SUMMARY
The aim of this study was to explore how the level of shiftwork exposure during an individual’s working life might be related to subjectively reported sleep quality and timing during retirement. Telephone interviews regarding past employment and sleep timing and quality (among other variables) were conducted using a pseudo-random age-targeted sampling process. Subjective sleep quality was assessed using a telephone version of the Pittsburgh Sleep Quality Index. Timing of reported habitual bedtimes and rise-times were assessed using the Sleep Timing Questionnaire. Questions measuring morningness and subjective health were also given. Retired seniors (aged 65 years+, n=1113) were studied. Analysis was by analysis of variance, with shiftwork exposure in three bins [0 (n=387), 1–15 (n=371) and >15 years (n=355)], gender (n=634 male, 479 female) and former occupation [in two broad categories, ‘managerial’ (n=437) versus ‘other’ (n=676)] as factors. In retired shiftworkers, relative to retired day workers, past exposure to shiftwork was associated with higher (worse) PSQI scores by 0.96 units (1–15 years) and 0.61 units (>15 years) (main effect P=0.005). There were also main effects of gender and former occupation (males and managerials reporting better sleep), but neither variable interacted with shiftwork exposure. The timing of current mean habitual bedtimes and rise-times (and also the variance around them) were very similar for the three shiftwork exposure groups. The shiftwork exposure effect did not appear to be mediated by either morningness or current health. Prior exposure to shiftwork would appear to be related to currently reported sleep problems during retirement.
Keywords: aging, human, night shiftwork, old, shiftwork, sleep
INTRODUCTION
Homo sapiens is a diurnal species, hard-wired to spend much of the night in sleep (Moore, 1997). Having to work at night, and thus sleep during the day, is essentially an unnatural act, often requiring a circadian phase shift equivalent in magnitude, for example, to that of a flight from Moscow to Chicago (Monk, 2000). Moreover, even permanent night workers invariably revert to a diurnal orientation during their days off and are thus, in practice, experiencing repeated circadian phase shifts on a weekly basis, much as is the case for rotating shiftworkers (Knauth and Hornberger, 2003). Not surprisingly, while these profound circadian phase shifts are happening to the individual (perhaps repeatedly for several decades), sleep is often severely impaired. There are many empirical studies documenting the fact that shiftworkers sleep more poorly than day workers during their working lives, confirming the conventional wisdom of the shiftworkers themselves (Akerstedt, 2005; Drake et al., 2004). However, there are also data that suggest that the point can be overstated (Akerstedt et al., 2008). The present study addresses the question of whether (relative to retired day workers) former shiftworkers’ sleep is still impaired after they have retired, even though they are now able to sleep at night on a permanent basis. It also addresses the question of whether they actually choose to sleep at night during retirement. With a long history of having abnormal and/or irregular bedtimes and rise-times, as dictated by their shiftwork schedule, it is an empirical question as to whether retired shiftworkers have regular nighttime bedtimes and morning rise-times, or whether instead they have a more casual attitude to sleep timing than do retired day workers. A priori, it is possible that in the higher-exposure categories there may have developed (or had always been) a greater inherent flexibility in their 24-hour patterning of bed timings. In our 1970s study (Folkard et al., 1979) of night nurses using a questionnaire tapping into sleep timing flexibility (the Circadian Type Questionnaire: CTQ), we showed that flexible-sleep types showed greater physiological circadian adaptation to night work than did more rigid types. This might suggest that these types may naturally exhibit greater flexibility in their approach to sleep timing, and might thus remain shiftworkers more easily, but would still show such flexibility in their retirement years.
Although retirement per se has been found to improve sleep (Vahtera et al., 2009) (arguably because of the removal of the stress and temporal restraints of working life), it is well documented in the literature that older adults experience much greater fragility in their sleep than do younger adults. In older adults, the ‘deeper’ levels of sleep are less evident, there are more bouts of unwanted wakefulness during the night and there is a tendency to wake earlier than desired (Ancoli-Israel, 2005; Bliwise, 2005). Thus, the retired >65-year-old shiftworker represents an individual whose general age-related sleep fragility might allow any residual sleep impairment from shiftwork exposure to be revealed when compared to that of an equivalently aged retired day worker. From the literature, a monozygotic twins study (Ingre and Akerstedt, 2004), showing that a twin with a history of night work reports worse sleep than the corresponding twin without such a history, suggests that such a difference may indeed be apparent.
Because shiftwork-intolerant individuals can often (but not always) switch to a day-working job, any survey of shiftwork exposure must take into account the likelihood that individuals finding shiftwork particularly difficult might switch to day work early on in their careers. People who are able to undertake shiftwork for >15 years or so are the survivors who are still ‘left standing’, as it were, and still working shiftwork, even as they approach their middle-age years—a particularly vulnerable time of life regarding shiftwork coping ability (Monk, 2000). Thus, these survivors might comprise a particularly resilient group relative to those who have switched early on to day work, and who thus have less experience with shiftwork by the time they reach retirement. This effect has been observed in the cardiovascular findings of Knutsson and colleagues (Knutsson, 2003) and in our own study of the effects of shiftwork exposure on clinical depression (Scott et al., 1997), both of which showed a lessened risk in those with>20 years’ shiftwork exposure. Thus, rather than use a simple dichotomy between retired shiftworker and retired day worker, in the present analysis the shiftworker group was divided further into two exposure bins (1–15, >15 years) of roughly equal size, by considering the detailed work history which was taken from each subject over the telephone (see below). It should be recognized, however, that there are other reasons such as seniority in the position and career advancement that cause shiftworkers to change to day work.
This report is concerned with findings from a telephone survey of 1113 retired workers from whom a detailed work history and complete telephone versions of the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) and the Sleep Timing Questionnaire (STQ) (Monk et al., 2003) were available. Also available was a measure of morningness from the Composite Scale of Morningness (CSM; Smith et al., 1989) and a simple question regarding self-rated health (see below). A preliminary analysis of some of these data (n=654) has been published previously on a topic unrelated to shiftwork (Monk et al., 2011). In that analysis we showed that a morning-type orientation and regularity in bed timings were both conducive to better sleep in retirement.
The primary hypotheses to be tested by the present study were: [hypothesis 1 (H1)] that exposure to shiftwork in retirees will lead to poorer self-rated sleep when compared to retired day workers; and (H2) that retired shiftworkers will have abnormal and/or a wider spread of bedtimes and rise-times between individuals when compared to retired day workers. Secondary hypotheses were that poorer sleep in retired shiftworkers may be mediated by (H3) poorer health; or (H4) a reduced tendency for them to be morning types, as evening types might be more comfortable with night work. These hypotheses were based on the findings that healthy seniors sleep better than unhealthy ones (Ohayon et al., 2004), and that morning-type seniors sleep better than evening or intermediate-type ones (Monk et al., 2011).
METHOD
Telephone survey methodology
The telephone survey lasted approximately 20–30 min and comprised telephone-modified versions of well-validated self-report questionnaires and study-specific interview questions. It was conducted by the Survey Research Program of the University Center for Social and Urban Research (UCSUR). Commercially available lists of telephone numbers which had a high likelihood of having older people in the household were purchased. Postal codes in the Greater Pittsburgh area that were more likely to have retired shiftworkers were oversampled to increase efficiency. In the initial design of the study, five shiftwork exposure bins were considered: 0, 1–7, 8–14, 15–20 and >20 years. Occasionally, as the study progressed, various shiftwork exposures (including zero) were favored and/or excluded in order to try to maintain a balance between different levels of shiftwork exposure. The survey was thus not a true random sample of older people, but nor was it a self-selected or convenience sample. We eventually divided the shiftwork exposure bins into tertiles to increase power.
The survey instrument was programmed into a Computer-Assisted Telephone Interviewing (CATI) system. The CATI system allowed the interviews to be conducted by a cadre of trained interviewers using personal computers that displayed the questions in proper order and automatically controlled question skips and flow. The CATI system additionally had built-in sample management and call scheduling routines to maximize the probability of contacting households. This technology eliminated the need for paper call records and manual data entry. In order to maximize response rates, at least eight calls were made on varying days of the week at different times to maximize the probability of contacting respondents, and attempts were made to convert initial refusals into completed interviews.
The first section of the interview screened the household for retired residents aged 65 years or older, asking if they would come to the telephone. Then, following permission being granted to continue, questions regarding former shiftwork, including length of exposure, were asked. This involved the taking of a detailed work history, progressing from position to position back through the subject’s entire working life. Questions were asked as to what the work schedule for that job was (e.g. permanent, weekly rotating, etc.), roughly what the work involved, as well as starting and ending dates (at least to the nearest year). The interviewers were skilled at helping subjects give this information by suggesting time anchors such as the birth of a child to help them remember. In order to lessen subject burden, questions were not asked about workload, chemical exposure, salary or specific job title or grade. Most subjects reported that periods of time (years) with a shiftwork routine were often interspersed with those involving a day-working routine.
The sleep and circadian questionnaires then followed. We developed a telephone version of the PSQI (Buysse et al., 1989) and the STQ (Monk et al., 2003). Because all subjects were retired, no distinction was made between workdays and weekends in the STQ. PSQI questions concerning snoring as reported by a bed-partner (which do not contribute to the overall PSQI score) were not included in the telephone interview. Also included were questions to glean information regarding morningness, physical health, depressive symptoms and demographics. The interview was anonymous, and had been ruled as exempt (i.e. not requiring signed informed consent) by the University of Pittsburgh Institutional Review Board.
Subjects
All subjects were required to be aged 65 years or older, to have not conducted any shiftwork during the past 12 months and to be now retired (i.e. not working for pay for more than 10 hours per week outside the home). Both men and women were eligible, and race was not a factor in subject recruitment. All subjects were required to speak and understand English and to be cognitively able to understand and answer the questions asked of them.
We contacted 3545 eligible possible interviewees. Of these, 1207 eligible respondents refused to participate, 292 could not be recontacted to complete the interview and 315 eligible respondents were unable to participate due to health, physical or cognitive problems. A total of 1731 interviews were started, but 565 of these represented individuals whose work history seemed dubious and/or confused. Forty-five subjects with incomplete data from the PSQI and/or STQ were also excluded, as well as eight interviews whose STQ data indicated an apparent habitual sleep time of <3 or >12 hours. This left a total of 1113 subjects who were included in the present analysis (634 men, 479 women); ages ranged from 65 to 94 years [mean: 74.7 years, standard deviation (SD): 6.3 years]. The three shiftwork exposure groups were within 1.5 years of each other in mean age. Five subjects asserted that they were >65 years but declined to give their exact age. Subject demographics are given in Table 1. Subjects were not paid for their participation.
Table 1.
Sample demographics (n=1113)
| Exposure group | n | Mean (SD) age* | % Male | % Managerial (n) |
|---|---|---|---|---|
| 0y | 387 | 75.5 (6.1y) | 48.3 | 49.1 |
| 1 year=15 years | 371 | 74.1 (6.5y) | 52.0 | 38.5 |
| >15 years | 355 | 74.6 (6.4y) | 71.6 | 29.3 |
| Whole sample | 1113 | 74.7 (6.3) | 57.0 | 39.3 |
Sample size reduced by 5 (see text).
SD: standard deviation.
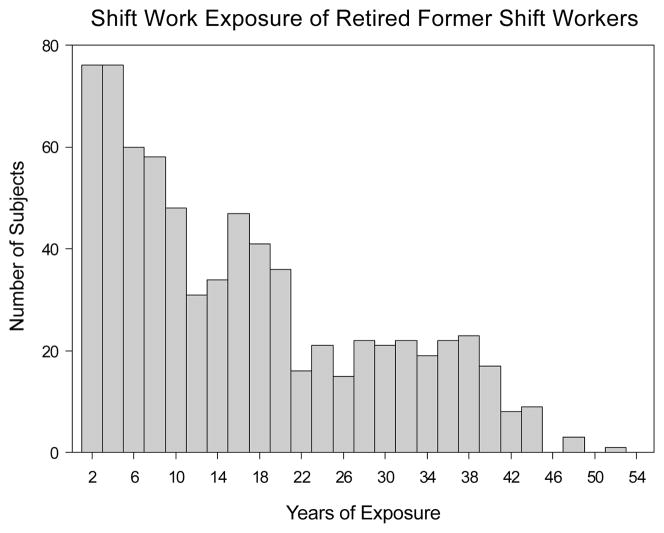
Definitions
Shiftwork and day work were both defined very specifically with regard to working times and hours worked per month. Only jobs requiring at least 35 hours per week of work outside the home were included in the definitions of shiftwork and day work. Military service was not included in the present analysis. Shiftwork was defined as non-overtime scheduled work outside the home overlapping the midnight to 06:00 hours window (i.e. night work) on either a fixed or rotating basis (details of which were taken). The present analysis was restricted to interviews in which a full work-history was given. The work-history details were then used to calculate a ‘years of shiftwork exposure’ value for each interview, counting the years (and part-years) spent in work positions that included shiftwork as defined above. In order to be included in the 0 years exposure group, the subject was required to answer ‘no’ to the question: ‘Have you ever worked a job that required regular (non-overtime) work after 9 p.m.?’. In order to constitute shiftwork exposure groups of approximately equal size, while still accounting for possible shiftwork ‘survivor effects’ (see above), tertiles were examined post hoc and subjects then cast into three bins [0 (n=387), 1–15 (n=371) and >15 years (n=355)] for the present analysis. The frequency distribution of shiftwork exposures is shown in Fig. 1. The 387 0 years exposure subjects were not included, so that the y-axis was scaled appropriately.
Figure 1.
Frequency distribution of shiftwork exposures as calculated from job history of the 726 subjects who were not in the 0 years exposure group.
Also assigned was a general measure of former employment, cast into various categories (professional, manager/supervisor, public service, technical, sales/clerical, manual). This was an inexact measure counting the majority category for a given subject. In order to simplify the analysis, for the present purposes it was collapsed into two categories: managerial (professional or manager/supervisor) (n=437) and other (n=676).
Primary variables
The main independent measure was shiftwork exposure with three levels (0, 1–15 and >15 years). The prime dependent measure was the PSQI total score—a whole number between 0 and 21, with higher numbers indicating poorer sleep and a value above 5 considered as indicating possible sleep problems (Buysse et al., 1989). Also analyzed was habitual bedtime and habitual rise-time as reported in the STQ (Monk et al., 2003). Gender and former employment were extracted as factors in the analyses. Statistical analysis was by three-way analysis of variance (ANOVA) (factors: shiftwork exposure, gender, former employment) and models included main effects as well as interactions taking a P-value of <0.05 as indicating a significant effect. Post-hoc comparisons used the Tukey–Kramer method to examine all pairwise differences between the three shiftwork exposure levels.
Secondary variables
In the telephone interview, a number of simple health-related questions were also asked. One question asked: ‘In general would you say your health is excellent, very good, good, fair, or poor?’. Subjects were dichotomized into those reporting less than good (i.e. fair or poor) health (n=265), and those reporting good, very good or excellent health (n=848). Also given in the interview was a telephone version of the CSM (Smith et al., 1989). Not all subjects gave complete answers to this instrument, and a morningness score could be calculated for only 951 subjects. Following procedures we used in an early study on a subset of these data (Monk et al., 2011), a cut-off CSM score of 44 was used to dichotomize subjects into morning-type (M-type) and other-type (O-type) groups of approximately equal size (n=479, 472).
RESULTS
Main effects of shiftwork exposure on PSQI (H1)
Results are given in Tables 2 and 3. Compared to the retired day worker (0 years) group, the 1–15 years exposure group reported worse sleep by 0.94 PSQI units (main effect P=0.005, post-hoc Tukey–Kramer adjusted P<0.004). This was comparable to the gender difference which was 1.02 PSQI units. The 0.61 difference between 0 years and >14 years groups did not achieve significance by post-hoc test. In addition to a main effect of shiftwork exposure, there were also main effects of gender (P<0.001) and past employment (P=0.03), with male and professional/managerial subjects reporting better sleep. However, neither of these variables interacted significantly with shiftwork exposure. Frequency distributions of PSQI scores for retired shiftworkers and retired day workers are given in Fig. 2.
Table 2.
Descriptive statistics for (for some variables, missing responses led to a reduced n). Given is mean and standard deviation (SD). Significant main effects are shown in bold type
| Dependent variable | Whole group n=1113 |
Exposure | Gender | Employment | ||||
|---|---|---|---|---|---|---|---|---|
| 0 years n=387 |
1–15 years n=371 |
>15 years n=355 |
Male n=634 |
Female n=479 |
Managerial n=437 |
Other n=676 |
||
| PSQI | 5.6 (3.6) | 5.1 (3.3) | 6.1 (3.8) | 5.7 (3.8) | 5.2 (3.4) | 6.2 (3.8) | 5.3 (3.6) | 5.8 (3.6) |
| Rise-time | 07:32 (84.2) | 07:29 (82.8) | 07:38 (85.6) | 07:29 (83.9) | 07:27 (80.6) | 07:39 (88.2) | 07:28 (86.4) | 07:34 (82.6) |
| Bedtime | 23:15 (73.8) | 23:08 (69.2) | 23:21 (78.9) | 23:15 (72.8) | 23:12 (69.7) | 23:19 (78.8) | 23:14 (74.3) | 23:15 (73.5) |
PSQI: Pittsburgh Sleep Quality Index.
Table 3.
Results of analysis of variance (ANOVA) statistical tests (for some variables, missing responses led to a reduced n); significant effects are shown in bold type
| Dependent variable | Exposure | Gender | Employment | Exposure × gender | Gender × employment | Exposure × employment | Exposure × gender × employment | Post hoc |
|---|---|---|---|---|---|---|---|---|
| PSQI | F(2,1038)=5.27, P=0.005 | F(1,1038)=24.5, P=<0.001 | F(1,1038)=4.64, P=0.031 | F(2,1038)=0.35, P=0.703 | F(1,1038)=0.00, P=0.996 | F(2,1038)=1.27, P=0.281 | F(2,1038)=0.01, P=0.985 |
0 < 1–15 years Male < female Managerial < other |
| Rise-time | F(2,1101)=2.31, P=0.099 | F(1,1101)=4.97, P=0.026 | F(1,1101)=0.67, P=0.414 | F(2,1101)=0.24, P=0.786 | F(1,1101)=0.10, P=0.756 | F(2,1101)=0.25, P=0.778 | F(2,1101)=2.07, P=0.127 | Male < female |
| Bedtime | F(2,1101)=3.46, P=0.032 | F(1,1101)=3.48, P=0.063 | F(1,1101)=0.01, P=0.931 | F(2,1101)=0.04, P=0.961 | F(1,1101)=0.04, P=0.839 | F(2,1101)=1.50, P=0.223 | F(2,1101)=1.59, P=0.204 | 0 < 1–15 years |
PSQI: Pittsburgh Sleep Quality Index.
Figure 2.
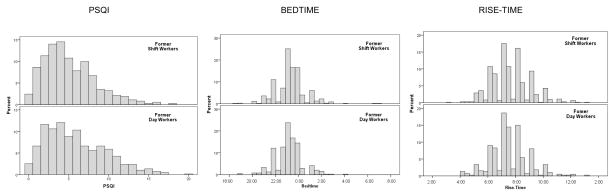
Frequency distribution of Pittsburgh Sleep Quality Index (PSQI) scores, bedtimes and rise-times for former shiftworkers (FSW) (combining 1–15 years and >15 years groups) and former day workers (FDW) (0 years group). Sample sizes were 726 (FSW) and 387 (FDW) with missing data lowering that figure for some measures.
Habitual bedtime and rise-time (H2)
Results for current (i.e. during retirement) habitual bedtimes and rise-times from the STQ are given in Tables 2 and 3. On average, subjects habitually reported a bedtime of about 23:15 hours and a rise-time of about 07:30 hours. Mean habitual rise-times were within 9 min of each other for the three shiftwork exposure groups and standard deviations were within 3 min. There was a significant gender difference in rise-times, with males rising an average of 12 min earlier than females. There were no significant effects or interactions with shiftwork exposure. Mean habitual bedtimes were within 13 min of each other for the three shiftwork exposure groups and standard deviations were within 10 min. The ANOVA indicated a significant effect of shiftwork exposure, with the 1–15 years group having a 13 min later mean habitual bedtime than the 0 years group. There were no significant main effects or interactions with gender or former occupation. Frequency distributions of habitual bedtimes and rise-times for retired shiftworkers and retired day workers are given in Fig. 2.
Health (H3)
In the literature (Costa, 2003), shiftwork has often been reported to be associated with disease, and it was thus possible that the present shiftwork exposure effect in the PSQI may have been mediated by the subject’s health in retirement. In response to our very simple health question, we did indeed find that the percentage of subjects responding that their health was less than good (i.e. fair or poor) rose significantly with shiftwork exposure [17.1, 25.6 and 29.3% for the 0 years, 1–15 and >15 years groups (χ2(2)=16.29, P<0.001)]. We thus repeated the analysis after deleting all subjects reporting less than good health. A significant effect of shiftwork exposure on PSQI still emerged in the remaining subjects (F(2,789)=3.41, P=0.034) where the 0 years group had lower PSQI scores than the 1–15 years group.
Morningness (H4)
When a count was made, M-types represented 50.0, 49.4 and 49.5% of the 0, 1–15 and >15 years shiftwork exposure groups, respectively, indicating an approximately even spread of M-types across the three shiftwork exposure groups [χ2(2)<1, not significant (NS)]. An ANOVA with morningness as an additional factor confirmed the earlier finding on a subset of these data, with a significant main effect of morningness on PSQI (M-type 4.79, O-type 6.39; F(1,892)=49.07, P=<0.001). However, there was no significant interaction between morningness and shiftwork exposure (F(2,892)=1.98, P=0.14).
DISCUSSION
The present results showed that retired shiftworkers do indeed report poorer sleep than retired day workers, thus confirming H1. Importantly, although there were also significant main effects of both gender and former employment, neither factor showed a significant interaction with shiftwork exposure, suggesting a fairly general exposure effect. Moreover, it is noteworthy, given the power of the study emanating from a sample size of more than 1000, that the magnitude of the shiftwork exposure effect was roughly equivalent to that of gender [at 1.0 PSQI units in the present study and 0.7 PSQI units in the original PSQI study of seniors (Buysse et al., 1991)]. Because gender differences in perceived sleep quality are well known and widely accepted by clinicians (Ancoli-Israel, 2005; Bliwise, 2005), one can advance the case that the present shiftwork exposure effects should be considered to be at least as important. The fairly modest effect size of about 0.27 we found in both gender and shiftwork exposure, however, suggests that the present results should not be overstated.
With regard to H2, the analysis of habitual bedtimes and rise-times confirmed that, in this sample, the shiftwork exposure effect could not be explained simply by either different timing or different between-subjects variability in timing between the three shiftwork exposure groups. Thus, those with a history of shiftwork do not appear to be more casual in their approach to bed-timing than their retired day worker counterparts. Instead, it would appear that the natural tendency of H. sapiens to sleep at night, and/or the social pressures from day-oriented family members and the surrounding community, predominated, leading to fairly normal bedtimes of about 23:15 hours and rise-times of about 07:30 hours.
Questions regarding the mechanism by which shiftwork exposure effects on PSQI might arise were addressed by H3 (health) and H4 (morningness). Because of the well-established finding in the literature that ill-health can be associated with shiftwork in existing shiftworkers (Costa, 2003), and that poorer health in seniors is associated with worse sleep (Ohayon et al., 2004), we hypothesized in H3 that those with shiftwork exposure showed poorer health than those without, and that it was this poorer health that led to poorer sleep. An effect of shiftwork exposure on self-reported health has also been found in retired shiftworkers in a monozygotic twins study (Ingre and Akerstedt, 2004). In our study, perceived health appeared to worsen with shiftwork exposure, with the percentage reporting their health as not good (i.e. fair or poor) rising from about 17% to about 29% over the three shiftwork exposure groups. However, H3 was not supported by the secondary analyses. When we controlled for health and repeated the ANOVA, a significant main effect of shiftwork exposure (in a very similar pattern) still emerged in the remaining subjects.
H4 posited that individuals falling into the M-type chronotype category would probably be under-represented in the higher levels of shiftwork exposure, and that shiftwork exposure effects in PSQI were mediated by this relative absence of M-types in those groups. In an earlier paper (Monk et al., 2011), using a subset of the present study data, we have shown a morning-type orientation to be generally associated with a better (i.e. lower) PSQI score in seniors. Thus, if (as seems reasonable) a smaller proportion of the retired shiftworkers happened to be morning types (M-types), then the present shiftwork exposure effect may be explained by that mechanism. However, the hypothesis was not supported by secondary analyses. When a count was made, there was an even spread of M-types across the three shiftwork exposure groups. Thus, although M-types did indeed report better sleep, there was no paucity of them in the retired shiftworker groups. H4 was thus not supported.
The finding of a slightly smaller shiftwork exposure effect in the >15 years group suggests that in the present study, as in others (Dumont et al. 1997; Knutsson, 2003; Scott et al., 1997), there was a small ‘survivor effect’ appearing in those with long shiftwork exposures. Those with the constitution and/or domestic circumstances to survive for >15 years without switching to day work may comprise a special set of people who thus show fewer adverse effects on their sleep in retirement and thus have slightly lower PSQI scores.
In addition to a monozygotic twins study (Ingre and Akerstedt, 2004) showing shiftwork exposure effects on sleep in retired shiftworkers, there are two studies of young and middle-aged adults which pertain directly to the present results, in that they present data from workers not currently undertaking shiftwork. In 1997, Brugere et al. (1997) reported data from a large-scale French epidemiological study with 21 378 subjects, 9584 of whom were shiftworkers. Sleep symptoms were extracted from a self-report questionnaire of health symptoms. Subjects were separated into those currently working shifts (‘present’), those who previously worked shifts but were not current shiftworkers (‘past’) and those who had never been shiftworkers (‘never’), plotting the number of subjects with insomnia symptoms by different age groups. The observed frequency in sleep disorders revealed the expected worsening with age. Interestingly, however, the ‘past’ line was intermediate between ‘never’ and ‘present’ lines approaching the ‘present’ line at the highest age group (52 years). Thus, former shiftworkers in their 50s reported almost as much sleep disruption as current shiftworkers in that age group, and substantially more than those who had never worked shifts. There is also the work by Dumont et al., 1997, who studied insomnia symptoms in currently day-working nurses who had previously experienced shiftwork for several years. The greatest effect of shiftwork exposure on sleep was observed in the 57 nurses who had between 4 and 10 years of exposure. For these nurses there was more evidence of insomnia than in the low (<4 years) exposure group. For nurses with more than 10 years of exposure there appeared to be a ‘survivor effect’ lessening the risk (see above). Thus, it would appear that the present results are in agreement with conclusions made by earlier authors.
The failure of H3 and H4 to explain the present findings means there is still a void to fill in terms of the explanation of why sleep quality should be lower in retired shiftworkers compared to retired day workers. In a recent review paper (Buysse et al., 2011) we have discussed some of the possible neurobiological mechanisms for late-life insomnia in general. These mechanisms involve processes related to circadian rhythms, stress reactivity, genetics and sleep homeostasis. This approach may provide one possible roadmap for future research concerned with the processes underlying the insomnia experienced by many retired shiftworkers.
CONCLUSION
Shiftwork exposure is associated with poorer reported sleep in retired seniors (65 years+) compared to retired day workers. The effect appears to be equivalent to that seen in gender. There appears to be no interaction of the effect with gender or with type of occupation prior to retirement. The effect appears not to be mediated simply by health or chronotype. Habitual bedtimes and rise-times (and their variability) in retirement appear not to be affected by shiftwork exposure.
Acknowledgments
Special thanks are owed to Jean Miewald for help with data analysis, to Melissa Clark for pilot work, to the UCSUR team of interviewers for their hard work and to our subjects for their time. Support for this work was provided by National Institute on Aging Grants AG-13396 and AG-20677, and by RR-024153. Neither the University of Pittsburgh nor the funding agencies necessarily agree with the statements made in this paper.
Footnotes
DISCLOSURE STATEMENT
None of the authors has any conflict of interest with respect to this paper.
References
- Akerstedt T. Shift work and sleep disorders. Sleep. 2005;28:9–11. [PubMed] [Google Scholar]
- Akerstedt T, Ingre M, Broman JE, Kecklund G. Disturbed sleep in shift workers, day workers, and insomniacs. Chronobiol Int. 2008;25:333–348. doi: 10.1080/07420520802113922. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S. Sleep and aging: prevalence of disturbed sleep and treatment considerations in older adults. J Clin Psychiatry. 2005;66 (Suppl 9):24–30. [PubMed] [Google Scholar]
- Bliwise DL. Normal aging. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. Elsevier Saunders; Philadelphia, PA: 2005. pp. 24–38. [Google Scholar]
- Brugere D, Barrit J, Butat C, Cosset M, Volkoff S. Shiftwork, age, and health: an epidemiologic investigation. Int J Occup Environ Health. 1997;3:S15–S19. [PubMed] [Google Scholar]
- Buysse DJ, Germain A, Hall M, Monk TH, Nofzinger EA. A neurobiological model of insomnia. Drug Discov Today Dis Mod. 2011;8:129–137. doi: 10.1016/j.ddmod.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14:331–338. [PubMed] [Google Scholar]
- Costa G. Shift work and occupational medicine: an overview. Occup Med (Lond) 2003;53:83–88. doi: 10.1093/occmed/kqg045. [DOI] [PubMed] [Google Scholar]
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- Dumont M, Montplaisir J, Infant-Rivard C. Sleep quality of former night-shift workers. Int J Occup Environ Health. 1997;3:S10–S14. [PubMed] [Google Scholar]
- Folkard S, Monk TH, Lobban MC. Towards a predictive test of adjustment to shiftwork. Ergonomics. 1979;22:79–91. doi: 10.1080/00140137908924591. [DOI] [PubMed] [Google Scholar]
- Ingre M, Akerstedt T. Effect of accumulated night work during the working lifetime, on subjective health and sleep in monozygotic twins. J Sleep Res. 2004;13:45–48. doi: 10.1111/j.1365-2869.2004.00390.x. [DOI] [PubMed] [Google Scholar]
- Knauth P, Hornberger S. Preventive and compensatory measures for shift workers. Occup Med (Lond) 2003;53:109–116. doi: 10.1093/occmed/kqg049. [DOI] [PubMed] [Google Scholar]
- Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53:103–108. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- Monk TH. What can the chronobiologist do to help the shift worker? J Biol Rhythms. 2000;15:86–94. doi: 10.1177/074873040001500202. [DOI] [PubMed] [Google Scholar]
- Monk TH, Buysse DJ, Billy BD, et al. Circadian type and bed-timing regularity in 654 retired seniors: correlations with subjective sleep measures. Sleep. 2011;34:235–239. doi: 10.1093/sleep/34.2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TH, Buysse DJ, Kennedy KS, Potts JM, DeGrazia JM, Miewald JM. Measuring sleep habits without using a diary: the sleep timing questionnaire (STQ) Sleep. 2003;26:208–212. doi: 10.1093/sleep/26.2.208. [DOI] [PubMed] [Google Scholar]
- Moore RY. Circadian rhythms: basic neurobiology and clinical applications. Annu Rev Med. 1997;48:253–266. doi: 10.1146/annurev.med.48.1.253. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- Scott AJ, Monk TH, Brink L. Shiftwork as a risk factor for depression: a pilot study. Int J Occup Environ Health. 1997;3:S2–S9. [PubMed] [Google Scholar]
- Smith CS, Reilly C, Midkiff K. Evaluations of three circadian rhythm questionnaires with suggestions for an improved measure of morningess. J Appl Psychol. 1989;74:728–738. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- Vahtera J, Westerlund H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep. 2009;32:1459–1466. doi: 10.1093/sleep/32.11.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]