Abstract
Background/Aims
During endoscopic retrograde cholangiopancreatography (ERCP), all efforts should be made to be aware of radiation hazards and to reduce radiation exposure. The aim of this study was to investigate the status of radiation protective equipment and the awareness of radiation exposure in health care providers performing ERCP in Korean hospitals.
Methods
A survey with a total of 42 questions was sent to each respondent via mail or e-mail between October 2010 and March 2011. The survey targeted nurses and radiation technicians who participated in ERCP in secondary or tertiary referral centers.
Results
A total of 78 providers from 38 hospitals responded to the surveys (response rate, 52%). The preparation and actual utilization rates of protective equipment were 55.3% and 61.9% for lead shields, 100% and 98.7% for lead aprons, 47.4% and 37.8% for lead glasses, 97.4% and 94.7% for thyroid shields, and 57.7% and 68.9% for radiation dosimeters, respectively. The common reason for not wearing protective equipment was that the equipment was bothersome, according to 45.7% of the respondents.
Conclusions
More protective equipment, such as lead shields and lead glasses, should be provided to health care providers involved in ERCP. In particular, the actual utilization rate for lead glasses was very low.
Keywords: Endoscopic retrograde cholangiopancreatography, Radiation exposure, Protective equipment
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) has been used to diagnose and treat pancreatobiliary diseases for over 40 years. Recently, magnetic resonance cholangiopancreatography and endoscopic ultrasonography have been used more frequently to diagnose pancreatic and biliary diseases, but there are no alternatives that can replace ERCP in respect to therapeutic procedures.
However, ERCP is associated with radiation exposure, due to the concomitant use of fluoroscopy. Radiation exposure poses hazards for health care providers, as well as patients, and may have somatic and genetic effects.1,2 Therefore, several studies have been conducted in response to growing interest in radiation exposure during ERCP, but these studies have produced contradictory results. Cohen et al.3 argued for the need for extensive care and protection against very high doses of radiation arising from ERCP procedures. On the other hand, Wagner et al.4 countered that a health care provider is exposed to much lower doses of radiation than the patient on whom the procedure is performed, and other studies also reported the safety of the procedure regarding radiation exposure, if protective equipment such as a lead apron is worn.5 Levels of radiation exposure may vary considerably depending on the voltage of the radiation source, exposure time, whether protective equipment is worn, and the distance of the patient and the operator from the source.
Although previous studies may have produced different results and opinions with regard to radiation exposure and the hazards arising from ERCP, there is a general consensus that efforts should be made to reduce radiation exposure affecting health care providers. Therefore, health care providers participating in ERCP procedures should be aware of the radiation hazards, and protective equipment such as lead aprons, thyroid shields, lead glasses, lead shields, and radiation dosimeters. In light of this, in 2009, the Korean Pancreatobiliary Association (KPBA) announced recommendations for ERCP-related radiation damage prevention. However, many health care providers are not aware of these recommendations and may be rather negligent about using complete personal protective equipment.
Our study was planned to investigate the current status of Korean health care providers' radiation protective equipment, their actual usage of the equipment, and their awareness of radiation exposure during ERCP by survey. Based on current status, we wanted to enhance improvement of the ERCP curriculum and awareness of radiation protective systems.
MATERIALS AND METHODS
Survey responses were collected anonymously via mail or e-mail between October 2010 and March 2011. The questionnaire consisted of 42 questions in total: those about respondent information, ERCP circumstance, the current status and awareness of radiation protective equipment, those about awareness and attitude changes after the recommendations for ERCP-related radiation damage prevention in 2009, and detailed questions. The survey targeted nurses and radiation technicians participating in ERCP procedures at secondary general hospitals (n=58) and tertiary referral centers (n=35) in Korea.
RESULTS
1. Respondent information
A total of 78 providers from 38 hospitals answered the questions (response rate, 52%). All 78 respondents were women, and mean age (SD) was 34.6 (5.97). The respondents' positions were as follows: 62 (79.5%) registered nurses, 13 (16.7%) charge nurses, two (2.6%) radiation technicians, and one (1.3%) head nurse. Tertiary referral centers and secondary general hospitals were 55.3% (21/38) and 44.7% (17/38), respectively (Table 1).
Table 1.
Baseline Characteristics of the Respondents
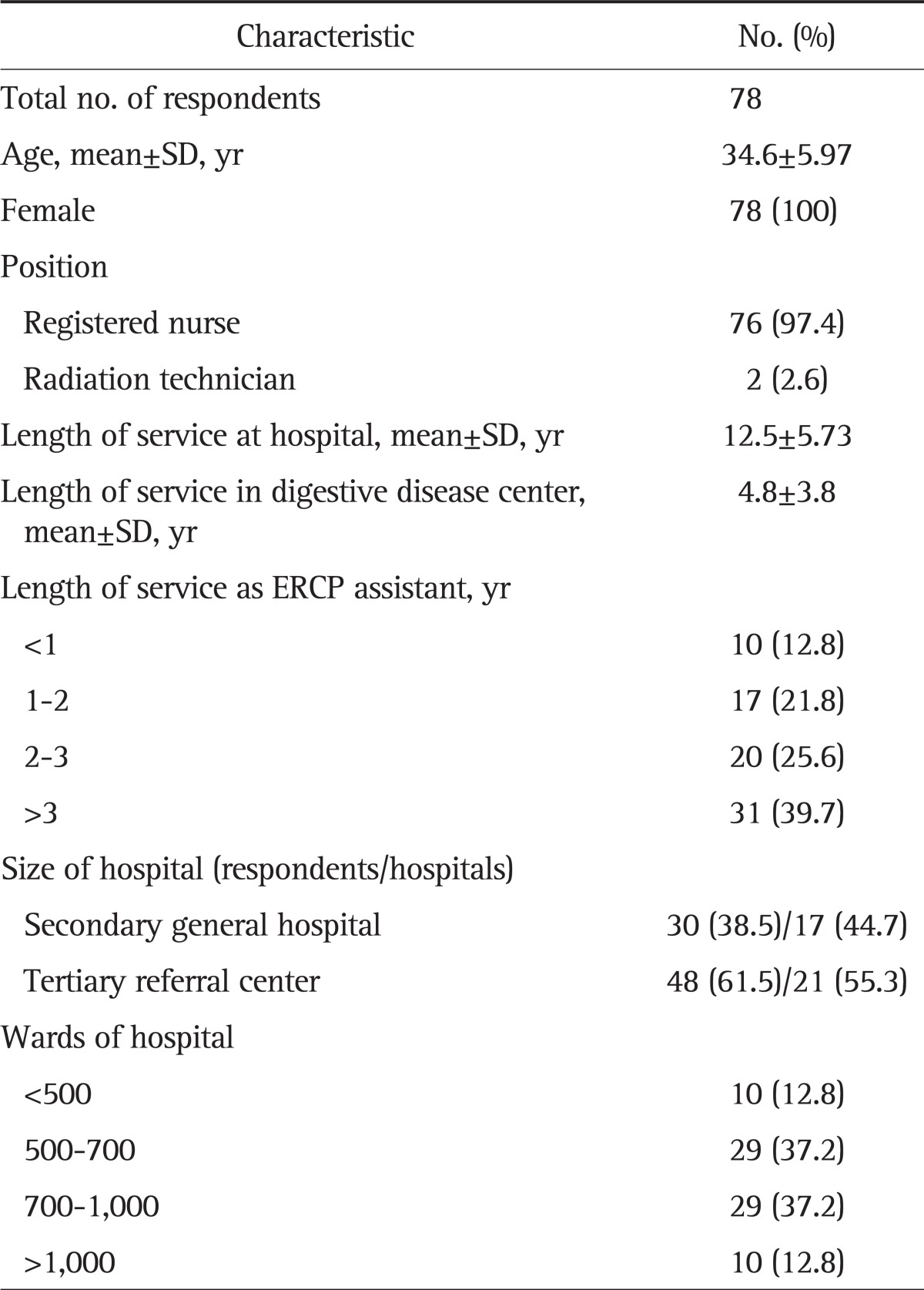
ERCP, endoscopic retrograde cholangiopancreatography.
2. Current status of ERCP
Of the 38 hospitals, seven hospitals (18.4%) had independent ERCP rooms in their digestive disease centers, whereas the other hospitals did not have independent ERCP rooms. Mean number of ERCP procedures was 39.3 (range, 8 to 100) per month in each hospital. Mean procedure time was between 30 minutes and 1 hour. Mean radiation exposure time per procedure was between 5 and 10 minutes. Mean number of pictures per procedure was 5 to 10 pictures.
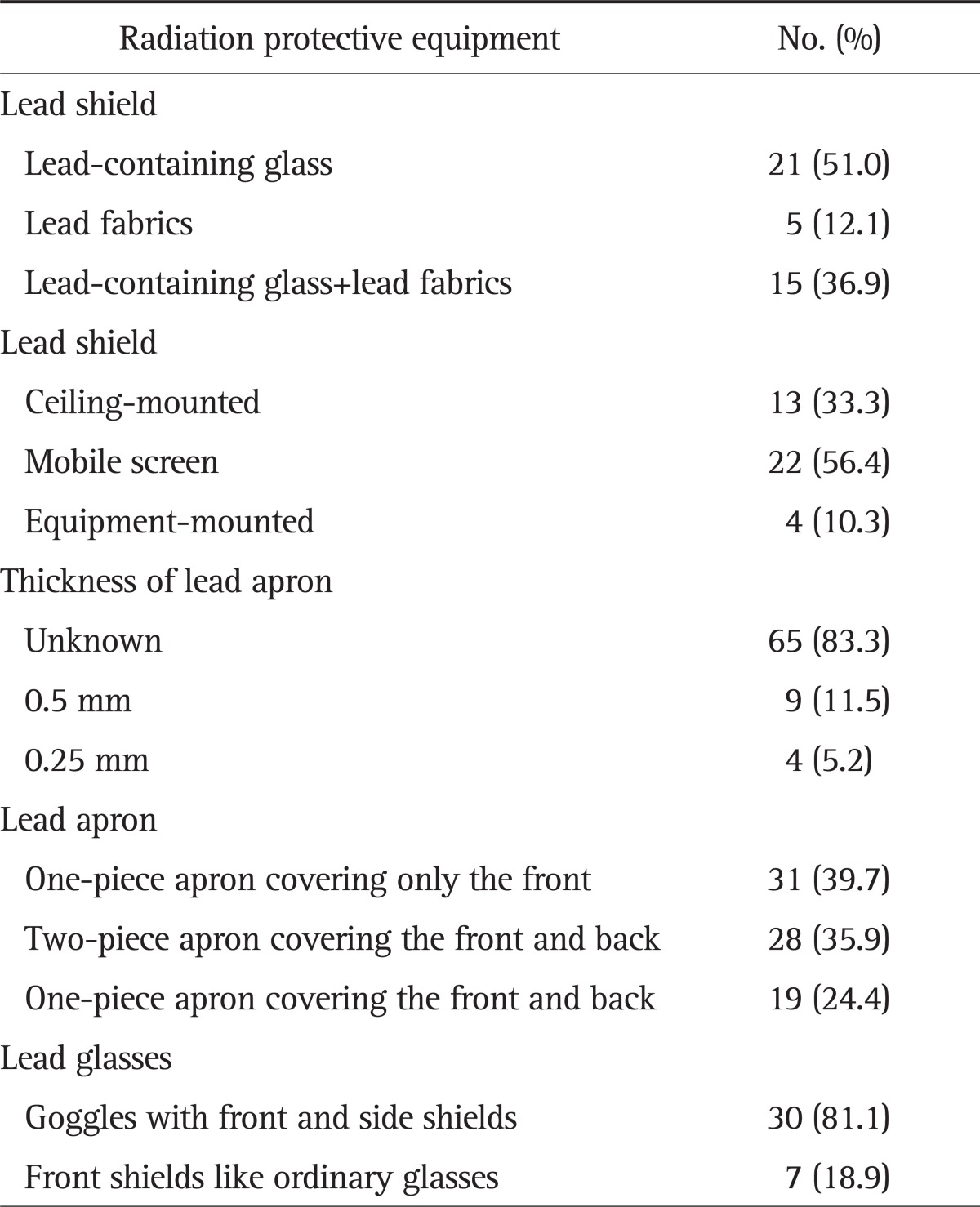
3. Radiation protective equipment
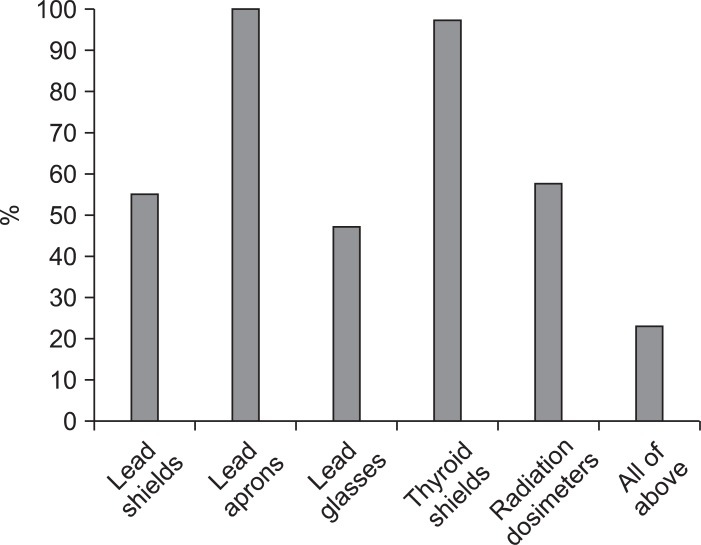
Among lead shield, lead apron, lead glasses, thyroid shield, and radiation dosimeter, 61 respondents (78.2%) considered lead aprons as the most important protective equipment, followed by thyroid shields (n=9, 11.5%). The preparation rates were 55.3% (21/38 hospitals) in lead shields, 100% (78/78) in lead aprons, 47.4% (37/78) in lead glasses, 97.4% (76/78) in thyroid shields, 57.7% (45/78) in radiation dosimeters, and 23.1% (18/78) in all of the above (Fig. 1). The most common type and form of lead shields were lead-containing glass and mobile screens, 51% (21/41) and 56.4% (22/39), respectively. The most common form of lead apron was a full-length (one-piece) apron covering only the front of the body in 39.7% (31/78). The most common type of lead glasses was goggles with front and side shields in 81.1% (30/37) (Table 2). The locations of radiation dosimeters were as follows: 73.3% (33/45) chest or waist inside lead apron, and 26.7% (12/45) outside lead apron. Respondents stated that they checked dosimeters every 3 or 6 months, 72.2% (26/36) and 22.2% (8/36), respectively.
Fig. 1.
The preparation rate of protective equipment.
Table 2.
Type of Radiation Protective Equipment
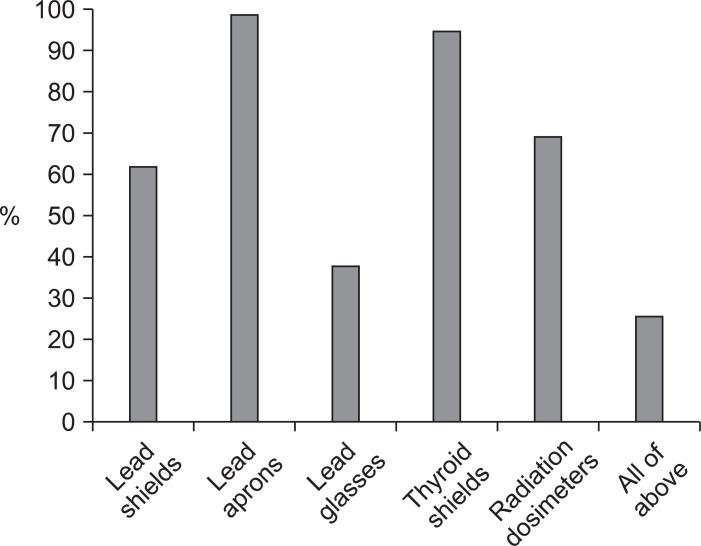
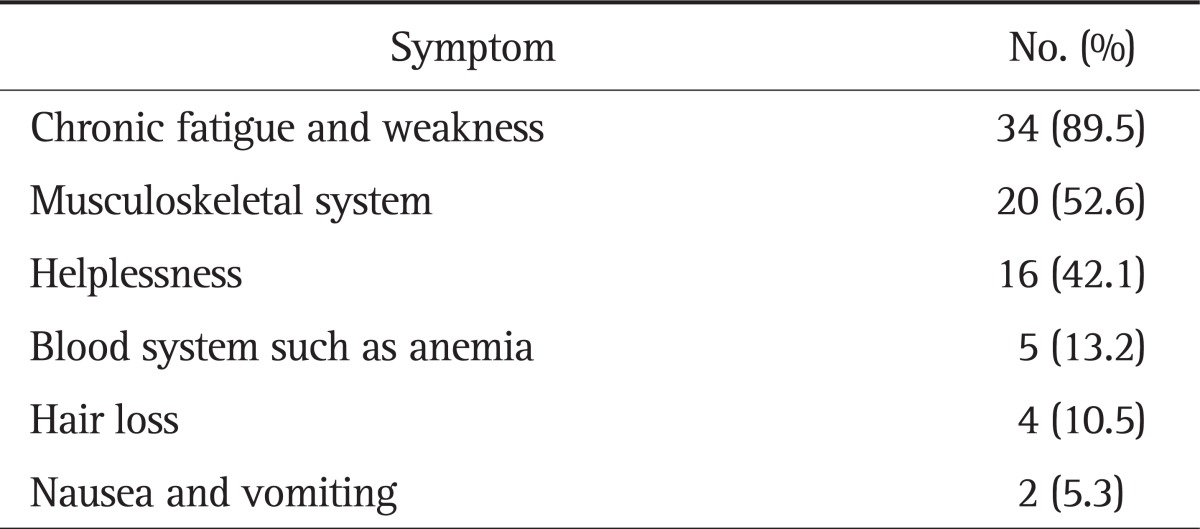
The respondents used lead aprons and thyroid shields, 98.7% and 94.7%, respectively; however, actual utilization rate of lead glasses was very low (37.8%) (Fig. 2). The most common reason for not using protective equipment was that it was bothersome in 45.7% (21/46), followed by frequently forgetful in 26.1% (12/46) (Table 3). Thirty-eight respondents (50%) reported having experienced physical abnormalities resulting from ERCP procedures (Table 4). When not wearing protective equipment during ERCP, the body parts most worried about were as follows: thyroid in 30 (38.5%), reproductive system in 21 (27%), eyes in 16 (20.5%), head in five (6.3%), whole body in four (5.1%), limbs in one (1.3%), and skin in one (1.3%).
Fig. 2.
The actual utilization rate of protective equipment. The actual utilization rate is defined as the rate of actual usage of prepared equipment.
Table 3.
Reason for Not Wearing Protective Equipment
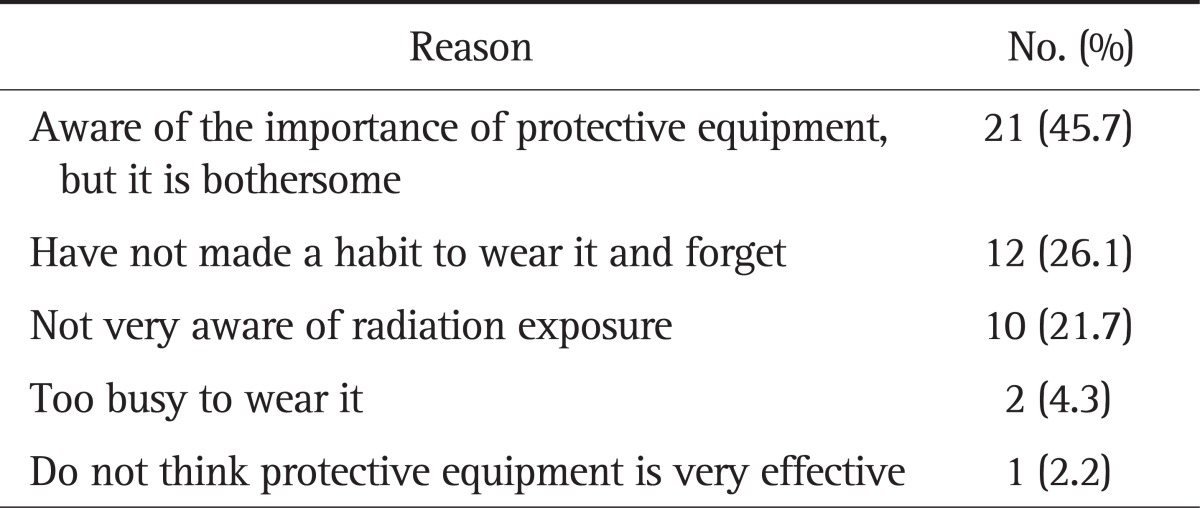
Table 4.
Subjective Symptoms after Radiation Exposure
4. Changes in awareness and attitude after announcement of recommendations for ERCP-related radiation damage prevention
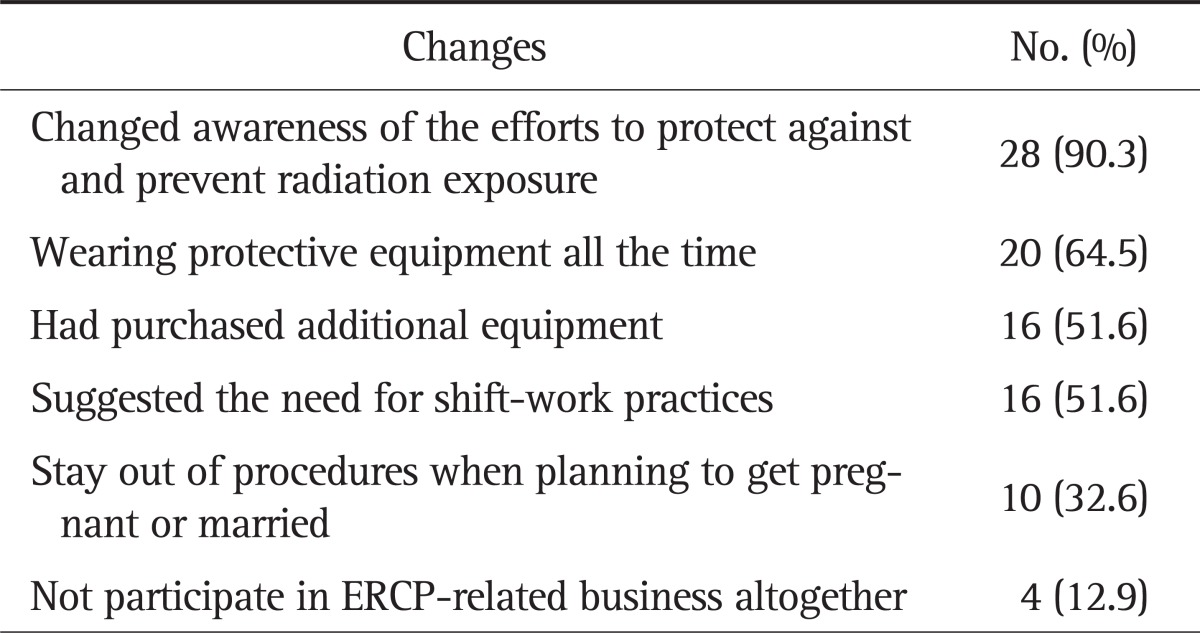
With regard to the 2009 ERCP-related radiation damage prevention recommendations of the KPBA (Appendix), only 31 of the respondents (39.7%) have attended lectures or read documents on the subject. After reading the recommendations, what they considered most important was as follows: lead aprons in 64.5% (20/31), lead shields in 19.4% (6/31), lead glasses in 9.7% (3/31), radiation dosimeters in 6.4% (2/31), and thyroid shields in 0%. Twenty-eight (90.3%) reported a changed awareness of the efforts to protect against and prevent radiation exposure; 16 (51.6%) were aware of the importance of protective equipment and had purchased additional equipment; 20 (64.5%) wore protective equipment all the time; and 16 (51.6%) suggested the need for shift-work practices; 10 (32.6%) were willing to stay out of procedures when planning to get pregnant or married, and four (12.9%) were willing to not participate in ERCP-related business altogether (Table 5). After the recommendations, additional equipment was bought in 48.1% of hospitals (13/27); lead glasses in 69.2% (9/13); and lead shields in 53.8% (7/13).
Table 5.
Changes after Reading the Recommendations for ERCP-Related Radiation Damage Prevention
ERCP, endoscopic retrograde cholangiopancreatography.
DISCUSSION
Since the discovery of radiation, X-rays have been an integral part of medical care, and ERCP using fluoroscopy has become an important tool in diagnosis and treatment of pancreatobiliary disease. Therefore, radiation protective equipment has become an important tool for health care providers, and there has been growing interest in reducing radiation exposure.
Acute effects of radiation can be observed within a few weeks of exposure, including gastrointestinal symptoms such as nausea, vomiting, and diarrhea, central nervous system symptoms causing nerve damage and disorders, and bone marrow symptoms such as anemia. Chronic effects include leukemia, weakened immune system, mutation, and cancer. The International Commission on Radiological Protection (ICRP), through its recommendations, ICRP-60,6 divides exposure into occupational, public, and medical exposures. The recommendations allow occupational exposure of up to 50 millisivert (mSv) per year, but limit annual average doses below 20 mSv per year for 5 consecutive years. Public exposure doses are limited to 1 mSv per year. For occupational exposure, equivalent doses of exposure to lens are limited to 150 mSv per year, and those of exposure to skin, hands, and feet are limited to 500 mSv per year. The Korean Radioisotope Association also applies the limits recommended by ICRP-60.
Previous studies of radiation hazards during ERCP show different opinions on the amount of radiation exposure and hazard affecting health care providers. Cohen et al.3 reported that an ERCP procedure produces a high dose of radiation exposure. Their study warned of radiation hazards affecting health care providers during ERCP, arguing that health care providers must wear 0.5 mm-thick lead aprons, perform 23 procedures or less each month, not to exceed the annual radiation exposure limits affecting their bodies, that they are allowed to perform fewer than 19 procedures without thyroid shields and up to seven procedures without lead glasses. However, Heyd et al.5 countered that an average radiation dose from 25 ERCP procedures or more without protective equipment equaled 8.3 milliroentgen (mR), and that the dose can be reduced to 0.6 mR with a single piece of protective equipment such as a lead apron, or to 0.4 mR with two layers of protection such as a lead apron and a portable lead shield.
The doses of radiation exposure affecting health care providers during ERCP may vary depending on the imaging exposure time, the distance from the patient, and the use of protective equipment.7 It is therefore important to minimize radiation exposure using the aforementioned factors.
A study reported that radiation imaging time was reduced by 30% when an operator monitored the imaging time.8 Since most of those who practice ERCP focus on the procedure itself, they do not pay as much attention to the imaging time, but action is still needed to reduce imaging times to minimize radiation exposure during ERCP. Our survey implies that an ERCP procedure requires a long period of time of exposure to radiation, but does not reflect accurate periods of time, because the answers were based on the ERCP participants' opinions.
Protective equipment is essential to reduce radiation exposure. During an ERCP procedure, a lead apron, a thyroid shield, and lead glasses must be worn, whereas portable lead shields, lead gloves, and lead caps may be optional. The American Society for Gastrointestinal Endoscopy recommends that all health care providers wear lead aprons and have thyroid shields in place in order to practice ERCP, that those performing procedures close to their patients should wear lead glasses as well, and that lead shields should be set up in front of those performing endoscopy.9 Our survey found that most hospitals have lead aprons and thyroid shields in place, but only about 50% have lead glasses and lead shields, showing that many hospitals still lack essential equipment.
Regarding each form of protective equipment, first, a lead apron is the most essential piece of equipment to reduce radiation exposure. Naidu et al.10 reported that wearing a 0.25 mm-thick lead apron can prevent 90% of the radiation scattered at right angles. It is also reported that a lead apron covering the back and front of a person performing ERCP is a much better choice than a lead apron covering only the front of the body, because the person performing ERCP is forced to twist their body.11 Our survey showed that most health care providers wear lead aprons (98.7%). However, most respondents did not know the thickness of their lead aprons, but those who knew answered that their aprons were thicker than 0.25 mm. However, it was also found that many respondents still use lead aprons covering only the front part of their body in 39.7% of cases, indicating that the providers were still not very aware of the importance of the form of the lead apron. Second, a thyroid shield is also considered important protective equipment that reduces whole-body exposure, as well as thyroid exposure. A study reported that wearing thyroid shields can reduce the annual effective dose of radiation exposure by 46%.12 Our survey showed that most hospitals have thyroid shields available. Although thyroid shields are not considered as important as lead aprons, most health care providers still wear thyroid shields during ERCP. Third, lead glasses provide protection against cataracts arising from radiation exposure. Cumulative exposure over 2 Gray (Gy) reportedly causes cataracts.13 Therefore, those who practice ERCP for a few years or decades increase their risk for cataracts each year. However, lead glasses are less frequently worn than lead aprons or thyroid shields. Our survey showed that less than half of respondents have lead glasses in place and many respondents do not wear them often in 62.2% of cases. The common reason for not wearing protective equipment is that it is bothersome. It is important for health care providers participating in ERCP procedures to be aware of the importance of lead glasses and make it mandatory to wear them. Fourth, lead shields are known as an effective tool to provide protection against scattered radiation arising from ERCP. Chen et al.14 argued that, without lead shields in place, a person practicing a procedure is exposed to an average dose of 2.5 millirem (mrem), but with a 0.5 mm-thick lead shield, exposure can be reduced to 0.27 mrem. Therefore, it is very important to pay attention to secondary equipment such as lead shields. Our survey found that the preparation and actual utilization rate of lead shields were 55.3% and 61.9%, respectively. More attention needs to be paid to lead shields as well as lead glasses. Finally, radiation dosimeters do not provide protection against radiation, but tend to reduce radiation exposure because they are a crucial tool in drawing attention to radiation hazards. Those who practice ERCP should always measure radiation exposure and check their dosimeters on a periodic basis. Our survey found that the preparation and actual utilization rate of radiation dosimeters are 57.7% and 68.9%, respectively, indicating low interest in radiation exposure monitoring.
Recently in our country, the KPBA announced recommendations for ERCP-related radiation damage prevention in 2009. However, only 31 of the respondents to our survey (39.7%) were aware of the recommendations and only a few respondents had an accurate understanding of equipment priorities (16.1%), although most respondents considered lead aprons the most important. This indicated that the KPBA promotion for the recommendations may not be enough, and those who practice ERCP were not very interested in the recommendations. However, after reading the recommendations, there have been positive changes, such as changes in awareness of the efforts to prevent radiation exposure, the importance of protective equipment and purchases of additional equipment, and use of protective equipment at all times. After reading the recommendations, many hospitals have purchased lead glasses or lead shields, because most of them already had lead aprons, thyroid shields, and radiation dosimeters. However, because of the emphasis on the recommendations, there have been negative effects, such as a vague anxiety and avoidance of radiation exposure.
In limitations, first, there was no research regarding doses of radiation exposure, and the survey only targeted nurses and assistants. Recently, Son et al.15 reported that the actual utilization rate for lead aprons was 100% among endoscopists performing ERCP in Korea. However, compared with the health-care providers in our study, the actual utilization rates by endoscopists for other items were relatively low as follows: 94.7% versus 73% for thyroid shields, and 37.8% versus 20% for lead glasses, and 68.9% versus 13% for radiation dosimeters. Second, we could not objectively evaluate the actual correlations between health-care providers' exposure to radiation doses and their descriptions of the symptoms they experienced. The symptoms they presented were merely based on their subjective perceptions. Buls et al.16 reported that the gastroenterologists received, per procedure, a median dose of 0.34 mGy to the lens of the eye, 0.30 mGy to the skin at the level of the thyroid, and 0.44 mGy to the skin of the hands. Generally, in those radiation exposures, the symptoms described may be not associated with radiation exposure. In our survey, there were actually no responders who underwent medical management of these symptoms. Future surveys should include a study of doses of radiation exposure in Korean examples and target all health care providers, including doctors, nurses, and radiation technicians.
In conclusion, this survey identified the current status of radiation protective equipment in hospitals practicing ERCP, health care providers' usage of protective equipment, and their awareness of radiation exposure. Many hospitals still lack lead shields and lead glasses, and the actual utilization rate of lead glasses, especially, is low. Future efforts should include minimizing radiation exposure during ERCP procedures, and more interest in wearing and preparing protective equipment is needed. Also, KPBA should provide continuous education and supervision for radiation protection.
Footnotes
No potential conflict of interest relevant to this article was reported.
Appendix
The recommendation for endoscopic retrograde cholangiopancreatography-related radiation protection by the Korean Pancreatobiliary Association.
References
- 1.Hendee WR. Estimation of radiation risks. BEIR V and its significance for medicine. JAMA. 1992;268:620–624. [PubMed] [Google Scholar]
- 2.Kronenberg A. Radiation-induced genomic instability. Int J Radiat Biol. 1994;66:603–609. doi: 10.1080/09553009414551691. [DOI] [PubMed] [Google Scholar]
- 3.Cohen RV, Aldred MA, Paes WS, et al. How safe is ERCP to the endoscopist? Surg Endosc. 1997;11:615–617. doi: 10.1007/s004649900405. [DOI] [PubMed] [Google Scholar]
- 4.Wagner RH, Boles MA, Henkin RE. Treatment of radiation exposure and contamination. Radiographics. 1994;14:387–396. doi: 10.1148/radiographics.14.2.8190961. [DOI] [PubMed] [Google Scholar]
- 5.Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM. Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287–292. doi: 10.1016/s0016-5107(96)70166-9. [DOI] [PubMed] [Google Scholar]
- 6.1990 Recommendations of the international commission on radiological protection. Ann ICRP. 1991;21:1–201. [PubMed] [Google Scholar]
- 7.Uradomo LT, Goldberg EM, Darwin PE. Time-limited fluoroscopy to reduce radiation exposure during ERCP: a prospective randomized trial. Gastrointest Endosc. 2007;66:84–89. doi: 10.1016/j.gie.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 8.Vehmas T. Hawthorne effect: shortening of fluoroscopy times during radiation measurement studies. Br J Radiol. 1997;70:1053–1055. doi: 10.1259/bjr.70.838.9404210. [DOI] [PubMed] [Google Scholar]
- 9.Kimmey MB, Al-Kawas FH, Burnett DA, Carr-Locke DL, Gannan RM, Saeed ZA. Radiation safety during endoscopy. Gastrointest Endosc. 1994;40:801–804. [Google Scholar]
- 10.Naidu LS, Singhal S, Preece DE, Vohrah A, Loft DE. Radiation exposure to personnel performing endoscopic retrograde cholangiopancreatography. Postgrad Med J. 2005;81:660–662. doi: 10.1136/pgmj.2004.031526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell N, Sparrow K, Fortier M, Ponich T. Practical radiation safety and protection for the endoscopist during ERCP. Gastrointest Endosc. 2002;55:552–557. doi: 10.1067/mge.2002.122578. [DOI] [PubMed] [Google Scholar]
- 12.Niklason LT, Marx MV, Chan HP. Interventional radiologists: occupational radiation doses and risks. Radiology. 1993;187:729–733. doi: 10.1148/radiology.187.3.8497622. [DOI] [PubMed] [Google Scholar]
- 13.Merriam GR, Jr, Focht EF. A clinical study of radiation cataracts and the relationship to dose. Am J Roentgenol Radium Ther Nucl Med. 1957;77:759–785. [PubMed] [Google Scholar]
- 14.Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest Endosc. 1996;43:1–5. doi: 10.1016/s0016-5107(96)70250-x. [DOI] [PubMed] [Google Scholar]
- 15.Son BK, Lee KT, Kim JS, Lee SO. Lack of radiation protection for endoscopists performing endoscopic retrograde cholangiopancreatography. Korean J Gastroenterol. 2011;58:93–99. doi: 10.4166/kjg.2011.58.2.93. [DOI] [PubMed] [Google Scholar]
- 16.Buls N, Pages J, Mana F, Osteaux M. Patient and staff exposure during endoscopic retrograde cholangiopancreatography. Br J Radiol. 2002;75:435–443. doi: 10.1259/bjr.75.893.750435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The recommendation for endoscopic retrograde cholangiopancreatography-related radiation protection by the Korean Pancreatobiliary Association.