys (n=6,600). There was a 66.6% response rate for the HealthStyles survey (n=4,398). This study’s final sample (n=3,644) was restricted to those who completed both surveys, self-identified as White, Black, or Hispanic, and provided data on self-rated health and key predictor variables. The Harvard School of Public Health’s Human Subjects Committee approved this study’s protocol.
Measures
Self-rated health
The dependent variable in this study, self-rated health, was assessed using a standard question “In general, would you say your health is…?” with the response options as: ‘excellent’, ‘very good’, ‘good’, ‘fair’, and ‘poor’. Self-rated health was dichotomized for most analyses as poor or fair health=1; excellent, very good or good health=0, consistent with previous health studies (e.g., Idler & Benyamini, 1997; Kennedy et al., 1998; Subramanian, Kim, & Kawachi, 2005).
Subjective social status (SSS)
The measure for SSS, the independent variable of special interest, was similar to that used in previously published studies (Dunn, Veenstra, & Ross, 2006; Siahpush et al., 2006; Stiles & Kaplan, 2004; Stiles, Liu, & Kaplan, 2000; Tropp & Wright, 1999; Zagefka & Brown, 2005). To assess SSS, respondents were asked to: “Please think about success in life. Some people are better off—they have more money, more education, and better jobs. Other people are worse off—they have less money, less education, and worse jobs.” The question then asked participants to check a box indicating whether they are ‘a lot worse off, ‘somewhat worse off, ‘about the same’, ‘somewhat better off, or ‘a lot better off than the following: 1) ‘Others in American society’, 2) ‘Others of your same race or ethnicity’, 3) ‘Your neighbors’, and 4) ‘Your parents when they were your age’. This measure was selected because it efficiently allowed respondents to rate their SSS against different referents within the same question. Also, whereas other measures consider SSS as a continuous variable so researchers can analyze the SSS-health as a linear relationship, the measure used in this study views SSS as a nominal variable for making relative comparisons to various referents, so that analyses can further explore the pattern of this relationship.
Race/ethnicity
Two separate questions were used to assess respondents’ race/ethnicity. The first question asked respondents to indicate their race, with options including ‘White’; ‘Black/African American’; ‘Asian’; ‘American Indian/Alaskan Native’; ‘Native Hawaiian/Pacific Islander’; and ‘Other’. The second question asked respondents whether or not they were of Spanish or Hispanic ethnicity. For this study’s analyses, race/ethnicity includes the categories of White, non-Hispanic; Black/African American, non-Hispanic; and Hispanic (any race). Respondents were considered White or Black if they self-identified as such but reported that they were not Hispanic on the ethnicity question. Hispanic respondents included all individuals who indicated that they were of Spanish or Hispanic origin, regardless of race.
Objective social status (OSS)
Three variables—household income, education, and home ownership—were assessed as OSS indicators.
Household income
Respondents were provided 27 income categories and asked to check off the category that best matched their total annual household income of all household members before taxes. Based on the distribution of responses, household income was then collapsed into seven categories (under $10,000; $10,000–$24,999; $25,000–$39,999; $40,000–$59,999; $60,000–$74,999; $75,000–$99,999; $100,000 or more).
Education
Survey respondents indicated the highest level of education they achieved, by marking one of seven categories. Responses were later collapsed into five main categories for analyses (no high school degree; high school graduate; attended some college; college graduate; post-graduate degree (including master’s, doctorate, or professional degree)).
Home ownership
Home ownership was self-reported and captured by three categories (‘owned by you or someone else in your household’; ‘rented for cash rent’; ‘occupied without payment of rent’). Responses were dichotomized for analyses as: 1=do not own; 0=owned by you or someone else in your household.
Mental health conditions
Mental health conditions were included as covariates in multivariable models and assessed with five variables. Respondents were asked if ‘they have or have had in the past year’: ‘depression’, ‘bipolar disorder’, and ‘anxiety disorder’. Each condition was treated as a dichotomous variable (1=yes; 0=no). Mental health conditions were controlled for in analyses to minimize confounding by any negative psychological factors resulting from these specific conditions.
Physical health conditions and risk factors
Physical health conditions and risk factors were included in the multivariable models to control for major comorbidities and risk factors that are strongly associated with self-rated health (DeSalvo et al., 2006; Idler & Benyamini, 1997). These conditions and risk factors were assessed with six outcomes. Respondents were asked if ‘they have or have had in the past year’: ‘diabetes’, ‘skin cancer’, ‘other cancer’, ‘high cholesterol’, and ‘high blood pressure’. Each condition was treated as a dichotomous variable (1=yes; 0=no). Body mass index (BMI) (continuous, based on respondents’ self-reported height and weight) was also included as a risk factor.
Other covariates
Several other sociodemographic characteristics were included in analyses as covariates. These included gender, age (continuous in years), household size (categorized as one person; two people; three people; four people; five or more people), marital status (categorized as married; widowed; divorced; separated; never married; domestic partnership), and health insurance status (dichotomized as yes/no).
Statistical Analyses
Statistical analyses were conducted with SAS software version 9.1 (SAS Institute Inc., Cary, NC), and level of significance was set at p=0.05. Correlations, chi-square tests, and T-tests were used for bivariate analyses as appropriate. For rank ordered variables such as education and income, Spearman rank correlation analyses were conducted which allowed for less sensitivity to non-normal distributions. To build the multivariable models, logistic regression was used since the outcome variable of self-rated health was dichotomized. Five separate multivariable models were examined, with Models 1–4 each including an SSS predictor with a different referent group, and Model 5 modeling all the SSS measures simultaneously to identify whether comparisons to the specific referent groups were significantly related to self-rated health independently of the other SSS measures. Theoretically relevant covariates were included in all adjusted analyses. To examine effect modification by race/ethnicity in the relationship between SSS and self-rated health, interaction terms (race/ethnicity*SSS) were entered into the models using the CLASS statement in SAS, which indicates that these specific variables are categorical rather than continuous. Results from the models with the interaction terms are discussed in the paper and presented in the electronic appendix.
We tested whether the overall interaction term in each model was significant. Sampling weights were applied in all analyses to take into account the survey’s stratified random sampling method and to achieve additional representativeness. Sampling weights were based on the U.S Census Bureau’s 2006 Current Population Survey and factored in gender, age, income, race, and household size.
Results
Table 1 presents the descriptive characteristics of the entire sample and the bivariate analyses for these characteristics by self-rated health. Among survey respondents, 15.3% reported that they would describe their health as poor or fair. Income, education, home ownership, marital status, and age were all significantly associated with poor/fair health (p<0.05). There were no differences by race/ethnicity or gender in the percentage of respondents who reported poor/fair health. The distribution of responses for the various SSS ratings is provided in Table 2. In bivariate analyses by self-rated health, SSS with each of the four referent groups was significantly associated with poor/fair health.
Table 1.
Sociodemographic characteristics of the sample and bivariate associations with self-rated health (n=3644)
| Total* | Self-rated health* | ||||
|---|---|---|---|---|---|
| Weighted | Good/very good/excellent health |
Poor/fair health |
P-value | ||
| n | (%) | (%) | (%) | ||
| Overall | n=3600 (weighted) |
100 | 84.7 | 15.3 | |
| Race/ethnicity | |||||
| White, non-Hispanic | 2777 | 77.1 | 77.6 | 74.4 | 0.18 |
| Black, non-Hispanic | 410 | 11.4 | 11.3 | 11.3 | |
| Hispanic | 414 | 11.5 | 11.1 | 13.6 | |
| Gender | |||||
| Male | 1708 | 47.5 | 47.6 | 46.6 | 0.66 |
| Female | 1892 | 52.5 | 52.4 | 53.4 | |
| Marital status | |||||
| Married | 2109 | 58.6 | 61.4 | 42.9 | |
| Widowed | 259 | 7.2 | 6.2 | 12.7 | <0.0001 |
| Divorced | 380 | 10.6 | 9.4 | 17.1 | |
| Separated | 51 | 1.4 | 1.3 | 2.0 | |
| Never married | 661 | 18.4 | 17.7 | 21.9 | |
| Domestic partnership | 141 | 3.9 | 4.0 | 3.4 | |
| Income | |||||
| Under $10,000 | 342 | 9.5 | 7.1 | 23.1 | |
| $10,000–$24,999 | 570 | 15.8 | 13.6 | 28.3 | <0.0001 |
| $25,000–$39,999 | 655 | 18.2 | 18.5 | 16.4 | |
| $40,000–$59,999 | 668 | 18.6 | 19.2 | 15.0 | |
| $60,000–$74,999 | 316 | 8.8 | 9.5 | 4.8 | |
| $75,000–$99,999 | 541 | 15.0 | 16.6 | 6.4 | |
| $100,000 or more | 508 | 14.1 | 15.6 | 6.1 | |
| Education | |||||
| No high school degree | 194 | 5.4 | 4.2 | 11.8 | |
| High school graduate | 950 | 26.4 | 25.0 | 34.0 | <0.0001 |
| Some college | 1326 | 36.8 | 36.8 | 36.8 | |
| College graduate | 662 | 18.4 | 19.8 | 10.6 | |
| Post-graduate degree | 468 | 13.0 | 14.1 | 6.7 | |
| Home ownership | |||||
| Does not own residence | 842 | 23.4 | 20.7 | 38.5 | <0.0001 |
| Owns residence | 2758 | 76.6 | 79.4 | 61.5 | |
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Age (in years) | 48.3 (16.6) | 47.7 (16.4) | 51.5 (17.2) | <0.0001 | |
Bolded values are statistically significant, p<0.05.
Weighted numbers and frequencies reported for all sociodemographic characteristics. Weighted numbers may not exactly equal weighted sample size and weighted frequencies may not exactly equal 100% due to rounding.
Table 2.
Distribution of subjective social status (SSS) responses of the sample and bivariate associations with self-rated health (n=3644)
| Total* | Self-rated health* | ||||
|---|---|---|---|---|---|
| Weighted | Good/very good/excellent health |
Poor/fair health |
P-value | ||
| n | (%) | (%) | (%) | ||
| Overall | n=3600 (weighted) |
100 | 84.7 | 15.3 | |
| SSS compared to | |||||
| Others in American society | |||||
| A lot worse off | 114 | 3.2 | 1.9 | 10.0 | |
| Somewhat worse off | 421 | 11.7 | 10.0 | 21.3 | <0.0001 |
| Same as | 1520 | 42.2 | 42.3 | 41.9 | |
| Somewhat better off | 1233 | 34.3 | 36.4 | 22.4 | |
| A lot better off | 311 | 8.6 | 9.4 | 4.4 | |
|
Others of the same race/ethnicity |
|||||
| A lot worse off | 97 | 2.7 | 2.0 | 6.5 | |
| Somewhat worse off | 489 | 13.6 | 12.2 | 21.6 | <0.0001 |
| Same as | 1692 | 47.0 | 46.5 | 49.6 | |
| Somewhat better off | 1096 | 30.5 | 32.5 | 19.3 | |
| A lot better off | 226 | 6.3 | 6.9 | 3.0 | |
| Your neighbors | |||||
| A lot worse off | 75 | 2.1 | 1.5 | 5.5 | |
| Somewhat worse off | 436 | 12.1 | 10.9 | 18.7 | <0.0001 |
| Same as | 2079 | 57.8 | 58.4 | 54.2 | |
| Somewhat better off | 832 | 23.1 | 24.0 | 18.3 | |
| A lot better off | 178 | 4.9 | 5.2 | 3.3 | |
|
Your parents when they were your age |
|||||
| A lot worse off | 171 | 4.8 | 3.6 | 11.1 | |
| Somewhat worse off | 434 | 12.0 | 11.2 | 16.5 | <0.0001 |
| Same as | 857 | 23.8 | 23.2 | 27.3 | |
| Somewhat better off | 1312 | 36.4 | 37.5 | 30.5 | |
| A lot better off | 827 | 23.0 | 24.5 | 14.7 | |
Bolded values are statistically significant, p<0.05.
Weighted numbers and frequencies reported for all sociodemographic characteristics. Weighted numbers may not exactly equal weighted sample size and weighted frequencies may not exactly equal 100% due to rounding.
Table 3 shows the bivariate correlations for SSS, OSS, self-rated health, and mental and physical health conditions. All measures of SSS, OSS, and self-rated health were significantly correlated with each other (p<0.001). Among the various SSS measures, correlation was strongest between the measure of SSS compared with ‘others of the same race/ethnicity’ and SSS compared with ‘others of the same race/ethnicity’ (r=0.77). The correlation between the SSS measures using the referent of ‘your neighbors’ and ‘your parents at the same age’ was the weakest (r=0.35) among all the SSS measures, but was still significant. Additionally, OSS indicators were significantly correlated to each other, with income and education having the strongest correlation (r=0.42), and each OSS indicator was significantly correlated to the various SSS measures and to self-rated health. All the mental health conditions were also correlated with the SSS, OSS, and self-rated health measures (p<0.001), while BMI was the only physical health condition that was consistently significant in the bivariate correlations.
Table 3.
Correlation matrix of subjective social status (SSS), objective social status (OSS), self-rated health, and mental and physical health conditions (n=3644)
| SSS compared to | OSS measures | SRH | ||||||
|---|---|---|---|---|---|---|---|---|
| Others in American society |
Others of same race/ethnicity |
Your neighbors |
Your parents when they were your age |
Income | Education | Home ownership |
Self- rated health |
|
| SSS compared to1 | ||||||||
| Others in American society | 1 | |||||||
| Others of same race/ethnicity | 0.77* | 1 | ||||||
| Your neighbors | 0.51* | 0.53* | 1 | |||||
| Your parents when they were your age | 0.42* | 0.46* | 0.35* | 1 | ||||
| OSS measures2 | ||||||||
| Income | 0.37* | 0.32* | 0.21* | 0.25* | 1 | |||
| Education | 0.38* | 0.25* | 0.16* | 0.14* | 0.42* | 1 | ||
| Home ownership | 0.18* | 0.14* | 0.08* | 0.17* | 0.38* | 0.16* | 1 | |
| Self-rated health3 | 0.26* | 0.22* | 0.16* | 0.18* | 0.32* | 0.23* | 0.16* | 1 |
| Mental health conditions2,4 | ||||||||
| Depression | −0.18* | −0.16* | −0.13* | −0.13* | −0.16* | −0.10* | −0.11* | −0.23* |
| Bipolar disorder | −0.09* | −0.08* | −0.04** | −0.10* | −0.11* | −0.06* | −0.10* | −0.11* |
| Anxiety disorder | −010* | −0.12* | −0.08* | −0.11* | −0.10* | −0.09* | −0.11* | −0.14* |
| Physical health conditions2,4 | ||||||||
| Body mass index (BMI)1 | −0.12* | −0.12* | −0.06** | −0.12* | −0.14* | −0.10* | −0.10* | −0.30* |
| Diabetes | −0.05* | −0.03 | −0.01 | −0.01 | −0.14* | −0.04*** | 0.05** | −0.28* |
| Cancer | 0.02 | 0.02 | 0.01 | 0.01 | −0.02 | −0.003 | −0.02 | −0.08* |
| High blood pressure | −0.02 | 0.003 | 0.003 | 0.01 | −0.15* | −0.10* | −0.03 | −0.25* |
| High cholesterol | −0.01 | 0.01 | −0.01 | 0.03 | −0.06* | −0.04** | −0.001 | −0.20* |
Correlations are significant at:
p<0.001;
p<0.01;
p<0.05
Pearson correlation used for correlations of SSS measures with each other, self-rated health, and BMI.
Spearman rank correlation used for all correlations involving OSS measures and mental and physical health conditions (except BMI).
5-point scale for self-rated health: 1=poor, 2=fair, 3=good, 4=very good, 5=excellent
All mental and health conditions except BMI are dichotomous, 0=do not have or have not had the condition in the past year; 1= have or have not had the condition in the past year
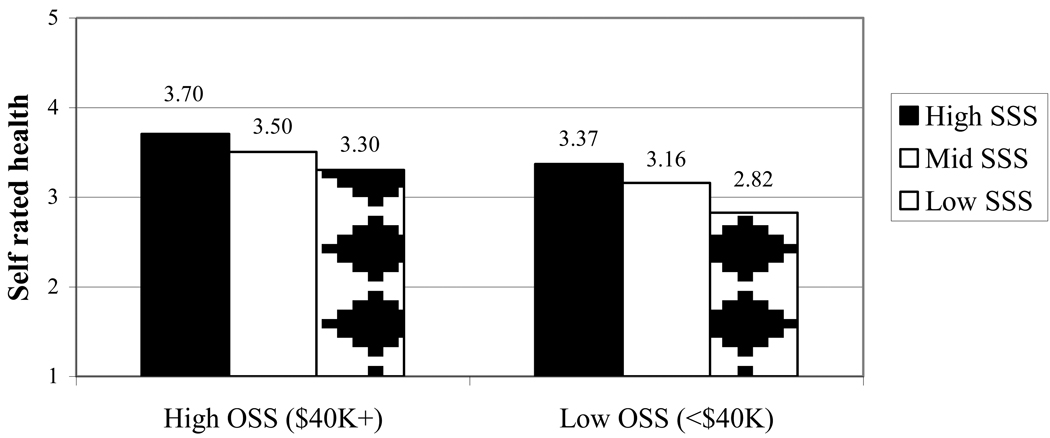
While SSS and OSS measures were strongly correlated with each other, there were differences in self-rated health scores by SSS rating among individuals with high and low objective status, where objective status was measured by income. Figure 1 shows the mean self-rated health response among those with high objective status (household income of $40,000 (median income) or over) and low objective status (household income of under $40,000) grouped by whether their SSS was high (somewhat/a lot better off), mid (same as), or low (somewhat/a lot worse off) compared to others in American society. For example, among those with an income of under $40,000, the mean self-rated health score was 3.37 for those perceiving their own status as higher than others in American society, whereas the mean health score was 2.82 among individuals of the same income group but who perceived themselves as lower status (p<0.0001). Similarly, among those with higher household income ($40,000 or more), individuals with higher perceived status than others in American society had significantly higher mean self-rated health scores than those with lower perceived status (3.70 vs. 3.30, p<0.0001).
Figure 1. Mean self-rated health scores by OSS (income) and SSS with the referent of others in American society.
5-point scale for self-rated health: 1=poor, 2=fair, 3=good, 4=very good, 5=excellent
Table 4 presents the logistic regression results of the multivariable associations between SSS and self-rated health. Results for Models 1–4 indicate that there were significant associations between SSS using each of the referent groups and reporting poor/fair health. While odds ratios from the different models cannot be statistically compared, qualitatively it appears that SSS with the referent of others in American society had a stronger relationship to self-rated health than SSS using the other referent groups. For example in Model 1, those who indicated that they were a lot worse off had significantly greater odds (OR:3.44, 95%CI:2.11–5.50)—and those who reported they were a lot better off had significantly lower odds (OR:0.55, 95%CI:0.34–0.91)—of reporting poor/fair health than those who considered themselves the same as others in American society. In Model 5, which mutually controls for SSS with all four referent groups, SSS was significantly associated with poor/fair health only when the referent group of others in American society was used for social comparison. In this model, the association between SSS with the other three referents and reporting poor/fair health was no longer significant.
Table 4.
Predictors of poor/fair health: multiple logistic regression models (n=3644)
| Model 1* | Model 2* | Model 3* | Model 4* | Model 5* | |
|---|---|---|---|---|---|
|
SSS compared to others in American society |
|||||
| A lot worse off | 3.44 (2.11–5.60) | - | - | - | 4.29 (2.18–8.41) |
| Somewhat worse off | 1.33 (0.98–1.80) | - | - | - | 1.48 (1.00–2.18) |
| Same as | Ref | - | - | - | Ref |
| Somewhat better off | 0.82 (0.63–1.08) | - | - | - | 0.97 (0.69–1.36) |
| A lot better off | 0.55 (0.34–0.91) | - | - | - | 0.84 (0.43–1.65) |
|
SSS compared to others of the same race/ethnicity |
|||||
| A lot worse off | - | 1.98 (1.16–3.39) | - | - | 0.54 (0.24–1.18) |
| Somewhat worse off | - | 1.18 (0.88–1.58) | - | - | 0.78 (0.53–1.17) |
| Same as | - | Ref | - | - | Ref |
| Somewhat better off | - | 0.74 (0.56–0.98) | - | - | 0.79 (0.55–1.13) |
| A lot better off | - | 0.45 (0.25–0.79) | - | - | 0.56 (0.26–1.21) |
| SSS compared to your neighbors | |||||
| A lot worse off | - | - | 2.09 (1.18–3.73) | - | 0.99 (0.49–2.00) |
| Somewhat worse off | - | - | 1.11 (0.81–1.51) | - | 0.89 (0.62–1.29) |
| Same as | - | - | Ref | - | Ref |
| Somewhat better off | - | - | 0.89 (0.68–1.18) | - | 1.04 (0.77–1.40) |
| A lot better off | - | - | 0.63 (0.36–1.12) | - | 0.97 (0.50–1.88) |
|
SSS compared to your parents when they were your age |
|||||
| A lot worse off | - | - | - | 1.86 (1.21–2.88) | 1.58 (0.97–2.57) |
| Somewhat worse off | - | - | - | 1.19 (0.84–1.67) | 1.15 (0.81–1.65) |
| Same as | - | - | - | Ref | Ref |
| Somewhat better off | - | - | - | 0.85 (0.64–1.12) | 0.87 (0.65–1.15) |
| A lot better off | - | - | - | 0.71 (0.51–1.00) | 0.83 (0.58–1.19) |
| Race/ethnicity | 0.76 (0.54–1.07) | 0.81 (0.57–1.14) | 0.76 (0.54–1.08) | 0.79 (0.56–1.11) | 0.78 (0.55–1.11) |
| Black | |||||
| Hispanic | 0.87 (0.62–1.21) | 0.88 (0.63–1.23) | 0.86 (0.62–1.20) | 0.86 (0.62–1.19) | 0.88 (0.63–1.23) |
| White | Ref | Ref | Ref | Ref | Ref |
| Household income | |||||
| Under $10,000 | 1.54 (1.01–2.36) | 1.65 (1.08–2.51) | 1.68 (1.11–2.56) | 1.63 (1.07–2.48) | 1.49 (0.97–2.29) |
| $10,000-$24,999 | 1.27 (0.89–1.82) | 1.32 (0.93–1.89) | 1.31 (0.92–1.87) | 1.28 (0.89–1.83) | 1.26 (0.88–1.81) |
| $25,000-$39,999 | 0.86 (0.60–1.22) | 0.88 (0.61–1.26) | 0.86 (0.60–1.23) | 0.85 (0.59–1.12) | 0.88 (0.61–1.26) |
| $40,000-$59,999 | Ref | Ref | Ref | Ref | Ref |
| $60,000-$74,999 | 0.68 (0.41–1.13) | 0.69 (0.42–1.14) | 0.66 (0.40–1.10) | 0.67 (0.40–1.10) | 0.68 (0.41–1.13) |
| $75,000-$99,999 | 0.60 (0.38–0.93) | 0.59 (0.38–0.93) | 0.57 (0.36–0.89) | 0.57 (0.36–0.89) | 0.59 (0.38–0.93) |
| $100,000 or more | 0.87 (0.54–1.38) | 0.88 (0.55–1.40) | 0.79 (0.50–1.26) | 0.80 (0.51–1.28) | 0.89 (0.56–1.43) |
| Education | |||||
| No HS degree | 1.79 (1.19–2.71) | 1.89 (1.26–2.84) | 1.92 (1.28–2.87) | 1.90 (1.27–2.85) | 1.76 (1.16–2.68) |
| HS graduate | 1.23 (0.95–1.60) | 1.22 (0.94–1.59) | 1.25 (0.97–1.62) | 1.27 (0.98–1.65) | 1.26 (0.97–1.64) |
| Some college | Ref | Ref | Ref | Ref | Ref |
| College graduate | 0.93 (0.66–1.33) | 0.94 (0.66–1.33) | 0.91 (0.64–1.29) | 0.89 (0.63–1.27) | 0.95 (0.66–1.35) |
| Post-grad degree | 0.69 (0.45–1.06) | 0.69 (0.45–1.06) | 0.65 (0.42–1.00) | 0.64 (0.42–0.99) | 0.69 (0.45–1.07) |
| Home ownership | |||||
| Does not own residence | 1.56 (1.20–2.03) | 1.56 (1.20–2.02) | 1.55 (1.20–2.02) | 1.55 (1.19–2.01) | 1.54 (1.18–2.01) |
| Owns residence | Ref | Ref | Ref | Ref | Ref |
| Nagelkerke’s pseudo R2 | 0.34 | 0.33 | 0.33 | 0.33 | 0.34 |
Bolded figures are significant at p<0.05. In some instances, upper or lower confidence intervals are rounded to 1.00. In cases where bolded, exact figures did not cover 1.00.
All variables were entered simultaneously into the model, so each odds ratio is controlled for the other variables. All models also include covariates of age, gender, household size, marital status, health insurance, mental health conditions, and physical health conditions/risk factors.
To examine whether the models that included only one referent group for SSS (Models 1, 2, 3, and 4 in Table 4) were a better fit to the data than the model with all the SSS variables (Model 5 with all referent groups, in which each of the simpler models was nested), we conducted likelihood ratio tests. For likelihood ratio tests of nested models, the null hypothesis indicates that the restricted model is a better fit to the data than the full model (Pampel, 2000). When testing Models 1–4 separately against Model 5, likelihood ratio test results were not significant for Model 1 (with the referent, others in American society) (p=0.39) which indicates that the simpler Model 1 was a better fit to the data than Model 5. Results were significant (p<0.05) for the other three models, revealing that Model 5 was a better fit to the data than Models 2, 3, and 4. Overall, the likelihood ratio results suggest that using the referent group of others in American society alone provides the most parsimonious model.
It should also be noted that, even though SSS ratings were significantly associated with self-rated health, several of the OSS indicators still remained significant in the fully adjusted models. For income, having the lowest income level (under $10,000) was associated with worse self-rated health. Conversely, having slightly higher income appeared to have a protective effect, where in all five adjusted models, those earning $75,000–$99,999 had approximately 40% lower odds of reporting poor/fair health than those in the middle income bracket ($40,000–$59,999). For education and home ownership, not having a high school degree or not owning one’s home was significantly related to reporting poor/fair health in all five models. For example, in Model 1, individuals without a high school degree had 79% greater odds (95%CI:1.19–2.71) compared to those with some college and those not owning one’s home had 56% greater odds (95%CI:1.20–2.03) compared to home owners of reporting poor/fair health.
We also tested whether the relationship between SSS with each referent group and self-rated health varied by race/ethnicity by including interaction terms in each of the models. Results for the overall interaction terms of race/ethnicity*SSS were not significant in any of the four models (p>0.05), indicating no effect modification by race/ethnicity in the association between subjective status and self-rated health. Results for the overall interaction terms can be found in Electronic Appendix 1, which is available in the electronic publication only.
Discussion
In light of the current gap in the literature, this paper sought to explore whether the relationship between SSS and self-rated health was sensitive to the referent group used for social comparison. Results from the multivariable logistic regression models and subsequent likelihood ratio tests indicate that an SSS measure using the more distal referent group, others in American society, appears to have a stronger association with self-rated health than measures using other referent groups and also provides the most parsimonious model. A more distal referent group, such as others in American society, is one that is typically used in the growing subjective status literature within public health, and our results further validate these previous studies’ findings.
We had hypothesized that SSS with the referents of others of same race/ethnicity, neighbors, and parents at the same age would remain significant in the full model since each of these groups captures unique characteristics that are similar or proximal to the respondent. While social psychology research has yielded inconsistent evidence on referent group salience, several previous studies have shown that some individuals, particularly racial/ethnic minorities, make more frequent comparisons to more proximal referents such as those within their in-group (Guimond, 2006; Kulik & Ambrose, 1992; Leach & Smith, 2006; Suls & Wills, 1991). Yet in our study, there were no significant racial/ethnic differences in SSS ratings alone when using a more distal referent group (others in American society) and when controlling for OSS indicators. More importantly, the relationship between SSS and self-rated health was strongest with this national comparison and also did not differ by race/ethnicity. Furthermore, while Blacks had higher average SSS ratings than Whites when more proximate referents (others of the same race or ethnicity, neighbors, or parents) were used, there were no racial/ethnic differences in the SSS-health relationship in any of the models, and the effect sizes overall for these associations were smaller than when the national norm was respondents’ frame of reference. These findings suggest that more distal referent groups may be universally salient in our global society. One possibility for this result may be the more globalized nature of our environment, and “as a result of increasing technology and a highly mobile society, individuals do not necessarily need actual individuals with whom to compare themselves but instead can draw on national norms for social comparison” (Stiles, Liu, & Kaplan, 2000, p.80).
Overall, results from this study provide additional evidence that, regardless of their actual economic circumstances, how people perceive their subjective social position is strongly predictive of their self-rated health status. In the fully adjusted models, subjective status for all referent groups was significantly associated with self-rated health, while Figure 1 reveals, that even within the same income categories, self-rated health responses differed by the perception of one’s status. Research on how emotional and psychological factors related to perceived relative deprivation may indirectly or directly affect health is growing, and further work in this area will help elucidate the physiological and psychological mechanisms underlying this relationship. Understanding the nature and patterning of this association will also be important in future research. We expected to see a significant linear relationship between SSS and self-rated health in this study which did not emerge. Rather, in each model, feeling a lot worse off than a particular referent was significantly associated with poor/fair health, while only in the simpler Models 1, 2, and 4 was considering oneself better off significantly protective. It is possible that it is this most extreme category of perceived lower status that is associated with the chronic stress, anxiety, and other harmful effects of relative deprivation which may directly or indirectly influence health (Baum, Garofalo, & Yalli, 1999; Kubzansky & Kawachi, 2000; Marmot, 2000; Wilkinson, 1999). More research is warranted to explore whether there is a threshold effect, where only having the lowest levels of perceived status is significantly related to health. Most SSS studies in public health have used the ladder-based MacArthur Scale of Subjective Social Status as a linear predictor, and, therefore, have not conducted adjusted analyses with SSS as a nominal variable to examine this issue. However, Dunn et al. (2006), who used an SSS measure similar to the one in this study, also found a significant association between SSS and self-rated health only among those who considered themselves a lot worse off.
As in previous research, the OSS measures in our study—income, education, and home ownership—were found to have an independent effect on self-rated health. It is most likely that these objective indicators capture other important aspects of socioeconomic status not addressed by SSS. For example, in our study lower education (i.e., no high school degree) was consistently associated with reporting poor/fair health, although for Models 3 and 4, having a post-graduate degree was significantly protective. Some researchers have suggested that education may be the socioeconomic indicator that has the strongest indirect effect on health, since education itself has an effect on the more proximal measures of social position, income, and occupation which directly influence health (Singh-Manoux, Clarke, & Marmot, 2002). In addition to education, home ownership was associated with self-rated health in the multivariable models. Additional analyses showed a significant interaction between home ownership and SSS with only the referent of others in American society. Among non-home owners, those with lower SSS ratings when using the referent of others in American society had significantly greater odds of reporting poor/fair health; this was not the case among home owners. (Results are presented in Electronic Appendix 2, which is available in the electronic publication only.) It is possible that home ownership, which is a key component of wealth in the U.S., is a protective factor for health independent of income, by providing additional financial security in uncertain economic times (Pollack, Chideya, Cubbin, Williams, Dekker, & Braveman, 2007).
It was surprising that we did not find any racial/ethnic differences in the relationship between SSS and self-rated health given findings from previous research with smaller samples, which have shown a weaker or insignificant association between SSS and self-rated health among Blacks and Hispanics. From their work comparing Whites and Blacks, Adler et al. (2008) have suggested that the relationship between SSS and health is weaker among Blacks because they receive differential returns and fewer rewards from educational and occupational prestige than Whites. Others have come to a similar conclusion about this relationship among Hispanics (Ostrove et al., 2000). There may be several reasons why there were no racial/ethnic differences seen in our study. Previous research exploring racial/ethnic differences have generally used small samples, such as pregnant women or urban residents from a community sample or prepaid health plan (Adler et al., 2008; Ostrove et al., 2000), where findings may have limited generalizeability. It may be that racial/ethnic differences are not as strong when using a more nationally representative sample, as our study did. Alternatively, another possibility for this finding may also be a limitation of our sample, in that the racial/ethnic distribution of health status responses was slightly different than that seen in previous research. In our sample, a smaller percentage of Blacks and Hispanics—and a larger percentage of Whites—reported that they were in poor/fair health than respondents in other national surveys such as the BRFSS (Centers for Disease Control and Prevention, 2007). While we did not see any differences in the main effects between race/ethnicity and poor/fair health, there were significant racial/ethnic differences on the other end of the self-rated health spectrum. In our sample, Whites were more likely to report their health as excellent/very good than Blacks or Hispanics. There could be several explanations for these results. It is possible that these findings may be unique to this specific study’s sample or may indicate a methodological limitation of the survey panel. However, previous assessments of the validity of the sampling method used in the Styles surveys has shown that Styles responses have a high correlation with answers to similar questions administered via surveys that use probability sampling (Pollard, 2002). These results may also have surfaced due to racial/ethnic differences in the conceptualization of self-rated health. Qualitative research has found that Whites, Blacks, and Hispanics use different meanings of health when responding to a single self-rated health item, in that Whites are more likely to think about physical functioning issues, while Blacks and Hispanics are more likely to consider health problems as their frame of reference (Krause and Jay, 1994). Among Hispanics, language and acculturation level have also been found to be significant factors in how individuals assess their own health (Bzostek, Goldman, & Pebley, 2007; Finch, Hummer, Reindl, & Vega, 2002). The Styles surveys were only administered in English, and we do not know the nativity or acculturation level of Hispanics respondents. Whatever may be the reason, the inconsistent findings in our study compared to previous work on self-rated health suggests that additional research may be warranted to explore potential racial/ethnic differences in the relationship between SSS and health status.
As with all research, there are other limitations to this study. It is possible that psychological factors affect perceptions of both health and status. Previous researchers have argued that SSS and self-rated health are psychological measures that are functions of self-worth and other personal attributes, and health perceptions may in fact influence one’s judgments of whether he or she is better off or worse off than others (Ostrove et al., 2000). However, other studies have concluded that SSS is not entirely driven by psychological functioning (Singh-Manoux, Adler, & Marmot, 2003) or that psychological factors such as negative affect operate as mediators and not confounders in the relationship between SSS and health (Operario, Adler, & Williams, 2004). While we did not measure negative affect in this study, we did control for mental health conditions to reduce any possibility of confounding by related psychological factors. In bivariate analyses, there was a significant inverse relationship between each mental health condition (depression, bipolar disorder, and anxiety disorder) and all the SSS measures. Additionally, when the multivariate models in Table 4 were run without the mental and physical health conditions, results were very similar—but with only slightly larger effect sizes—to those in the final models which included these conditions as covariates. (Results are presented in Electronic Appendix 3, which is available in the electronic publication only.)
This study also is subject to the standard limitations of cross-sectional research. Findings can provide information on associations between variables, but not causation. Since there is no temporal ordering in this study, reverse causation is a possibility. However, the current study controls for several objective economic measures, which helps minimize the effect if worse health results in decreased income or employment status leading to lower SSS. Lastly, since cross-sectional research captures only one point in time, these data do not depict the dynamic nature of these concepts. SSS and self-rated health are both considered dynamic concepts that may change based on past and current circumstances and judgments of one’s perceived trajectories (Idler & Benyamini, 1997; Schnittker & McLeod, 2005; Wilkinson, 1999).
Despite these limitations, this study provides an important contribution to the emerging research on SSS and health. Previous public health studies have not explored the sensitivity of the relationship between SSS and self-rated health to various referent groups. Most SSS research has been conducted using small, homogenous samples within the U.S. or large samples from other countries which may not have the same level of racial/ethnic diversity. In using a national sample of adults in the U.S., this study provides additional evidence on the strength of the relationship between SSS and self-rated health, independent of economic measures. Additionally, it validates findings of previous studies that use a distal referent group in social comparison research when exploring the relationship between SSS and self-rated health. Future research will need to examine whether this type of distal referent group also seems the most appropriate to use when considering the association of SSS with other health measures such as health behaviors (e.g., smoking), chronic disease risk factors (e.g., being overweight or obese), or chronic conditions (e.g., cardiovascular disease, diabetes).
Acknowledgment
SVS is supported by the National Institutes of Health Career Development Award (NHLBI 1 K25 HL081275).
Contributor Information
Lisa S. Wolff, Director, Research and Evaluation, Health Resources in Action, 95 Berkeley Street, Boston, MA 02116, (617) 279-2240 x201, LWolff@hria.org.
S. V. Subramanian, Associate Professor, Department of Society, Human Development, and Health Harvard School of Public Health, 677 Huntington Avenue, Boston, MA 02115-6096.
Dolores Acevedo-Garcia, Associate Professor, Bouvé College of Health Sciences, and Associate Director, Institute on Urban Health Research, Northeastern University, 360 Huntington Avenue, Boston, MA 02115.
Deanne Weber, Senior Vice President, Strategic Planning and Research, Porter Novelli, 1909 K Street, Washington, DC.
Ichiro Kawachi, Chair, Department of Society, Human Development, and Health Professor of Social Epidemiology, Harvard School of Public Health, 677 Huntington Avenue, Kresge Building 7th Floor, Boston, Massachusetts 02115.
References
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychology. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Adler NE, Singh-Manoux A, Schwartz J, Stewart J, Matthews K, Marmot MG. Social status and health: A comparison of British civil servants in Whitehall-II with European- and African-Americans in CARDIA. Social Science and Medicine. 2008;66:1034–1045. doi: 10.1016/j.socscimed.2007.11.031. [DOI] [PubMed] [Google Scholar]
- Agyemang C, Denktas S, Buijnzeels M, Foets M. Validity of the single-item question on self-rated health status in first generation Turkish and Moroccans versus native Dutch in the Netherlands. Public Health. 2006;120(6):534–550. doi: 10.1016/j.puhe.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Baum A, Garofalo JP, Yalli AM. Socioeconomic status and chronic stress: Does stress account for SES effects on health? Annals of the New York Academy of Sciences. 1999;896:131–144. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Dallo FJ. Self-rated health and race among Hispanic and non-Hispanic adults. Journal of Immigrant and Minority Health. 2008;10(3):229–238. doi: 10.1007/s10903-007-9074-6. [DOI] [PubMed] [Google Scholar]
- Brown RA, Adler NE, Worthman CM, Copeland WE, Costello J, Angold A. Cultural and community determinants of subjective social status among Cherokee and White youth. Ethnicity and Health. 2008;13(4):289–303. doi: 10.1080/13557850701837302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bzostek S, Goldman N, Pebley A. Why do Hispanics in the USA report poor health? Social Science and Medicine. 2007;65(5):990–1003. doi: 10.1016/j.socscimed.2007.04.028. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System prevalence data, health status by race. 2007 Retrieved June 24, 2008, from http://www.cdc.gov/brfss/
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn JR, Veenstra G, Ross N. Psychosocial and neo-material dimensions of SES and health revisited: Predictors of self-rated health in a Canadian national survey. Social Science & Medicine. 2006;62(6):1465–1473. doi: 10.1016/j.socscimed.2005.07.038. [DOI] [PubMed] [Google Scholar]
- Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino(a)s. American Journal of Epidemiology. 2002;155(8):755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Social Science and Medicine. 2006;63(3):788–804. doi: 10.1016/j.socscimed.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Guimond S. Social comparison and social psychology: Understanding cognition, intergroup relations, and culture. New York, NY, US: Cambridge University Press; 2006. [Google Scholar]
- Hu P, Adler NE, Goldman N, Weinstein M, Seeman TE. Relationship between subjective social status and measures of health in older Taiwanese persons. Journal of the American Geriatrics Society. 2005;53(3):483–488. doi: 10.1111/j.1532-5415.2005.53169.x. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Jylhä M, Guralnik JM, Ferruci L, Jokela J, Heikkinen E. Is self-rated health comparable across cultures and genders? Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1998;53(3):S144–S152. doi: 10.1093/geronb/53b.3.s144. [DOI] [PubMed] [Google Scholar]
- Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: Multilevel analysis. British Medical Journal. 1998;317(7163):917–921. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause NM, Jay GM. What do global self-rated health items measure? Medical Care. 1994;32(9):930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Krieger N, Williams DR, Moss NE. Measuring social class in U.S. public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Kawachi I. Affective states and health. In: Berkman L, Kawachi I, editors. Social epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Kulik CT, Ambrose ML. Personal and situational determinants of referent choice. Academy of Management Review. 1992;17(2):212–237. [Google Scholar]
- Leach CW, Smith HJ. By whose standard? The affective implications of ethnic minorities' comparisons to ethnic minority and majority referents. European Journal of Social Psychology. 2006;36(5):747–760. doi: 10.1002/ejsp.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch J, Kaplan G. Socioeconomic position. In: Kawachi I, Berkman L, editors. Social epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Macleod J, Smith GD, Metcalfe C, Hart C. Is subjective social status a more important determinant of health than objective social status? Evidence from a prospective observational study of Scottish men. Social Science & Medicine. 2005;61(9):1916–1929. doi: 10.1016/j.socscimed.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Marmot M. Multilevel approaches to understanding social determinants. In: Berkman L, Kawachi I, editors. Social epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. American Journal of Epidemiology. 1999;149(1):41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- Oakes JM, Rossi PH. The measurement of SES in health research: Current practice and steps toward a new approach. Social Science and Medicine. 2003;56(4):769–784. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychology & Health. 2004;19(2):237–246. [Google Scholar]
- Ostrove JM, Adler NE, Kupperman M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychology. 2000;19(6):613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- Pampel FC. Logistic regression: A primer. Thousand Oaks, CA: Sage Publications; 2000. [Google Scholar]
- Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. American Journal of Preventive Medicine. 2007;33(3):250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- Pollard W. Use of consumer panel survey data for public health communication planning: An evaluation of survey results; Paper presented at the Annual Meeting of the American Statistical Association; New York, NY. 2002. Aug 11–15, [Google Scholar]
- Ren XS, Amick BC. Racial and ethnic disparities in self-assessed health status: Evidence from the National Survey of Families and Households. Ethnicity and Health. 1996;1(3):293–303. doi: 10.1080/13557858.1996.9961798. [DOI] [PubMed] [Google Scholar]
- Schnittker J, McLeod JD. The social psychology of health disparities. Annual Review of Sociology. 2005;31:75–103. [Google Scholar]
- Siahpush M, Borland R, Taylor J, Singh GK, Ansari Z, Serraglio A. The association of smoking with perception of income inequality, relative material well-being, and social capital. Social Science & Medicine. 2006;63:2801–2812. doi: 10.1016/j.socscimed.2006.07.015. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine. 2003;56(6):1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Clarke P, Marmot M. Multiple measures of socio-economic position and psychosocial health: Proximal and distal measures. International Journal of Epidemiology. 2002;31(6):1192–1199. doi: 10.1093/ije/31.6.1192. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67(6):855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. Journal of Epidemiology and Community Health. 2006;60:364–372. doi: 10.1136/jech.2005.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles BL, Kaplan HB. Adverse social comparison processes and negative self-feelings: A test of alternative models. Social Behavior and Personality. 2004;32(1):31–44. [Google Scholar]
- Stiles BL, Liu X, Kaplan HB. Relative deprivation and deviant adaptations: The mediating effects of negative self-feelings. Journal of Research in Crime and Delinquency. 2000;37(1):64–90. [Google Scholar]
- Subramanian SV, Kim D, Kawachi I. Covariation in the socioeconomic determinants of self rated health and happiness: A multivariate multilevel analysis of individuals and communities in the USA. Journal of Epidemiology and Community Health. 2005;59(8):664–669. doi: 10.1136/jech.2004.025742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, Wills TA, editors. Social comparison: Contemporary theory and research. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1991. [Google Scholar]
- Tropp LR, Wright SC. Ingroup identification and relative deprivation: An examination across multiple social comparisons. European Journal of Social Psychology. 1999;29(5):707–724. [Google Scholar]
- Veenstra G. Social status and health: Absolute deprivation or relative comparison, or both? Health Sociology Review. 2005;14(2):121–134. [Google Scholar]
- Weber D, Wolff LS, Orleans T, Mockenhaupt RE, Massett HA, Vose KK. Smokers’ attitudes and behaviors related to consumer demand for cessation counseling in the medical care setting. Nicotine & Tobacco Research. 2007;9(5):571–580. doi: 10.1080/14622200701189024. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG. Socioeconomic determinants of health: health inequalities: Relative or absolute material standards? British Medical Journal. 1997;314:591–595. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. Annals of the New York Academy of Sciences. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Wolff LS, Massett HA, Maibach EW, Weber D, Mockenhaupt RE, Hassmiller S. Validating a health consumer segmentation model: Behavioral and attitudinal differences in disease prevention-related practices. Journal of Health Communication. 2010;15(2) doi: 10.1080/10810730903528041. in press. [DOI] [PubMed] [Google Scholar]
- Wood JA, Taylor KL. Serving self-relevant goals through social comparison. In: Suls J, Wills TA, editors. Social comparison: Contemporary theory and research. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1991. [Google Scholar]
- Yip W, Adler NE. Does social standing affect health and happiness in rural China? Barcelona, Spain: Abstract presented at the International Health Economics Association; 2005. [Google Scholar]
- Zagefka H, Brown R. Comparisons and perceived deprivation in ethnic minority settings. Personality and Social Psychology Bulletin. 2005;31(4):467–482. doi: 10.1177/0146167204271711. [DOI] [PubMed] [Google Scholar]