Abstract
The purpose of this study was to investigate effect of nutrition education at worksite program in male workers. The subjects were 75 male workers who had received nutrition education by a clinical dietitian for 4 months. The anthropometric data, blood pressure and biochemical blood indices were measured before and after nutrition education. Dietary habits and lifestyle were investigated by self-administered questionnaires. Nutrients intake was determined by 24-hour dietary recall method. The results showed significant decreases in body mass index (p < 0.05), fasting blood sugar (p < 0.01), total cholesterol (p < 0.05), and LDL-cholesterol (p < 0.05) after nutrition education. The correlation analyses among anthropometric and clinical parameters after nutrition education indicated that there was a significantly positive correlations between blood pressure and weight, r-GTP. A significantly positive correlations was observed between fasting blood sugar and triglycerides. A significantly positive correlations was observed between triglycerides and body mass index, r-GTP, SGPT. A significantly positive correlations was observed between SGPT and weight, body mass index. A significantly negative correlations was observed between HDL-cholesterol and weight. It could be concluded that nutrition education might be effective tool to improve anthropometric measures and clinical parameters in male workers. Continuing and systematic nutritional management programs should be developed and implemented for male workers at the worksites to maintain optimal health status.
Keywords: Body mass index, Blood lipids, Blood pressure, Blood glucose, Liver function tests, Nutrition eduction
Introduction
The rapid economic growth and westernized diet of Korea have triggered energy overconsumption [1], whereas the convenient modern lifestyle has led to the lack of exercise to increase metabolic syndromes, such as hypertension, diabetes and dyslipidemia [2,3]. Wilson et al. [4] defined metabolic syndrome as metabolic disorders that increase the risk of chronic diseases in which hypertension, hyperglycemia, dyslipidemia and abdominal obesity are simultaneously generated and progressed. Metablic syndromes are viewed as diseases that can be prevented by managing risk factors including obesity, drinking, smoking and wrong dietary habits to raise the importance of managing chronic illnesses and providing medical service [5].
The National Health Promotion Act enacted in 1995 regulates the nation and local autonomous entities to actively promote the regional society health project for improving the health of the public. This act has promoted the activation of health projects. As a part of the health project, nutrition education and consulting programs help subjects with nutritional issues to analyze their own dietary habits, learn proper living habits and solve problems. In particular, nutrition education provided in the workplace is especially beneficial to office workers that are unable to visit the hospital due to their work schedule. In the welfare aspect, it can also boost the work ambition of workers [6].
According to the study conducted by Lee & Suh [7], office workers began to become more interested in health as the society began to place greater emphasis on individual engagement and responsibility for health in relation to the increase in chronic diseases. However, due to various environmental factors, such as irregular work time, poor dietary habits, low nutrition knowledge, stress due to overwork and lack of health management efforts, chronic illnesses can be easily progressed among office workers. In fact, among chronic diseases, the prevalence rate of dyslipidemia is continuously increasing among men aged 30 and higher [8]. In particular, low HDL-cholesterolemia was increased from 22.8% in 1998 to 47.6% in 2007, thus presenting a 25.4% increase in 10 years (Ministry for Health, Welfare and Family Affairs & Korea Centers for Disease Control and Prevention, 2008). However, the opportunity of nutrition education, an essential factor in preventing and treating such diseases, remains insufficient [9].
According to precedent studies conducted on workers, providing a fixed period of nutrition education improved the dietary habits and lifestyles of subjects and positively influenced the clinical standard, thus reporting that significant effects can be acquired by implementing nutrition education in work places that provide at least one meal a day [10,11]. In a study conducted on office workers, Lee et al. [11] reported that providing a fixed period of nutrition education produced positive effects in reducing the weight and obesity of subjects, enhancing healthy behaviors and improving clinical standards [11-15]. In particular, by developing, systemizing and implementing an appropriate nutrition education program for workers according to workplace characteristics, the health conditions and the work morale of employees will be boosted increasing the pride for the company and productivity and reducing of national medical expenses. Furthermore, if the education content can be appropriately delivered to households, the nutrition education program implemented in the workplace after health check-up can also contribute to the improvement of domestic dietary life [16]. Thus, it is stipulated that providing an appropriate nutrition management education related with diseases and implementing continuous nutritional care and education through clinical nutritionists are not only essential for improving the health of office workers, enhancing company welfare and reducing medical costs, important for work efficacy. Furthermore, the role of the clinical nutritionist is to coach the subjects to independently find answers to change their dietary behaviors and maintain such changes in their dietary behaviors.
According to the results of the 2007 National Health Promotion Act, the obesity rate of Korean adults is gradually increasing from 30.6% in 2001, 31.5% in 2005 and 31.7% in 2007, along with the increased prevalence rate of obesity-related diseases. In case of metabolic syndromes, the prevalence rate of men have continuously increased from 20.8% to 32.9% after 1998 [17]. Furthermore, the study conducted by Bae et al. [18] on the changes in the obesity prevalence rate for 10 years (1997-2007) indicated that the obesity rate of men aged between 30-39 was increased 11.2% in a decade, from 20.7% in 1997 to 31.8% in 2007, whereas the obesity rate of men aged between 40-49 was increased 9.2%, from 25.6% in 1997 to 34.8% in 2007. The study also reported that it is necessary to evaluate and intervene dietary habits and health-related behaviors in order to reduce the obesity trend.
Hereupon, this study carried out health examination on male office workers with higher risk of having metabolic syndrome and classified subjects with abnormal findings (hypertension, diabetes, dyslipidemia, abnormal liver function indices). This study implemented the workplace-visiting nutrition education program based on the self-directed coaching method for changing poor dietary habits to proper dietary behaviors and attempted to analyze the effectiveness of the program.
Materials and Methods
Subjects and period
This study selected subjects with abnormal laboratory findings (hypertension, diabetes, dyslipidemia, abnormal liver function indices) among employees of L Company that received health examination and comprehensive medical checkup implemented by the National Health Insurance Workplace-visiting nutrition eduction program was implemented from June to September 2011. A total of 75 male office workers were included to evaluate the effectiveness of nutrition education. Subjects with abnormal findings related with metabolic syndromes were classified into the metabolic syndrome group if there were relevant to at least 3 out of 5 items in the NCEP ATPIII (Executive Summary of the Third Report of The National Cholesterol Education Program, 2001). The standards are as follows.
Fasting blood sugar ≥110 mg/dL
Waist circumference >90 cm (Men)
Blood pressure ≥130/85 mmHg
Triglycerides ≥150 mg/dL
HDL-cholesterol <40 mg/dL (Men)
Survey content and method
This study was conducted in a process consisting of basic survey, consulting of examination results, nutrition education and assessment. In the basic survey, the general information, physical measurement, meal journal, life styles, clinical and biochemical parameters were obtained. Nutrition education was conducted in a self-directed coaching method according to metabolic syndrome types based on examination results. Afterward, the final examination and assessment were carried out.
Anthropometric and biochemical measurements
Age and anthropometric measures including height (HT), weight (WT), waist circumference (WC) were obtained and body mass index was calculated. Subjects were asked to record the meal journal written based on the food intake survey chart of the 2009 Korean National Health and Nutrition Examination Survey developed by using the 24-hour recall method. The regularity of meals, drinking and smoking habits were asked. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and fasting blood sugar (FBS) were measured. Serum glutamic oxalacetic transaminase (SGOT), serum glutamic pyruvic transaminase (SGPT) and r-GTP (Gamma-glutamyl transpeptidase) were analyzed. As measures of liver function test. total cholesterol (TC), triglycerides (TG), high density lipoprotein cholesterol (HDLc), low density lipoprotein cholesterol (LDLc) were determined before and after the nutrition education.
Nutrition education program
Dietary habits were analyzed using the nutrition consulting program. Based on the dietary habits of study subjects, the clinical nutritionist implemented meal therapy consulting. Afterward, clinical nutritionists visited the workplace to provide nutrition assessment and education to observe the progress of subjects every month. Nutrition analysis program CAN-Pro version 3.0 (computer aided nutritional analysis program, Korean Nutrition Society, 2005) was used to analyze the nutrient intake. Based on nutritional intake data and clinical measures including blood pressure, blood lipids and blood glucose, nutrition consulting was conducted. Each educational session was carried out for 20 minutes and subjects received consulting 2 times on average. For educational tools, this study used the self-developed nutrition education leaflet.
Life style and nutrient intake analyses
To analyze life styles, this study asked subjects to fill out questionnaires based on the medical examination chart provided by the National Health Insurance during health check-up. The regularity of meals, drinking and smoking habits of subjects were included in the questionnaire. We used the CAN-Pro version 3.0 to analyze the average daily nutrient intake based on the meal journals recorded during the first examination.
Statistical analysis
This study used SPSS Statistic 18 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA) for statistical processing. This study used descriptive statistics of mean and standard deviation to analyze general characteristics, the non-parametric wilcoxon signed ranked test of the paired t-test was used to analyze clinical and biochemical measurements including blood pressure, blood lipids, blood glucose, and liver function indicators. This study classified body mass index (BMI) according to normal weight (BMI < 23.0 kg/m2), overweight (23.0 ≤ BMI < 25.0 kg/m2) and obese (BMI ≥ 25.0 kg/m2) and used the non-sequential variable with the non-parametric method for analysis. Spearman's correlation was used to verify factors that influence clinical indicators related with metabolic syndrome in the significance level of p < 0.05.
Results
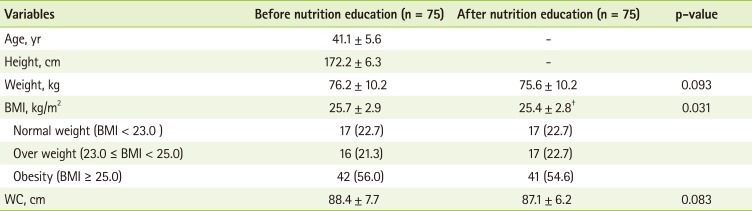
General characteristics and anthropometric measurement
The general characteristics of research subjects are presented in Table 1. All subjects were male and the average age was analyzed to be 41. The height was measured as 172.2 cm. The weight was reduced from 76.2 kg to 75.6 kg after nutrition education. The body mass index was significantly reduced from 25.7 kg/m2 to 25.4 kg/m2 after nutrition education (p < 0.05). The waist circumference of subjects was reduced from 88.4 cm to 87.1 cm after nutrition education, which was lower than the 90 cm, the diagnostic standard component of metabolic syndrome as established by NCEP ATPIII (Executive Summary of the Third Report of The National Cholesterol Education Program, 2001).
Table 1.
General characteristic and anthropometric parameters of subjects before and after nutrition education*
BMI: body mass index, WC: waist circumference.
*Values are presented as mean ± SD or N (%); †Significantly different at a p < 0.05.
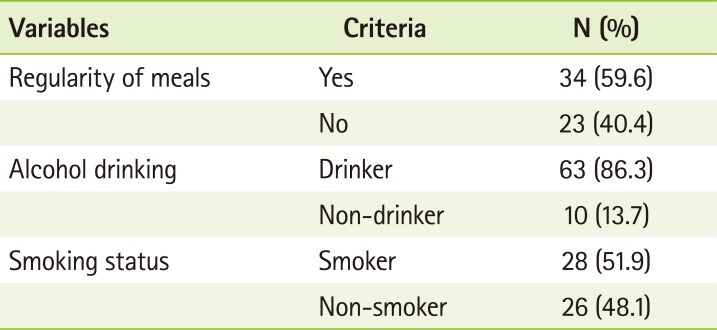
Characteristics of life style
The life study of study subjects are presented in Table 2. The proportion of study subjects having 3 meals a day with regularity was 59.6%, whereas the remaining 40.4% answered that they did not regularly eat 3 meals a day. Regular drinkers were 86.3% of the study subjects and only 13.7% did not drink at all. Smokers were 51.9% of the subjects whereas 48.1% were non-smokers.
Table 2.
Life style and dietary habits*
*Values are presented as N (%).
Changes in blood pressure before and after nutrition education
The changes in blood pressure before and after nutrition education are presented in Table 3. The systolic blood pressure was reduced from 120.0 mmHg to 117.8 mmHg after nutrition education. The diastolic blood pressure was also reduced from 79.1 mmHg to 77.0 mmHg after nutrition education, however, no significant difference was found.
Table 3.
Changes in blood pressure before and after nutrition education*
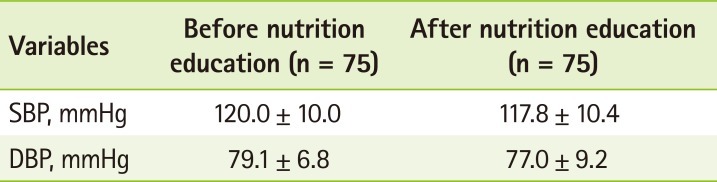
SBP: systolic blood pressure, DBP: diastolic blood pressure.
*Values are presented as mean ± SD.
Changes in fasting blood sugar before and after nutrition education
The changes in fasting blood sugar, the diabetes indicator, before and after nutrition education, were presented in Table 4. Fasting blood sugar was significantly reduced from 100.5 mg/dl to 97.0 mg/dL after nutrition education (p < 0.01). This shows that the workplace-visiting nutrition education of hospital clinical nutritionists is effective in reducing the blood sugar of subjects with impaired fasting blood sugar.
Table 4.
Changes in blood glucose concentration before and after nutrition education*
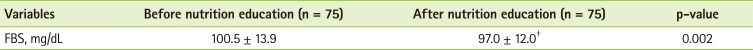
FBS: fasting blood sugar.
*Values are presented as mean ± SD; †Significantly different at a p < 0.01.
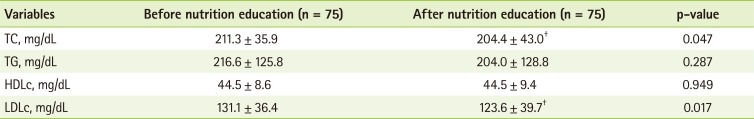
Changes in serum lipid before and after nutrition education
The changes in serum lipid, the indicator for dyslipidemia, before and after nutrition education are presented in Table 5. The total cholesterol was significantly reduced from 211.3 mg/dL to 204.4 mg/dL (p < 0.05), whereas triglycerides was reduced from 216.6 mg/dL to 204.0 mg/dL after nutrition education without showing a significant difference. High density lipoprotein cholesterol was similar before and after nutrition education, whereas low density lipoprotein cholesterol was significantly reduced from 131.1 mg/dL to 123.6 mg/dL after nutrition education (p < 0.05).
Table 5.
Changes in serum lipid profile before and after nutrition education*
TC: total cholesterol, TG: triglycerides, HDLc: high density lipoprotein cholesterol, LDLc: low density lipoprotein cholesterol.
*Values are presented as mean ± SD; †Significantly different at a p<0.05.
Changes in liver function indicators before and after nutrition education
The changes in liver function indicators of subjects are presented in Table 6. As indicators for liver function, serum glutamic oxalacetic transaminase, serum glutamic pyruvic transaminase and r-GTP were reduced after nutrition education, but did not present significant difference.
Table 6.
Changes in liver function indicators before and after nutrition education*
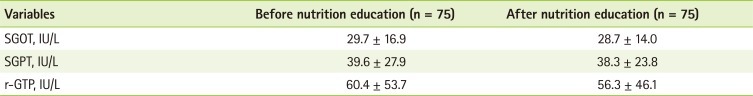
SGOT: serum glutamic oxaloacetic transaminase, SGPT: serum glutamic pyruvic transaminase, r-GTP: r-glutamyl transpeptidase.
*Values are presented as mean ± SD.
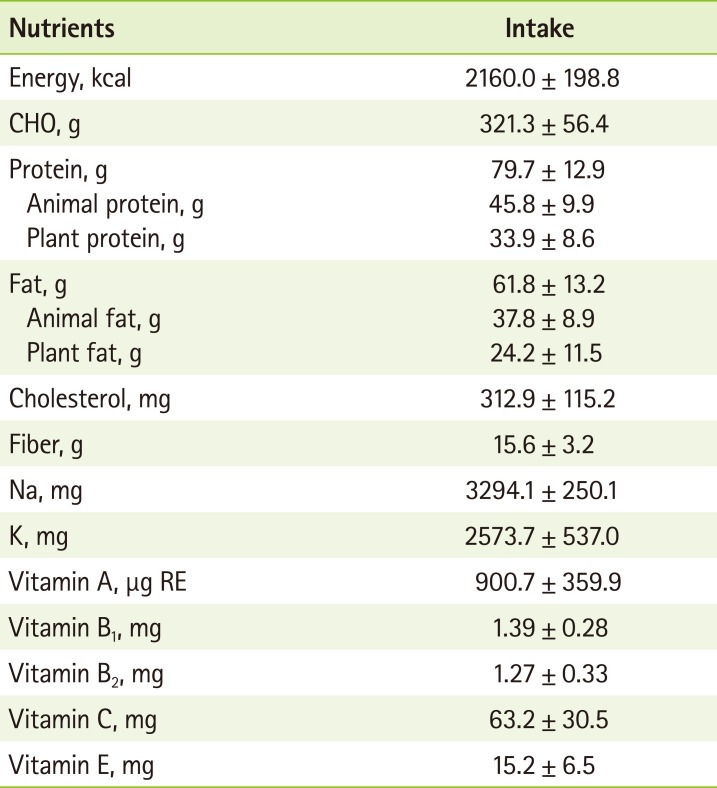
Nutrient intake analysis
The nutrient intake of study subjects is presented in Table 7. The meal intake survey presented that subjects consumed 2,160 kcal on average, which is 90% of the nutrient intake standards for men aged between 30-49. Subjects consumed 321.3 g of carbohydrate (60% of total calories) and 79.7 g of protein (15% of total calories), consisting of 57% animal protein and 43% of plant protein. The average fat consumption was 61.8 g, which is 26% of total calories, thus presenting that subjects ingested 15-25% more than the nutrient intake standard of Koreans. Subjects consumed 312.9 mg of cholesterol, which exceeded the 200 mg, the recommended quantitiy for dyslipidemia patients, and 15.6 g of dietary fiber per day, which was 25 g less than the daily nutrient intake standard for Koreans. Thus, the nutrition education placed emphasis on the increased intake of vegetables (especially seaweed) for dietary fiber intake. Dyslipidemia patients were educated to increase the intake of vegetables and fruits especially to increase the consumption of water-soluble dietary fiber. Subjects consumed 900.7 µg RE of vitamin A, which exceeds the recommended intake for men aged between 30-49 (750 µg RE). The intake of vitamins B1, B2, E met the nutrient intake standards of Koreans. However, subjects consumed 63.2 mg of vitamins C, which is less than the recommended intake quantity of men aged between 30-49 (100 mg). This is stipulated to be related with the low dietary fiber intake. Study subjects consumed appropriate level of calorie/protein, higher level of fat/cholesterol and lower level of dietary fiber.
Table 7.
Average daily nutrients intake*
CHO: carbohydrates.
*Values are presented as mean ± SD or N (%).
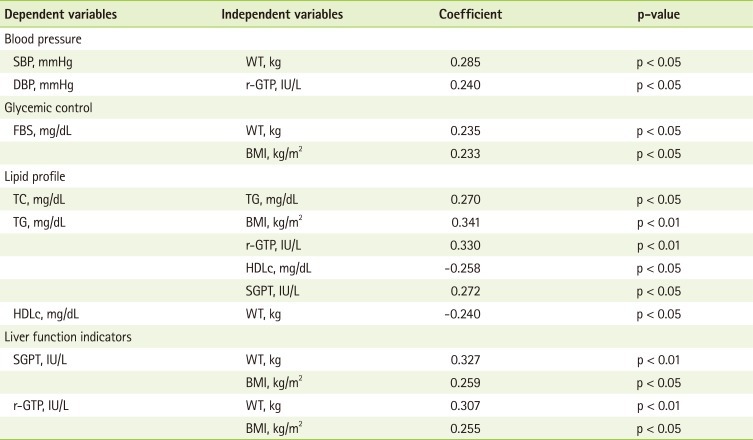
Correlation of factors that influence clinical indicators related with metabolic syndrome after nutrition education
The factors that influence clinical indicators related with metabolic syndrome after nutrition education are presented in Table 8. Results showed that systolic blood pressure presented a significantly positive correlation with weight (p < 0.05), whereas diastolic blood pressure presented a significantly positive correlation with r-GTP (p < 0.05). Fasting blood sugar presented a significantly positive correlation with weight (p < 0.05) and body mass index (p < 0.05). As a clinical indicator for dyslipidemia, total cholesterol presented a significantly positive correlation with triglycerides (p < 0.05). Triglycerides presented a significantly positive correlation with body mass index (p<0.01), serum glutamic pyruvic transaminase (p<0.05), and r-GTP (p < 0.01). On the other hand, blood total cholesterol showed significantly negative correlation with high density lipoprotein cholesterol (p < 0.05). High density lipoprotein cholesterol presented a significantly negative correlation with weight (p < 0.05). As an indicator for liver function, serum glutamic pyruvic transaminase presented a significantly positive correlation with weight (p < 0.01) and body mass index (p < 0.05) whereas r-GTP also presented a significantly positive correlation with weight (p < 0.01) and body mass index (p < 0.05). These results show that among subjects with one or more of metabolic syndrome criteria, it is important to provide specified nutrition education based on risk factors related to clinical and biochemical parameters.
Table 8.
Correlation coefficient between clinical indicators and WT, r-GTP, BMI, TG, HDLc, SGPT after nutrition education*
SBP: systolic blood pressure, DBP: diastolic blood pressure, WT: weight, r-GTP: r-glutamyl transpeptidase, FBS: fasting blood sugar, BMI: body mass index, TC: total cholesterol, TG: triglycerides, HDLc: high density lipoprotein cholesterol, SGPT: serum glutamic pyruvic transaminase.
*Analyzed with Spearman's correlation coefficient.
Discussion
Office workers frequently drink, dine out, miss breakfast, lack exercise and experience nutritional imbalance. The life style is formed based on such experiences cause chronic degenerative diseases including metabolic syndrome and cardiovascular diseases. during middle and old age. Nutrition education helps subjects to correct life styles to lower metabolic syndromes. Hereupon, among subjects that presented abnormal clinical findings in the health examination and comprehensive medical checkup implemented by the National Health Insurance, the workplace-visiting nutrition eduction was implemented for 75 male office workers, and the effectiveness was analyzed. We used self-directed coaching method based on metabolic syndrome components that each study subjects possess.
By analyzing the changes in anthropometric measurement, clinical and biochemical measurement before and after the 4-month nutrition education program, it is concluded that the body mass index (p < 0.05), fasting blood sugar (p < 0.01), total cholesterol (p < 0.05) and low density lipoprotein cholesterol (p < 0.05) were significantly reduced. The significant decrease in fasting blood sugar (p < 0.01) was similar to the study of Kim [19], which emphasized the significance of nutrition education and exercise in regulating blood sugar of diabetes patients. Decreases in serum lipid and total cholesterol is viewed as the effect produced by weight loss which is accomplished by nutrition education. The study conducted by Briley et al. [20] also indicated the decrease in weight and total cholesterol after nutrition education, and the study conducted by Epstein et al. [21] and Choi [22] also reported that weight loss can reduce total blood cholesterol and triglycerides concentration. Summer et al. [23] reported that the nutrition education provided for office workers was effective in reducing the weight and cholesterol standard of subjects. Low density lipoprotein cholesterol was also significantly reduced after nutrition education (p < 0.05), which is viewed to be related with weight loss.
The nutrient intake of subjects was presented as follows: calories 2160 kcal, carbohydrate 321.3 g, protein 79.7 g, fat 61.8 g. The ratio of carbohydrate, protein and fat to total calories was presented as 60%:15%:26%, respectively. When compared with the nutrient intake standard of Koreans (55-70%:7-20%:15-25%), subjects presented a higher fat ratio. Hunink et al. [24] reported that the increase in total fat intake increased the synthesis of chylomicron and very low density lipoprotein (VLDL) to increase the concentration of blood triglycerides and cholesterol. Subjects ingested 312.9 mg of total cholesterol, which is higher than the recommended intake for dyslipidemia patients (200 mg). The 2001 NCEP (National Cholesterol Education Program) reported that increased cholesterol intake in meals presented increased concentration of total cholesterol and low density lipoprotein cholesterol [25]. As results showed that subjects ingested 15.6 g of dietary fiber per day, which was 25 g less than the daily nutrient intake standard for Koreans [26], education to increase the intake of dietary fiber was also carried out during the nutrition education. The results of factor analysis, which influence clinical indicators related with metabolic syndrome after needs of providing, raise the needs of providing education on weight loss for subjecits with metabolic disorders.
However, the subjects of this study experienced difficulties in writing the meal journal during the basic survey. Requesting male office workers who possess low knowledge of food to write time-consuming meal journals can reduce the participation rate. In this regard, it is urgent to develop a program in consideration of the unique characteristics of subjects to help subjects to write easily and to view results immediately. Furthermore, to efficiently implement nutrition education to a large number of subjects in a fixed period of time, it is necessary to develop various nutrition education and assessment programs of outstanding quality and content to help subjects take interest and stay motivated. In addition, as the 4-month nutrition education effectively reduced body mass index, fasting blood sugar, total cholesterol and low density lipoprotein cholesterol, the nutrition education was verified to be effective in that experienced clinical nutritionists actively encouraged subjects through the self-directed coaching method. Thus, it can be stipulated that a customized nutrition education program must be implemented to reduce medical costs, improve work efficiency and enhance quality of life in the long run through enhanced health of subjects.
Conclusion
The results of this study verified that the visiting nutrition education provided to male workers through the individual-based, self-directed was effective in reducing body mass index and improving clinical quality index. In Korea, nutrition education and consulting have been mostly provided in hospitals. However, when considering the fact that the health of workplace workers, which compose a very large group, is directly connected with their work efficiency, it is important to achieve nutrition management through systematic education or consulting. Such nutrition education and consulting programs can be efficiently implemented by nutritionists within the workplace and thus requires the development of a program suitable for the workplace and the regular implementation of the program. However, as professional clinical nutritionists are absent in most work places, it is possible to consider the method of connecting hospitals with health check-up programs of work places. As health care professionals, nutritionists will actively contribute to the improvement of national health.
References
- 1.Jung MS, Bae JH, Kim YH. Relationships between dietary intake and serum lipid profile of subjects who visited health promotion center. J Korean Soc Food Sci Nutr. 2008;37:1583–1588. [Google Scholar]
- 2.Ministry of Health and Welfare. Report on 2005 National health and nutrition survey. Ministry of Health and Welfare; 2006. [Google Scholar]
- 3.Van Gaal L, Vansant G, Van Campenhout G, Lepoutre L, De Leeuw I. Apolipoprotein concentrations in obese subjects with upper and lower body fat mass distribution. Int J Obes. 1989;13:255–263. [PubMed] [Google Scholar]
- 4.Wilson PW, Kannel WB, Silbershatz H, D'Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159:1104–1109. doi: 10.1001/archinte.159.10.1104. [DOI] [PubMed] [Google Scholar]
- 5.Marmott MG, Poulter NR. Primary prevention of stroke. Lancet. 1992;339:344–347. doi: 10.1016/0140-6736(92)91659-v. [DOI] [PubMed] [Google Scholar]
- 6.Park HD, Kim EJ, Hwang MO, Paek YM, Choi TI, Park YK. Effets of Workplace nutrition education program tailored for the individual chronic disease risks. Korean J Nutr. 2010;43:246–259. [Google Scholar]
- 7.Lee SY, Suh I. Relationship of health status and health practices. Korean J Epidemiol. 1995;17:48–63. [Google Scholar]
- 8.Choi MK, Kim JM, Kim JK. A study on the dietary habit and health of office workers in Seoul. Korean J Food Cult. 2003;18:45–55. [Google Scholar]
- 9.Sim KS, Lee KH. The effect of nutrition education on nutrition knowledge and health improvement in dyslipidemic industrial employees. J Korean Diet Assoc. 2012;18:43–58. [Google Scholar]
- 10.Jang JH, Cho SH. Effectiveness of worksite nutrition counselling for hyperlipidemic employees in Kyung-buk area. J Korean Diet Assoc. 1999;5:1–9. [Google Scholar]
- 11.Lee MS, Kang HJ, Oh HS, Paek YM, Chou RW, Park YK, Choi TI. Effects of worksite nutrition counseling for health promotion; Twelve-weeks of nutrition counseling has positive effect on metabolic syndrome risk factors in male workers. Korean J Community Nutr. 2008;13:46–61. [Google Scholar]
- 12.Son SM, Kim HJ. Effect of 12-week low calorie diet and behavior modification on the anthropometric indices and biochemical nutritional status of obese woman. Korean J Community Nutr. 2005;10:525–535. [Google Scholar]
- 13.Cho KO, Jeong SY. The effect of regular dietary habits on obesity indices and nutrition intakes in adult males. J Korean Diet Assoc. 2007;13:114–122. [Google Scholar]
- 14.Moon HK, Lee HJ, Park Y. Comparison of health status and dietary habits by percent body fat (PBF) changes for adult women in the weight control program by the community health center. Korean J Community Nutr. 2007;12:477–488. [Google Scholar]
- 15.Lee YA, Kim KN, Chang N. The effect of nutrition education on weight control and diet quality in middle-aged women. Korean J Nutr. 2008;41:54–64. [Google Scholar]
- 16.Woo MK, Jegal SA, Kim SA. Development and evaluation of nutrition education program for middle agged men at worksite. Korean J Community Nutr. 1998;3:261–272. [Google Scholar]
- 17.Ministry of Health and Welfare. Report on 2007 National health and nutrition survey. Seoul: Ministry of Health and Welfare; 2008. pp. 56–57. [Google Scholar]
- 18.Bae NK, Kim KH, Kwon IS, Cho YC. Changes in prevalence of obesity for 10 years (1997~2007) and its related factors in health checkup examinees. J Korean Academia-Industrial Cooperation. 2009;10:1091–1099. [Google Scholar]
- 19.Kim HI. The effect of 12 weeks aerobic exercise on body composition blood glucose and lipoprotein in middle-age, menopause and elderly women. J Korea Sport Res. 2004;15:3–12. [Google Scholar]
- 20.Briley ME, Montgomery DH, Blewett J. Worksite nutrition education can lower total cholesterol levels and promote weight loss among police department employees. J Am Diet Assoc. 1992;92:1382–1384. [PubMed] [Google Scholar]
- 21.Epstein LH, Wing RR, Koeske R, Valoski A. Long term effects of family-based treatment of childhood obesity. J Consult Clin Psychol. 1987;55:91–95. doi: 10.1037//0022-006x.55.1.91. [DOI] [PubMed] [Google Scholar]
- 22.Choi MJ. Relations of life style, nutrient intake, and blood lipids in middle-aged men with borderline hyperlipidemia. Korean J Community Nutr. 2005;10:281–289. [Google Scholar]
- 23.Summer SK, Schiller EL, Marr ER, Thompson DA. A weight control and nutrition education program for insurance company employees. J Nutr Educ. 1986;18:S60–S62. [Google Scholar]
- 24.Hunink MG, Goldman L, Tosteson AN, Mittleman MA, Goldman PA, Williams LW, Tsevat J, Weinstein MC. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535–542. [PubMed] [Google Scholar]
- 25.National Cholesterol Education Program. 2001. Third report of the expert panel on detection evaluation and treatment of high blood cholesterol in adults. Bethesda: Maryland: 2001. [Google Scholar]
- 26.The Korean Nutrition Society. Dietary Reference Intakes for Koreans. Seoul: Hanarum Publishers; 2010. [Google Scholar]