Abstract
Cognitive impairments associated with dysfunction of the medial prefrontal cortex (mPFC) are prominent in stress-related psychiatric disorders. We have shown that enhancing noradrenergic tone acutely in the rat mPFC facilitated extra-dimensional (ED) set-shifting on the attentional set-shifting test (AST), whereas chronic unpredictable stress (CUS) impaired ED. In this study, we tested the hypothesis that the acute facilitatory effect of norepinephrine (NE) in mPFC becomes detrimental when activated repeatedly during CUS. Using microdialysis, we showed that the release of NE evoked in mPFC by acute stress was unchanged at the end of CUS treatment. Thus, to then determine if repeated elicitation of this NE activity in mPFC during CUS may have contributed to the ED deficit, we infused a cocktail of α1-, β1-, and β2-adrenergic receptor antagonists into the mPFC prior to each CUS session, then tested animals drug free on the AST. Antagonist treatment prevented the CUS-induced ED deficit, suggesting that NE signaling during CUS compromised mPFC function. We confirmed that this was not attributable to sensitization of adrenergic receptor function following chronic antagonist treatment, by administering an additional microinjection into the mPFC immediately prior to ED testing. Acute antagonist treatment did not reverse the beneficial effects of chronic drug treatment during CUS, nor have any effect on baseline ED performance in chronic vehicle controls. Thus, we conclude that blockade of noradrenergic receptors in mPFC protected against the detrimental cognitive effects of CUS, and that repeated elicitation of noradrenergic facilitatory activity is one mechanism by which chronic stress may promote mPFC cognitive dysfunction.
Keywords: depression, chronic stress, norepinephrine, medial prefrontal cortex, cognitive flexibility
INTRODUCTION
Cognitive deficits associated with prefrontal cortical dysfunction play an integral role in the onset and maintenance of stress-related neuropsychiatric illnesses, such as depression and anxiety disorders (Kendler et al, 1999; Murphy et al, 1999; Austin et al, 2001; Beck, 2005; Disner et al, 2011). Depressed patients commonly express impairments in cognitive flexibility, that is, the ability to modify pre-established patterns of thought or behavior based on feedback from the environment (Channon, 1996; Merriam et al, 1999; Murphy et al, 1999; Austin et al, 2001; Disner et al, 2011). The attentional set-shifting test (AST) was developed to measure cognitive flexibility in rats, including extra-dimensional (ED) cognitive set-shifting, which depends critically on the functional integrity of the medial prefrontal cortex (mPFC) (Birrell and Brown, 2000). This region has been shown to be hypoactive in depressed patients and individuals exposed to chronic psychosocial stress (Stuss et al, 2000; Siegle et al, 2007; Fales et al, 2009; Liston et al, 2009). In previous studies, we found that chronic unpredictable stress (CUS) compromised the performance of rats on the ED stage of the AST (Bondi et al, 2008, 2010). However, despite clinical and preclinical evidence demonstrating that chronic stress impairs mPFC cognitive function and is a risk factor for depression, the mechanisms underlying these relationships remain unknown.
Norepinephrine (NE) modulates cortical function under conditions of stress, vigilance, arousal, and attention (Aston-Jones et al, 1991; Cole and Robbins, 1992; Berridge et al, 1993; Berridge and Waterhouse, 2003; Morilak et al, 2005). Previous results from our laboratory showed that enhancing noradrenergic tone acutely by administration of the α2-adrenergic autoreceptor antagonist, atipamezole, facilitated ED performance through activation of α1-adrenergic receptors in the mPFC (Lapiz and Morilak, 2006). Further, chronic administration of the selective NE reuptake inhibitor, desipramine, during CUS prevented the stress-induced ED deficits (Bondi et al, 2008, 2010). These observations are consistent with monoamine theories of depression, which suggest that depressive behaviors (eg, impairments of cognitive flexibility) result from deficiencies in monoaminergic modulatory function (Glavin, 1985; Anisman and Zacharko, 1990; Ressler and Nemeroff, 2000; Nutt, 2002; Morilak and Frazer, 2004). However, recently we showed that noradrenergic modulation in the mPFC remains intact after CUS, in that acute atipamezole administration still enhanced ED performance, and α1-receptors in the mPFC continued to facilitate cognitive flexibility after CUS (Bondi et al, 2010). Given that acute stress evokes NE release in the mPFC (Nakane et al, 1994), these observations suggested that stress-induced NE activity may be maintained over the course of CUS, and that repeated elicitation could impair the functional integrity of the mPFC, that is, that repeated facilitation creates an allostatic overload (McEwen, 2004).
Allostatic overload, a physiological mediator's inability to maintain homeostasis after prolonged activation induces maladaptive responses, has been studied extensively with respect to the stress hormone corticosterone (McEwen, 2003, 2004; de Kloet et al, 2005). Studies have shown that acute stress and systemic corticosterone administration evoke glutamate release in the hippocampus and mPFC (Moghaddam et al, 1994; Bagley and Moghaddam, 1997; Venero and Borrell, 1999). This acute response is associated with glutamate facilitating cognitive function, thus enabling an organism to better cope with environmental demands (Joels et al, 2006; Yuen et al, 2009, 2011). Conversely, prolonged stress exposure and chronic corticosterone treatment lead to dendritic atrophy in the hippocampus and mPFC (Magarinos and McEwen, 1995; Wellman, 2001; Cook and Wellman, 2004). This morphological consequence of chronic corticosterone exposure has been associated with excessive glutamate release and impaired cognitive function (Magarinos and McEwen, 1995; McEwen et al, 1997; Liston et al, 2006; Martin and Wellman, 2011).
Similar to corticosterone, NE modulates basal excitatory signaling and acute stress-evoked glutamate release in the mPFC (Marek and Aghajanian, 1999; Lupinsky et al, 2010). Therefore, through a process of cumulative excitotoxicity or similar negative consequence of repeated facilitation, repeated stress-induced noradrenergic activity in the mPFC may play a role in the development of CUS-induced ED deficits. Thus, the present study tested the hypothesis that the modulatory effects of NE in the mPFC, which enhance cognitive flexibility acutely, may contribute to the development of cognitive dysfunction when elicited repeatedly over the course of CUS treatment. We first used in vivo microdialysis to establish that acute stress continues to induce NE release in the mPFC at the end of the 2-week CUS procedure. Subsequently, to determine if this repeated elicitation of NE activity in the mPFC during CUS compromises cognitive flexibility, we microinjected α1-, β1-, and β2-adrenergic receptor antagonists into the mPFC prior to each CUS session. Following chronic drug and stress treatment, cognitive set-shifting capability was tested on the AST. Portions of this work have been presented in abstract form (Jett et al, 2008).
MATERIALS AND METHODS
Animals
A total of 152 adult male Sprague-Dawley rats (Harlan, USA), 230–250 g upon arrival, were initially grouped-housed (three rats/cage) in 25 × 45 × 15 cm3 cages, on a 12/12-h light/dark cycle (lights on at 0700 hours), and provided food and water ad libitum. For social defeat, 24 male Long-Evans rats, 400–450 g (Charles River, USA), were pair-housed with ovariectomized females in large cages (63 × 63 × 40 cm3) in an adjacent room. Experiments were conducted during the light phase. All procedures were in accordance with NIH guidelines and approved by the UTHSCSA Institutional Animal Care and Use Committee.
Chronic Unpredictable Stress
CUS was conducted as described previously (Bondi et al, 2008, 2010), excluding swim stress to avoid infection following surgery. A different stressor was administered daily, at various times of day, for 2 weeks (Table 1). Following each session, rats recovered for 1 h in an isolated room, then were transferred to clean cages and returned to housing. Unstressed controls were handled 2–3 min/day.
Table 1. CUS Treatment Schedule.
| Day 1 | 30-min restraint |
|---|---|
| Day 2 | 1-h shaking/crowding (6 rats/box, 220 shakes/min) |
| Day 3 | Social defeat (with 45 min protected exposure post-defeat) |
| Day 4 | 10-min tail pinch (in restraint tube) |
| Day 5 | 24-h wet bedding |
| Day 6 | Social defeat |
| Day 7 | 1-h shaking/crowding |
| Day 8 | 15-min mild footshock (30 s every 3 min, 5 s on/5 s off. 1.5 mA) |
| Day 9 | 30-min restraint |
| Day 10 | Social defeat (begin food restriction, when applicable, for AST expts) |
| Day 11 | 15-min mild footshock |
| Day 12 | 10-min tail pinch |
| Day 13 | 24-h wet bedding |
| Day 14 | 15-min mild footshock |
| Day 15 | Habituation day for AST |
| Day 16 | Training day for AST |
| Day 17 | Testing day for AST |
Attentional Set-Shifting Test
AST procedures were as described previously (Lapiz and Morilak, 2006). One week before testing, rats were food restricted to 14 g/day. The testing arena was 75 × 44 × 30 cm3 with a removable divider at one end to form a start box. A clear panel divided the opposite third into two sections. A terracotta digging pot (diameter 7 cm, depth 6 cm) was placed in each section. Pots were differentiated along two dimensions, digging medium and odor (see Table 2). Each pot was initially scented with 20 μl of aromatic oil (Frontier Natural Brands, Boulder, CO, USA), then 1–2 μl daily for consistency. Only one combination of odor/medium was applied to each pot. A 1/4 piece of Honey Nut Cheerio (General Mills Cereals, Minneapolis, MN, USA), was buried at a depth of 3 cm in the ‘positive' pot. Prior to each stage, powdered Cheerio was sprinkled onto the medium of both pots to prevent location of the reward by smell. Trials were initiated by lifting the start gate, allowing access to both pots. AST was conducted over 3 days:
Table 2. Attentional Set-Shifting Test Protocola.
| Discrimination stage | Dimensions | Example combinations | ||
|---|---|---|---|---|
| |
Relevant |
Irrelevant |
(+) |
(−) |
| Simple (SD) | Odor | Clove/Sawdust | Nutmeg/Sawdust | |
| Compound (CD) | Odor | Medium | Clove/Raffia Clove/Metallic Filler | Nutmeg/Metallic Filler Nutmeg/Raffia |
| Reversal 1 (R1) | Odor | Medium | Nutmeg/Raffia Nutmeg/Metallic Filler | Clove/Metallic Filler Clove/Raffia |
| Intra-dimensional shift (ID) | Odor | Medium | Rosemary/Wood balls Rosemary/Plastic beads | Cinnamon/Plastic beads Cinnamon/Wood balls |
| Reversal 2 (R2) | Odor | Medium | Cinnamon/Plastic beads Cinnamon/Wood balls | Rosemary/Wood balls Rosemary/Plastic beads |
| Extra-dimensional set-shift (ED) | Medium | Odor | Velvet/Citronella Velvet/Thyme | Crepe/Thyme Crepe/Citronella |
Representative examples of stimulus pairs, and the progression through the stages of the attentional set-shifting test, with odor as the initial discriminative dimension, shifting to digging medium in the ED stage. Half the rats began with medium as the initial stimulus and shifted to odor. For each task, the positive stimulus is in bold, and is paired randomly across trials with the two stimuli from the irrelevant dimension.
Day 1: Habituation
Rats were trained to dig for reward in unscented pots filled with sawdust.
Day 2: Training
Rats were trained to make simple discriminations (SDs) in the testing arena. They first learned to associate reward with odor (lemon vs rosewood, pots filled with sawdust) then digging medium (felt vs paper, no odor). Training stimuli were not used during testing.
Day 3: Testing
Rats were tested on a series of discrimination tasks, in which the discriminative stimulus dimension and positive cue within that dimension were varied according to the contingency schedule in Table 2. The first task was a SD, similar to the training trials, involving only one stimulus dimension. Half the rats had to discriminate between pots differentiated by odor, and the other half discriminated between digging media in unscented pots (for clarity, the remainder of this description will consider odor discrimination). The second task was a compound discrimination (CD), in which the same discrimination was required, but the second, irrelevant stimulus (eg, medium) was introduced. The third task was a reversal (R1), in which the same odors and media were used, but the negative odor from the previous task was now positive. The fourth task was an intra-dimensional shift (ID), in which all new stimuli were introduced, and odor remained the relevant dimension. The fifth task was a reversal of this discrimination (R2). The sixth task required an ED cognitive set-shift, in which all new stimuli were again introduced, but this time the relevant dimension was also changed, that is, digging medium became the relevant dimension and odor was irrelevant. The dependent measure was the number of trials required to reach criterion of six consecutive correct responses on each task (Trials to Criterion, TTC).
Experiment 1: Effects of CUS on Acute Stress-Evoked NE Release in the mPFC
Sixteen rats were divided into CUS or control groups. They were anesthetized (ketamine 43 mg/ml, acepromazine 1.4 mg/ml, xylazine 8.6 mg/ml, 1.0 ml/kg i.m., 25% supplement as needed), and a microdialysis guide cannula (CMA Microdialysis, North Chelmsford, MA, USA) was implanted unilaterally, terminating 2 mm above the infralimbic/prelimbic boundary in the mPFC (coordinates relative to bregma, with a 10° lateral angle: AP +2.6 mm, ML±1.4 mm, DV −1.7 mm; Paxinos and Watson, 1998). The cannula was anchored to the skull using jeweler screws and dental acrylic. Rats were treated prophylactically with antibiotic (penicillin G, 300 000 IU/ml, 1.0 ml/kg, s.c.), hydrated, and singularly housed in fresh cages. Experimental procedures commenced 1-week post-surgery.
All rats were habituated to the microdialysis room and buckets (60 cm height × 30 cm diameter) for 10 min/day after CUS or handling sessions on days 12–14. Microdialysis was conducted 1 day after CUS (day 15). A microdialysis probe (CMA/12) with 20 kDa MW cutoff was inserted, extending 4 mm beyond the tip of the guide, centering the active membrane in the mPFC. Artificial cerebral spinal fluid (147 mM NaCl, 2.5 mM KCl, 1.3 mM CaCl2, 0.9 mM MgCl2, pH 7.4) was perfused though the probe at 1.0 μl/min. After 2 h equilibration, four baseline samples were collected at 30 min intervals into tubes containing 2.5 μl of 0.2 μM EDTA. The fifth sample was collected during acute immobilization stress, a novel stimulus that was not applied during CUS. The rats were held prone on a plastic rack large enough to support their body (26 × 13 cm2), and their head, limbs, and torso were taped gently but securely to the rack. After 30 min, the rat was returned to the bucket for four 30-min recovery samples. NE in the dialysate was quantified by HPLC with coulometric detection (Coulochem II, ESA, East Chelmsford, MA, USA). Mobile phase contained 60 mM sodium phosphate, 75 μM EDTA, 1.5 mM sodium 1-octanesulfonic acid, 6% methanol, pH 4.6, at a flow rate of 0.6 ml/min. NE was measured against a calibration curve established daily. Detection limit was 0.5 pg/sample.
Experiment 2: Effect of Blocking Adrenergic Receptors in the mPFC During Each Stress Treatment on the CUS-Induced Cognitive Set-Shifting Deficit on the AST
Forty-three rats were assigned to four groups defined by chronic stress (CUS or control), and drug treatments (vehicle or antagonists). Six additional rats were used as shams to determine if repeated bilateral microinjections alone altered performance on the AST. All rats were implanted with bilateral 23 ga stainless steel guide cannulae terminating 1 mm above the mPFC (10° approach; coordinates relative to bregma: AP +2.6 mm, ML±1.4 mm, DV −2.7 mm; Paxinos and Watson, 1998). CUS and non-stress control treatments were as above. Prior to each stress or handling session, rats were gently restrained in a towel while the obdurators were removed and replaced with 30 ga stainless steel microinjectors. Animals were returned to their home cage to receive a microinjection (0.5 μl/side at 0.25 μl/min) of 0.6% saline vehicle, or a cocktail containing the α1-adrenergic receptor antagonist, benoxathian (2 nmol/0.5 μl, Sigma), the β1-receptor antagonist, betaxolol (1 nmol/0.5 μl, Tocris), and the β2-antagonist, ICI 118,551 (1 nmol/0.5 μl, Tocris). In previous studies, these doses were shown to be effective in blocking acute noradrenergic modulation of specific behavioral responses in the hypothalamus, extended amygdala, and mPFC (Cecchi et al, 2002a, 2002b; Lapiz and Morilak, 2006). Microinjectors were left in place for 2 min to allow for diffusion, then removed and the obdurators replaced. Uninjected shams were handled similarly, without inserting microinjectors. For CUS rats, stress sessions commenced 5 min after removing the injectors, while control rats and shams were returned to housing. Thus, all rats (excluding shams) received 14 microinjections in the mPFC over 2 weeks. AST testing was conducted 3 days after the last stress/drug session. The experimenter was blind to drug conditions.
Experiment 3: Control Experiment to Test if Repeated Antagonist Treatment During CUS May Have Masked the Cognitive Deficit by Sensitizing Adrenergic Receptors in mPFC
The hypothesis tested in experiment 2 was that chronic adrenergic antagonist treatment prevented CUS-induced ED deficits by protecting the mPFC from the detrimental effects of repeated NE-mediated facilitation. We have shown previously that under basal conditions, blocking NE receptors in the mPFC during testing had no effect on cognitive set-shifting, whereas acutely elevating NE transmission facilitated set-shifting by activating α1-adrenergic receptors (Lapiz and Morilak, 2006). Therefore, an alternative explanation must be considered, that repeated antagonist treatment could have sensitized adrenergic receptor function in mPFC, essentially mimicking the effects of elevated NE transmission. Thus, experiment 3 tested whether the seemingly protective effects of adrenergic antagonist treatment during CUS were instead attributable to sensitization of basal adrenergic receptor function.
Eighty-seven rats were divided by stress (CUS or control) and repeated microinjection treatment (vehicle or antagonists). On the testing day, after completing the R2 stage, rats were removed from the testing arena and administered an additional acute vehicle or adrenergic antagonist injection into the mPFC as above. The experimenter was blind to both chronic and acute drug treatments. Behavioral testing resumed with the ED stage 5 min after injection.
Statistical Analysis
Cannulae placement was determined by histology. Animals with cannulae outside the mPFC, or that did not complete the behavioral procedures were removed from analysis a priori. In experiment 1, baseline NE levels in control and CUS-treated rats were compared by Student's t-test. Two-way multivariate analysis of variance (MANOVA) with repeated measures was used to analyze the effect of acute immobilization stress. In experiment 2, we first confirmed that repeated daily microinjections did not alter behavior by comparing non-injected shams to vehicle-controls. Effects of CUS and antagonist administration on ED set-shifting were then analyzed by two-way MANOVA. Secondarily, potential effects on the other tasks (SD-R2) leading up to the ED stage were similarly analyzed by two-way MANOVA. In experiment 3, ED performance was analyzed by three-way MANOVA (Stress × Chronic Drug × Acute Drug). Because acute drug administration occurred after the test stages preceding ED, performance on these tasks was analyzed as in experiment 2, by two-way MANOVA. Where significant main effects or interactions were detected, post hoc comparisons were made using the Newman–Keuls test. Significance was determined at p<0.05.
RESULTS
Experiment 1: Effects of CUS on Acute Stress-Evoked NE Release in the mPFC
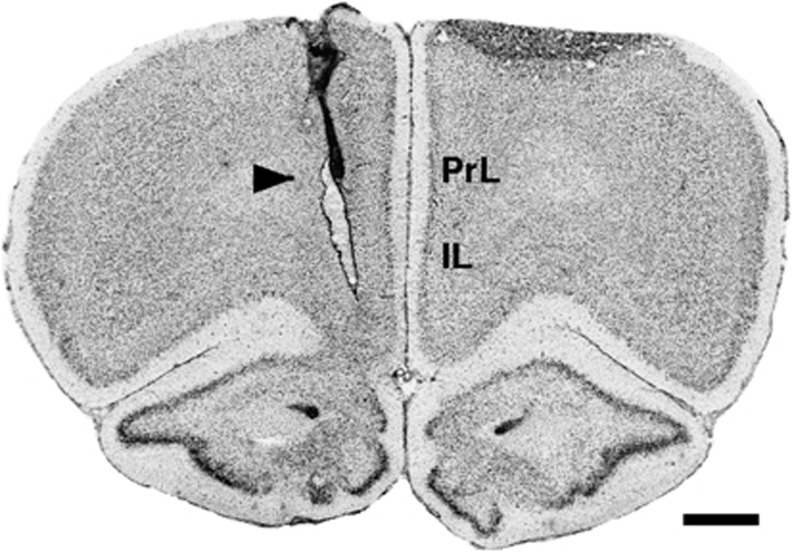
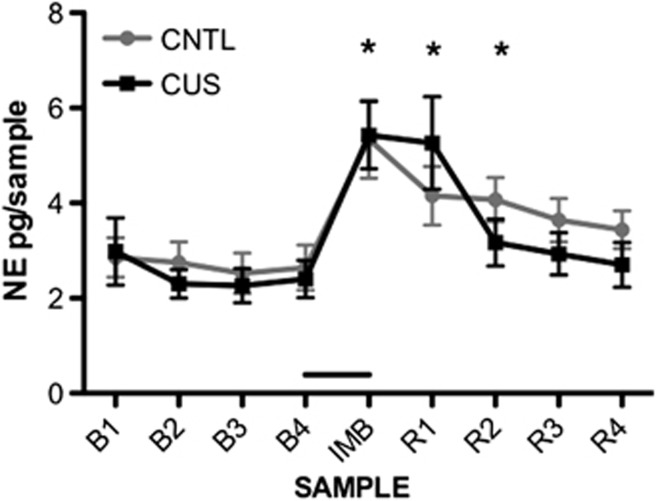
Figure 1 shows an example of a microdialysis probe track located in the mPFC. Figure 2 shows extracellular NE levels collected from the mPFC before, during, and after acute immobilization stress. There were no differences in mean baseline NE levels in control and CUS-treated rats (Control: 2.69±0.42 pg/sample; CUS: 2.49±0.40 pg/sample; t13=0.352, p=0.73, n=7–8/group), and acute immobilization induced a similar increase in NE in the mPFC of CUS and control rats (Control: 5.34±0.82 pg/sample; CUS: 5.43±0.71 pg/sample). Two-way MANOVA revealed a significant main effect of Sample (F8,104=20.05, p<0.001), with NE levels significantly elevated in the samples collected during and immediately after immobilization stress (p<0.05). There was no effect of CUS (F1,13=0.11, p=0.74), nor a CUS × Sample interaction (F8,104=1.75, p=0.095). One animal was eliminated due to misplaced probe.
Figure 1.
A representative photomicrograph of a coronal section through the mPFC stained with Cresyl Violet, showing a unilateral microdialysis cannula track terminating 2 mm above the mPFC. A microdialysis probe extended 4 mm beyond the cannula tip, centering the active membrane in the mPFC (arrowhead). IL, infralimbic cortex; PrL, prelimbic cortex. Scale bar=1 mm.
Figure 2.
Effects of CUS on NE levels in microdialysate samples collected from the mPFC. There were no baseline differences (samples B1–B4) between control and CUS rats before 30 min of acute immobilization stress. Acute immobilization stress (bar) significantly elevated NE levels in the immobilization sample (IMB), and in the first two recovery samples (R1–R2). The acute stress-induced increase in NE levels in mPFC was comparable in CUS-treated rats and controls (main effect of sample, p<0.001; post hoc comparisons: *p<0.05 compared with baseline samples). Data are expressed as pg/sample (mean±SEM; n=7–8/group).
Experiment 2: Effect of Blocking Adrenergic Receptors in the mPFC During Each Stress Treatment on the CUS-Induced Cognitive Set-Shifting Deficit on the AST
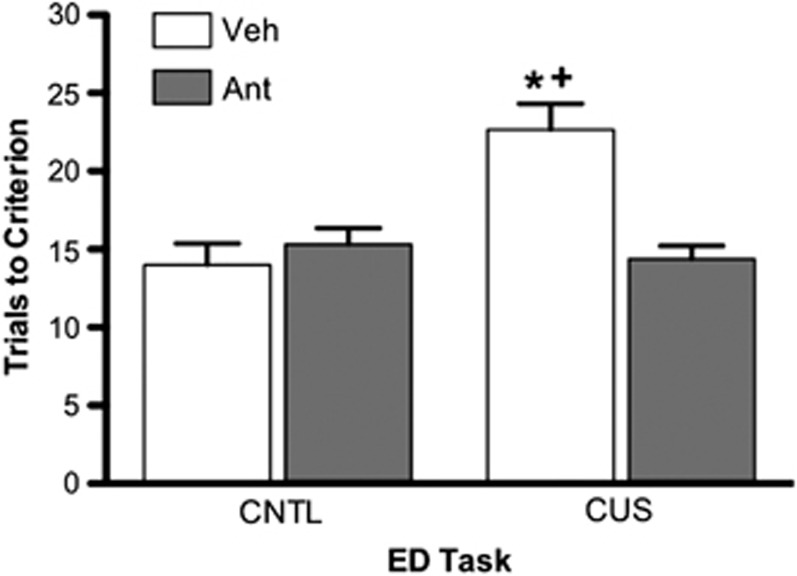
Figure 3 shows the localization of bilateral cannulae tracks in the mPFC. The microinjection procedure alone did not affect behavior on the AST, as there were no differences in TTC between sham-implanted and vehicle-injected controls. Further, the CUS and Drug treatment groups did not differ on the training discrimination the day before testing (p>0.05), indicating that there were no pre-existing differences between treatment groups on their ability to learn the contingencies or perform the required tasks prior to testing.
Figure 3.
A representative photomicrograph of a coronal section through the mPFC stained with Cresyl Violet, showing bilateral guide cannulae tracks terminating 1 mm above the mPFC. Microinjectors extended 1 mm beyond the cannulae, centering the tips in the mPFC (arrowheads). IL, infralimbic cortex; PrL, prelimbic cortex. Scale bar=1 mm.
In the analysis of CUS and repeated drug treatment effects on ED set-shifting, two-way MANOVA revealed significant main effects of Stress (F1,33=9.76, p<0.01), Drug treatment (F1,33=7.85, p<0.01), and a Stress × Drug interaction (F1,33=15.05, p<0.001). Figure 4 shows the TTC for all groups on the ED set-shifting task. Replicating the effects of CUS previously demonstrated (Bondi et al, 2008, 2010), CUS rats treated with vehicle microinjections into mPFC before each stress session had significantly higher TTC than the non-stressed vehicle-injected controls (p<0.001). However, treating rats with adrenergic receptor antagonists prior to each stress session prevented the CUS-induced deficit in cognitive set-shifting, as TTC were significantly lower than in vehicle-treated CUS rats (p<0.001) and were comparable to non-stressed vehicle-controls. Repeated antagonist treatment alone, in the absence of CUS, had no effect on subsequent set-shifting performance (p>0.05). Analysis of the SD-R2 stages preceding the ED set-shifting task revealed the expected effect of Task (F4,132=36.54, p<0.001), but not for Stress (F1,33=2.75, p>0.1), Chronic Drug (F1,33=0.724, p>0.4) nor an interaction (F4,132=1.46, p>0.21). No animals were excluded from analysis.
Figure 4.
Protective effects of noradrenergic receptor blockade in mPFC during CUS on ED set-shifting. A cocktail of the α1-adrenergic receptor antagonist, benoxathian, the β1-adrenergic antagonist, betaxolol, and the β2-adrenergic antagonist, ICI 118,551 was microinjected bilaterally into the mPFC prior to each CUS stress session. CUS rats given vehicle microinjections (Veh) expressed a significant ED set-shifting deficit compared with unstressed controls (*p<0.001) and compared to CUS rats treated with the antagonists (Ant; +p<0.001). All data are expressed as mean±SEM, n=9–10/group.
Experiment 3: Control Experiment to Test if Repeated Antagonist Treatment During CUS May Have Masked the Cognitive Deficit by Sensitizing Adrenergic Receptors in mPFC
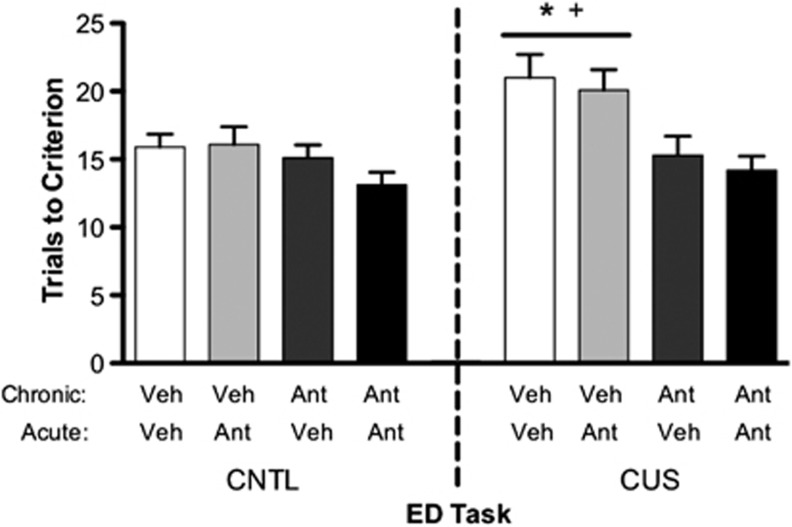
There were no pre-existing differences in TTC on the training day discrimination (p>0.05). Figure 5 shows the TTC for all groups on the ED set-shifting task. A three-way MANOVA revealed significant main effects of Stress (F1,71=8.37, p<0.01), Chronic Drug (F1,71=18.34, p<0.001), and a Stress × Chronic Drug interaction (F1,71=4.76, p<0.04). However, there was no effect of Acute Drug treatment immediately prior to ED (F1,71=1.13, p=0.29). As in experiment 2, post hoc analysis indicated that CUS rats chronically treated with vehicle had significantly higher TTC compared with unstressed controls (p<0.05). Further, repeated administration of adrenergic receptor antagonists again prevented the detrimental effects of CUS, reducing TTC compared with vehicle-treated CUS rats (p<0.05), to a level comparable to unstressed vehicle-controls. Most importantly, acute adrenergic receptor blockade in mPFC immediately prior to ED did not hinder performance in CUS rats treated with chronic antagonists during CUS. If repeated antagonist treatment during CUS had sensitized adrenergic receptors in mPFC, inducing facilitation under basal conditions, then acute antagonist treatment prior to ED testing would have been expected to compromise ED performance and increase TTC. Thus, these data do not support the alternate interpretation that receptor sensitization may have masked a CUS-induced deficit. Three animals were excluded from analysis in experiment 3 due to cannula misplacement, one failed to complete training (unstressed/chronic drug) and four dropped out during testing (three from the CUS/vehicle group, one from the unstressed/chronic drug group).
Figure 5.
Effects of noradrenergic receptor blockade in mPFC during CUS, followed by an acute microinjection into the mPFC immediately prior to testing on the ED task. Acute antagonist (Ant) administration immediately prior to the ED task had no effect in any condition. As in Figure 4, after collapsing across acute drug treatment, CUS induced a significant ED set-shifting deficit (CUS+chronic vehicle compared with controls: *p<0.001) that was prevented by chronic Ant treatment (CUS+chronic antagonists compared with CUS+chronic vehicle: +p<0.001). All data are expressed as mean±SEM, n=9–11/group.
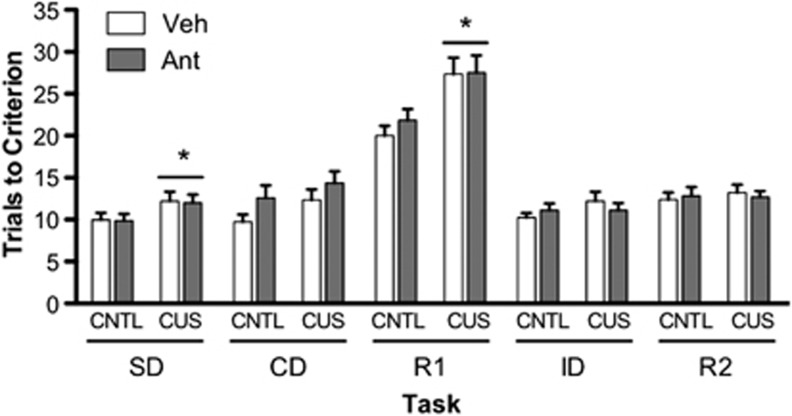
Behavioral Specificity of Repeated Adrenergic Antagonist Treatment in mPFC During CUS
In both experiments 2 and 3, there was no effect of chronic drug treatment on any task preceding ED set-shifting (SD-R2, p>0.05 for all analyses). Further, there were no main effects of CUS, nor CUS × Chronic Drug interactions for any task except the first reversal (R1). On the R1 reversal task, in agreement with previous reports (Bondi et al, 2008, 2010), there was a significant effect of CUS in both experiment 2 (F1,33=4.1366, p<0.05) and experiment 3 (F1,75=14.54, p<0.001). However, as expected, and by contrast with ED, the CUS-induced deficit in reversal learning was not prevented by chronic adrenergic antagonist treatment in the mPFC during CUS (in experiment 2, Chronic Drug: F1,33=0.2704, p>0.60; CUS × Chronic Drug interaction: F1,33=1.4193, p>0.24; in experiment 3, Chronic Drug: F1,75=0.087, p>0.79; interaction: F1,75=0.606, p>0.44; see Figure 6), confirming the behavioral specificity of the drug treatment in mPFC.
Figure 6.
Behavioral specificity of adrenergic antagonist treatment in the mPFC during CUS. Performance on each task of the AST preceding the ED set-shifting task is shown in experiment 3. In this experiment, as in experiment 2 (not shown), CUS induced a deficit on the R1 reversal learning task (*p<0.001), which was not prevented by chronic adrenergic antagonist treatment in the mPFC during CUS (p>0.43). Note that in experiment 3, but not experiment 2 (nor in previous studies), CUS had a very modest effect on the SD task (*p<0.03), which also was not affected by chronic adrenergic antagonist treatment in the mPFC (p>0.98). The lack of effect on other components of the AST confirms the behavioral specificity of drug treatment in the mPFC on ED set-shifting. All data are expressed as mean±SEM, n=18–21/group.
In experiment 3, but not experiment 2, there was also a very modest effect of CUS on the SD task, from 9.9±0.6 to 12.0±0.7 TTC (F1,75=5.46, p<0.05, see Figure 6), but no effect of Chronic Drug (F1,75=0.008, p=0.93) nor an interaction (F1,75=0.0004, p=0.98). While it is not unusual for CUS to have occasional effects on a task other than ED or R1, this is not a consistent finding. Moreover, the mild effect on the SD task did not impact performance on the subsequent CD task, and it was not affected by chronic drug treatment in the mPFC.
DISCUSSION
Our laboratory and others have demonstrated that NE facilitates ED set-shifting in the mPFC (Lapiz and Morilak, 2006; Tait et al, 2007; Bondi et al, 2008; McGaughy et al, 2008). Further, we showed recently that increasing noradrenergic transmission acutely in the mPFC continued to facilitate cognitive set-shifting that had been compromised by chronic stress exposure (Bondi et al, 2010). In the current study, acute stress-evoked NE release in the mPFC after 2 weeks of CUS exposure was comparable to that in unstressed control rats. This implies that each acute stressor administered over the course of CUS treatment elicited an effective NE response in the mPFC, a necessary pre-requisite for the hypothesis that repeated activation of acute NE facilitation might contribute to the CUS-induced ED deficit. Subsequently, we showed that adrenergic receptor blockade in the mPFC prior to each stress session prevented the CUS-induced ED deficit. The beneficial effect of antagonist treatment was not attributable to masking of the CUS-induced deficit by noradrenergic receptor super-sensitivity. Moreover, the CUS-induced deficit in reversal learning was unaffected by antagonist treatment in mPFC. Because ED set-shifting is dependent on the functional integrity of the mPFC (Birrell and Brown, 2000), whereas reversal learning is dependent on the orbitofrontal cortex (McAlonan and Brown, 2003), the lack of drug effect on reversal learning confirmed the behavioral and anatomical specificity of antagonist treatment in the mPFC.
High levels of tonic noradrenergic activity have been associated with ‘scanning attention' and vigilance (Aston-Jones et al, 1999, 2000). Under these conditions, animals are more broadly receptive to environmental stimuli, as opposed to being focused on an established or expected contingency (Sara et al, 1994; Aston-Jones et al, 1999). Thus, elevated NE tone appears to enhance cognitive flexibility by allowing the organism to disengage pre-eminent responses, and to re-direct behavior to new or alternative strategies that may be required by the demands of a changing or challenging environment. We have shown previously that activation of α1-adrenergic receptors in many brain regions facilitates a range of behavioral and physiological responses to acute stress, including shock probe defensive burying, reductions in open-arm exploration on the elevated plus maze, and activation of the hypothalamic–pituitary–adrenal (HPA) axis (Cecchi et al, 2002b; Pardon et al, 2003; Ma and Morilak, 2005a, 2005b; Morilak et al, 2005; Bondi et al, 2007). In addition, we found that α1-adrenergic receptor activation enhances cognitive flexibility in the mPFC (Lapiz and Morilak, 2006; Bondi et al, 2010). The α1-adrenergic receptor enhances cortical excitatory signaling and acute stress-evoked glutamate release (Marek and Aghajanian, 1999; Lupinsky et al, 2010), thereby facilitating the signal-to-noise ratio of evoked synaptic transmission and sharpening cellular responses in cortex (Waterhouse et al, 1981, 2000). Thus, elevated NE levels may facilitate cognitive flexibility and behavioral adaptation by increasing glutamate neurotransmission in the mPFC circuitry. However, these acutely adaptive effects of NE may come at a cost when elicited repeatedly by chronic stress, as excessive glutamate signaling can also induce excitotoxicity, leading to cellular damage or even cell loss (Bruno et al, 1993; Skaper et al, 2001). In other studies, repeated stress-induced cognitive impairments have been attributed to glutamate-mediated pyramidal cell dendritic atrophy in the mPFC and hippocampus (Woolley et al, 1990; Liston et al, 2006; Martin and Wellman, 2011). The α1-adrenergic receptor is expressed on mPFC pyramidal cells, in which stress-induced dendritic remodeling has been noted (Marek and Aghajanian, 1999; Wellman, 2001; Radley et al, 2004; Lupinsky et al, 2010). Thus, CUS-induced deficits in cognitive flexibility may be the result of repeated induction of noradrenergic facilitation in mPFC, leading to excessive glutamate transmission and pyramidal cell dysfunction.
In our previous studies, blocking β-adrenergic receptors in mPFC did not affect acute noradrenergic modulation of cognitive set-shifting (Lapiz and Morilak, 2006). Nonetheless, β-receptors have been shown to facilitate glutamate signaling in the mPFC, and to enhance signal-to-noise ratio of evoked synaptic responses in many brain regions (Woodward et al, 1991; Ji et al, 2008). In addition, chronic stress downregulates β-adrenergic receptor binding in the cortex (Nomura et al, 1981). Although our previous results suggest that cortical α1-receptors are most likely responsible for the effects observed in the present study, it is possible that chronic stress could recruit receptor mechanisms that were not involved in acute modulatory processes. Thus, to minimize excessive animal use and resource expenditure, while optimizing the likelihood of revealing an effect of noradrenergic modulation during chronic stress, we elected to administer a cocktail of α1, β1-, and β2-adrenergic receptor antagonists during CUS rather than test each subtype-specific antagonist separately. Having now demonstrated an important role for NE in CUS-induced cognitive dysfunction, future investigations will determine the specific adrenergic receptor involved in this effect.
In the context of stress, the HPA axis is activated together with the brain noradrenergic system (Joels and Baram, 2009; Joels et al, 2011). Consequently, elevated noradrenergic signaling would have converged with stress-evoked glucocorticoid signaling over the course of CUS. Glucocorticoids have also been shown to have facilitatory as well as potentially damaging effects in the brain, and to interact with NE specifically in the context of stress-induced plasticity (McGaugh and Roozendaal, 2002; Roozendaal et al, 2008; Krugers et al, 2012). Administration of glucocorticoid receptor antagonists during chronic stress or during prolonged corticosterone treatment has been shown to prevent dendritic atrophy in the mPFC and hippocampus (Magarinos and McEwen, 1995; Wellman, 2001; Liu and Aghajanian, 2008; Popoli et al, 2012). Therefore, corticosterone may contribute to chronic stress-induced cognitive impairments associated with these regions (Musazzi et al, 2011; Popoli et al, 2012). NE and glucocorticoids converge to facilitate glutamate signaling in the hippocampus and basolateral amygdala during consolidation of memory for fear conditioning (McGaugh and Roozendaal, 2002; Roozendaal et al, 2008; Krugers et al, 2012). Thus, corticosterone and NE may likewise act synergistically during chronic stress to compromise the functional integrity of the mPFC. In other studies, neither α1-adrenergic receptor antagonist administration nor removal of the adrenal glands alone completely blocked acute stress-evoked glutamate release in the mPFC (Moghaddam et al, 1994; Lupinsky et al, 2010). This suggests that individually inhibiting the modulatory actions of either NE or corticosterone during chronic stress may reduce stress-evoked glutamate release to a level that maintains function, but is no longer so excessive as to compromise the integrity of the mPFC. The present results are consistent with this, as noradrenergic receptor blockade in mPFC during CUS, presumably in the presence of stress-evoked corticosterone activity, protected cognitive function.
The NE and HPA systems in the brain may also interact indirectly to influence cognition in the mPFC. Although the prelimbic region of the mPFC does not innervate the paraventricular nucleus of the hypothalamus (PVN) directly, there is evidence that attenuating stress-evoked NE release in the mPFC can reduce acute activation of the PVN (Radley et al, 2008). Thus, adrenergic receptor blockade in the mPFC may decrease the repeated stress-induced activation of the HPA axis, thereby reducing circulating levels of corticosterone during CUS and protecting the mPFC indirectly. This hypothesis remains to be tested.
Recent studies from our laboratory have demonstrated that chronic administration of the selective NE reuptake inhibitor, desipramine (DMI), during CUS prevented the stress-induced impairment of cognitive set-shifting (Bondi et al, 2008, 2010). These results may at first seem contradictory to the current finding that repeated activation of noradrenergic transmission in the mPFC during CUS compromised cognitive set-shifting. As discussed above, elevating NE may enhance ED performance by facilitating glutamate signaling in the mPFC. Depression has been associated with hypoactivity, reduced glutamate levels, and decreased NMDA receptor expression in the mPFC (Hasler et al, 2007; Feyissa et al, 2009; Merkl et al, 2011). Chronic stress has been shown to impair limbic-prefrontal cortical function by downregulating NMDA receptor expression in the mPFC of rats (Lee and Goto, 2011). By contrast, chronic DMI administration has been shown to attenuate acute stress-induced enhancement of glutamate release (Musazzi et al, 2011), thereby ‘dampening' potentially excessive excitation. Chronic DMI treatment tonically elevates extracellular NE, effectively uncoupling NE transmission from phasic activity in the presynaptic NE neuron. DMI also can dampen the stress-evoked activation of the noradrenergic system through the persistent inhibitory influence of α2-adrenergic autoreceptors, which remain functional after chronic DMI treatment (Lapiz et al, 2007). Therefore, with chronic reuptake blockade, the modulatory effects of NE are exerted tonically, and are dissociated from the phasic convergence with other stress-activated modulatory influences, such as glucocorticoids, that may otherwise lead to excessive facilitation of glutamate signaling, possible neurotoxicity, and functional dysregulation in mPFC. Thus, chronic NE reuptake blockade may restore glutamate signaling and enhance mPFC-mediated cognitive function sufficiently to overcome the CUS-induced deficit (Bondi et al, 2010), while limiting the degree of facilitation to a level that does not induce further damage.
Aston-Jones et al (2000) described an inverted U-shaped relationship between noradrenergic activity and cognitive performance on a focused attention task. However, they were describing electrical activity of noradrenergic neurons on a msec time frame, relating a low tonic but highly reactive pattern of activity (ie, high signal-to-noise ratio) to high performance on a signal detection task, in which a burst of activity in noradrenergic neurons would enhance the salience of a target stimulus relative to background or distracting stimuli. By contrast, a pattern of high tonic activity but less phasic reactivity would be more conducive to ‘scanning' attention, in which unexpected environmental stimuli would be more detectable. However, this inverted-U is unlikely to pertain in the present study. The multiple acute stressors comprising the CUS procedure induce elevated noradrenergic activity that is phasic in the sense that it is time-locked to a temporally distinct stressful stimulus, and thus convergent with other stress-evoked processes (eg, glucocorticoid secretion, glutamate activation, cytokine induction, etc). But that is on a minutes-to-hours time frame. On the msec time frame considered by Aston-Jones et al, the electrical activity of noradrenergic neurons elicited during acute stress is most likely ‘tonic' (Jacobs et al, 1991). This is consistent with the observation that acute elevation of NE enhances cognitive flexibility on the AST (Lapiz and Morilak, 2006), as these tasks require that new cues from the environment disengage the previously learned contingency to allow plasticity, thus resembling a state of ‘scanning' rather than focused attention. The present data suggest that the cumulative effect of repeatedly activating this acutely facilitatory noradrenergic process in the mPFC, perhaps in concert with other convergent processes evoked by acute stress, ultimately contributes to the detrimental consequences of chronic stress on cognitive capability in the mPFC.
The observation in the present study that blockade of adrenergic receptors in mPFC is protective against the detrimental consequences of chronic stress may be relevant to recent reports of the potentially beneficial effects of the α1-adrenergic receptor antagonist, prazosin, in the treatment of trauma-related nightmares and sleep disturbance in post-traumatic stress disorder (PTSD) (Raskind et al, 2007). In our animal experiments, drug was administered during the application of chronic stress, which was then terminated prior to testing. However, in patients suffering from PTSD, even after the traumatic event or situation has passed, the cognitive process of re-experiencing the trauma may in itself become a secondary chronic stressor that maintains a dysregulatory state. Thus, blocking noradrenergic facilitation may likewise ‘protect' the mPFC during the ongoing stress of PTSD, restoring prefrontal cognitive function to a point where behavioral interventions, such as cognitive-behavioral therapy, may become effective (Gehrman and Harb, 2010). Similar treatment strategies may be effective in reducing the risk of relapse of depression or anxiety disorders when faced with subsequent life stress (Kendler et al, 1998, 1999).
It is increasingly recognized that cognitive dysfunction underlies many of the affective symptoms associated with stress-related neuropsychiatric illnesses, such as depression, PTSD, and other anxiety disorders (Beck et al, 1987; Beck, 2005). Noradrenergic signaling in the mPFC is important for the cognitive changes that accompany arousal and attention (Aston-Jones et al, 2000), and NE modulates executive processes that are essential to effectively adapt to the demands of a changing or challenging environment (Lapiz and Morilak, 2006; Bondi et al, 2010). With such modulatory systems, either too much or too little can be detrimental, and the ‘optimal level' of modulation constantly changes relative to changes in both the context and activity in the circuits being modulated. Understanding this dynamic balance, and the mechanisms through which it can be dysregulated by factors such as chronic stress, may inform the development of more effective strategies for the treatment or prevention of stress-related psychiatric disorders.
Acknowledgments
We thank Ms Ashley Wallace and Ms Kale Naegeli for excellent technical assistance. These studies were supported by research Grant MH053851 from the National Institute of Mental Health.
JJ has no scientific or financial conflicts of interest to disclose. Within the past 3 years, DM has received research funding from Lundbeck and Forest Laboratories, and received honoraria from Dey Pharmaceuticals (now Mylan) and Forest.
References
- Anisman H, Zacharko RM. Multiple neurochemical and behavioral consequences of stressors: implications for depression. Pharmacol Ther. 1990;46:119–136. doi: 10.1016/0163-7258(90)90039-5. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Chiang C, Alexinsky T. Discharge of noradrenergic locus coeruleus neurons in behaving rats and monkeys suggests a role in vigilance. Prog Brain Res. 1991;88:501–520. doi: 10.1016/s0079-6123(08)63830-3. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Rajkowski J, Cohen J. Role of locus coeruleus in attention and behavioral flexibility. Biol Psychiatry. 1999;46:1309–1320. doi: 10.1016/s0006-3223(99)00140-7. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Rajkowski J, Cohen J. Locus coeruleus and regulation of behavioral flexibility and attention. Prog Brain Res. 2000;126:165–182. doi: 10.1016/S0079-6123(00)26013-5. [DOI] [PubMed] [Google Scholar]
- Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200–206. doi: 10.1192/bjp.178.3.200. [DOI] [PubMed] [Google Scholar]
- Bagley J, Moghaddam B. Temporal dynamics of glutamate efflux in the prefrontal cortex and in the hippocampus following repeated stress: effects of pretreatment with saline or diazepam. Neuroscience. 1997;77:65–73. doi: 10.1016/s0306-4522(96)00435-6. [DOI] [PubMed] [Google Scholar]
- Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch Gen Psychiatry. 2005;62:953–959. doi: 10.1001/archpsyc.62.9.953. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Steer RA, Eidelson JI, Riskind JH. Differentiating anxiety and depression: a test of the cognitive content-specificity hypothesis. J Abnorm Psychol. 1987;96:179–183. doi: 10.1037//0021-843x.96.3.179. [DOI] [PubMed] [Google Scholar]
- Berridge CW, Page ME, Valentino RJ, Foote SL. Effects of locus coeruleus inactivation on electroencephalographic activity in neocortex and hippocampus. Neuroscience. 1993;55:381–393. doi: 10.1016/0306-4522(93)90507-c. [DOI] [PubMed] [Google Scholar]
- Berridge CW, Waterhouse BD. The locus coeruleus-noradrenergic system: modulation of behavioral state and state-dependent cognitive processes. Brain Res Brain Res Rev. 2003;42:33–84. doi: 10.1016/s0165-0173(03)00143-7. [DOI] [PubMed] [Google Scholar]
- Birrell JM, Brown VJ. Medial frontal cortex mediates perceptual attentional set shifting in the rat. J Neurosci. 2000;20:4320–4324. doi: 10.1523/JNEUROSCI.20-11-04320.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bondi CO, Barrera G, Lapiz MD, Bedard T, Mahan A, Morilak DA. Noradrenergic facilitation of shock-probe defensive burying in lateral septum of rats, and modulation by chronic treatment with desipramine. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:482–495. doi: 10.1016/j.pnpbp.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Bondi CO, Jett JD, Morilak DA. Beneficial effects of desipramine on cognitive function of chronically stressed rats are mediated by alpha1-adrenergic receptors in medial prefrontal cortex. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:913–923. doi: 10.1016/j.pnpbp.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bondi CO, Rodriguez G, Gould GG, Frazer A, Morilak DA. Chronic unpredictable stress induces a cognitive deficit and anxiety-like behavior in rats that is prevented by chronic antidepressant drug treatment. Neuropsychopharmacology. 2008;33:320–331. doi: 10.1038/sj.npp.1301410. [DOI] [PubMed] [Google Scholar]
- Bruno V, Scapagnini U, Canonico PL. Excitatory amino acids and neurotoxicity. Funct Neurol. 1993;8:279–292. [PubMed] [Google Scholar]
- Cecchi M, Khoshbouei H, Javors M, Morilak DA. Modulatory effects of norepinephrine in the lateral bed nucleus of the stria terminalis on behavioral and neuroendocrine responses to acute stress. Neuroscience. 2002a;112:13–21. doi: 10.1016/s0306-4522(02)00062-3. [DOI] [PubMed] [Google Scholar]
- Cecchi M, Khoshbouei H, Morilak DA. Modulatory effects of norepinephrine, acting on alpha 1 receptors in the central nucleus of the amygdala, on behavioral and neuroendocrine responses to acute immobilization stress. Neuropharmacology. 2002b;43:1139–1147. doi: 10.1016/s0028-3908(02)00292-7. [DOI] [PubMed] [Google Scholar]
- Channon S. Executive dysfunction in depression: the Wisconsin Card Sorting Test. J Affect Disord. 1996;39:107–114. doi: 10.1016/0165-0327(96)00027-4. [DOI] [PubMed] [Google Scholar]
- Cole BJ, Robbins TW. Forebrain norepinephrine: role in controlled information processing in the rat. Neuropsychopharmacology. 1992;7:129–142. [PubMed] [Google Scholar]
- Cook SC, Wellman CL. Chronic stress alters dendritic morphology in rat medial prefrontal cortex. J Neurobiol. 2004;60:236–248. doi: 10.1002/neu.20025. [DOI] [PubMed] [Google Scholar]
- de Kloet ER, Joels M, Holsboer F. Stress and the brain: from adaptation to disease. Nat Rev Neurosci. 2005;6:463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- Disner SG, Beevers CG, Haigh EA, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. 2011;12:467–477. doi: 10.1038/nrn3027. [DOI] [PubMed] [Google Scholar]
- Fales CL, Barch DM, Rundle MM, Mintun MA, Mathews J, Snyder AZ, et al. Antidepressant treatment normalizes hypoactivity in dorsolateral prefrontal cortex during emotional interference processing in major depression. J Affect Disord. 2009;112:206–211. doi: 10.1016/j.jad.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feyissa AM, Chandran A, Stockmeier CA, Karolewicz B. Reduced levels of NR2A and NR2B subunits of NMDA receptor and PSD-95 in the prefrontal cortex in major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:70–75. doi: 10.1016/j.pnpbp.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehrman PR, Harb GC. Treatment of nightmares in the context of posttraumatic stress disorder. J Clin Psychol. 2010;66:1185–1194. doi: 10.1002/jclp.20730. [DOI] [PubMed] [Google Scholar]
- Glavin GB. Stress and brain noradrenaline: a review. Neurosci Biobehav Rev. 1985;9:233–243. doi: 10.1016/0149-7634(85)90048-x. [DOI] [PubMed] [Google Scholar]
- Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64:193–200. doi: 10.1001/archpsyc.64.2.193. [DOI] [PubMed] [Google Scholar]
- Jacobs BL, Abercrombie ED, Fornal CA, Levine ES, Morilak DA, Stafford IL. Single-unit and physiological analyses of brain norepinephrine function in behaving animals. Prog Brain Res. 1991;88:159–165. doi: 10.1016/s0079-6123(08)63805-4. [DOI] [PubMed] [Google Scholar]
- Jett JD, Bédard T, Rodriguez G, Morilak DA. Blockade of adrenergic receptors during chronic unpredictable stress prevents the detrimental effects on cognitive flexibility in rats. Soc Neurosci Abstr 34, Online: Program number. 2008;195:8. [Google Scholar]
- Ji XH, Cao XH, Zhang CL, Feng ZJ, Zhang XH, Ma L, et al. Pre- and postsynaptic beta-adrenergic activation enhances excitatory synaptic transmission in layer V/VI pyramidal neurons of the medial prefrontal cortex of rats. Cereb Cortex. 2008;18:1506–1520. doi: 10.1093/cercor/bhm177. [DOI] [PubMed] [Google Scholar]
- Joels M, Baram TZ. The neuro-symphony of stress. Nat Rev Neurosci. 2009;10:459–466. doi: 10.1038/nrn2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joels M, Fernandez G, Roozendaal B. Stress and emotional memory: a matter of timing. Trends Cogn Sci. 2011;15:280–288. doi: 10.1016/j.tics.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Joels M, Pu Z, Wiegert O, Oitzl MS, Krugers HJ. Learning under stress: how does it work. Trends Cogn Sci. 2006;10:152–158. doi: 10.1016/j.tics.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Stressful life events and major depression: risk period, long-term contextual threat, and diagnostic specificity. J Nerv Ment Dis. 1998;186:661–669. doi: 10.1097/00005053-199811000-00001. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Krugers HJ, Karst H, Joels M. Interactions between noradrenaline and corticosteroids in the brain: from electrical activity to cognitive performance. Front Cell Neurosci. 2012;6:15. doi: 10.3389/fncel.2012.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapiz MD, Morilak DA. Noradrenergic modulation of cognitive function in rat medial prefrontal cortex as measured by attentional set shifting capability. Neuroscience. 2006;137:1039–1049. doi: 10.1016/j.neuroscience.2005.09.031. [DOI] [PubMed] [Google Scholar]
- Lapiz MD, Zhao Z, Bondi CO, O'Donnell JM, Morilak DA. Blockade of autoreceptor-mediated inhibition of norepinephrine release by atipamezole is maintained after chronic reuptake inhibition. Int J Neuropsychopharmacol. 2007;10:827–833. doi: 10.1017/S1461145707007651. [DOI] [PubMed] [Google Scholar]
- Lee YA, Goto Y. Chronic stress modulation of prefrontal cortical NMDA receptor expression disrupts limbic structure--prefrontal cortex interaction. Eur J Neurosci. 2011;34:426–436. doi: 10.1111/j.1460-9568.2011.07750.x. [DOI] [PubMed] [Google Scholar]
- Liston C, McEwen BS, Casey BJ. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proc Natl Acad Sci USA. 2009;106:912–917. doi: 10.1073/pnas.0807041106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liston C, Miller MM, Goldwater DS, Radley JJ, Rocher AB, Hof PR, et al. Stress-induced alterations in prefrontal cortical dendritic morphology predict selective impairments in perceptual attentional set-shifting. J Neurosci. 2006;26:7870–7874. doi: 10.1523/JNEUROSCI.1184-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RJ, Aghajanian GK. Stress blunts serotonin- and hypocretin-evoked EPSCs in prefrontal cortex: role of corticosterone-mediated apical dendritic atrophy. Proc Natl Acad Sci USA. 2008;105:359–364. doi: 10.1073/pnas.0706679105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupinsky D, Moquin L, Gratton A. Interhemispheric regulation of the medial prefrontal cortical glutamate stress response in rats. J Neurosci. 2010;30:7624–7633. doi: 10.1523/JNEUROSCI.1187-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma S, Morilak DA. Chronic intermittent cold stress sensitises the hypothalamic-pituitary-adrenal response to a novel acute stress by enhancing noradrenergic influence in the rat paraventricular nucleus. J Neuroendocrinol. 2005a;17:761–769. doi: 10.1111/j.1365-2826.2005.01372.x. [DOI] [PubMed] [Google Scholar]
- Ma S, Morilak DA. Norepinephrine release in medial amygdala facilitates activation of the hypothalamic-pituitary-adrenal axis in response to acute immobilisation stress. J Neuroendocrinol. 2005b;17:22–28. doi: 10.1111/j.1365-2826.2005.01279.x. [DOI] [PubMed] [Google Scholar]
- Magarinos AM, McEwen BS. Stress-induced atrophy of apical dendrites of hippocampal CA3c neurons: comparison of stressors. Neuroscience. 1995;69:83–88. doi: 10.1016/0306-4522(95)00256-i. [DOI] [PubMed] [Google Scholar]
- Marek GJ, Aghajanian GK. 5-HT2A receptor or alpha1-adrenoceptor activation induces excitatory postsynaptic currents in layer V pyramidal cells of the medial prefrontal cortex. Eur J Pharmacol. 1999;367:197–206. doi: 10.1016/s0014-2999(98)00945-5. [DOI] [PubMed] [Google Scholar]
- Martin KP, Wellman CL. NMDA receptor blockade alters stress-induced dendritic remodeling in medial prefrontal cortex. Cereb Cortex. 2011;21:2366–2373. doi: 10.1093/cercor/bhr021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlonan K, Brown VJ. Orbital prefrontal cortex mediates reversal learning and not attentional set shifting in the rat. Behav Brain Res. 2003;146:97–103. doi: 10.1016/j.bbr.2003.09.019. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54:200–207. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann NY Acad Sci. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Conrad CD, Kuroda Y, Frankfurt M, Magarinos AM, McKittrick C. Prevention of stress-induced morphological and cognitive consequences. Eur Neuropsychopharmacol. 1997;7 (Suppl 3:S323–S328. doi: 10.1016/s0924-977x(97)00064-3. [DOI] [PubMed] [Google Scholar]
- McGaugh JL, Roozendaal B. Role of adrenal stress hormones in forming lasting memories in the brain. Curr Opin Neurobiol. 2002;12:205–210. doi: 10.1016/s0959-4388(02)00306-9. [DOI] [PubMed] [Google Scholar]
- McGaughy J, Ross RS, Eichenbaum H. Noradrenergic, but not cholinergic, deafferentation of prefrontal cortex impairs attentional set-shifting. Neuroscience. 2008;153:63–71. doi: 10.1016/j.neuroscience.2008.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkl A, Schubert F, Quante A, Luborzewski A, Brakemeier EL, Grimm S, et al. Abnormal cingulate and prefrontal cortical neurochemistry in major depression after electroconvulsive therapy. Biol Psychiatry. 2011;69:772–779. doi: 10.1016/j.biopsych.2010.08.009. [DOI] [PubMed] [Google Scholar]
- Merriam EP, Thase ME, Haas GL, Keshavan MS, Sweeney JA. Prefrontal cortical dysfunction in depression determined by Wisconsin Card Sorting Test performance. Am J Psychiatry. 1999;156:780–782. doi: 10.1176/ajp.156.5.780. [DOI] [PubMed] [Google Scholar]
- Moghaddam B, Bolinao ML, Stein-Behrens B, Sapolsky R. Glucocorticoids mediate the stress-induced extracellular accumulation of glutamate. Brain Res. 1994;655:251–254. doi: 10.1016/0006-8993(94)91622-5. [DOI] [PubMed] [Google Scholar]
- Morilak DA, Barrera G, Echevarria DJ, Garcia AS, Hernandez A, Ma S, et al. Role of brain norepinephrine in the behavioral response to stress. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:1214–1224. doi: 10.1016/j.pnpbp.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Morilak DA, Frazer A. Antidepressants and brain monoaminergic systems: a dimensional approach to understanding their behavioural effects in depression and anxiety disorders. Int J Neuropsychopharmacol. 2004;7:193–218. doi: 10.1017/S1461145704004080. [DOI] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, et al. Emotional bias and inhibitory control processes in mania and depression. Psychol Med. 1999;29:1307–1321. doi: 10.1017/s0033291799001233. [DOI] [PubMed] [Google Scholar]
- Musazzi L, Racagni G, Popoli M. Stress, glucocorticoids and glutamate release: effects of antidepressant drugs. Neurochem Int. 2011;59:138–149. doi: 10.1016/j.neuint.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Nakane H, Shimizu N, Hori T. Stress-induced norepinephrine release in the rat prefrontal cortex measured by microdialysis. Am J Physiol. 1994;267 (6 Pt 2:R1559–R1566. doi: 10.1152/ajpregu.1994.267.6.R1559. [DOI] [PubMed] [Google Scholar]
- Nomura S, Watanabe M, Ukei N, Nakazawa T. Stress and beta-adrenergic receptor binding in the rat's brain. Brain Res. 1981;224:199–203. doi: 10.1016/0006-8993(81)91133-1. [DOI] [PubMed] [Google Scholar]
- Nutt DJ. The neuropharmacology of serotonin and noradrenaline in depression. Int Clin Psychopharmacol. 2002;17 (Suppl 1:S1–12. doi: 10.1097/00004850-200206001-00002. [DOI] [PubMed] [Google Scholar]
- Pardon MC, Ma S, Morilak DA. Chronic cold stress sensitizes brain noradrenergic reactivity and noradrenergic facilitation of the HPA stress response in Wistar Kyoto rats. Brain Res. 2003;971:55–65. doi: 10.1016/s0006-8993(03)02355-2. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C.1998The Rat Brain in Stereotaxic Coordinates4th EditionAcademic Press: San Diego [Google Scholar]
- Popoli M, Yan Z, McEwen BS, Sanacora G. The stressed synapse: the impact of stress and glucocorticoids on glutamate transmission. Nat Rev Neurosci. 2012;13:22–37. doi: 10.1038/nrn3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radley JJ, Sisti HM, Hao J, Rocher AB, McCall T, Hof PR, et al. Chronic behavioral stress induces apical dendritic reorganization in pyramidal neurons of the medial prefrontal cortex. Neuroscience. 2004;125:1–6. doi: 10.1016/j.neuroscience.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Radley JJ, Williams B, Sawchenko PE. Noradrenergic innervation of the dorsal medial prefrontal cortex modulates hypothalamo-pituitary-adrenal responses to acute emotional stress. J Neurosci. 2008;28:5806–5816. doi: 10.1523/JNEUROSCI.0552-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry. 2007;61:928–934. doi: 10.1016/j.biopsych.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Ressler KJ, Nemeroff CB. Role of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disorders. Depress Anxiety. 2000;12 (Suppl 1:2–19. doi: 10.1002/1520-6394(2000)12:1+<2::AID-DA2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Roozendaal B, Schelling G, McGaugh JL. Corticotropin-releasing factor in the basolateral amygdala enhances memory consolidation via an interaction with the beta-adrenoceptor-cAMP pathway: dependence on glucocorticoid receptor activation. J Neurosci. 2008;28:6642–6651. doi: 10.1523/JNEUROSCI.1336-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sara SJ, Vankov A, Herve A. Locus coeruleus-evoked responses in behaving rats: a clue to the role of noradrenaline in memory. Brain Res Bull. 1994;35:457–465. doi: 10.1016/0361-9230(94)90159-7. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Thompson W, Carter CS, Steinhauer SR, Thase ME. Increased amygdala and decreased dorsolateral prefrontal BOLD responses in unipolar depression: related and independent features. Biol Psychiatry. 2007;61:198–209. doi: 10.1016/j.biopsych.2006.05.048. [DOI] [PubMed] [Google Scholar]
- Skaper SD, Facci L, Strijbos PJ. Neuronal protein kinase signaling cascades and excitotoxic cell death. Ann NY Acad Sci. 2001;939:11–22. doi: 10.1111/j.1749-6632.2001.tb03606.x. [DOI] [PubMed] [Google Scholar]
- Stuss DT, Levine B, Alexander MP, Hong J, Palumbo C, Hamer L, et al. Wisconsin Card Sorting Test performance in patients with focal frontal and posterior brain damage: effects of lesion location and test structure on separable cognitive processes. Neuropsychologia. 2000;38:388–402. doi: 10.1016/s0028-3932(99)00093-7. [DOI] [PubMed] [Google Scholar]
- Tait DS, Brown VJ, Farovik A, Theobald DE, Dalley JW, Robbins TW. Lesions of the dorsal noradrenergic bundle impair attentional set-shifting in the rat. Eur J Neurosci. 2007;25:3719–3724. doi: 10.1111/j.1460-9568.2007.05612.x. [DOI] [PubMed] [Google Scholar]
- Venero C, Borrell J. Rapid glucocorticoid effects on excitatory amino acid levels in the hippocampus: a microdialysis study in freely moving rats. Eur J Neurosci. 1999;11:2465–2473. doi: 10.1046/j.1460-9568.1999.00668.x. [DOI] [PubMed] [Google Scholar]
- Waterhouse BD, Moises HC, Woodward DJ. Alpha-receptor-mediated facilitation of somatosensory cortical neuronal responses to excitatory synaptic inputs and iontophoretically applied acetylcholine. Neuropharmacology. 1981;20:907–920. doi: 10.1016/0028-3908(81)90020-4. [DOI] [PubMed] [Google Scholar]
- Waterhouse BD, Mouradian R, Sessler FM, Lin RC. Differential modulatory effects of norepinephrine on synaptically driven responses of layer V barrel field cortical neurons. Brain Res. 2000;868:39–47. doi: 10.1016/s0006-8993(00)02261-7. [DOI] [PubMed] [Google Scholar]
- Wellman CL. Dendritic reorganization in pyramidal neurons in medial prefrontal cortex after chronic corticosterone administration. J Neurobiol. 2001;49:245–253. doi: 10.1002/neu.1079. [DOI] [PubMed] [Google Scholar]
- Woodward DJ, Moises HC, Waterhouse BD, Yeh HH, Cheun JE. Modulatory actions of norepinephrine on neural circuits. Adv Exp Med Biol. 1991;287:193–208. doi: 10.1007/978-1-4684-5907-4_16. [DOI] [PubMed] [Google Scholar]
- Woolley CS, Gould E, McEwen BS. Exposure to excess glucocorticoids alters dendritic morphology of adult hippocampal pyramidal neurons. Brain Res. 1990;531:225–231. doi: 10.1016/0006-8993(90)90778-a. [DOI] [PubMed] [Google Scholar]
- Yuen EY, Liu W, Karatsoreos IN, Feng J, McEwen BS, Yan Z. Acute stress enhances glutamatergic transmission in prefrontal cortex and facilitates working memory. Proc Natl Acad Sci USA. 2009;106:14075–14079. doi: 10.1073/pnas.0906791106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen EY, Liu W, Karatsoreos IN, Ren Y, Feng J, McEwen BS, et al. Mechanisms for acute stress-induced enhancement of glutamatergic transmission and working memory. Mol Psychiatry. 2011;16:156–170. doi: 10.1038/mp.2010.50. [DOI] [PMC free article] [PubMed] [Google Scholar]