Abstract
Background
Little is known about whether neighborhood factors are associated with HPV vaccine uptake, especially among disadvantaged groups that can benefit most from the vaccine.
Methods
We used data collected from immigrant, low-income mothers of adolescent girls and data from the 2005–2009 American Community Survey to investigate the relationship between HPV vaccine initiation and neighborhood characteristics. We compared initiation rates across levels of neighborhood disadvantage and employed multilevel logistic regression models to examine contextual effects on uptake.
Results
Overall, 27% of girls (n=479) initiated the vaccine. Initiation rates were highest among girls from the most disadvantaged neighborhoods (30%), however, neighborhood factors were not independently associated with vaccine initiation after adjusting for individual factors. Mother’s awareness of HPV, age, and insurance status were strong predictors for initiation.
Conclusions
Future interventions should focus on improving awareness among low-income mothers as well as targeting vulnerable families outside the catchment area of public programs.
Keywords: Human Papillomavirus (HPV) Vaccine, Cervical Cancer, Neighborhood Characteristics, Immigrant, Low Income
INTRODUCTION
The American Cancer Society estimates that 12,710 new cases and 4,220 deaths from cervical cancer will occur in 2012 [1]. Cervical cancer is unevenly distributed across socioeconomic status, racial/ethnic groups, and geography [2–5]. Despite the widespread adoption of Pap testing, disadvantaged groups often have much lower rates of screening compared to the general population [6–8]. While many studies link low screening rates to individual health insurance status, socioeconomic status, English proficiency, and lack of awareness [9, 10], an increasing number of studies also consider cervical cancer disparities to be markers of larger social inequalities rooted in the context of geographically-based characteristics [7, 11–13].
The recently available human papillomavirus (HPV) vaccines provide an opportunity for a new generation of adolescents to be protected from high risk HPV infection and cervical cancer [14]. Unless the vaccine is adopted by all subgroups, including girls that are most at risk for cervical cancer, disparities will likely remain. Recent national data indicate HPV vaccination rates are low among all groups. Only 53% of girls in the U.S. initiated the vaccine in 2011 and just under 35% completed the 3-dose series [15].
Most HPV vaccine studies to date have focused on individual level factors related to uptake. Little is known about whether neighborhood factors influence HPV vaccine initiation among disadvantaged adolescent girls [16–24]. Research in other areas has examined the influence of neighborhood characteristics on individual health status and health behaviors through a variety of pathways related to residential segregation, community level exposure to disease, availability of health care resources, and social capital [25–30]. By conceptualizing the influence of neighborhood disadvantage on HPV vaccination to be similar to other health services utilization scenarios, neighborhood disadvantage may be inversely associated with vaccine initiation. Lower vaccine uptake among girls in disadvantaged neighborhoods could be due to increased economic or logistical barriers associated with not having a usual source of care and fewer health care resources [31]. Similarly, lower uptake among girls in predominantly ethnic minority neighborhoods may be due to limited access to new health information or awareness of vaccination services [32].
On the contrary, disadvantaged neighborhoods are also targeted for the placement of safety-net services, including vaccination services, and girls from these neighborhoods may actually have more access to the vaccine. Furthermore, the Vaccines for Children (VFC) Program subsidizes vaccines for low-income children thereby reducing the economic barriers to the vaccine for disadvantaged groups [33]. The VFC Program often covers new vaccines soon after recommendations are passed by the Advisory Committee on Immunization Practices. This allows new vaccines to be available for low-income girls even before the vaccines are covered under commercial insurance programs. In addition, social networks might also facilitate the dissemination of information and acceptability of the vaccine among parents of low-income, ethnic minority girls living in predominantly minority neighborhoods [32, 34, 35].
These competing hypotheses make it unclear whether the usual relationship between neighborhood disadvantage and lower uptake of health services holds in the case of HPV vaccination among low-income girls living in predominantly disadvantaged neighborhoods. The few recent studies that examined whether neighborhood factors were associated with HPV vaccine uptake demonstrated conflicting results and did not focus on underserved populations. Chao et al found that girls living in poorer neighborhoods were less likely to initiate the vaccine [36] while Pruitt and Schootman showed girls living in poorer counties to be more likely to initiate the vaccine [37]. These studies had limited samples of low-income, minority girls and also used varying units of geography.
This study extends the current cervical cancer disparity literature by employing a social-ecological perspective, which focuses on external factors related an individual’s neighborhood or environment that could influence one’s health, to examine whether neighborhood socio-demographic characteristics are significantly associated with HPV vaccine initiation after controlling for individual level factors.
METHODS
This multi-level analysis combined individual level data from a telephone survey with data from the U.S Census Bureau. Survey respondents were geocoded to their census tracts to obtain estimates of neighborhood characteristics.
Individual Level Data
This study employed individual level data previously collected from low-income caregivers of adolescent girls eligible for the HPV vaccine (ages 9 – 18 years). All study participants were recruited from the Los Angeles County Department of Public Health (LACDPH) Office of Women’s Health (OWH) telephone hotline. Study participants completed interviews between January and November 2009. The OWH multi-language toll-free hotline provides services, such as scheduling of cervical and breast cancer screening appointments and providing health information, to low-income (<200% federal poverty level) and uninsured women. Callers of the hotline are women who routinely use the Los Angeles County (LAC) safety-net system.
Details of the study design have been previously reported [38]. Briefly, eligibility criteria included any female caller between 18 and 65 years and the medical decision-maker for at least one HPV vaccine-eligible adolescent girl (9–18 years) in the household. Among eligible callers, 93% (n=490) provided informed consent to answer a survey. This data, therefore, represents nearly all OWH hotline callers who make medical decisions for at least one adolescent girl. Because 85% of women who participated in the study were mothers, rather than grandmothers, aunts, or sisters, study participants are referred to as “mothers” for simplicity. Mothers completed a 75-item telephone survey to assess their daughters’ HPV vaccine uptake and correlates of uptake. An important feature of this survey is that mothers provided their home addresses, allowing for geographic analyses. A $10 grocery card incentive was provided for each study participant.
Neighborhood Level Data
Geo-coded addresses of adolescent girls from the individual level data were linked to census tracts. Census tract characteristics were derived from the 2005–2009 American Community Survey [39]. While census tracts have some limitations, prior studies have shown that census-tract level neighborhood data provide the most sensitive measures of neighborhood health disparities and are most easily linkable to other datasets [11]. In addition, geographical units from the census are relatively permanent and follow visible and political boundaries (e.g. counties, cities) [40]. A major value of using census tracts for research purposes is that they allow for replication across studies.
Measures
Our measures included both individual characteristics of mothers and daughters, as reported by each mother, and neighborhood characteristics associated with their place of residence.
HPV vaccine initiation was defined as a dichotomous (yes/no) outcome for whether daughters received at least one dose of the quadrivalent HPV vaccine. Daughters were classified as “initiated” (yes) if they had at least one dose of the vaccine. They were classified as “uninitiated” (no) if they had no receipt of the vaccine or if the mother had no awareness of the vaccine. Eleven mothers reported having never heard of the HPV vaccine prior to the interview despite also reporting their daughters had received at least one dose of the HPV vaccine; these girls were still classified into the initiated group.
Other characteristics included the daughter’s age, insurance type, and usual source of care. For daughter’s age, we used the Advisory Committee on Immunization Practices recommendations for HPV vaccines [41] to transform the continuous age of adolescent girls to a categorical variable (9–10 years – pre-recommendation age group, 11–18 years – recommended age group) [14]. In addition, we control for mother’s race/ethnicity, age, and awareness of HPV. Mother’s HPV awareness was a dichotomous (yes/no) variable determined by asking all mothers the following: “Have you ever heard of HPV? HPV stands for Human Papilloma virus.”
We included a number of neighborhood socio-demographic factors for this study based on previously defined measures used for neighborhood disadvantage [26, 31] as well as prior literature related to neighborhood influence on use of cancer screening and vaccination [6, 7, 37]. The following neighborhood factors were included: percentage of census tract residents living below the federal poverty level, percentage of unemployed census tract residents over age 16, percentage of minority race/ethnicity census tract residents (i.e. those who were not Non-Hispanic white), and percentage of census tract residents without access to a private vehicle. Percentage living below poverty was categorized into quartiles based on the distribution of poverty rates across census tracts. The measures for neighborhood racial/ethnic composition, unemployment, and access to a private vehicle were converted to standardized coefficients for ease of interpretation. The coefficients for these variables were standardized to have a mean of zero and a variance of 1. This allows the beta coefficients to be interpreted as the change in vaccine initiation associated with every standard deviation change in the percent of each neighborhood characteristic (i.e. minority composition, unemployment, access to vehicle).
Statistical Analysis
Initial descriptive statistics were conducted to describe the study sample and to examine the distribution of the primary outcome and predictor variables. Bivariate logistic regression models were used to examine the association between individual level predictors and vaccine uptake.
A random-effects multilevel logistic regression model was employed to examine the association between individual and neighborhood level variables on vaccine uptake while adjusting for the correlation between individuals living within the same census tract. We obtained odds ratios for the following logistic regression models: (1) individual level variables only, (2) neighborhood level variables only and (3) individual and neighborhood level variables together. The final neighborhood variables for Models 2 and 3 included poverty categorized into distributional quartiles and the standardized coefficient for percentage of minority residents. Statistical significance for beta coefficients will be determined at the p<0.05 level. Results are reported in odds ratios and 95% confidence intervals.
This study was approved by the UCLA Institutional Review Board.
RESULTS
Sample Characteristics
Over half (53%) of mothers in the sample (n=479) were Latina and a third (32%) were Asian within this low-income sample (Table 1). One-third of mothers reported their daughters did not have insurance or a usual source of care. Over a quarter (27%) of all daughters in the sample initiated the HPV vaccine. The highest initiation rate was among Latinas (33%), with Chinese, Korean, and African American at lower initiation rates ranging from 21% to 25%. A larger proportion of daughters in the older age group, those with public insurance, and those with mothers who were aware of HPV had initiated the vaccine.
Table 1.
Demographic and health care characteristics of study participants
| Characteristic | Total Sample % (n) | Initiated HPV Vaccine % (n) | No Initiation of HPV Vaccine % (n) |
|---|---|---|---|
|
| |||
| Mothers/Caregivers | |||
|
| |||
| Total | 100.0 (479) | 26.9 (129) | 73.1 (350) |
| Race/ethnicity | |||
| Latina | 53.1 (243) | 32.5 (79) | 67.5 (164) |
| Chinese | 19.0 (87) | 25.3 (22) | 74.7 (65) |
| Korean | 13.1 (60) | 21.7 (13) | 78.3 (47) |
| African American | 8.3 (38) | 21.1 (8) | 78.9 (30) |
| Other race | 6.6 (30) | 23.3 (7) | 76.7 (23) |
| Interview Language | |||
| Spanish | 47.4 (217) | 33.2 (72) | 66.8 (145) |
| Chinese | 21.0 (96) | 22.8 (18) | 77.2 (61) |
| Korean | 13.3 (61) | 19.7 (12) | 80.3 (49) |
| English | 17.3 (79) | 28.1 (27) | 71.9 (69) |
| Education | |||
| < High School Diploma | 50.5 (242) | 29.8 (72) | 70.2 (170) |
| High School Diploma or more | 49.5 (237) | 24.1 (57) | 75.9 (180) |
| Nativity | |||
| Foreign-born | 87.7 (420) | 27.6 (116) | 72.4 (304) |
| Born in U.S. | 12.3 (59) | 22.0 (13) | 78.0 (46) |
| Percent Life in U.S> | |||
| < 25% life spent in U.S. | 16.5 (79) | 20.3 (16) | 79.8 (63) |
| >=25% time spent in U.S. | 83.5 (400) | 28.3 (113) | 71.8 (287) |
| Mother Heard of HPV | |||
| Yes | 62.1 (284) | 41.6 (118) | 58.5 (166) |
| No | 37.9 (173) | 5.6 (11) | 94.4 (184) |
| Age (mean, SD) | 43.9 (7.1) | 43.4 (7.3) | 44.1 (321) |
|
| |||
| Vaccine-eligible daughters | |||
|
| |||
| Age | |||
| 9–10 years | 14.6 (70) | 5.7 (4) | 94.3 (66) |
| 11–12 years | 19.6 (94) | 28.7 (27) | 71.3 (67) |
| 13–18 years | 65.8 (315) | 31.1 (98) | 68.9 (217) |
| Insurance status | |||
| No Insurance | 32.2 (154) | 19.6 (22) | 80.4 (132) |
| Public | 56.8 (272) | 33.1 (90) | 66.9 (182) |
| Private | 11.1 (53) | 22.6 (12) | 77.4 (41) |
| Have Usual Source of Care | |||
| Yes | 65.6 (314) | 31.9 (100) | 68.2 (214) |
| No | 34.5 (165) | 17.6 (29) | 82.4 (136) |
Neighborhood Characteristics of Sample Compared to Los Angeles County
An average of 1.4 girls (range: 1–7) was clustered within each census tract (i.e. 341 unique neighborhoods for the 483 individual girls). Characteristics of sampled neighborhoods (n=341) were compared to the broader Los Angeles County in several ways (Table 2). Our neighborhoods were similar with regards to the composition of non-Latino whites and the proportion of residents without access to a private vehicle. For example, 11% people in our neighborhoods and 10% of the County neighborhoods did not have access to a private vehicle. However, neighborhoods in the sample had a larger proportion of ethnic minorities (87%) compared all neighborhoods within LA County (70%).
Table 2.
Characteristics of Study Neighborhoods Compared to All Neighborhoods in Los Angeles County, 2005–2009 American Community Survey
| HPV Sample (n=341 census tracts) | LA County (n=2,054 census tracts) | |
|---|---|---|
|
| ||
| Neighborhood Characteristic | Mean % (SD)* | Mean % (SD)* |
|
| ||
| SES | ||
| Living Below Poverty^ | 19 (12) | 16 (12) |
| Unemployed^ | 42 (6) | 41 (9) |
| RACE/ETHNICITY | ||
| Minority^ | 87 (17) | 70 (28) |
| Latino^ | 55 (29) | 46 (30) |
| Non-Latino African American^ | 11 (17) | 8 (14) |
| Non-Latino Asian^ | 17 (22) | 13 (15) |
| Non-Latino Other Race | 2 (2) | 2 (2) |
| Non-Latino White^ | 14 (18) | 30 (28) |
| TRANSPORTATION | ||
| No access to vehicle | 11 (9) | 10 (10) |
Mean values represent average percentages of each neighborhood characteristic across sample and county census tracts.
Mean % for sample neighborhoods significantly different from LAC neighborhoods at p<0.01 level
Neighborhood Characteristics and HPV Vaccine Initiation
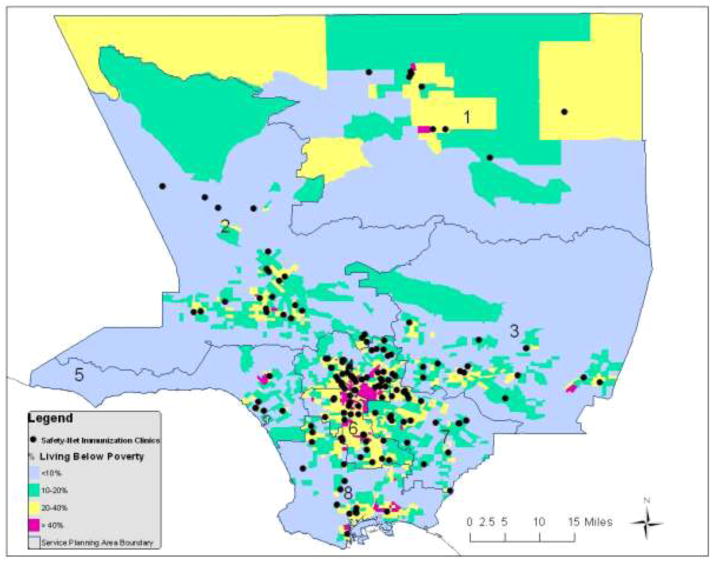
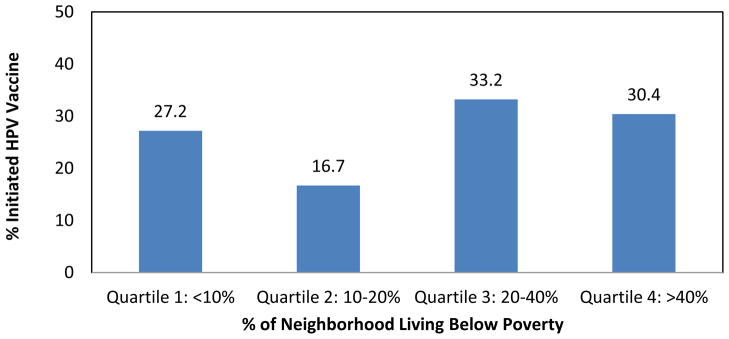
Rates of initiation were highest among girls living in neighborhoods with higher poverty (Figure 1). Surprisingly, girls in the second to lowest poverty quartile (Quartile 2) had the lowest rates of initiation (16.7%) compared to girls in other neighborhoods. These differences were significant at the p<0.05 level. For percentage of minority residents within neighborhoods (Figure 2) and percentage of unemployed residents within neighborhoods (Figure 3) rates of initiation were highest among girls in the neighborhoods with the greatest proportion of minorities and the highest unemployment rates. The difference in rates of initiation between neighborhoods with the greatest access to vehicles and least access to vehicles was only 5% and not statistically significant (data not shown).
Figure 1.
HPV Vaccine Initiation Rates by Neighborhood Poverty
Figure 2.
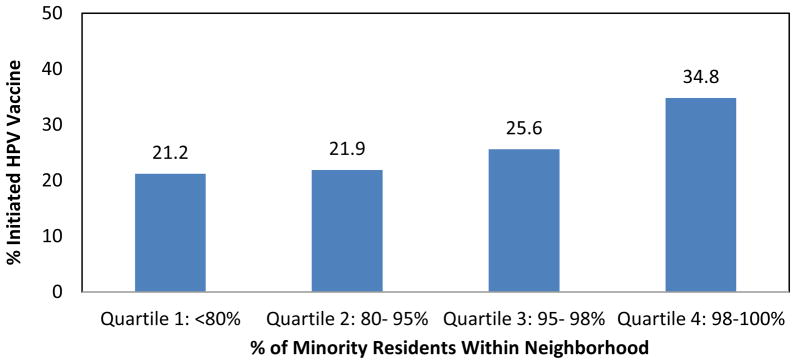
HPV Vaccine Initiation Rates by Neighborhood Racial/ethnic Composition
Figure 3.
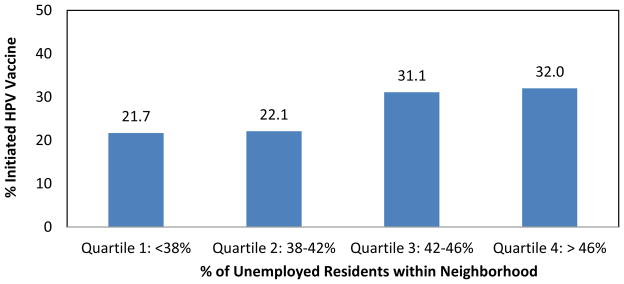
HPV Vaccine Initiation Rates by Neighborhood Unemployment Rate
Bivariate and Multivariate Results
Unadjusted odds ratios for neighborhood-level variables on HPV vaccine initiation are shown in Table 3. Girls living in neighborhoods with poverty rates between 10–20% (Quartile 2) had 0.50 times the odds of initiating the HPV vaccine compared to girls living in other neighborhoods (p<0.05). On the other hand, girls living in neighborhoods with poverty rates greater than 30% (Quartile 4) had 1.79 times the odds of initiating the HPV vaccine compared to girls living in other neighborhoods. The percentage of unemployed residents and the percentage of minority residents were also both positively associated with HPV vaccine initiation at the bivariate level.
Table 3.
Bivariate and Multivariate Associations between Neighborhood Characteristics and HPV Vaccine Initiation
| Bivariate Analysis | Model 1: Individual Level Covariates | Model 2*: Neighborhood Level Covariates | Model 3**: Individual + Neighborhood | |
|---|---|---|---|---|
|
| ||||
| Mother/Caregiver | ||||
| Latino (Ref: Non-Latino) | 1.59 (1.05–2.41) | 1.68 (1.03, 2.72) | 1.52 (0.87, 2.66) | |
| Heard of HPV (Ref: No) | 11.9 (6.19–22.8) | 10.31 (5.28, 20.1) | 10.39 (4.99, 21.6) | |
|
| ||||
| Adolescent Girl | ||||
| Age 11–18 (Ref: 9–10) | 7.26 (2.59–20.4) | 9.42 (3.24, 27.4) | 9.56 (3.16, 29.1) | |
| Insurance status | ||||
| Uninsured | 0.46 (0.29–0.75) | 1.0 | 1.0 | |
| Public | 2.13 (1.39–3.27) | 1.91 (1.10, 3.20) | 1.91 (1.08, 3.41) | |
| Private | 0.77 (0.39–1.52) | 1.19 (0.50, 2.80) | 1.17 (0.49, 2.79) | |
|
| ||||
| Neighborhood Characteristic | ||||
| % Poverty Quartiles | ||||
| 1 (<10%, Low Poverty) | 0.99 (0.61, 1.60) | 0.95 (0.44, 2.07) | 0.94 (0.39, 2.23) | |
| 2 (10–20%) | 0.50 (0.30, 0.85) | 0.47 (0.23, 0.93) | 0.53 (0.25, 1.14) | |
| 3 (20–40%) | 1.01 (0.63, 1.64) | 0.70 (0.38, 1.29) | 0.64 (0.36, 1.21) | |
| 4 (>40%, High Poverty) | 1.79 (1.13, 2.82) | 1.0 | 1.0 | |
| STD_Minority^ | 1.30 (1.00, 1.69) | 1.28 (0.93, 1.78) | 1.09 (0.77, 1.54) | |
| STD_Unemployment^ | 1.32 (1.04, 1.68) | |||
| STD_No Vehicle Access^ | 1.10 (0.87, 1.39) | |||
|
| ||||
| Intraclass Correlation | 0.045 | 0.109 | 0.014 | |
Neighborhood models used logistic regression with robust standard errors.
Two-level models used xtlogit random effects model
Standardized coefficients (Odds ratios represent change in one standard deviation above mean)
Results from the multivariate analyses are also shown in Table 3. Mother’s awareness of HPV, age of adolescent girl, having public health insurance, and Latina ethnicity were significantly associated with increased odds of vaccine uptake at the individual level (Model 1); these findings were similar to prior publications focusing on individual level predictors for HPV vaccine initiation using this same dataset [16]. In the ecologic model (Model 2), girls living in moderately low-income neighborhoods (Quartile 2: 10–20% poverty) had 0.47 times the odds of receiving the HPV vaccine compared to girls who lived lowest income neighborhoods (Quartile 4: >40% poverty). In the multilevel model (Model 3), only mother’s awareness of HPV, age of adolescent girl, and having public insurance remained significant predictors of vaccine initiation. Results were similar when the multilevel model included only mothers aware of the HPV vaccine (data not shown).
DISCUSSION
In this study of low-income, ethnic minority girls, neighborhood socio-demographic factors were not significantly associated with HPV vaccine initiation after controlling for individual level factors. Our findings were not consistent with the two previous studies focused on neighborhood factors and HPV vaccine initiation [36, 37]. The lack of a significant association may be related to our unique sample of low-income girls with mothers who already use safety-net services through the county health system. These mothers may be intrinsically more motivated to overcome the influences of neighborhood disadvantage on accessing safety-net services as they already utilize safety-net services for themselves. For this population of girls, neighborhood context may be less important than other factors such as mother’s awareness of HPV and adequate insurance coverage for vaccination services. Furthermore, there may have been limited variability within our sample neighborhoods of mostly disadvantaged areas.
Findings from our descriptive analyses revealed higher rates of vaccine initiation among girls living in the most disadvantaged neighborhoods. Further research is needed to confirm whether low-income girls living in relatively less impoverished neighborhoods face additional barriers to accessing the HPV vaccine compared to low-income girls living in the most impoverished neighborhoods. Contrary to the expected direct relationship between increasing neighborhood advantage and positive health outcomes or behaviors, these observations may be explained by the increased density of safety-net immunization services in the most impoverished areas and access to subsidized vaccines via the VFC program [42]. However, these neighborhood factors did not remain significant after controlling for individual factors and thus warrant additional investigation.
Girls in our sample living in less disadvantaged neighborhoods may lack nearby safety-net clinics where they can access the HPV vaccine. These inferences are supported by a recent report using the same 2005–2009 American Community Survey data employed in our study, which showed an increasing shift in concentrated poverty within suburban areas in the late 2000s [43]. This report, along with others, indicate that the suburban poor often face barriers to resources that are similar to the urban poor but experience an added barrier of having fewer safety-net resources available in their immediate neighborhood [34, 43, 44]. A more in-depth geographic examination of census tracts in the county indicated neighborhoods that are moderately low-income in Los Angeles County appear to be located outside the immediate urban center and in more suburban areas (Figure 5), supporting the possibility that low-income girls in moderately impoverished areas may face additional barriers to vaccination services.
Figure 5.
Neighborhood Poverty Quartiles by Census Tracts in Los Angeles County
The positive relationship between having public insurance (i.e. Medicaid or Healthy Kids) and higher odds of vaccine initiation may serve as a proxy measure for having a usual and affordable source of care for girls in the sample. Those with insurance coverage are more likely to receive any type of recommended vaccinations [45], especially if they rely on safety-net clinics that are traditionally focused on preventive care for adolescents. Low-income girls with private insurance, however, often face additional out-of-pocket costs for vaccinations as well as increased barriers to care [46]. Multiple studies have documented the sizeable increase in the costs of adolescent vaccinations over the past decade and how these costs have been passed on from insurance companies to patients [42, 47]. Furthermore, recent studies have also noted that low reimbursement rates for HPV vaccines as well as other market factors have prevented doctors from recommending or providing adolescent immunizations [48, 49]. Our study findings, combined with others, indicate a need to continue to focus on promoting vaccinations services for girls who are uninsured or who may be underinsured.
Some study limitations should be noted. First, due to the modest sample size and a small number of girls per neighborhood, our study serves as an initial exploration of neighborhood factors on HPV vaccine uptake. Larger samples of girls and neighborhoods would yield greater statistical power for multi-level analyses. As with many area-based studies, our analysis relied on census tracts as a proxy measure for neighborhood boundaries. While census tracts have been shown to be adequate proxies for measuring area-level factors, qualitatively defined neighborhood boundaries may be more suitable for low-income, ethnic minority populations. In addition, there may be limited variability within our study sample of low-income girls with mothers that called into a county health hotline. Lastly, due to the cross sectional nature of this data and inability to measure residential mobility, temporality may be an issue in the relationships between neighborhood factors and vaccine uptake. However, we did attempt to use temporally aligned neighborhood level data by linking to the 2005–2009 American Community Survey, rather than the 2000 Census, because the individual level data was collected in 2009.
This study continues to show the need to improve HPV vaccine initiation rates among the most disadvantaged groups, especially given the much lower initiation rates seen in our study sample (27%) compared to nationally reported rates. Interventions aimed to increase vaccine uptake among vulnerable populations should focus on improving awareness of HPV vaccines among mothers as well as providing adequate health care coverage to underserved populations [45]. In addition, given the recently recommended set of adolescent vaccinations, it is important that safety-net clinics serving vulnerable populations maximize adolescent clinic visits as opportunities to provide the HPV vaccine [24]. Lastly, lower vaccination rates among disadvantaged girls living in relatively less impoverished neighborhoods point to the importance of targeting vulnerable populations both within the highest need areas as well as within less impoverished areas where disadvantaged girls may face additional barriers to accessing care.
CONCLUSIONS
This study is one of the first to explore the relationship between neighborhood socio-demographic characteristics and HPV vaccine initiation among low-income, minority girls. By focusing on this high-risk population, study results contribute to the current understanding of neighborhood context in relation to vaccine uptake. As stated in prior research, merely targeting the poorest areas to increase uptake of cancer prevention services may leave out a large proportion of the low-income population that otherwise could benefit from preventive services [50]. Future interventions should consider low-income adolescent girls living outside the catchment area of safety-net services that may face additional barriers to accessing vaccination services.
Acknowledgments
This study was supported by the UCLA NIH/NCI R25 Cancer Education and Career Development Program and the AHRQ Grants for Health Services Research Dissertation Program (1-R36-HS020172-01). We would like to thank the Office of Women’s Health hotline operators for conducting the telephone surveys and the mothers who participated in the study.
References
- 1.American Cancer Society; A.C. Society, editor. Cancer Facts and Figures 2012. Atlanta: 2012. [Google Scholar]
- 2.Freeman HP, Wingrove BK. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. National Cancer Institute, Center to Reduce Cancer Health Disparities; Rockville, MD: 2005. [Google Scholar]
- 3.Krieger N, et al. Social class, race/ethnicity, and incidence of breast, cervix, colon, lung, and prostate cancer among Asian, Black, Hispanic, and White residents of the San Francisco Bay Area, 1988–92 (United States) Cancer Causes Control. 1999;10(6):525–37. doi: 10.1023/a:1008950210967. [DOI] [PubMed] [Google Scholar]
- 4.McDougall JA, et al. Racial and ethnic disparities in cervical cancer incidence rates in the United States, 1992–2003. Cancer Causes Control. 2007;18(10):1175–86. doi: 10.1007/s10552-007-9056-y. [DOI] [PubMed] [Google Scholar]
- 5.Saraiya M, et al. Cervical cancer incidence in a prevaccine era in the United States, 1998–2002. Obstet Gynecol. 2007;109(2 Pt 1):360–70. doi: 10.1097/01.AOG.0000254165.92653.e8. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin SS, et al. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Soc Sci Med. 2008;66(2):260–75. doi: 10.1016/j.socscimed.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Datta GD, et al. Individual-, neighborhood-, and state-level socioeconomic predictors of cervical carcinoma screening among U.S. black women: a multilevel analysis. Cancer. 2006;106(3):664–9. doi: 10.1002/cncr.21660. [DOI] [PubMed] [Google Scholar]
- 8.Tsui J, et al. Cervical cancer screening among foreign-born women by birthplace and duration in the United States. J Womens Health (Larchmt) 2007;16(10):1447–57. doi: 10.1089/jwh.2006.0279. [DOI] [PubMed] [Google Scholar]
- 9.Ponce NA, et al. Is there a language divide in pap test use? Med Care. 2006;44(11):998–1004. doi: 10.1097/01.mlr.0000233676.61237.ef. [DOI] [PubMed] [Google Scholar]
- 10.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Asian and Pacific Islander women in the United States, 1994–1997. Cancer Epidemiol Biomarkers Prev. 2000;9(6):597–603. [PubMed] [Google Scholar]
- 11.Krieger N, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy AM, et al. Racial/ethnic and socioeconomic disparities in mortality among women diagnosed with cervical cancer in New York City, 1995–2006. Cancer Causes Control. 2010 doi: 10.1007/s10552-010-9593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh GK, Miller BA. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health. 2004;95(3):I14–21. doi: 10.1007/BF03403660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CDC. MMWR Early Release. Centers for Disease Control and Prevention; 2007. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) pp. 1–24. [PubMed] [Google Scholar]
- 15.CDC. Morbidity and Mortality Weekly Report 2012. National, state, and local area vaccination coverage among adolescents aged 13 through 17 years - United States, 2011; pp. 671–677. [PubMed] [Google Scholar]
- 16.Bastani R, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1463–72. doi: 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Cates JR, et al. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. J Rural Health. 2009;25(1):93–7. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- 19.Constantine NA, Jerman P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: a representative statewide analysis. J Adolesc Health. 2007;40(2):108–15. doi: 10.1016/j.jadohealth.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Dempsey AF, et al. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. 2009;19(8):531–8. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health. 2009;45(5):528–31. doi: 10.1016/j.jadohealth.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Hughes J, et al. Disparities in how parents are learning about the human papillomavirus vaccine. Cancer Epidemiol Biomarkers Prev. 2009;18(2):363–72. doi: 10.1158/1055-9965.EPI-08-0418. [DOI] [PubMed] [Google Scholar]
- 23.Rosenthal SL, et al. Uptake of HPV vaccine: demographics, sexual history and values, parenting style, and vaccine attitudes. J Adolesc Health. 2008;43(3):239–45. doi: 10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 24.Tiro JA, et al. Multilevel correlates for human papillomavirus vaccination of adolescent girls attending safety net clinics. Vaccine. 2011 doi: 10.1016/j.vaccine.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 25.Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Soc Sci Med. 2000;51(8):1143–61. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- 26.Kawachi I, Berkman LF. Neighborhoods and Health. New York, NY: Oxford University Press; 2003. p. 352. [Google Scholar]
- 27.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Achat H, et al. Social networks, stress and health-related quality of life. Qual Life Res. 1998;7(8):735–50. doi: 10.1023/a:1008837002431. [DOI] [PubMed] [Google Scholar]
- 29.Borrell LN, et al. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33(2):398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- 30.Browning CR, Cagney KA, Wen M. Explaining variation in health status across space and time: implications for racial and ethnic disparities in self-rated health. Soc Sci Med. 2003;57(7):1221–35. doi: 10.1016/s0277-9536(02)00502-6. [DOI] [PubMed] [Google Scholar]
- 31.Kirby JB, Kaneda T. Neighborhood socioeconomic disadvantage and access to health care. J Health Soc Behav. 2005;46(1):15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- 32.Rogers EM. In: Diffusion of Innovations. Press F, editor. New York: Simon & Schuster New York; 2003. [Google Scholar]
- 33.CDC. ACIP-VFC Vaccine Resolutions for Vaccines to Prevent Human Papillomavirus. 2011:1–2. [Google Scholar]
- 34.Mobley LR, et al. Heterogeneity in mammography use across the nation: separating evidence of disparities from the disproportionate effects of geography. Int J Health Geogr. 2008;7:32. doi: 10.1186/1476-072X-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kawachi I, Berkman L. Social Cohesion, Social Capital, and Health, in Social Epidemiology. Oxford University Press; New York: 2000. pp. 174–190. [Google Scholar]
- 36.Chao C, et al. Correlates for human papillomavirus vaccination of adolescent girls and young women in a managed care organization. Am J Epidemiol. 2010;171(3):357–67. doi: 10.1093/aje/kwp365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pruitt SL, Schootman M. Geographic disparity, area poverty, and human papillomavirus vaccination. Am J Prev Med. 2010;38(5):525–33. doi: 10.1016/j.amepre.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bastani R, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev. 20(7):1463–72. doi: 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. American Community Survey. 2012 [cited 2012 March 10]; Available from: http://www.census.gov/acs/www/about_the_survey/american_community_survey/
- 40.U.S. Census Bureau. US Census Geographic Terms and Concepts, in 2008 Redistricting Data Prototype (Public Law 94–171) Summary File USC Bureau, Editor. Washington, D.C: 2008. [Google Scholar]
- 41.ACIP. ACIP Provisional Recommendations for HPV Vaccine. ACIP Meeting; October, 21, 2009; Atlanta, GA. 2009. [Google Scholar]
- 42.Smith PJ, et al. Underinsurance and adolescent immunization delivery in the United States. Pediatrics. 2009;124(Suppl 5):S515–21. doi: 10.1542/peds.2009-1542K. [DOI] [PubMed] [Google Scholar]
- 43.Kneebone E, Nadeau C, Berube A. The Re-Emergence of Concentrated Poverty: Metropolitan Trends in the 2000s. In: Brookings TMPPa., editor. The Brookings Institute; Washington D.C: 2011. (Metropolitan Opportunity Series). [Google Scholar]
- 44.Silver D, Blustein J, Weitzman BC. Transportation to Clinic: Findings from a Pilot Clinic-Based Survey of Low-Income Suburbanites. J Immigr Minor Health. 2010 doi: 10.1007/s10903-010-9410-0. [DOI] [PubMed] [Google Scholar]
- 45.Gowda C, Dempsey AF. Medicaid reimbursement and the uptake of adolescent vaccines. Vaccine. 2012 doi: 10.1016/j.vaccine.2011.12.097. [DOI] [PubMed] [Google Scholar]
- 46.Lavarreda SA, Brown ER, Bolduc CD. Underinsurance in the United States: an interaction of costs to consumers, benefit design, and access to care. Annu Rev Public Health. 2011;32:471–82. doi: 10.1146/annurev.publhealth.012809.103655. [DOI] [PubMed] [Google Scholar]
- 47.Bednarczyk RA, Birkhead GS. Reducing financial barriers to vaccinating children and adolescents in the USA. Curr Opin Pediatr. 2011;23(1):105–9. doi: 10.1097/MOP.0b013e328341ebbf. [DOI] [PubMed] [Google Scholar]
- 48.Freed GL, Cowan AE, Clark SJ. Primary care physician perspectives on reimbursement for childhood immunizations. Pediatrics. 2009;124(Suppl 5):S466–71. doi: 10.1542/peds.2009-1542F. [DOI] [PubMed] [Google Scholar]
- 49.Young JL, et al. Human papillomavirus vaccination recommendation may be linked to reimbursement: a survey of Virginia family practitioners and gynecologists. J Pediatr Adolesc Gynecol. 2011;24(6):380–5. doi: 10.1016/j.jpag.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 50.Schootman M, et al. Self-report by elderly breast cancer patients was an acceptable alternative to surveillance, epidemiology, and end results (SEER) abstract data. J Clin Epidemiol. 2005;58(12):1316–9. doi: 10.1016/j.jclinepi.2005.04.002. [DOI] [PubMed] [Google Scholar]