Abstract
Background/Aims
To determine if hepatocellular carcinoma refractory to conventional transarterial chemoembolization (TACE) responds to TACE with DC beads.
Methods
Between July 2008 to June 2010, 435 patients underwent TACE. Of these, 10 patients who had tumors refractory to conventional TACE and who thus were treated with TACE with DC beads were enrolled in this study. The treatment response after TACE with DC beads was evaluated according to the modified Response Evaluation Criteria in Solid Tumors (mRECIST) and the Response Evaluation Criteria in Cancer of the Liver (RECICL).
Results
Ten tumors were treated in 10 patients. Using the mRECIST and the RECICL, a complete response was observed in four (40%) of the tumors, and six tumors (60%) showed a partial response. Eight (80%) out of 10 HCCs showed delayed enhancement patterns upon angiography, and better responses were observed in these cases following DC bead treatment. The adverse effects of treatment with DC beads became tolerable.
Conclusions
TACE with DC beads was effective for HCCs refractory to conventional TACE, and this treatment elicited a better response, especially when the tumors were small and showed a delayed enhancement pattern upon angiography.
Keywords: Bead, Chemoembolization, Refractory, Hepatocellular carcinoma
INTRODUCTION
Hepatocellular carcinoma (HCC) is the sixth most common cancer in the world and the third most common cause of cancer mortality.1 The Barcelona Clinic Liver Cancer (BCLC) staging system directs therapy according to tumor stage, liver functional status, physical status, and cancer related symptoms.2 However, over 60% to 70% of HCC patients are diagnosed at late stages and therefore curative therapies such as resection, liver transplantation, or local ablation therapy cannot be applied.3
Transarterial chemoembolization (TACE) is the primary treatment used most frequently for unresectable HCCs. TACE has been shown to improve survival in comparison to best supportive care for unresectable HCC.4,5 However, the objective response rate of TACE is only 15% to 55%,6 and the tumor recurrence rate is 70% at 5 years.7 In addition, the systemic release of chemotherapeutic agents is frequent, and many patients suffer from systemic side effects.8
DC beads are a novel drug delivery embolization system comprised of biocompatible, nonresorbable polyvinyl alcohol polymer hydrogel beads which can be loaded with cytotoxic drugs.9 The beads have a high affinity for drugs and this enables the gradual release of doxorubicin into the tumor, allowing a longer intratumoral exposure and less systemic exposure of the drug, reducing systemic toxicity.10 In an in vivo study using a rabbit model, the intratumor drug level after the use of DC beads was much higher than after conventional chemoembolization.11 Some studies showed that TACE with DC Beads resulted in a better response compared to conventional TACE, with more complete response (CR) rate and histological necrosis rate.7,10,12 However, it has not been clearly defined whether tumors that are refractory to conventional TACE would show good response to TACE with DC beads. Thus, we retrospectively analyzed patients who underwent TACE with DC beads for HCC refractory to conventional TACE. In addition, we assessed the tumor characteristics that showed good response to TACE with DC beads.
MATERIALS AND METHODS
1. Patients refractory to conventional TACE
Between July 2008 and June 2010, 435 patients underwent TACE at Seoul St. Mary's Hospital. Of those patients, 10 consecutive patients who had tumors refractory to conventional TACE and were treated with DC beads were enrolled in this study. Ten tumors refractory to conventional TACE were analyzed in the 10 patients.
Tumors refractory to conventional TACE were defined as those with more than two consecutive incomplete necrosis (depositions <50% of lipiodol) on computed tomography (CT) that was used to evaluate response to TACE.13 We performed the response evaluation with CT at 1 to 2 months after conventional TACE.
2. Procedure of TACE with DC Beads
After a full angiographic study of the celiac trunk, superior mesenteric artery, and hepatic artery using a peripheral arterial approach, highly selective catheterization of the segmental arterial branches feeding the tumor was performed. Doxorubicin uploaded in 2 mL of DC beads with diameters ranging from 100 to 300 µm or from 300 to 500 µm, were injected into the arterial branches feeding the tumor. The dose of doxorubicin was determined by tumor size.
3. Classification of tumor staining in angiography
According to the angiographic findings, we divided the tumors into two groups, one group with regular enhancement pattern and one with a delayed enhancement pattern. If the tumor was stained at the time when the common, proper, and right and left hepatic arteries were observed, it was defined as a regular enhancement pattern (Fig. 1). If the tumor was stained when the segmental or subsegmental arteries were observed, it was defined as a delayed enhancement pattern (Fig. 2).
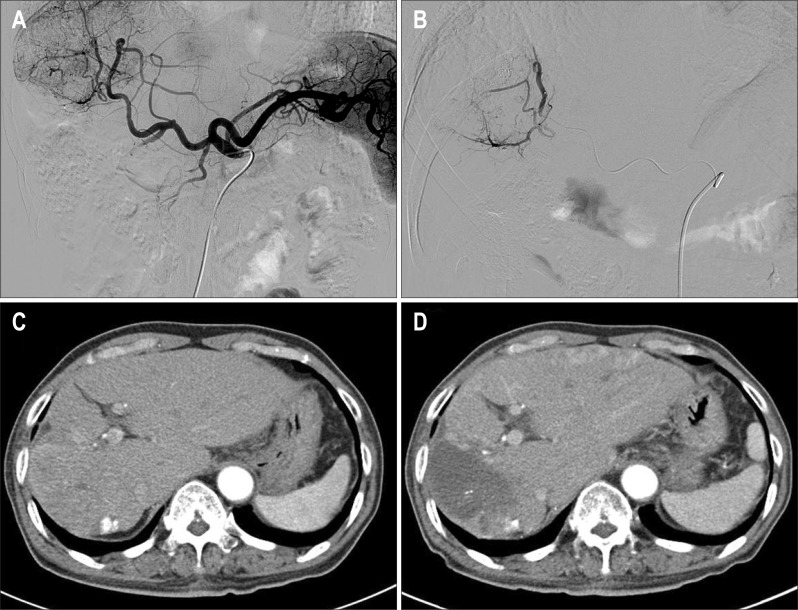
Fig. 1.
The representative angiogram of regular enhancement pattern (A, B) and treatment outcome (C, D) (Patients number 6). (A) Arterial stain in angiography of celiac trunk. (B) Selection of feeding artery and embolization using DC beads. (C) Computed tomography (CT) imaging before treatment with DC beads. (D) CT imaging after treatment with DC beads (partial response by modified Response Evaluation Criteria in Solid Tumors).
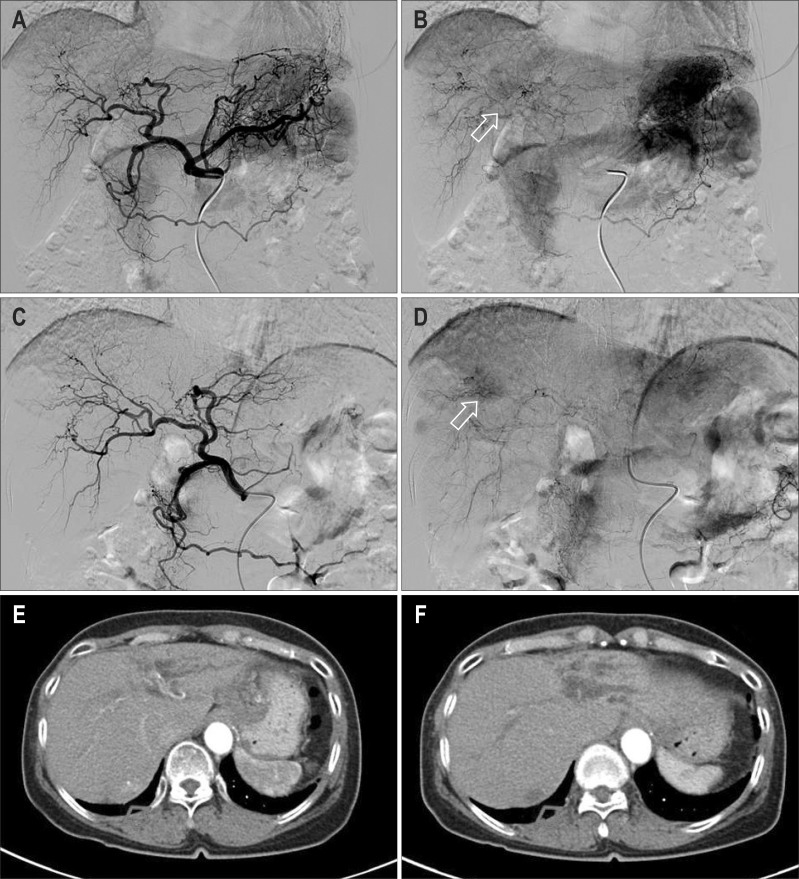
Fig. 2.
The representative angiogram of delayed enhancement pattern (A, B, C, D) and treatment outcome (E, F) (Patients number 1). (A, C) No arterial enhance while proper, right, and left hepatic artery were seen in angiography of celiac trunk and common hepatic artery. (B, D) Tumor staining while segmental and subsegmental arteries were seen in angiography of celiac trunk and hepatic artery. (E) Computed tomography (CT) imaging before treatment with DC beads. (F) CT imaging after treatment with DC beads (complete response by modified Response Evaluation Criteria in Solid Tumors).
4. Assessment of the therapeutic effects
Antitumor effect was evaluated by comparing the dynamic CT imaging before treatment to the imaging 1 to 2 months after treatment with DC beads.
Treatment response of the target tumor was evaluated by two methods: the modified Response Evaluation Criteria in Solid Tumors (mRECIST)14 and the Response Evaluation Criteria in Cancer of the Liver (RECICL).15 According to the mRECIST for HCC, CR of the target tumor was defined as the disappearance of any intratumoral enhancement on CT obtained 1 month after treatment. Partial response (PR) was defined as at least a 30% decrease in the sum of diameters of viable (contrast enhancement in the arterial phase) target lesions, taking as reference the baseline sum of the diameters of target lesions. Progressive disease was defined as an increase of at least 20% in the sum of the diameters of viable (enhancing) target lesions. Stable disease was defined as any cases that did not qualify for either PR or progressive disease.
The necrotizing effect of the DC beads was evaluated by calculating the size reduction rate according to RECICL.15 The direct treatment effect on the target nodule was divided into four categories according to size reduction rate. CR was defined as a 100% tumor-necrotizing effect or 100% tumor size reduction rate. The tumors with a necrotizing effect or size reduction rate between 50% and 100% were considered to have PR. Progressive disease (PD) was when the tumors grew over 25%, regardless of the necrotizing effect.
Toxicity related to treatment with DC beads was assessed by Common Terminology Criteria for Adverse Events version 4.0.16 In addition, tumor markers, such as alpha-fetoprotein and protein induced by vitamin K absence or antagonist-II, were checked before and after TACE with DC beads.
5. Statistical analysis
In this study, statistical analysis was performed to compare the size reduction ratio. Size reduction ratio according to the tumor size was compared using the Mann-Whitney U test. A p-value of less than 0.05 was considered statistically significant. Analysis was performed using SPSS version 15.0 software (SPSS Inc., Chicago, IL, USA).
RESULTS
1. Patients and tumor characteristics
The characteristics of the patients are listed in Table 1. Ten patients were men, and one patient was a woman, with a median age of 64.5 years (range, 45 to 75 years). The etiology of HCC was related to hepatitis B virus (HBV) in five patients, co-infection of HBV and hepatitis C virus in three patients, alcoholic liver disease in one patient, and another factor in one patient. There was no hepatitis C related patient.
Table 1.
Baseline Characteristics of 10 Patients Refractory to Conventional TACE
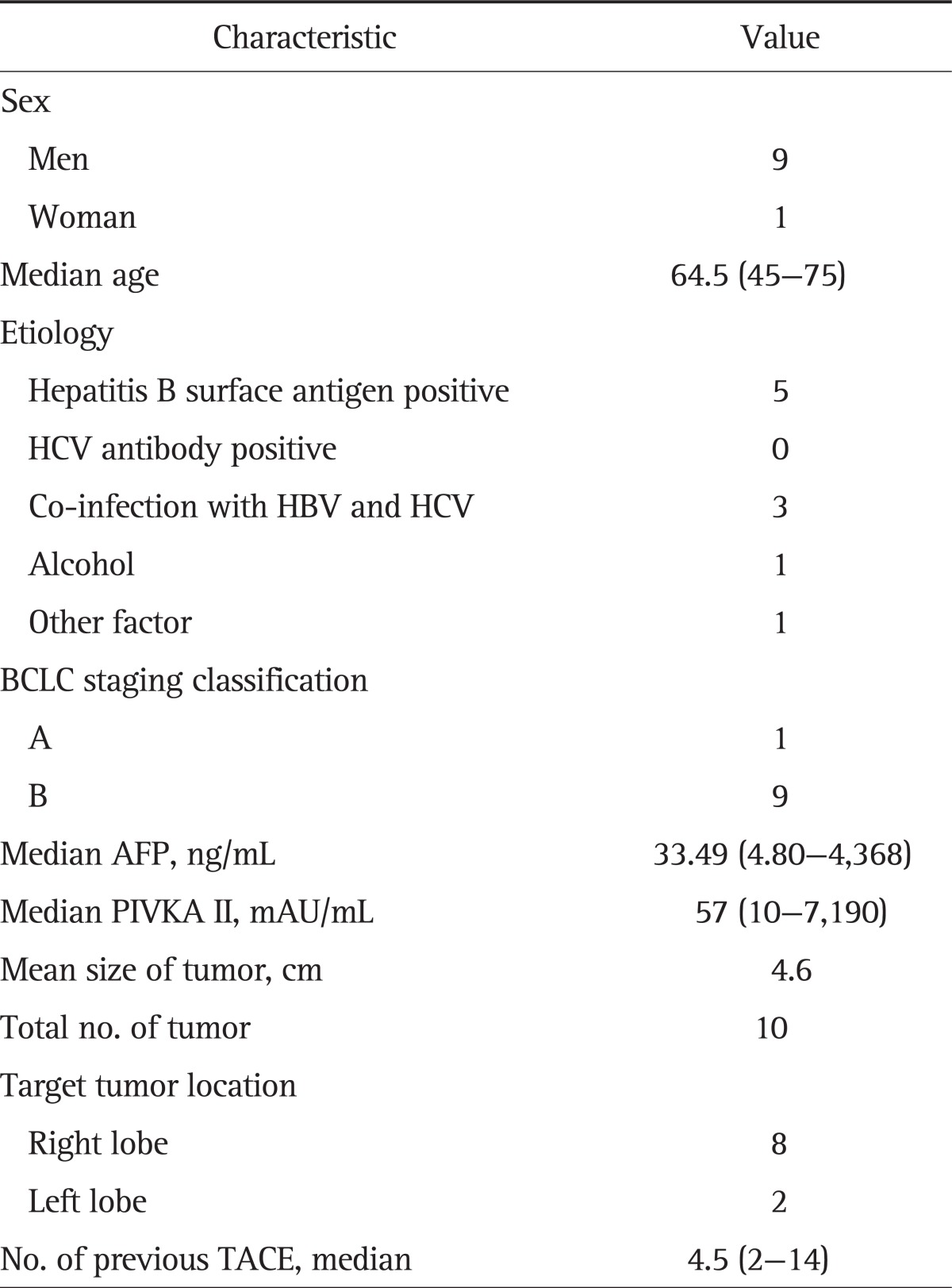
Data are presented as number or median (range).
TACE, transarterial chemoembolization; HBV, hepatitis B virus; HCV, hepatitis C virus; BCLC, Barcelona Clinic Liver Cancer; AFP, alpha-fetoprotein; PIVKA II, protein induced by the absence of vitamin K or antagonist II.
According to the Barcelona Clinic for Liver Cancer staging classification, one patient was in stage A, and nine patients were in stage B. One patient who was in BCLC stage A had three tumors less than 3 cm, but could not undertake curative treatment. The mean size of the target tumor was 4.6 cm at the time of treatment. Four tumors were of infiltrating types, one was multinodular, and the others were of nodular types. The patients underwent conventional TACE a median of 4.5 times (range, 2 to 14 times) before TACE with DC beads.
2. Pattern of tumor staining and tumor response after TACE with DC beads
The initial CT findings, angiographic enhancement pattern, follow-up CT findings, and responses are listed in Table 2. Eight (80.0%) of 10 tumors showed delayed enhancement pattern on angiography. According to the mRECIST and RECICL criteria, CR was observed in four tumors (40%) and PR in six tumors (60%). Objective response was seen in all tumors (100%). All tumors that achieved CR had delayed enhancement pattern. Of the six tumors that achieved PR, four tumors showed delayed enhancement pattern, and two tumors regular enhancement pattern.
Table 2.
Response to Conventional TACE and DC Bead TACE
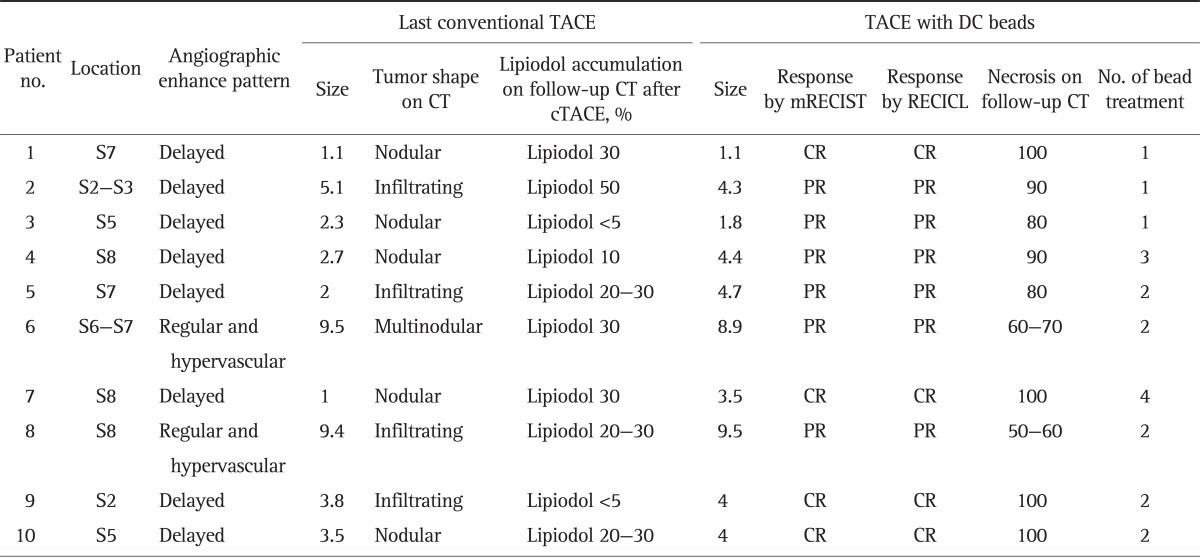
TACE, transarterial chemoembolization; CT, computed tomography; mRECIST, modified Response Evaluation Criteria in Solid Tumors; RECICL, Response Evaluation Criteria in Cancer of the Liver; CR, complete response; PR, partial response.
When the tumors were evaluated by RECICL criteria, those which showed regular and hypervascular pattern on angiography resulted in lower size reduction rate compared with the tumors which showed delayed enhancement pattern (92.5% vs 60.0%). Patients with HCC under 4 cm showed better response as in size reduction rate (mean, 96% vs 76%; p=0.03).
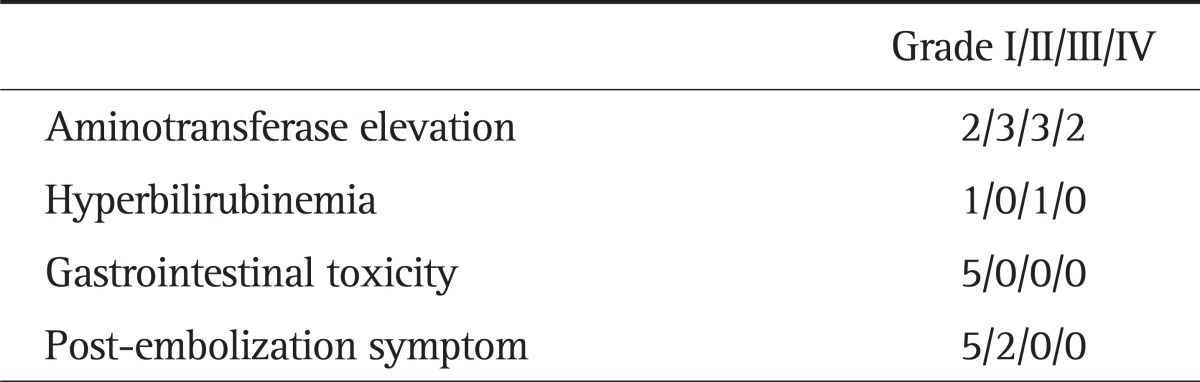
3. Treatment-related toxicity
Toxicities associated with treatment are reported in Table 3. Overall, toxicities were transient and tolerable and they were successfully managed by conservative treatment. Post-embolization symptoms, such as fever or pain, occurred in seven patients, and its degree was mild. The most common toxicity was aminotransferase elevation (10 patients). Two patients experienced grade IV, three patients grade III, and five patients a mild elevation (grade I and II). Elevation of bilirubin was documented in two patients. Five patients experienced mild gastrointestinal symptoms (nausea or vomiting) (Table 3).
Table 3.
Treatment-Related Toxicity
4. Clinical courses after TACE with DC beads
The clinical courses after treatment with DC bead are listed in Table 4. The mean follow-up duration after 1st TACE with DC bead was 616 days. Five patients died and four patients remained alive at the end of the follow-up. Seven out of 10 targeted tumors eventually progressed, and mean time to progression was 235 days. After DC bead treatment additional treatments such as external radiation therapy on bone metastases, hepatic arterial infusion chemotherapy, rachofrequency ablation and sorafenib were given as necessary.
Table 4.
Clinical Courses after TACE with DC Beads
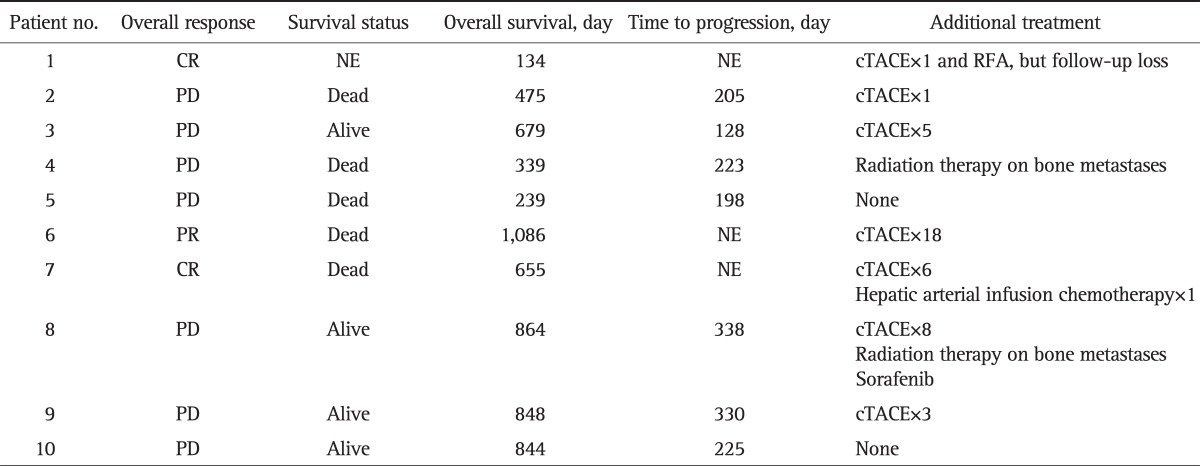
TACE, transarterial chemoembolization; CR, complete response; NE, not evaluable; RFA, rachofrequency ablation; PD, progressive disease; PR, partial response.
DISCUSSION
In this study, HCC refractory to conventional TACE tended to show better response to DC bead treatment. Objective response (CR and PR) with DC bead TACE was observed in 100% (10 tumors). Of the 10 refractory HCCs to conventional TACE, 40% showed CR. CR was more common in nodular type HCC than infiltrating or multinodular type HCC. In addition, all of the tumors that reached CR showed delayed enhancement pattern on angiography while two tumors that ended in PR showed regular and hypervascular enhancement pattern.
Several studies have suggested survival benefits from conventional TACE.4,5,17 However, some limitations lead to refractoriness to conventional TACE that uses a cytotoxic drug emulsified with lipiodol followed by the delivery of an embolizing agent. First, not all HCCs show lipiodol retention.18 Heterogeneous lipiodol retention in some HCCs may render the treatment less effective.19 Second, even with the use of lipiodol, the cytotoxic drug can be washed out into the systemic circulation20 which would decrease the effects of conventional TACE by reduced concentration of the drug in the tumor and at the same time incur systemic toxicity. In this study, tumors refractory to conventional TACE also showed little retention of lipiodol, mostly less than 50% of tumor. Therefore, DC beads can be a valuable alternative to some types of HCC refractory to conventional TACE due to their pharmacologic property.
In the porcine model, histological examination showed that induced necrosis radiated outwards with clusters of DC beads in the center. Both liquefactive and coagulative necrosis developed indicating the ischemic and toxic nature of cell death.21 Tumor necrosis was greatest at 7 to 14 days after treatment; during that period, the combined amount of damaged and necrotic cells approached 100%, while plasma concentration of doxorubicin was minimal.21 In a recent study on the explanted liver, histologic necrosis and the CR rate were significantly higher in the DC beads group than in the conventional TACE group.12 In addition, another study with explanted liver demonstrated that DC beads provided a sustained delivery of the drug for a period of 1 month with local tissue concentration above the cytotoxic threshold.22 Sustained drug release for a longer duration in the tumor with DC bead TACE explains the good response rate in HCC refractory to conventional TACE in which cases lipiodol accumulation rate is low and cytotoxic agents are washed out easily and quickly.
Interestingly, we found that most of the tumors refractory to conventional TACE had delayed enhancement pattern on angiography. In addition, those with delayed enhancement pattern showed better response to DC bead treatment than tumors that showed regular enhancement pattern. The enhancement pattern and response rate could be related to hepatocarcinogenesis. Hepatocarcinogenesis is a multistep process in which hyperplastic nodule develops to be an early HCC and eventually advanced overt hypervascular HCC.23 Most well-differentiated HCCs at an early stage do not stain upon angiography or do not retain lipiodol within the tumor.24-26 Although we did not perform biopsy, HCCs that had delayed enhancement pattern and did not retain lipiodol compactly in this study are likely be well-differentiated early stage HCCs in which the arterial vascularity did not develop fully enough. In contrast, good response to DC bead TACE would be associated with longer release of doxorubicin from the beads.
Tumor size is an important predictive factor for response to TACE. The responses after conventional TACE were better for small tumors than for larger tumors.27,28 In this study, small tumors with sizes less than 4 cm showed better response than larger tumors (mean size reduction rate, 96% vs 76%; p=0.03).
All patients developed more than one adverse symptom or sign after DC bead treatment. The most common adverse effect was elevation of liver enzymes (10 of 10 patients), followed by post-embolization symptom (seven of 10 patients). Grade 4 and grade 3 elevation of liver enzymes developed in two and three patients, respectively. However, all hepatic toxicity returned to baseline level in several days. The incidence and frequency of signs and symptoms were comparable to previous reports on adverse events of conventional TACE29 and DC beads treatment.30,31
This study has several limitations. First, the sample size was relatively small, enabling us to draw only preliminary conclusions regarding the potential value of TACE with DC beads on tumors refractory to conventional TACE. Second, this study is underpowered by its retrospective nature and single arm registry without a control group. Further studies in a larger cohort are undoubtedly necessary to confirm these preliminary findings.
In conclusion, this study demonstrated that TACE with DC beads could induce an objective response in tumors refractory to conventional TACE which suggests another specific indication of DC bead TACE in current practice. Among the tumors refractory to conventional TACE, TACE with DC beads can help to elicit a better response in BCLC stage B HCC especially if the tumor size is relatively small and in cases when delayed enhancement pattern is demonstrated on angiography.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Bruix J, Sherman M Practice Guidelines Committee; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 3.Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol. 2008;48(Suppl 1):S20–S37. doi: 10.1016/j.jhep.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 4.Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 5.Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: Chemoembolization improves survival. Hepatology. 2003;37:429–442. doi: 10.1053/jhep.2003.50047. [DOI] [PubMed] [Google Scholar]
- 6.Bruix J, Sala M, Llovet JM. Chemoembolization for hepatocellular carcinoma. Gastroenterology. 2004;127(5 Suppl 1):S179–S188. doi: 10.1053/j.gastro.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 7.Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 8.Marelli L, Stigliano R, Triantos C, et al. Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol. 2007;30:6–25. doi: 10.1007/s00270-006-0062-3. [DOI] [PubMed] [Google Scholar]
- 9.Lammer J, Malagari K, Vogl T, et al. Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Intervent Radiol. 2010;33:41–52. doi: 10.1007/s00270-009-9711-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meza-Junco J, Montano-Loza AJ, Liu DM, et al. Locoregional radiological treatment for hepatocellular carcinoma: which, when and how? Cancer Treat Rev. 2012;38:54–62. doi: 10.1016/j.ctrv.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Hong K, Khwaja A, Liapi E, Torbenson MS, Georgiades CS, Geschwind JF. New intra-arterial drug delivery system for the treatment of liver cancer: preclinical assessment in a rabbit model of liver cancer. Clin Cancer Res. 2006;12:2563–2567. doi: 10.1158/1078-0432.CCR-05-2225. [DOI] [PubMed] [Google Scholar]
- 12.Nicolini A, Martinetti L, Crespi S, Maggioni M, Sangiovanni A. Transarterial chemoembolization with epirubicin-eluting beads versus transarterial embolization before liver transplantation for hepatocellular carcinoma. J Vasc Interv Radiol. 2010;21:327–332. doi: 10.1016/j.jvir.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 13.Kudo M, Izumi N, Kokudo N, et al. Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig Dis. 2011;29:339–364. doi: 10.1159/000327577. [DOI] [PubMed] [Google Scholar]
- 14.Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30:52–60. doi: 10.1055/s-0030-1247132. [DOI] [PubMed] [Google Scholar]
- 15.Kudo M, Kubo S, Takayasu K, et al. Response Evaluation Criteria in Cancer of the Liver (RECICL) proposed by the Liver Cancer Study Group of Japan (2009 revised version) Hepatol Res. 2010;40:686–692. doi: 10.1111/j.1872-034X.2010.00674.x. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events (CTCAE) Bethesda: National Cancer Institute; 2009. [Google Scholar]
- 17.Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734–1739. doi: 10.1016/S0140-6736(02)08649-X. [DOI] [PubMed] [Google Scholar]
- 18.Poyanli A, Rozaneş I, Acunaş B, Sencer S. Palliative treatment of hepatocellular carcinoma by chemoembolization. Acta Radiol. 2001;42:602–607. doi: 10.1080/028418501127347278. [DOI] [PubMed] [Google Scholar]
- 19.Lee JK, Chung YH, Song BC, et al. Recurrences of hepatocellular carcinoma following initial remission by transcatheter arterial chemoembolization. J Gastroenterol Hepatol. 2002;17:52–58. doi: 10.1046/j.1440-1746.2002.02664.x. [DOI] [PubMed] [Google Scholar]
- 20.Johnson PJ, Kalayci C, Dobbs N, et al. Pharmacokinetics and toxicity of intraarterial adriamycin for hepatocellular carcinoma: effect of coadministration of lipiodol. J Hepatol. 1991;13:120–127. doi: 10.1016/0168-8278(91)90873-a. [DOI] [PubMed] [Google Scholar]
- 21.Lewis AL, Taylor RR, Hall B, Gonzalez MV, Willis SL, Stratford PW. Pharmacokinetic and safety study of doxorubicin-eluting beads in a porcine model of hepatic arterial embolization. J Vasc Interv Radiol. 2006;17:1335–1343. doi: 10.1097/01.RVI.0000228416.21560.7F. [DOI] [PubMed] [Google Scholar]
- 22.Namur J, Citron SJ, Sellers MT, et al. Embolization of hepatocellular carcinoma with drug-eluting beads: doxorubicin tissue concentration and distribution in patient liver explants. J Hepatol. 2011;55:1332–1338. doi: 10.1016/j.jhep.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 23.Kudo M. Multistep human hepatocarcinogenesis: correlation of imaging with pathology. J Gastroenterol. 2009;44(Suppl 19):112–118. doi: 10.1007/s00535-008-2274-6. [DOI] [PubMed] [Google Scholar]
- 24.Krinsky G. Imaging of dysplastic nodules and small hepatocellular carcinomas: experience with explanted livers. Intervirology. 2004;47:191–198. doi: 10.1159/000078472. [DOI] [PubMed] [Google Scholar]
- 25.Murakami T, Hori M, Kim T, Kawata S, Abe H, Nakamura H. Multidetector row CT and MR imaging in diagnosing hepatocellular carcinoma. Intervirology. 2004;47:209–226. doi: 10.1159/000078474. [DOI] [PubMed] [Google Scholar]
- 26.Kudo M. Atypical large well-differentiated hepatocellular carcinoma with benign nature: a new clinical entity. Intervirology. 2004;47:227–237. doi: 10.1159/000078475. [DOI] [PubMed] [Google Scholar]
- 27.Ebied OM, Federle MP, Carr BI, et al. Evaluation of responses to chemoembolization in patients with unresectable hepatocellular carcinoma. Cancer. 2003;97:1042–1050. doi: 10.1002/cncr.11111. [DOI] [PubMed] [Google Scholar]
- 28.Herber SC, Otto G, Schneider J, et al. Transarterial chemoembolization in patients not eligible for liver transplantation: single-center results. AJR Am J Roentgenol. 2008;190:1035–1042. doi: 10.2214/AJR.07.2755. [DOI] [PubMed] [Google Scholar]
- 29.Chan AO, Yuen MF, Hui CK, Tso WK, Lai CL. A prospective study regarding the complications of transcatheter intraarterial lipiodol chemoembolization in patients with hepatocellular carcinoma. Cancer. 2002;94:1747–1752. doi: 10.1002/cncr.10407. [DOI] [PubMed] [Google Scholar]
- 30.Sacco R, Bargellini I, Bertini M, et al. Conventional versus doxorubicin-eluting bead transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2011;22:1545–1552. doi: 10.1016/j.jvir.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Malagari K, Alexopoulou E, Chatzimichail K, et al. Transcatheter chemoembolization in the treatment of HCC in patients not eligible for curative treatments: midterm results of doxorubicin-loaded DC bead. Abdom Imaging. 2008;33:512–519. doi: 10.1007/s00261-007-9334-x. [DOI] [PubMed] [Google Scholar]