Abstract
The purpose of this study was to examine patterns of anxiety among siblings of children with autism spectrum disorders (ASD), and determine the characteristics of the child with ASD and their parents that predicted anxiety. Data was collected from 1755 siblings of children with ASD whose families participated in the Simons Simplex Collection; siblings ranged in age from 3 to 18 years (M=9 years). Male siblings were at increased risk for sub-clinical anxiety problems during middle childhood. Parental history of anxiety disorders, higher maternal pragmatic language, and more proband behavior problems predicted higher anxiety. While siblings overall did not show elevated anxiety symptoms, higher rates of sub-clinical anxiety problems among males and siblings in middle childhood are cause for concern.
Keywords: Anxiety, Autism Spectrum Disorder, Siblings, Broader Autism Phenotype
As rates of autism spectrum disorder (ASD) diagnoses have risen dramatically over the past 40 years (e.g. King & Bearman, 2011), so has the number of siblings growing up with a brother or sister with ASD. Despite the recent increase in research on siblings of individuals with ASD, there is no consensus on whether these siblings are at risk for negative outcomes (Yirmiya, Shaked, & Erel, 2001). Some studies show that siblings exhibit more internalizing and externalizing problems, peer and conduct problems, hyperactivity, delinquent behavior, and withdrawal when compared to siblings of children without ASD (e.g. Benson & Karlof, 2008; Gau et al., 2010; Verte, Roeyers, & Buysse, 2003). Others, however, report that siblings of individuals with ASD are well-adjusted and show no more negative outcomes than control groups (e.g. Hastings, 2003; Pilowsky. Yirmiya, Doppelt, Gross-Tsur, & Shaley, 2004). The present study examined patterns and predictors of one negative outcome that may be especially prevalent among siblings of children with ASD – anxiety.
Anxiety disorders are among the most common psychological disorders in childhood (Cartwright-Hatton, McNicol, & Doubleday, 2006). If left untreated, anxiety disorders in childhood can negatively impact academic, cognitive, and social development (Johnson, Chilcoat, Breslau, 2000; Visu-Petra, Tincas, Cheie, & Benga, 2010; Vitiello & Waslick, 2010). Children with anxiety problems are more likely to experience bouts of clinical anxiety throughout their lives (Cartwright-Hatton, 2006), as well as future episodes of depression (e.g. Caspi, Moffitt, Newman, & Silva, 1998; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Roza, Hofstra, van der Ende, & Verhulst, 2003). Thus, anxiety problems in siblings of children with ASD could negatively influence their current as well as future development.
Although it is unclear whether siblings of children with ASD experience elevated anxiety, there is evidence to suggest they may be at-risk for such problems. Family members of individuals with ASD tend to have increased rates of anxiety problems (Lainhart, 1999; Piven et al., 1991; Smalley, McCracken, & Tanguay, 1995). Micali, Chakrabarti, and Fombonne (2004), for example, found that mothers of children with ASD had anxiety disorders at three times the rate of mothers of typically developing children. A family history of mental illness, and particularly a parental anxiety diagnosis, is one of the most common predictors of anxiety in children (e.g. Cents et al., 2011; McClure, Brennan, Hammen, & Le Brocque, 2001), and thus siblings of children with ASD might be at increased risk for anxiety. To our knowledge, only one study has measured anxiety among siblings of individuals with ASD specifically (rather than all first-degree relatives), finding that siblings’ rates of anxiety problems did not differ from a normed comparison group (Orsmond & Seltzer, 2009). However, that study focused on adolescents; it is unknown whether child siblings of individuals with ASD have higher rates of anxiety problems.
Sibling characteristics, such as age and gender, may impact their likelihood of exhibiting anxiety problems. The literature on gender and anxiety is somewhat mixed. Most research shows that girls have higher anxiety than boys throughout childhood and adolescence (e.g. Bongers, Koot, van der Ende, & Verhulst, 2003; La Greca & Lopez, 1998; Wadsworth, Hudziak, Heath, & Achenbach, 2001), though a few studies have found no gender differences in anxiety disorders (Bernstein, Borchardt, & Perwien, 1996; Last, Perrin, Hersen, & Kazdin, 1992). No studies, that we are aware of, found higher rates of anxiety in males compared to females. Therefore, we hypothesized that female siblings of children with ASD would have higher rates of anxiety than male siblings.
The relation between age and anxiety seems dependent on gender. While numerous studies have found stable rates of anxiety for boys throughout childhood and adolescence (e.g. Bongers et al., 2003; Keiley, Bates, Dodge, & Pettit, 2000; van Oort, Greaves-Lord, Verhulst, Ormel, & Huizink, 2009; Wittchen, Nelson, & Lachner, 1998), one study found that more preadolescent boys than adolescent boys demonstrated a “severe” level of anxious/depressed problems (Wadsworth et al., 2001). Alternatively, research has consistently found that adolescent girls experience higher rates of anxiety than preadolescent girls (e.g. Bongers et al., 2003; Roza et al., 2003; Wadsworth et al., 2001; Wittchen et al., 1998).
Females may experience greater anxiety during adolescence because of gender differences in attunement (Kessler & McLeod, 1984). Starting in adolescence, females become more aware (both than they were previously and also compared to their male counterparts) of stressful events among their loved ones, which then leads to personal distress. Because stress tends to be particularly high among families of children with ASD (e.g. Gold, 1993; Verte et al., 2003), this theory would suggest that female siblings of individuals with ASD may be more attuned to such family stress, and exhibit an increase in anxiety symptoms during adolescence. Alternatively, male siblings’ anxiety symptoms would be stable across childhood and adolescence.
Siblings of children with ASD may also be at increased risk for anxiety problems due to parental characteristics such as the broader autism phenotype (BAP) and increased rates of anxiety disorders. BAP characteristics, which include rigid personality, aloof personality, and pragmatic language, are considered the behavioral expression of increased genetic risk to autism (Hurley, Losh, Parlier, Reznick, & Piven, 2007). Orsmond and Seltzer (2009) found that under conditions of heightened stress, higher maternal BAP characteristics were related to more depressive symptoms among adolescent siblings of individuals with ASD. Thus, we hypothesized that more parental BAP characteristics may relate to increased anxiety among siblings of children with ASD. As already mentioned, the presence of a parental anxiety diagnosis is a strong predictor of anxiety in children (Cents et al., 2011; McClure et al., 12001), and is likely an important factor in increased sibling anxiety.
Characteristics of the brother or sister with ASD, particularly behavior problems, are also likely related to sibling anxiety. Increased behavior problems among individuals with ASD predict more sibling behavior problems as well as less positive affect in the sibling relationship (Hastings, 2007; Orsmond, Kuo, & Seltzer, 2009). Although some studies have found that greater autism severity is related to poorer sibling outcomes (Benson & Karlof, 2008), this association is less consistent.
The Present Study
The present study used data from the Simons Foundation Autism Research Initiative Simplex Collection (SSC) to examine anxiety among typically developing siblings of children with ASD. The following research questions were examined: 1) Do siblings of children with ASD, as a group, have higher rates of anxiety problems relative to the normed sample described by Achenbach and Edelbrock (1983)? 2) Within siblings of individuals with ASD, how does anxiety differ by age and gender? 3) Do characteristics of the brother or sister with ASD (behavior problems, ASD severity) predict sibling anxiety? 4) Does the shared family environment, specifically characteristics of the parent (parental history of anxiety disorder, parental BAP characteristics), predict sibling anxiety above and beyond characteristics of the child with ASD? Conversely, do characteristics of the brother or sister with ASD continue to predict anxiety after controlling for the shared family environment?
We hypothesized that: 1) Siblings of individuals with ASD would have higher rates of anxiety than norms. 2) Within siblings of individuals with ASD, girls would show higher levels of anxiety than boys overall. Within gender, adolescent girls would show higher rates of anxiety than preadolescent girls, while rates of anxiety for males would be stable across ages. 3) More behavior problems in the brother/sister with ASD would predict higher levels of sibling anxiety. The severity of his/her autism symptoms, however, would not influence anxiety. 4) Parental history of anxiety and higher levels of parental BAP characteristics would predict increased sibling anxiety above and beyond characteristics of the brother/sister with ASD. Furthermore, more behavior problems present in the brother/sister with ASD would continue to predict increased anxiety after controlling for characteristics of the shared family environment.
Methods
Participants
The sample included 1755 siblings of children diagnosed with ASD (the children with ASD are hereafter referred to as probands). The siblings ranged in age from 3 – 18 years (M=9.48, SD=3.67). Approximately one-half of siblings were female (54.6%) and older than the proband (52.1%). The probands’ ages ranged from 4 – 18 years (M=9.12, SD=3.31) and they were primarily male (87.1%), with an average IQ of 81.54 (SD=27.74). While the majority of probands were diagnosed with autistic disorder (88.3%), 11.7% received other diagnoses on the autism spectrum.
Relative to national statistics, parents in this sample were more likely to be married (90.9% in this sample compared to 48% of American households; US Census Bureau, 2012) and to have a higher household income (Median household income of the sample was between $81,000 and $100,000 compared to the US median of $50,046; US Census Bureau, 2011). The number of children in the family ranged from 2 – 9 (M=2.54, SD=0.85). Of particular interest to this study, 3.9% of fathers and 10.4% of mothers reported a previous diagnosis of anxiety disorder. Cases where both parents reported an anxiety disorder were relatively rare (N=13 or 0.7% of the study sample). Of those with an anxiety disorder diagnosis, 54.4% of fathers and 32.8% of mothers had a history of at least one other mental illness. The most common comorbid disorders were depressive disorder (36.8% of fathers with anxiety disorder; 10.9% of mothers with anxiety disorder), attention deficit disorder (8.8% of fathers; 9.3% of mothers), and bipolar disorder (8.8% of fathers).
The present sample was derived from the SSC database, which included 2,443 probands with ASD. Of that sample, 1,996 families included information on a selected sibling and were thus eligible for the present study. Siblings were removed from the sample if they were missing data on anxiety symptoms (N=90) or parental history of anxiety disorders (N=151), leaving a final sample size of 1,755.
Procedure
Families of children with ASD participated in the SSC, a multi-site project carried out in North American, university-affiliated research clinics. All probands met autism spectrum cutoff scores on the Autism Diagnostic Observation Schedule (ADOS: Lord et al., 1989) and the Autism Diagnostic Interview-Revised (ADI-R; Rutter, LeCouteur, & Lord, 2003), and were issued a best estimate DSM-IV-TR (American Psychiatric Association, 2000) diagnosis of an ASD by study clinicians. If probands had sensory or motor impairments that prevented the valid use of assessments, the family was not eligible for the study. To participate, both the biological mother and father of the proband had to agree to be in the study (which is likely responsible for the high marriage rate in this sample). Parents could not have a diagnosis of ASD, intellectual disability, or schizophrenia. Families were excluded if any sibling (including the designated sibling), had the following: a diagnosis or referral for ASD, an intellectual disability, a diagnosis of schizophrenia or another psychiatric diagnosis requiring treatment with two or more psychotropic medications, or an Individualized Education Plan.
Sample recruitment procedures and data collection methods are reported elsewhere (Simons Foundation, 2010). The present study focused on the following measures: the Child Behavior Checklist (CBCL) regarding the sibling and the proband, parental mental health history, the Broader Autism Phenotype Questionnaire regarding the mother and the father, proband IQ, and an Autism Certainty Score from Clinician Report, as well as household income, number of children in the family, and sibling’s birth order in relation to the proband. Means and percentages for all independent variables can be found in Table 1. The present study was approved by the University’s Institutional Review Board.
Table 1.
Means and Standard Deviations for Independent Variables
| Mean (SD) | Minimum | Maximum | |
|---|---|---|---|
| Proband Total Internalizing Problems | 60.03 (9.53) | 33.00 | 90.00 |
| Proband Total Externalizing Problems | 56.21 (10.78) | 32.00 | 97.00 |
| Proband Autism Severity Score | 13.10 (2.40) | 6.00 | 15.00 |
| Maternal BAPQ Rigid Score | 2.67 (0.74) | 1.00 | 5.67 |
| Maternal BAPQ Pragmatic Language | 2.08 (0.60) | 1.00 | 4.50 |
| Maternal BAPQ Aloof Score | 2.38 (0.79) | 1.00 | 5.50 |
| Paternal BAPQ Rigid Score | 2.87 (0.75) | 1.00 | 5.75 |
| Paternal BAPQ Pragmatic Language | 2.35 (0.64) | 1.00 | 4.92 |
| Paternal BAPQ Aloof Score | 2.84 (0.87) | 1.00 | 5.50 |
Dependent Variable
Sibling Anxiety
Sibling anxiety was measured using the CBCL (Achenbach & Rescorla, 2001). The CBCL is one of the most widely used rating scales of children’s adjustment; it has been extensively used in community as well as clinic samples. Parents rated the sibling on items scored on a 3-point scale (0 = not true, 1 = sometimes or somewhat true, 2 = often true). These items fall into eight syndrome subscales, including the “Anxiety Problems” subscale that is the focus of our study. Parental report of child behaviors on this six-item subscale provides a dimensional measure of anxiety consistent with the DSM-IV-TR (American Psychological Association, 2000). Ebesutani et al. (2010) found that the “Anxiety Problems” subscale had good correspondence with DSM anxiety diagnoses (e.g., generalized anxiety disorder) derived from structured clinical interviews, and had better predictive validity than the Anxious/Depressed symptoms scale.
Scores for the broadband scales and subscales were normed based on gender and three age groups: 2–5 years, 6–11 years, 12–18 years. In the following analyses, participants’ CBCL scores are reported by these predetermined age groups, which reflect early childhood, middle childhood, and adolescence, respectively. Because Achenbach and Edelbrock (1983) recommend using T-scores when comparing subjects of different age categories, we used the standardized T-scores. Subscale scores are grouped into average (T-scores of 50–64), borderline (T-scores of 65–69), and clinical scores (T-scores ≥ 70; Achenbach & Edelbrock, 1983).
Independent Variables
Proband behavior problems
Proband internalizing and externalizing problems were measured by parental report using the corresponding subscales from the CBCL (Achenbach & Edelbrock, 1983). Higher scores indicate more proband internalizing and externalizing behaviors. While not developed for children with autism, the CBCL has been used extensively in populations of individuals with ASD (e.g. Snow & LeCavalier, 2011; Spratt et al. 2012).
Proband autism severity
The autism certainty score was chosen as a measure of autism severity. Although the SSC dataset includes the calibrated autism severity score derived from the ADOS (Gotham, Pickles, & Lord, 2009), severity scores were not available for probands tested using Module 4 of this instrument. Rather than eliminate siblings of these individuals, we instead used the autism certainty score, similar to the certainty scale described by Lord et al. (2006). The certainty score is a rough measure of symptom severity, as a diagnosis of classic autism (compared to diagnoses of other disorders on the autism spectrum), by definition, involves more comprehensive and/or intense symptoms (Lord et al., 2006). Possible scores ranged from 6 (highly uncertain the proband is on the autism spectrum) to 15 (highly certain the proband meets strict DSM-IV-TR Autism criteria).
Parental history of anxiety disorder
Mothers and fathers indicated whether they had ever received a diagnosis of any mental health disorder, with one option being anxiety disorder. Two dichotomous variables were used in analyses: 0 = mother/father has never received an anxiety disorder diagnosis; 1 = mother/father has received an anxiety disorder diagnosis.
Parental Broader Autism Phenotype
Mothers and fathers completed the Broader Autism Phenotype Questionnaire (BAPQ; Hurley, et al., 2007) about themselves. This 36-item questionnaire assesses the extent to which individuals display characteristics of the broader autism phenotype by asking participants to rate, on a 1–6 scale, how frequently each statement applies to them. It is divided into 3 subscales: rigid personality (e.g., “I act very set in my ways”), aloof personality (e.g., “Conversation bores me”), and pragmatic language (e.g. “I leave long pauses in conversation”). The BAPQ subscales have acceptable sensitivity and specificity (Hurley et al., 2007). Cronbach’s alphas for BAPQ subscales in this sample ranged from .76–.91. Higher scores on the subscales indicate a more rigid personality, a more aloof personality, and more use of pragmatic language.
Covariates
Proband IQ
Proband IQ was assessed with a variety of measures, based on age and verbal ability. These measures included the Mullen Scales of Early Learning (Mullen, 1995), Wechsler Abbreviated Scale of Intelligence (The Psychological Corporation, 1999), Differential Ability Scales – Second Edition (Elliot, 2007), and the Wechsler Intelligence Scale for Children (Wechsler et al., 2004). Each of these measures gives a full-scale standardized score with a mean of 100 and standard deviation of 15, and thus it was possible to combine IQ scores over different measures.
Demographics
Additional covariates included household income, number of siblings in the family, and sibling birth order in relation to the proband (0 = sibling is younger than the proband, 1 = sibling is older than the proband).
Data Analysis
For Research Question 1, which focused on patterns of anxiety in the entire sibling sample compared to norms, we examined frequencies to determine the percentage of siblings who fell above cutoffs for borderline and clinical anxiety problems. Research Question 2 focused on differences within the sample in patterns of anxiety by sibling age and gender. To address this question, sibling anxiety was examined three ways: continuous T-scores; percentage of siblings falling above borderline cutoffs; and percentage of siblings falling above clinical cutoffs. We used chi-squares to compare the percentages of siblings falling above cutoffs by gender and age category [2–5 years (early childhood); 6–11 years (middle childhood); 12–18 years (adolescence)]. Because of the skewed distribution of the continuous anxiety T-scores, nonparametric tests were used to compare T-scores among age and gender (Mann-Whitney tests for gender comparisons; Kruskal-Wallis tests for age comparisons).
Research Questions 3 and 4 focused on the proband and parent factors that independently predicted sibling anxiety. Anxiety problems T-scores are truncated on the lower end at 50, and the distribution was highly skewed, over-dispersed, with a preponderance of lowest-possible scores. Thus, we decided to use the nonlinear Negative Binomial Regression models to estimate relationships between independent variables and sibling anxiety (Gardner, Mulvey, & Shaw, 1995). The first regression model included the following independent variables: proband internalizing and externalizing behaviors, and proband autism severity. The second model added maternal and paternal history of anxiety disorder, as well as maternal and paternal BAPQ subscale scores (rigid, pragmatic language, and aloof) to the first model. Household income, sibling birth order, number of siblings in the family, and proband IQ were statistically controlled in all regression models. Because we suspected that there might be different patterns of prediction for male vs. female siblings, we ran 3 sets of regressions: 1) whole sample; 2) male siblings only; 3) female siblings only. Multicollinearity was tested among the independent variables using bivariate correlations. None of the correlations were above .54, suggesting that multicollinearity was not a problem. Because of the small amount of missing data (< 2% for any single question, except for income, which was missing 5.9%), mean substitution was used following the guidelines of Harrell (2001).
Results
Research Questions 1 and 2: Patterns of Sibling Anxiety
Overall
Median T-scores for sibling anxiety problems, and percentages of siblings falling above borderline and clinical cutoffs are presented in Table 2. In the general population, 7% of children fall above the borderline cutoff and 3% fall above the clinical cutoff (Achenbach & Edelbrock, 1983). The percentages of siblings in this sample in the borderline (8%) and clinical (4%) ranges were close to these expectations, and thus do not appear elevated.
Table 2.
Sibling Anxiety Scores and Percentages of Siblings Falling Above Borderline and Clinical Cutoffs for Anxiety Problems by Age and Gender
| N | Median T- Score |
Χ2/Z Value |
% Above Borderline |
Χ2 | % Above Clinical |
Χ2 | |
|---|---|---|---|---|---|---|---|
| All Siblings | 1755 | 50.00 | 8.0% | 4.0% | |||
| By Gender: Males | 797 | 50.00 | −1.04 | 9.5% | 4.83* | 4.3% | .18 |
| Females | 958 | 50.00 | 6.7% | 3.9% | |||
| By Age: 2–5 | 349 | 50.00 | 52.90** | 3.2% | 22.09*** | 2.6% | 4.13 |
| 6–11 | 940 | 51.00 | 10.6% | 4.9% | |||
| 12–18 | 466 | 50.00 | 6.2% | 3.4% | |||
| Males: 2–5 | 164 | 50.00 | 18.50*** | 3.0% | 15.23*** | 2.4% | 2.11 |
| 6–11 | 410 | 51.00 | 13.2% | 5.1% | |||
| 12–18 | 223 | 50.00 | 7.6% | 4.0% | |||
| Females: 2–5 | 185 | 50.00 | 37.90*** | 3.2% | 8.09* | 2.7% | 2.34 |
| 6–11 | 530 | 51.00 | 8.7% | 4.7% | |||
| 12–18 | 243 | 50.00 | 4.9% | 2.9% |
p > .05
p < .01
p < .001
Note: For the continuous T-scores, Z-scores from the Mann-Whitney U-test are presented for gender comparisons, and chi-squares from the Kruskal-Wallis test are presented for age comparisons.
Sibling Gender
Both males and females had a median anxiety T-score of 50. However, males were significantly more likely to have scores above the borderline cutoff, with nearly 10% of males falling above this score, compared to 6.7% of females (see Table 2). There were no gender differences in the percentage of siblings falling above the clinical cutoff.
Sibling Age
When dividing the sample by age groups, 6–11 year olds had both the highest median T-scores and the highest percentage of individuals falling above the borderline cutoff (10.6%, compared to 3.2% for 2–5 year olds and 6.2% for 12–18 year olds; see Table 2). There were no significant age differences in siblings who fell above the clinical cutoff.
This same pattern held when looking at effects of age for males and females separately. For both genders, 6–11 year olds had higher median T-scores than other age groups and a higher percentage of individuals falling above the borderline cutoff. Males showed the strongest age differences, with 6–11 year old males nearly twice as likely to have scores in the borderline or clinical range as would be expected from norms.
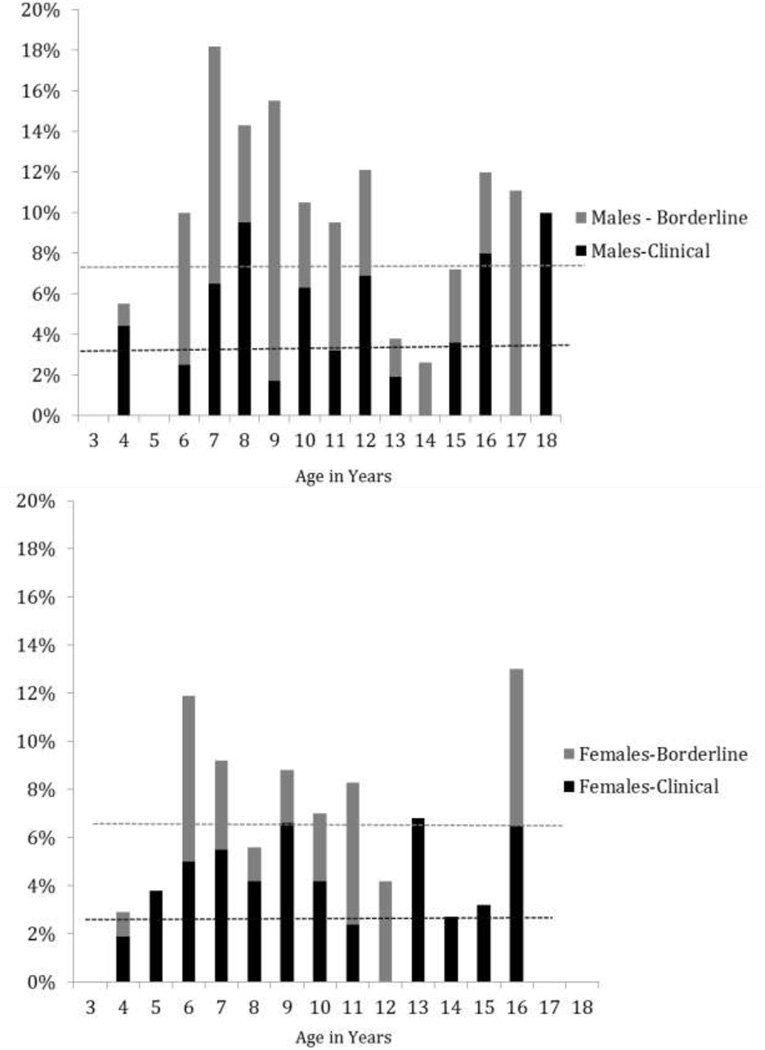
Because age differences were significant for both males and females, we further divided the sample into age by individual years. These results are presented in Figure 1. Nearly every age between 6 and 11 showed higher than expected percentages falling above the borderline cutoff, thus confirming the findings using age categories.
Figure 1.
The percentage of males (1a) and females (1b) at each age falling above the borderline and clinical cutoffs. The black dotted line represents the percentage of children expected to fall above the clinical cutoff. The gray dotted line represents the percentage of children expected to fall above the borderline cutoff.
Follow-up Analyses
We conducted follow-up analyses to determine whether the higher rate of borderline anxiety problems among 6–11 year old male siblings reflected elevated anxiety specifically, or elevated rates of behavior problems in general. Just over 14% of males in this age group had CBCL total problem behavior scores above the borderline cut-off, which is less than the 16% that would be expected in the general population (Achenbach and Edelbrock, 1983). These findings suggest that elevated rates of sub-clinical anxiety problems among 6–11 year old male siblings of children with ASD are not merely a result of higher rates of general problem behaviors.
Research Question 3: Proband Predictors of Sibling Anxiety
Unstandardized regression coefficients and standard errors of the estimates for regression models including all siblings, male siblings only, and female siblings only are presented in Table 3. In all regression models, more proband internalizing and externalizing behavior problems significantly predicted higher levels of sibling anxiety. Proband autism severity did not predict sibling anxiety in any of the models (see Table 3, Model 1).
Table 3.
Unstandardized Regression Coefficients and Standard Errors for Negative Binomial Regression Models Predicting Sibling Anxiety from Proband (Model 1) and Proband/Parental (Model 2) Characteristics
| All Siblings | Male Siblings | Female Siblings | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | Model 2 | Model | Model 2 | Model | Model 2 | |||||||
| B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | |
| Proband Characteristics | ||||||||||||
| Internalizing Problems | .03*** | .00 | .03*** | .00 | .02*** | .01 | .02*** | .01 | .04*** | .00 | .03*** | .01 |
| Externalizing Problems | .02*** | .00 | .01*** | .00 | .02*** | .00 | .01** | .00 | .02*** | .00 | .01** | .00 |
| Autism Severity | .01 | .01 | .02 | .01 | .01 | .02 | .02 | .02 | .00 | .02 | .01 | .02 |
| Parental Characteristics | ||||||||||||
| Maternal Anxiety Disorder | .46*** | .09 | .41** | .13 | .57*** | .12 | ||||||
| Maternal BAPQ Rigid | .05 | .04 | .08 | .07 | .02 | .06 | ||||||
| Maternal BAPQ Pragmatic Language | .38*** | .06 | .36*** | .08 | .38*** | .08 | ||||||
| Maternal BAPQ Aloof | −.10* | .04 | −.17* | .07 | −.03 | .06 | ||||||
| Paternal Anxiety Disorder | .36** | .14 | .53** | .20 | .12 | .20 | ||||||
| Paternal BAPQ Rigid | .01 | .04 | −.07 | .07 | .09 | .06 | ||||||
| Paternal BAPQ Pragmatic Language | .05 | .05 | .06 | .08 | .05 | .07 | ||||||
| Paternal BAPQ Aloof | .05 | .04 | .07 | .06 | .05 | .06 | ||||||
p > .05
p < .01
p < .001
Note The following variables were statistically controlled in all regression models: Proband IQ; household income; number of siblings; sibling birth order.
Research Question 4:Addition of Parental Predictors of Sibling Anxiety
All Siblings
Table 3, Model 2 includes both proband and parental predictors of sibling anxiety. For all siblings, higher levels of proband internalizing and externalizing problems (but not autism severity) continued to predict greater sibling anxiety after adding in parental predictors. In terms of parental variables, having a mother or father diagnosed with an anxiety disorder was related to more sibling anxiety. While no paternal BAPQ scores were related to anxiety, higher maternal pragmatic language predicted more sibling anxiety. Maternal aloof personality also predicted anxiety, but less strongly than pragmatic language and in the opposite direction as expected. The bivariate correlation showed a small, positive relation between maternal aloof personality scores and sibling anxiety (r=.06, p<.01), suggesting that the small negative effect in regression was an artifact.
Males
The pattern of prediction for male siblings’ anxiety was similar to that of the sample as a whole (see Table 3, Model 2).
Females
Maternal history of anxiety, higher maternal pragmatic language, and greater proband internalizing and externalizing problems predicted more female sibling anxiety, following the same patterns as for the whole sample. However, paternal history of anxiety and maternal aloof personality did not predict anxiety among females.
Follow-up Analyses
Because parental history of anxiety disorders was highly comorbid with other psychiatric disorders, we re-ran the regression models using parental history of any psychopathology in place of history of anxiety. The overall pattern of results remained the same (results available from corresponding author).
In order to ensure that the non-significant relations between proband autism severity and sibling anxiety were not an artifact of using the autism diagnostic certainty score instead of the ADOS autism severity score (Gotham et al., 2009), we re-ran our regression models using calibrated autism severity scores in place of diagnostic certainty (thus eliminating 37 siblings whose brother or sister with ASD was given Module 4 of the ADOS). The relations between ADOS autism severity scores and sibling anxiety did not reach statistical significance (Bs = .00, −.01, .03 for total sample, males, and females, respectively, ps > .30).
Discussion
Though individuals with ASD have been the focus of many studies over the past decades, research on the adjustment of their families, and particularly their siblings has lagged behind. To our knowledge, the present study is the first to examine age and gender influences on anxiety among a broad age range of siblings of children with ASD. As a whole, these siblings did not experience higher rates of borderline or clinical anxiety symptoms, which is consistent with other studies (e.g. Orsmond & Seltzer, 2009, Yirmiya et al., 2001). Stratification of the sample by gender and age, however, revealed interesting findings; although none of the age/gender groups had elevations in anxiety that reached the clinical range, male siblings in middle childhood were twice as likely as would be expected to fall above the borderline cutoff. These findings seem to be specific to anxiety, as siblings did not exhibit elevated rates of total behavior problems, which is consistent with previous research (Dempsey, Llorens, Brewton, Mulchandani, & Goin-Kochel, 2012). Thus, siblings of children with ASD as a whole appear not to experience elevated rates of anxiety disorders, but certain sibling groups may be at risk for increased anxiety symptoms, which are indicative of a need for professional help and concern (Achenbach & Rescorla, 2001).
Higher anxiety scores among male siblings of children with ASD compared to female siblings contradicts previous research showing that girls in the general population experience higher rates of anxiety than boys at all ages (Bongers et al., 2003; La Greca & Lopez, 1998; Wadsworth et al., 2001). This may be because of higher rates of sub-clinical autism symptoms among male siblings, due to the higher likelihood of ASD among boys compared to girls (e.g. Fombonne, 1999). Although siblings with an ASD or suspected ASD diagnosis were excluded from the SSC sample, sub-clinical autism symptoms may still be present in males. These symptoms can lead to or manifest as anxiety problems, as well as other problematic sibling outcomes (Petalas et al., 2012; Rosbrook & Whittingham, 2010). Sub-clinical autism symptoms were not measured in siblings in the SSC dataset, and future research would benefit from the inclusion of BAP symptoms when examining predictors of sibling adjustment, including anxiety.
An elevated rate of borderline and clinical anxiety scores among both male and female siblings in middle childhood (6–11 years old) was unexpected. There is some research to suggest that boys in this age range in the general population have higher rates of anxiety problems than their adolescent counterparts (Wadsworth et al., 2001), but studies tend to find that adolescent girls (compared to pre-adolescent) have higher rates of anxiety (Bongers et al., 2003; Roza et al., 2003; Wadsworth et al., 2001; Wittchen et al., 1998). Related developmental research may provide insight. Glasberg (2000) described how siblings’ understanding of autism and its implications increase significantly around age 7, as children advance in their cognitive development. Additionally, children within the 6–11 age group are starting school, creating a new environment for social anxiety (Beesdo, Knappe, & Pine, 2009). The newfound understanding of their brother/sister’s autism could lead to an increase in anxiety as siblings enter school and fear how peers will evaluate their family.
Additionally, the descriptive data examining anxiety by individual ages (instead of age groupings; see Figure 1) suggests that anxiety might decline in middle adolescence before rising in later years. This pattern must be interpreted with caution, however, as the study sample included far fewer siblings in middle and later adolescence than in childhood (e.g., there were 186 7-year old siblings but only 56 16-year old siblings and 26 17-year old siblings). Future research focused specifically on adolescence is needed to determine the longitudinal patterns of anxiety among adolescent siblings of children with ASD, as well as what factors (e.g. puberty, social experiences) influence anxiety at this age.
We found that parental history of anxiety and sibling behavior problems (but not autism severity) predicted sibling anxiety, which is consistent with existing research (Hastings, 2007; McClure et al., 2001; Neece, Blacher, & Baker, 2010). Follow-up analyses showed that any parental history of psychopathology had the same predictive relations with sibling anxiety as history of anxiety disorder. While some scientists hypothesize that children are at greatest risk for developing the same psychopathology exhibited by their parents (e.g. Merikangas, 2002), the high rate of comorbidity in our sample makes it difficult to ensure that it is truly anxiety, rather than any psychiatric diagnosis, that is related to sibling anxiety.
However, the observed relation between the pragmatic language aspect of the maternal broader autism phenotype and sibling anxiety is novel. Although one previous study found that the maternal broader autism phenotype predicted sibling depression (Orsmond & Seltzer, 2009), this study only included mothers and did not examine the different aspects of the broader autism phenotype. Problems with pragmatic language make it difficult to carry on reciprocal conversations and effectively communicate with others (Hurley et al., 2007), and parental communication has been linked to children’s development (e.g. Huang, 1999; Kelly et al., 2002). Most relevant to this study, Landman-Peeters et al. (2005) reported that problems in parent-child communication were an important predictor of child anxiety. Our finding that only certain BAP characteristics were related to sibling anxiety suggests that it is important to evaluate subcategories of the BAP when examining its effects on children.
Another novel finding of this study was that maternal, and not paternal, pragmatic language predicted sibling anxiety. This suggests that BAP symptoms may affect children through behavioral as well as genetic mechanisms. While little is known specifically about fathers of children with ASD, research among the general population shows that mothers participate in child-rearing activities at higher rates than fathers (e.g. Barnard & Solchany, 2002; Parke, 2002). If the same is true among families of children with ASD, it is logical to expect that maternal BAP symptoms, and the resulting effect of these symptoms on parenting behaviors, would be more influential on child development than paternal symptoms.
As with all research, the present study has limitations. First, although secondary data analyses allows for the examination of a larger group of siblings than could be studied in any one research project, we were limited to the variables that were collected as part of the SSC data collection. A measure of anxiety problems derived from clinical interviews was not available (although the CBCL anxiety problems subscale has high correspondence with clinical interview data; Ebesutani et al., 2010), nor is the CBCL an autism-specific measure of behavior problems. There are many other variables, unavailable in the SSC dataset, that might help explain patterns of anxiety in this population, including parental stress, pubertal timing, or sibling BAP symptoms.
Second, most measures were collected via parental report. Parental characteristics, including BAP symptoms and history of anxiety, may affect parental endorsement of child anxiety symptoms, thus lending bias to parent report measures. Future research should include multiple informants to gain a more complete picture of sibling anxiety. Finally, the SSC sample likely does not generalize to all families of children with ASD. The mean proband IQ, median household income, and percentage of married parents were all higher than would be expected, while the rates of parental anxiety were low (i.e., 10.4% of mothers of children with ASD compared to national lifetime prevalence rates of 28.8%; Kessler et al., 2005). These factors characterize the study sample as relatively high-functioning in comparison to all families of children with ASD, limiting generalizability. Additionally, SSC protocol excluded families if siblings had been diagnosed with any psychiatric disorder that required treatment with two or more psychotropic medications (Simons Foundation, 2010), including anxiety. Thus, the most severely affected siblings were not part of the SSC sample, suggesting that the rate of clinical-level anxiety problems among siblings of children with ASD may in fact be higher than in our study. Alternatively, the large sample size and multi-site nature of the SSC are considerable strengths of this study, as these findings are likely more generalizable than many smaller studies of siblings of individuals with ASD.
Conclusions
While previous studies have examined anxiety among first-degree relatives of individuals with ASD, this study is one of the first to measure both patterns and predictors of sibling anxiety. We found increased rates of sub-clinical anxiety problems among males and siblings in middle childhood. While these siblings may not meet DSM criteria for an anxiety disorder, borderline levels of anxiety may still be problematic and warrant further investigation. To build on the current study, future research should examine the factors that may place male siblings at greater risk for anxiety problems, as well as the role of maternal pragmatic language in the development of sibling anxiety.
Acknowledgments
We would like to thank the Simons Foundation Autism Research Initiative for the use of their data, with special thanks to Alison Vehorn and Melissa Potter for their help obtaining data. Core support was received from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P30 HD15052, E.M. Dykens, PI). Thanks to Dr. Warren Lambert for statistical consultation.
Footnotes
The authors report no financial interests or potential conflicts of interest.
References
- American Psychiatric Association. Diagnostics and Statistical Manual of Mental Disorders (DSM-IV-TR) 4th ed text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont; 1983. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASBEA School-Age Forms and Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Barnard KE, Solchany JE. Mothering. In: Bernstein MH, editor. Handbook of parenting: Vol. 3: Being and becoming a parent. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2002. pp. 3–25. [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson PR, Karlof KL. Child, parent, and family predictors of latter adjustment in siblings of children with autism. Research in Autism Spectrum Disorders. 2008;2(4):583–600. [Google Scholar]
- Bernstein GA, Borchardt CM, Perwien AR. Anxiety disorders in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(9):1110–1119. doi: 10.1097/00004583-199609000-00008. [DOI] [PubMed] [Google Scholar]
- Bongers IL, Koot HM, van der Ende J, Verhulst FC. The normative development of child and adolescent problem behavior. Journal of Abnormal Psychology. 2003;112(2):179–192. doi: 10.1037/0021-843x.112.2.179. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S. Editorial: Anxiety of childhood and adolescence: Challenges and opportunities. Clinical Psychology Review. 2006;26(7):813–816. doi: 10.1016/j.cpr.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, McNicol K, Doubleday E. Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review. 2006;26(7):817–833. doi: 10.1016/j.cpr.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. In: Hertzig ME, Farber EA, editors. Annual progress in child psychiatry and child development: 1997. Philadelphia, PA: Brunner/Mazel; 1998. pp. 319–331. [Google Scholar]
- Cents RAM, Tiemeier H, Luijk MPCM, Jaddoe VWV, Hofman A, Verhulst FC, et al. Grandparental anxiety and depression predict young children's internalizing and externalizing problems: The generation R study. Journal of Affective Disorders. 2011;128(1–2):95–105. doi: 10.1016/j.jad.2010.06.020. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dempsey AG, Llorens A, Brewton C, Mulchandani S, Goin-Kochel RP. Emotional and behavioral adjustment in typically developing siblings of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42(7):1393–1402. doi: 10.1007/s10803-011-1368-9. [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, Weisz JR. Concurrent validity of the Child Behavior Checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32(3):373–384. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot CD. Differential Ability Scales – Second Edition. Minneapolis, MN: Pearson; 2007. [Google Scholar]
- Fombonne E. The epidemiology of autism: A review. Psychological Medicine. 1999;29(4):769–786. doi: 10.1017/s0033291799008508. [DOI] [PubMed] [Google Scholar]
- Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological Bulletin. 1995;118(3):392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Gau SS, Chou M, Lee J, Wong C, Chou W, Chen M, et al. Behavioral problems and parenting style among Taiwanese children with autism and their siblings. Psychiatry and Clinical Neurosciences. 2010;64(1):70–78. doi: 10.1111/j.1440-1819.2009.02034.x. [DOI] [PubMed] [Google Scholar]
- Glasberg BA. The development of siblings’ understanding of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2000;30(2):143–156. doi: 10.1023/a:1005411722958. [DOI] [PubMed] [Google Scholar]
- Gold N. Depression and social adjustment in siblings of boys with autism. Journal of Autism and Developmental Disorders. 1993;23:147–163. doi: 10.1007/BF01066424. [DOI] [PubMed] [Google Scholar]
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(5):693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell FE. Regression modeling strategies. New York: Springer; 2001. [Google Scholar]
- Hastings RP. Behavioral adjustment of siblings of children with autism. Journal of Autism and Developmental Disorders. 2003;33(2):99–104. doi: 10.1023/a:1022290723442. [DOI] [PubMed] [Google Scholar]
- Hastings RP. Longitudinal relationships between sibling behavioral adjustment and behavior problems of children with developmental disabilities. Journal of Autism and Developmental Disorders. 2007;37(8):1485–1492. doi: 10.1007/s10803-006-0230-y. [DOI] [PubMed] [Google Scholar]
- Huang LN. Family communication patterns and personality characteristics. Communication Quarterly. 1999;47(2):230–243. [Google Scholar]
- Hurley RSE, Losh M, Parlier M, Reznick JS, Piven J. The broad autism phenotype questionnaire. Journal of Autism and Developmental Disorders. 2007;37(9):1679–1690. doi: 10.1007/s10803-006-0299-3. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Research. 2000;94(2):93–102. doi: 10.1016/s0165-1781(00)00145-1. [DOI] [PubMed] [Google Scholar]
- Keiley MK, Bates JE, Dodge KA, Pettit GS. A cross-domain growth analysis: Externalizing and internalizing behaviors during 8 years of childhood. Journal of Abnormal Child Psychology. 2000;28:161–179. doi: 10.1023/a:1005122814723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly L, Keaten JA, Finch C, Duarte IB, Hoffman P, Michels MM. Family communication and the development of reticence. Communication Edition. 2002;51(2):202–209. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distribution of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLeod JD. Sex differences in vulnerability to undesirable life events. American Sociological Review. 1984;49:620–631. [Google Scholar]
- King MD, Bearman PS. Socioeconomic status and the increased prevalence of autism in California. American Sociological Review. 2011;76(2):320–346. doi: 10.1177/0003122411399389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Lopez N. Social anxiety among adolescents: Linkages with peer relations and friendships. Journal of Abnormal Child Psychology. 26:83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- Lainhart JE. Psychiatric problems in individuals with autism, their parents and siblings. International Review of Psychiatry. 1999;11(4):278–298. [Google Scholar]
- Landman-Peeters KMC, Hartman CA, van der Pompe G, den Boer JA, Minderaa RB, Ormel J. Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Social Science & Medicine. 2005;60(11):2549–2559. doi: 10.1016/j.socscimed.2004.10.024. [DOI] [PubMed] [Google Scholar]
- Last CG, Perrin A, Hersen M, Kazdin AE. DSM-III-R anxiety disorders in children: Sociodemographic and clinical characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:1070–1076. doi: 10.1097/00004583-199211000-00012. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Archives of General Psychiatry. 2006;63(6):694–701. doi: 10.1001/archpsyc.63.6.694. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, et al. Autism diagnostic observation schedule: A standardized observation of communicative and social behavior. Journal of Autism and Developmental Disorders. 1989;19:185–212. doi: 10.1007/BF02211841. [DOI] [PubMed] [Google Scholar]
- McClure EB, Brennan PA, Hammen C, Le Brocque RM. Parental anxiety disorders, child anxiety disorders, and the perceived parent–child relationship in an Australian high-risk sample. Journal of Abnormal Child Psychology. 2001;29(1):1–10. doi: 10.1023/a:1005260311313. [DOI] [PubMed] [Google Scholar]
- Merikangas KR. Familial factors and substance use disorder. In: McMahon RJ, Peters RD, editors. The effects of parental dysfunction on children. New York: Kluwer Academic/Plenum Publishers; 2002. pp. 17–40. [Google Scholar]
- Micali N, Chakrabarti S, Fombonne E. The broad autism phenotype. Autism. 2004;8(1):21–37. doi: 10.1177/1362361304040636. [DOI] [PubMed] [Google Scholar]
- Mullen EM. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Services, Inc.; 1995. [Google Scholar]
- Neece CL, Blacher J, Baker BL. Impact on siblings of children with intellectual disability: The role of child behavior problems. American Journal on Intellectual and Developmental Disabilities. 2010;115(4):291–306. doi: 10.1352/1944-7558-115.4.291. [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Kuo H, Seltzer MM. Siblings of individuals with an autism spectrum disorder: Sibling relationships and wellbeing in adolescence and adulthood. Autism. 2009;13(1):59–80. doi: 10.1177/1362361308097119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmond GI, Seltzer MM. Adolescent siblings of individuals with an autism spectrum disorder: Testing a diathesis-stress model of sibling well-being. Journal of Autism and Developmental Disorders. 2009;39(7):1053–1065. doi: 10.1007/s10803-009-0722-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parke RD. Fathers and families. In: Bernstein MH, editor. Handbook of parenting: Vol. 3: Being and becoming a parent. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2002. pp. 27–74. [Google Scholar]
- Petalas MA, Hastings RP, Nash S, Hall LM, Joannidi H, Dowey A. Psychological adjustment and sibling relationships in siblings of children with Autism Spectrum Disorders: Environmental stressors and the Broad Autism Phenotype. Research in Autism Spectrum Disorders. 2012;6:546–555. [Google Scholar]
- Pilowsky T, Yirmiya N, Doppelt O, Gross-Tsur V, Shaley RS. Social and emotional adjustment of siblings of children with autism. Journal of Child Psychology and Psychiatry. 2004;45(4):855–865. doi: 10.1111/j.1469-7610.2004.00277.x. [DOI] [PubMed] [Google Scholar]
- Piven J, Chase GA, Landa R, Wzored M, Gayle J, Cloud D, et al. Psychiatric disorders in the parents of autistic individuals. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30(3):471–478. doi: 10.1097/00004583-199105000-00019. [DOI] [PubMed] [Google Scholar]
- Rosbrook A, Whittingham K. Autistic traits in the general population: What mediates the link with depressive and anxious symptomatology? Research in Autism Spectrum Disorders. 2010;4(3):415–424. [Google Scholar]
- Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: A 14-year follow-up during childhood, adolescence, and young adulthood. The American Journal of Psychiatry. 2003;160(12):2116–2121. doi: 10.1176/appi.ajp.160.12.2116. [DOI] [PubMed] [Google Scholar]
- Rutter M, LeCouteur A, Lord C. The Autism Diagnostic Interview-Revised (ADI-R) Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Simons Foundation. SFARI Base/SSC Researcher Welcome Packet. New York, NY: Simons Foundation; 2010. [Google Scholar]
- Smalley SL, McCracken J, Tanguay P. Autism, affective disorders, and social phobia. American Journal of Medical Genetics (Neuropsychiatric Genetics) 1995;60:19–26. doi: 10.1002/ajmg.1320600105. [DOI] [PubMed] [Google Scholar]
- Snow AV, Lecavalier L. Comparing autism, PDD-NOS, and other developmental disabilities on parent-reported behavior problems: Little evidence for ASD subtype validity. Journal of Autism and Developmental Disorders. 2011;41:302–310. doi: 10.1007/s10803-010-1054-3. [DOI] [PubMed] [Google Scholar]
- Spratt KG, Nicholas JS, Brady KT, Crpenter LA, Hatcher CR, Meekinds KA, et al. Enhanced cortisol response to stress in children in autism. Journal of Autism and Developmental Disorders. 2012;42:75–81. doi: 10.1007/s10803-011-1214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Psychological Corporation. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- United States Census Bureau. Household and families: 2010. (2010 Census Briefs No. 14) 2012 Retrieved on July 23, 2012 from http://www.census.gov/prod/cen2010/briefs/c2010br-14.pdf.
- United States Census Bureau. Household income for states: 2009 and 2010. (American Community Service Briefs No. 10-02) 2011 Retrieved on July 23, 2012 from http://www.census.gov/prod/2011pubs/acsbr10-02.pdf.
- van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: The TRIALS study. Journal of Child Psychology and Psychiatry. 2009;50(10):1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- Verte S, Roeyers H, Buysse A. Behavioural problems, social competence, and self-concept in siblings of children with autism. Child: Care, Health, and Development. 2003;29(3):193–205. doi: 10.1046/j.1365-2214.2003.00331.x. [DOI] [PubMed] [Google Scholar]
- Visu-Petra L, Tincas I, Cheie L, Benga O. Anxiety and visual-spatial memory updating in young children: An investigation using emotional facial expressions. Cognition and Emotion. 2010;24(2):223–240. [Google Scholar]
- Vitiello B, Waslick B. Pharmacotherapy for children and adolescents with anxiety disorders. Psychiatric Annals. 2010;40(4):185–191. [Google Scholar]
- Wadsworth ME, Hudziak JJ, Heath AC, Achenbach TM. Latent class analysis of child behavior checklist anxiety/depression in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(1):106–114. doi: 10.1097/00004583-200101000-00023. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligencescale for children. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychological Medicine. 1998;28:109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- Yirmiya N, Shaked M, Erel O. Comparison of siblings of individuals with autism and siblings of individuals with other diagnoses: An empirical summary. In: Schopler E, Yirmiya N, Schulman C, Marcus LM, editors. The research basics for autism intervention. New York: Kluwer Academic/Plenum Publishers; 2001. pp. 59–73. [Google Scholar]