Abstract
Background
Reducing weight-bearing stress to diabetic foot ulcers is critical to healing and commonly called offloading. Removable cast walkers are frequently used for offloading; however, patient compliance is often poor. Walkers commonly extend to the knee. Patients complain about walkers' weight and diminished balance with their use. This study compared the offloading capacity of walkers that varied by height. Heights included: knee, ankle, and shoe levels. To ensure a fair comparison the outsole and insole were standardized across the devices.
Methods
Eleven diabetic subjects with moderate to high risk of ulceration were recruited. Subjects completed four 20 m walking trials. Subjects performed one trial with each walker and one trial with an athletic shoe. Primary outcomes focused on plantar loading and were measured by pressure insoles. Secondary outcomes were associated with gait kinematics as collected by body worn sensors.
Findings
Significant differences were found for the peak pressure and pressure time integrals of the different footwear. All walkers performed better than the athletic shoe. The ankle and knee-high devices performed best. Center of mass rotation data showed a trend of the ankle walker yielding a smaller range of motion (18% medial/lateral and 22% anterior/posterior) than the knee level.
Interpretation
The ankle-high walker was able to provide similar offloading capacities as the knee-high walker. The diminished weight, along with potentially improved stability, may result in improved compliance with ankle-high walkers. A study comparing the use of the two devices for treating ulcers is now suggested.
Keywords: Offloading, Diabetic foot ulcer, Diabetes, Pedobarography
1. Introduction
Roughly 25% of all hospital days for persons with diabetes are due to foot complications (Block, 1981; Gibbons and Eliopoulos, 1984; Smith et al., 1987). A large number of these days are attributable to diabetic foot ulcers (DFU). Individuals with diabetes run a 12–25% lifetime risk of developing a DFU (Abbott et al., 2005; Singh et al., 2005). Foot ulcers are among the most serious complications associated with diabetes. Stockl et al. found that the average cost to treat a DFU during the years 2000–2001 was $13,179 and the mean cost for the most severe wounds was $27,721 (Stockl et al., 2004). Besides the sizable economic burden, these ulcers induce extensive emotional, physical, and productivity losses (Boulton et al., 2004; Meijer et al., 2001; Vileikyte, 2001; Vileikyte and Boulton, 2000). In addition to the immediate negative impact of ulcers on persons with diabetes, ulcers often lead to even more dire consequences. Persons with diabetes are 15 to 46 times more likely to have lower extremity amputations than persons without diabetes, (Armstrong et al., 1997; Lavery et al., 1999; Most and Sinnock, 1983; Reiber, 1996) and ulcerations are “the most important factor for lower-extremity amputation” (p 1725) (Cavanagh et al., 2005).
DFUs commonly occur on the plantar aspect of the foot in response to the repetitive trauma induced by the pressures generated by weight-bearing activities (Lavery et al., 1996; Wu et al., 2005). Thus one of the most critical components to the paradigm of preventing and healing these ulcers is pressure reduction at the wound site or “offloading” (Cavanagh et al., 2005; Wu et al., 2005). Knowing that offloading is critical, practitioners are still faced with the challenge of selecting the appropriate offloading modality for their patient. To date the total contact cast (TCC) and removable cast walkers — particularly the DH Pressure Relief Walker (Royce Medical, Camarillo, CA), have the most data to support their use in healing ulcers (Cavanagh and Bus, 2010). However, TCC are not commonly used in practice in the US, with only 1.7% of foot clinics using them as their standard offloading modality (Wu et al., 2008). Although RCW are used more commonly, they have been shown to provide poorer healing outcomes (Armstrong et al., 2001; Gutekunst et al., 2011). This is despite the fact that the two modalities provide nearly equivalent offloading (Baumhauer et al., 1997; Gutekunst et al., 2011; Lavery et al., 1996).
The specific mechanism by which RCW offload is not fully understood. RCW typically have rigid struts (or circumferential lattice encasements) that run up the majority of the shank. The struts are believed to limit isolated pockets of high pressure on the foot by immobilizing the ankle. With the ankle immobilized the foot is not free to progress through its typical heel strike to toe offloading pattern. Instead with the ankle locked and a rocker bottom sole on the RCW, a large portion of the foot maintains contact and subsequently loads throughout the step. Shaw et al. previously found that approximately 1/3 of a subject's load was transferred as shear stress to the walls of the TCC, which act as rigid conical receptacles to support the inverted cone shaped legs (Shaw et al., 1997). It is unlikely that RCW provide offloading by a similar means as they do not provide rigid direct contact with the entire surface of the leg, nor are they custom fit to legs. Whether any load might be transferred to the struts, which are circumferentially fixed to the leg, is unknown.
The decreased healing associated with RCW has been attributed to patient behavior as opposed to the device itself. When RCW are not securely fixed to a patient by casting tape or other means, many patients do not compliantly use them (Armstrong et al., 2003). Impeded balance (van Deursen, 2008) and the weight of the device likely contribute to this lack of adherence. While weight concerns may be argued to be more of an inconvenience than a serious problem, decreased stability poses a serious risk of fall related injuries to these patients. In 2009 59.9% of all US adults with diabetes reported some type of mobility limitation Centers for Disease Control and Prevention (2011). Furthermore, the same severe neuropathy that allows DFUs to form also puts individuals at risk of falls (Richardson, 2002) and individuals with DFU have been shown to have an even greater deterioration in balance than individuals with diabetic neuropathy alone (Kanade et al., 2008). Should a fall occur, it has been shown that diabetes is associated with longer hospital stays following falls (Kennedy et al., 2001). If lower (or no) struts that weighed less with a lesser impact on balance could provide similar offloading capabilities, the incorporation of them into RCW may improve compliance. Additionally, as peripheral edema is more common in individuals with type 2 diabetes than non-diabetic individuals (Brodovicz et al., 2009), patients with DFUs may present with large amounts of edema in the leg. When a RCW is used with these patients there may be tissue that hangs over the top of the rigid struts. Consequently, this poses the risk of the development of new wounds at the interface of this tissue and the strut.
The purpose of this study was to compare the offloading capacity of RCW of varied height. A comparison was made between RCW's that extended proximally: up the majority of the shank (knee-high), just past the ankle (ankle-high), or only encompassed the foot (shoe-offloader). To ensure a fair comparison, the rocker outsole and insole were standardized across the three devices. Should RCW with lowered strut height still provide adequate offloading, patients that use them may have better healing outcomes due to increased adherence.
2. Methods
2.1. Subjects
Subjects were eligible to participate if they were an adult with type 1 or 2 diabetes mellitus at moderate/high risk for DFU (risk grade 1 or higher: Diabetic Foot Risk Classification System of the International Working Group on the Diabetic Foot (Peters and Lavery, 2001)). Exclusion criteria included inability to walk without an assistive device such as a walker or crutches, and the presence of an active DFU. All subjects read and signed an institutional review board approved consent form prior to participation. Eleven subjects were recruited for participation (Table 1.)
Table 1.
Subject demographics.
| Age | 51.4 (10) years |
| Gender | Male = 7; Female = 4 |
| BMI | 33.9 (7.3) |
| Diabetes type | Type I = 2; type II = 9 |
| Duration of diabetes | 14.5 (9) years |
| Diabetic foot risk classification | Grade 1 = 8; grade 3 = 1; grade 4 = 2 |
Note: Values in parentheses are the standard deviation of the associated mean.
2.1.1. Sample size calculation
The sample size was based upon the work by Lavery et al., (1996). With an expected difference of 40 kPa between means and a SD of 20 kPa, seven observations would be required per condition at a power of 80 and a P=0.05 to demonstrate a difference between RCW. In order to allow for potentially greater variability within this subject sample and to allow for exploration of the secondary outcomes, 11 subjects were recruited.
2.2. Procedures
Each subject completed walking trials in the three RCW and a control condition of a standard athletic shoe (Fig. 1). The knee-high RCW was a standard DH Offloading Walker™ (Össur Americas, Foothill Ranch, CA), the ankle-high and shoe RCW only differed in regards to the height the side struts and soft goods extended up the shank. The ankle-high RCW consisted of the commercially available low top Equalizer Walker™ paired with the DH Offloading Walker's insole. The shoe RCW was created by cutting the side struts and accompanying softgoods off of DH Offloading Walkers. For a subject wearing a U.S. men's size 10 shoe the progressive weight from standard shoe to knee-high RCW would be 0.3, 1.0, 1.1, and 1.4 kg for the respective devices. Upon agreeing to participate, subjects were fitted for the appropriate sized RCWs and shoes. The order of footwear conditions was randomized for each subject. An investigator was responsible for securing each offloading device and shoe for subjects. The foot that was classified to be a higher risk donned the RCW's. If both feet were of equivalent risk, the right foot used the RCW. Subjects wore the standardized athletic shoe on the non-study limb for each trial. After putting on each device, the subjects had approximately 1–2 min to acclimate themselves to walking with the device. The subject then completed one 20-m walking trial during which data was collected. Subjects walked each trial at a self-selected speed. In order to ensure the insole consistency across the RCW's for each subject, the same insole was transferred between the three RCW's. No efforts were made to ensure a subject walked at equivalent speeds with each device. Although speed and stride length influence ground reaction forces generated during walking, the intent of this study was to assess the loading of the foot subjects were exposed to while wearing the different RCW. If walking speed were controlled, the results obtained may not represent the loading that subjects would experience if they weren't being observed.
Fig. 1.

Three RCW and standard athletic shoe. Footwear compared: 1) knee-high RCW; 2) ankle-high RCW; 3) shoe RCW; 4) standard athletic shoe. Relative weight of each device in comparison to the knee-high RCW is presented as a %.
The primary outcomes were concerned with the offloading capacity of the RCW. While completing the 20-m walking trial, the plantar pressure on the feet of the subject was recorded by in shoe pressure insoles at 100 Hz (Pedar-X, Novel, Germany). Secondary outcomes included balance as assessed by range of motion of the center of mass (CoM) (Najafi et al., 2010; Wrobel et al., 2010) and kinematic parameters such as stride length and velocity. This data was obtained by Physilog (BioAGM, CH) measurements. The method for calculating spatio-temporal parameters of gait and its validity has been previously described in detail (Aminian et al., 2002). Briefly, the Physilog system uses a series of body worn sensors including gyroscopes and accelerometers that are attached by elastic bands to the subject in order to calculate kinematic parameters of gait. Sensors were attached to the shins, thighs, and lumbar region of subjects. Data was collected at 200 Hz and saved on a secure digital (SD) memory card. After the completion of trials, data was transferred from the SD card to a personal computer for analysis.
2.3. Analysis
The primary outcomes of the study were the peak pressures and pressure time integrals associated with the different RCW. The sole of the foot was divided into nine masks (Fig. 2) for the purpose of analyzing the pressure data. The peak pressure and pressure time integral data were each applied to a repeated measures ANOVA with main effects of footwear condition and foot region. A Least Significant Difference test was used for post hoc analyses following ANOVA findings of P<0.05. One-way ANOVA test was used to assess gait velocity across conditions. Although the study was not powered to detect differences in CoM motion due to the novelty of this assessment, the data was applied to one-way (footwear condition) repeated measures ANOVA.
Fig. 2.

Masking scheme for peak pressure and pressure time integral data.
3. Results
3.1. Offloading
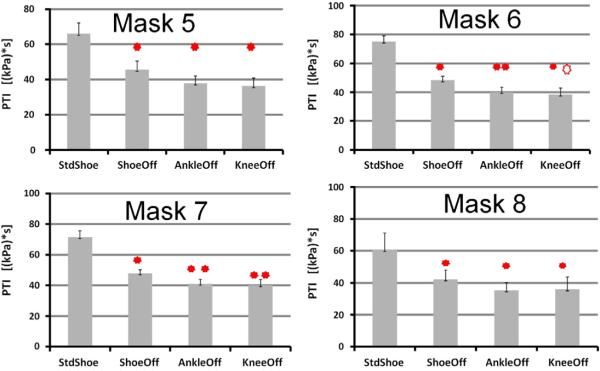
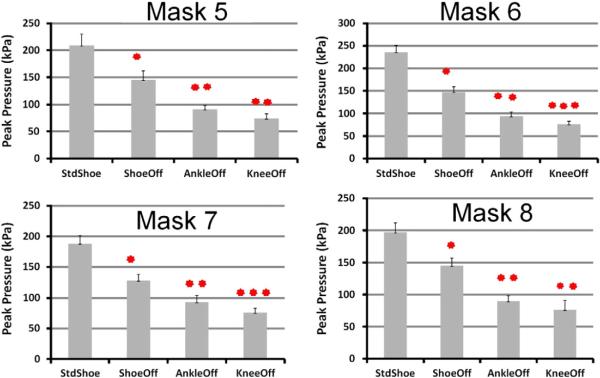
The peak pressure data revealed a significant interaction between footwear and foot region. Therefore, the Least Significant Difference post hoc was used to compare each footwear condition within each foot region. Fig. 3 displays the results of the post hoc analyses for four masks (5, 6, 7 and 8) corresponding to commonly ulcerated regions of the foot: the hallux and metatarsal heads. The pressure time integral data also yielded a significant difference for the interaction between footwear and foot region. The results of the post hoc analyses are presented in Fig. 4. Although gait velocity was not controlled, the ANOVA indicated there was no difference between the conditions (P=0.38).
Fig. 3.
Peak pressure at hallux and metatarsal heads. Note: Stars are used to identify progressively lower mean values (P<0.05) between the offloading devices.
Fig. 4.
Pressure time integral at hallux and metatarsal heads. Note: Stars are used to identify progressively lower mean values (P<0.05) between the offloading devices. A hollow star indicates that the associated offloading device had a value that fell between a device with one less total stars and a device with an equivalent number of total stars.
3.2. Balance and gait
During the first four steps of walking the medial/lateral CoM range of motion relative to the athletic shoe demonstrated a progressive increase in range of motion from the standard shoe to the shoe-offloader (+8.4%), ankle-high offloader (+11.5%), and finally knee-high offloader (+35.4%) (Fig. 5). This secondary outcome did not reach statistical significance. The CoM range of motion in the anterior/posterior direction progressed from the standard shoe to the ankle-high offloader (+3.9%), shoe offloader (+23.0%), and knee-high offloader (+33.7%) (Fig. 5). Gait parameters are presented in Table 2. A moderate deterioration in spatio-temporal parameters of gait was observed by wearing the RCW. Although the ANOVA indicated there was no difference between the groups, pairwise comparisons did suggest one pairing significantly differed in gait velocity. Specifically, gait velocity was reduced in average by 12% by wearing the knee-high RCW compared to regular shoes (P=0.028, 95%CI= [−0.22,−0.02]m/s).
Fig. 5.
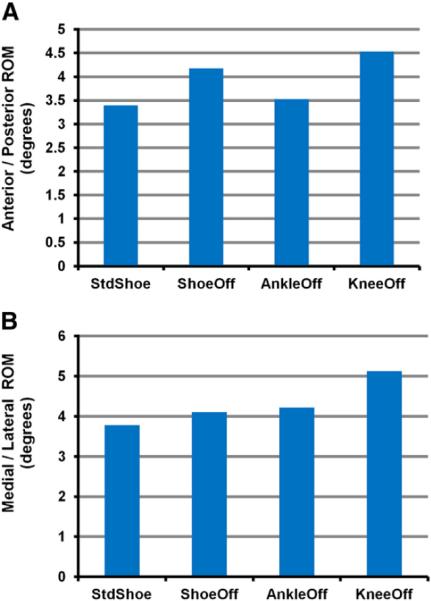
Center of mass range of motion (RoM) during first four steps.A). RoM in the anterior/posterior directionB). RoM in the medial/lateral direction.
Table 2.
Gait parameters.
| Standard athletic shoe | Shoe RCW | Ankle-high RCW | Knee-high RCW | |
|---|---|---|---|---|
| Stride velocity, m/s | 1.05 (0.20) | 1.07 (0.09) | 0.97 (0.18) | 0.93 (0.19) |
| Stride length, m | 1.22 (0.07) | 1.30 (0.12) | 1.17 (0.09) | 1.15 (0.12) |
| Stride time, m | 1.22 (0.24) | 1.23 (0.16) | 1.30 (0.24) | 1.31 (0.28) |
| Double support | 26.5 (8.0) | 26.4 (7.6) | 28.7 (5.8) | 28.6 (8.8) |
| Inter-cycle gait velocity variability, % | 4.68 (3.08) | 4.23 (2.12) | 6.68 (4.98) | 4.66 (2.84) |
Note: m = meter; s = second; values in parentheses are the standard deviation of the associated mean.
4. Discussion
The primary outcomes pressure data are in line with previous work. For example a previous study found the mean peak pressure at the hallux ranged from 64 to 122 kPa for four RCW in patients with a history of DFU (Lavery et al., 1996). In the present study the peak pressure at the hallux was 76 kPa in the knee-high, 90 kPa in the ankle-high, and 145 kPa in the shoe level RCW. As a gauge of cumulative stress, the pressure time integral indicated the ankle-high and knee-high RCW provided equivalent offloading of the metatarsals heads and hallux. The two RCW also yielded equivalent peak pressure values in the medial forefoot and hallux regions. There was a small but significant difference in the peak pressure at the mid and lateral forefoot masks between the two RCW. The peak pressure and pressure time integral data collectively indicated that the ankle-high RCW provided similar offloading as the traditional knee-high RCW. Thus extending RCW strut height beyond the region of the ankle does not appear to provide additional benefit. This is in contrast to the TCC in which the side walls have been found to actively take up loading (Shaw et al., 1997) and therefore, greater height/contact area could allow for greater offloading. Although, the struts of the RCW did not directly accept loading, they did play a part in offloading as evidenced by the shoe RCW performing worse than the knee and ankle-high versions. It is believed the struts contributed to offloading by locking the ankle joint and in combination with the rocker bottom sole, preventing normal heel to toe step progression.
Cumulatively, the pressure data indicates that the ankle-high and knee-high RCW should provide similar DFU healing benefits, assuming compliance is equivalent. There is reason to believe, however, that compliance with the ankle-high RCW might be higher than with the knee-high RCW. One incentive to increased compliance with the ankle-high RCW is the reduced weight. A second is the potentially improved balance. Although the secondary outcome of COM range of motion did not reach statistical significance in this initial study, a noteworthy trend was observed. The trend of decreased motion of the CoM during the first four steps of gait, a particularly high-risk time for falls, may be indicative of improved balance with the ankle-high RCW. Utilizing the data from this initial study, future studies can be designed to test this hypothesis.
One limitation in assessing the RCW's influence on balance in this study was the simplicity of the walking trials. Had a dual-task walking scenario or other more challenging activities been utilized, any differences in balance between the RCW would have likely been more easily seen. An initially somewhat surprising finding was the ankle-high RCW yielding the lowest range of motion of the three RCW. While reduced weight and size may have been advantageous relative to the knee-high RCW, the fixing of the ankle joint likely contributed to the greater stability than seen with the shoe RCW. The rigid rocker bottom sole used in all three RCW posed a challenge to gait. While the inclusion of struts fixed the ankle joint and limited some of the freedom and necessity to respond to this challenge, the shoe RCW allowed the ankle to plantar/dorsi-flex in response to the rocking motion of the foot. The challenge of eliciting a controlled response from the ankle to match the motion of the rocker bottom was likely very difficult for these individuals with challenged somatosensory feedback.
In addition to further investigation of influence of strut height on balance, other lines of research would be justified based upon this initial study. Previous work has been done to develop a means of determining adherence with offloading devices (Crews et al., 2009) and it would be of interest to see if ankle-high RCW do result in higher compliance than the knee-high in individuals with DFU. Additionally, a direct comparison between healing rates in the two devices is needed before practitioners can confidently prescribe the less commonly employed ankle-high RCW.
5. Conclusion
Considering the ankle-high RCW was a nearly equivalent offloader to the knee-high RCW, while weighing less and potentially providing better stability, it may prove to provide better outcomes in treating DFU. It may also be a good choice for individuals with significant edema at the proximal end of the leg, as it would likely conform better to edematous legs.
Acknowledgement
The project described was supported by Award Number T35DK074390 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. Removable cast walkers were provided at no cost by Össur, however, representatives from Össur had no role in the study design, data collection, data analysis, nor this manuscript.
Appendix A. Risk Categories of the Diabetic Foot Risk Classification System of the International Working Group on the Diabetic Foot
| grade 0 | no neuropathy |
| grade 1 | neuropathy without peripheral vascular disease (PAD) or foot deformity |
| grade 2 | neuropathy with foot deformity and /or PAD |
| grade 4 | history of foot ulcer, lower extremity amputation or end stage renal disease |
References
- Abbott CA, Garrow AP, Carrington AL, Morris J, Van Ross ER, Boulton AJ. Foot ulcer risk is lower in South-Asian and african-Caribbean compared with European diabetic patients in the U.K.: the North-West diabetes foot care study. Diabetes Care. 2005;28:1869–1875. doi: 10.2337/diacare.28.8.1869. [DOI] [PubMed] [Google Scholar]
- Aminian K, Najafi B, Bula C, Leyvraz PF, Robert P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J. Biomech. 2002;35:689–699. doi: 10.1016/s0021-9290(02)00008-8. [DOI] [PubMed] [Google Scholar]
- Armstrong DG, Lavery LA, Van Houtum WH, Harkless LB. Seasonal variations in lower extremity amputation. J. Foot Ankle Surg. 1997;36:146–150. doi: 10.1016/s1067-2516(97)80062-2. [DOI] [PubMed] [Google Scholar]
- Armstrong DG, Nguyen HC, Lavery LA, Van Schie CH, Boulton AJ, Harkless LB. Off-loading the diabetic foot wound: a randomized clinical trial. Diabetes Care. 2001;24:1019–1022. doi: 10.2337/diacare.24.6.1019. [DOI] [PubMed] [Google Scholar]
- Armstrong DG, Lavery LA, Kimbriel HR, Nixon BP, Boulton AJ. Activity patterns of patients with diabetic foot ulceration: patients with active ulceration may not adhere to a standard pressure off-loading regimen. Diabetes Care. 2003;26:2595–2597. doi: 10.2337/diacare.26.9.2595. [DOI] [PubMed] [Google Scholar]
- Baumhauer JF, Wervey R, Mcwilliams J, Harris GF, Shereff MJ. A comparison study of plantar foot pressure in a standardized shoe, total contact cast, and prefabricated pneumatic walking brace. Foot Ankle Int. 1997;18:26–33. doi: 10.1177/107110079701800106. [DOI] [PubMed] [Google Scholar]
- Block P. The diabetic foot ulcer: a complex problem with a simple treatment approach. Mil. Med. 1981;146:644–646. [PubMed] [Google Scholar]
- Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N. Engl. J. Med. 2004;351:48–55. doi: 10.1056/NEJMcp032966. [DOI] [PubMed] [Google Scholar]
- Brodovicz KG, Mcnaughton K, Uemura N, Meininger G, Girman CJ, Yale SH. Reliability and feasibility of methods to quantitatively assess peripheral edema. Clin. Med. Res. 2009;7:21–31. doi: 10.3121/cmr.2009.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh PR, Bus SA. Off-loading the diabetic foot for ulcer prevention and healing. J. Am. Podiatr. Med. Assoc. 2010;100:360–368. doi: 10.7547/1000360. [DOI] [PubMed] [Google Scholar]
- Cavanagh PR, Lipsky BA, Bradbury AW, Botek G. Treatment for diabetic foot ulcers. Lancet. 2005;366:1725–1735. doi: 10.1016/S0140-6736(05)67699-4. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [[Accessed 2011]];Diabetes Public Health Resource. (online) Available: http://www.cdc.gov/diabetes/
- Crews RT, Armstrong DG, Boulton AJ. A method for assessing off-loading compliance. J. Am. Podiatr. Med. Assoc. 2009;99:100–103. doi: 10.7547/0980100. [DOI] [PubMed] [Google Scholar]
- Gibbons G, Eliopoulos GM. Infection of the diabetic foot. In: Kozak GP, Hoar CS, Rowbotham JL, editors. Management of Diabetic Foot Problems. WB Saunders; Philadelphia: 1984. [Google Scholar]
- Gutekunst DJ, Hastings MK, Bohnert KL, Strube MJ, Sinacore DR. Removable cast walker boots yield greater forefoot off-loading than total contact casts. Clin. Biomech. 2011;26(6):649–654. doi: 10.1016/j.clinbiomech.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanade RV, Van Deursen RW, Harding KG, Price PE. Investigation of standing balance in patients with diabetic neuropathy at different stages of foot complications. Clin. Biomech. 2008;23:1183–1191. doi: 10.1016/j.clinbiomech.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Kennedy RL, Grant PT, Blackwell D. Low-impact falls: demands on a system of trauma management, prediction of outcome, and influence of comorbidities. J. Trauma. 2001;51:717–724. doi: 10.1097/00005373-200110000-00016. [DOI] [PubMed] [Google Scholar]
- Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Reducing dynamic foot pressures in high-risk diabetic subjects with foot ulcerations. A comparison of treatments. Diabetes Care. 1996;19:818–821. doi: 10.2337/diacare.19.8.818. [DOI] [PubMed] [Google Scholar]
- Lavery LA, Van Houtum WH, Ashry HR, Armstrong DG, Pugh JA. Diabetes-related lower-extremity amputations disproportionately affect Blacks and Mexican Americans. South. Med. J. 1999;92:593–599. doi: 10.1097/00007611-199906000-00008. [DOI] [PubMed] [Google Scholar]
- Meijer JW, Trip J, Jaegers SM, Links TP, Smits AJ, Groothoff JW, et al. Quality of life in patients with diabetic foot ulcers. Disabil. Rehabil. 2001;23:336–340. doi: 10.1080/09638280010005585. [DOI] [PubMed] [Google Scholar]
- Most RS, Sinnock P. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes Care. 1983;6:87–91. doi: 10.2337/diacare.6.1.87. [DOI] [PubMed] [Google Scholar]
- Najafi B, Miller D, Jarrett BD, Wrobel JS. Does footwear type impact the number of steps required to reach gait steady state?: an innovative look at the impact of foot orthoses on gait initiation. Gait Posture. 2010;32:29–33. doi: 10.1016/j.gaitpost.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EJ, Lavery LA. Effectiveness of the diabetic foot risk classification system of the International Working Group on the Diabetic Foot. Diabetes Care. 2001;24:1442–1447. doi: 10.2337/diacare.24.8.1442. [DOI] [PubMed] [Google Scholar]
- Reiber GE. The epidemiology of diabetic foot problems. Diabet. Med. 1996;13(Suppl. 1):S6–S11. [PubMed] [Google Scholar]
- Richardson JK. Factors associated with falls in older patients with diffuse polyneuropathy. J. Am. Geriatr. Soc. 2002;50:1767–1773. doi: 10.1046/j.1532-5415.2002.50503.x. [DOI] [PubMed] [Google Scholar]
- Shaw JE, Hsi WL, Ulbrecht JS, Norkitis A, Becker MB, Cavanagh PR. The mechanism of plantar unloading in total contact casts: implications for design and clinical use. Foot Ankle Int. 1997;18:809–817. doi: 10.1177/107110079701801210. [DOI] [PubMed] [Google Scholar]
- Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–228. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- Smith D, Weinberger M, Katz B. A controlled trial to increase office visits and reduce hospitalization in diabetic patients. J. Gen. Intern. Med. 1987;2:232–238. doi: 10.1007/BF02596446. [DOI] [PubMed] [Google Scholar]
- Stockl K, Vanderplas A, Tafesse E, Chang E. Costs of lower-extremity ulcers among patients with diabetes. Diabetes Care. 2004;27:2129–2134. doi: 10.2337/diacare.27.9.2129. [DOI] [PubMed] [Google Scholar]
- Van Deursen R. Footwear for the neuropathic patient: offloading and stability. Diabetes Metab. Res. Rev. 2008;24(Suppl. 1):S96–S100. doi: 10.1002/dmrr.827. [DOI] [PubMed] [Google Scholar]
- Vileikyte L. Diabetic foot ulcers: a quality of life issue. Diabetes Metab. Res. Rev. 2001;17:246–249. doi: 10.1002/dmrr.216. [DOI] [PubMed] [Google Scholar]
- Vileikyte L, Boulton AJM. Psychological/behavioral issues in diabetic neuropathic foot ulceration. Wounds. 2000;12(6 Suppl. B):43B–47B. [Google Scholar]
- Wrobel JS, Edgar S, Cozzetto D, Maskill J, Peterson P, Najafi B. A proof-of-concept study for measuring gait speed, steadiness, and dynamic balance under various footwear conditions outside of the gait laboratory. J. Am. Podiatr. Med. Assoc. 2010;100:242–250. doi: 10.7547/1000242. [DOI] [PubMed] [Google Scholar]
- Wu SC, Crews RT, Armstrong DG. The pivotal role of offloading in the management of neuropathic foot ulceration. Curr. Diab. Rep. 2005;5:423–429. doi: 10.1007/s11892-005-0049-5. [DOI] [PubMed] [Google Scholar]
- Wu SC, Jensen JL, Weber AK, Robinson DE, Armstrong DG. Use of pressure offloading devices in diabetic foot ulcers: do we practice what we preach? Diabetes Care. 2008;31:2118–2119. doi: 10.2337/dc08-0771. [DOI] [PMC free article] [PubMed] [Google Scholar]