Abstract
Objective
Although antidepressants are an effective treatment for later-life depression, older patients often choose not to initiate or to discontinue medication treatment prematurely. While racial differences in depression treatment preferences have been reported, little is known about racial differences in antidepressant medication adherence among older patients.
Design
Prospective, observational study comparing antidepressant adherence for older African-American and white primary care patients.
Participants
One hundred and eighty-eight subjects aged 60 and older, diagnosed with clinically significant depression with a new recommendation for antidepressant treatment by their primary care physician.
Measurement
Study participants were assessed at study entry and at four-month follow-up (encompassing the acute treatment phase). Depression medication adherence was based on a well-validated self-report measure.
Results
At four-month follow-up, 61.2% of subjects reported that they were adherent to their antidepressant medication. In unadjusted and two of the three adjusted analyses, African-American subjects (n=82) had significantly lower rates of four-month antidepressant adherence than white subjects (n=106). African-American females had the lowest adherence rates (44.4%) followed by African-American males (56.8%), white males (65.3%) and white females (73.7%). In logistic regression models controlling for demographic, illness, and functional status variables, significant differences persisted between African-American women and white women in reported four-month antidepressant adherence (OR 3.58, 95% CI 1.27-10.07, Wald Chi-square =2.42, df=1, p<0.02).
Conclusions
The results demonstrate racial and gender differences in antidepressant adherence in older adults. Depression treatment interventions for the older adults should take into account the potential impact of race and gender on adherence to prescribed medications.
Introduction
A large proportion of the older adult population experiences depression, which can have serious, negative consequences in terms of morbidity [1], mortality [2-6], and quality of life [7-9]. Depression among older adults is also associated with excess utilization of health care, increased nursing home placement, greater burden to medical care providers, and higher annual health care costs [10-14]. Of gravest concern, depression is the condition most commonly associated with suicide in older adults [15].
Primary care physicians provide the majority of treatment for later-life depressive illness [14, 16]. Antidepressant treatment is often the evidence-based choice for older adults seen in primary care settings, as psychotherapy may not be readily available, accessible, or preferred by older adults [17]. In recent years, with the availability of selective serotonin-reuptake inhibitors (SSRIs), depression screening initiatives, and collaborative care interventions, advances have been made in ‘first-generation problems’ in depression diagnosis and treatment [18], resulting in improved rates of detection and increased treatment initiation for later-life depression in primary care.
Although antidepressants are an effective treatment for geriatric depression, older patients may choose not to take prescribed antidepressants or they may discontinue treatment prematurely. Non-adherence is common, with estimates ranging from 40% to 75% [19]. Thus, even with successful screening and diagnosis of late-life depression in health care settings, a second-generation problem of a “treatment gap”, has emerged. Poor depression treatment adherence may limit the extent to which older patients with depression realize the benefits of efficacious treatment options.
Given the limited amount of research regarding geriatric issues in general in African Americans [20], there is an even greater paucity of information on depression medication adherence rates in this population. Prior studies indicate that African-American older adults have lower rates of depression diagnoses in clinical settings than older white patients [21-24], and results from qualitative studies of mixed-age samples suggest that African-American patients may find antidepressant treatment less acceptable than white patients [25]. When African Americans do seek specialty mental health care, they have fewer appointments and are more likely than white patients to terminate treatment prematurely [26, 27]. A prior study of depressed and non-depressed community older adults also found that African-American elders were less likely than their white counterparts to be taking antidepressants [28]. However, it was unclear if this treatment gap resulted from providers being less likely to diagnose depression or prescribe antidepressants to African-American patients or to patients having fewer depressive symptoms or lower rates of medication adherence. To our knowledge, no prior studies have examined whether adherence rates differ between African-American and white older adults who have been diagnosed with depression and prescribed an antidepressant.
A further understanding of adherence among both African-American and white older patients with depression is critical to designing tailored and culturally-sensitive interventions to improve overall depression care in the elderly. Given that older adults and particularly African Americans are more likely to seek mental health treatment in primary care rather than mental health settings, it is important to examine adherence to depression treatments in primary care [29-31]. In this study, we followed older African-American and white patients whose primary care physicians (PCPs) had diagnosed depression and recommended antidepressant treatment to examine their rates of adherence at the end of the acute treatment period (four months). Based upon prior studies finding racial differences in rates of treatment and acceptability of antidepressants, we hypothesized that older African-American patients would report significantly lower rates of four-month adherence than older white patients.
Methods
This study received approval from the University of Michigan Medical School Institutional Review Board. Study participants were recruited between March 2007 and March 2010 from 13 primary care clinics located in Ann Arbor, Michigan and surrounding communities. Potentially eligible subjects were older adults (aged 60 years and over) with diagnoses of clinically significant depression seen in participating primary care clinics and newly recommended antidepressant treatment by their PCPs. Subjects were either referred to the study by their PCPs directly or were identified through the electronic medical record for study recruitment. Our methods for identifying potential subjects through the electronic medical record have been previously reported [32]. After obtaining PCP consent, subjects were contacted by study staff and recruited via mail and telephone.
Clinically significant depression was defined as having: 1) a new prescription from the primary care physician (encompassing both newly diagnosed patients as well as patients with recurrent depression receiving a new antidepressant prescription for a new depressive episode and 2) a score of 5 or higher on the Geriatric Depression Scale-Short Form [33]; patients not meeting these criteria were excluded to ensure a more homogeneous sample of depressed elders. Also excluded were patients who had active suicidal ideation, psychosis, a history of mania, cognitive impairment (≥3 errors on the Six Item Screener [34]), were a race other than white or African American, or were unable to communicate in English.
Research Assessments
Research assessments were conducted with participants at study entry and at 4-month follow-up. A four-month follow-up was chosen because the early phase of treatment is a particularly critical time period with an increased risk of treatment drop-out, medication discontinuation [35, 36], and vulnerability to suicide [37]. Assessments were conducted by trained research assistants and all participants provided written informed consent prior to study participation.
A structured interview at baseline included assessment of: 1) demographic variables including age, race, gender, marital status, and educational level); 2) illness variables including past antidepressant use, number of prescribed medications, physical health status (SF-12 physical component scale), mental health status (SF-12 mental component scale) [38], comorbid anxiety (anxiety items of the Hospital Anxiety and Depression Scale (HADS-A) [39]), somatic anxiety (Anxiety Sensitivity Index-Revised ASI-R; subscales pertaining to beliefs and fears about somatic sensations) [40], further assessment of depression using the Patient Health Questionnaire depression scale (PHQ-9) [41]; and 3) functional assessment including instrumental [42] and basic (Katz ADL) [43] activities of daily living and executive function (Wechsler Letter-Number Sequencing or LNS subscale) [44]
At four-month follow-up, adherence was measured using the validated self-report adherence question from the Brief Medication Questionnaire [45] that asks the subject about how consistently they took their medication on a daily basis in the week prior to the interview. This item has been found to be significantly correlated with pharmacy refill records [46]. Consistent with prior studies [47] that consider an antidepressant medication possession ratio (MPR) of less than 80% to be inadequate, we rated those as missing 2 or more daily doses in a given week as non-adherent. Those subjects who chose never to initiate the antidepressant medication by not filling the prescription or not ever taking the medication were also recorded as non-adherent.
Statistical Analysis
Four month adherence was calculated by race, by gender, and by race and gender subgroups. Although our primary interest was in racial differences in adherence, we also performed exploratory analyses to assess adherence differences by the four distinct race by gender subgroups because preliminary focus group data suggested adherence differences between white and African-American women with depression. Logistic regression analysis was used to compare four-month adherence between racial groups as well as across race by gender subgroups, after adjusting for baseline characteristics. Baseline covariates were entered hierarchically in a predefined order of variable sets (blocks) in order to examine the influence on adherence of each potentially explanatory set of covariates in a sequential way. The order of entry for blocks was determined so that the potentially confounding contextual variables were entered first in order to control for their effects. Based on this reasoning, demographic characteristics were entered first, followed by treatment and illness burden variables, and then functional status variables. Within each block, baseline covariates were assessed for multi-collinearity, and highly collinear variables were not included together. No pairs of covariates had a correlation coefficient higher than 0.5 or lower than -0.5. Because 15% of subjects were missing data for at least one covariate such as income, we applied a multiple imputation strategy using the MI procedure in SAS (SAS Institute Inc., Cary, NC) under a multivariate normal model that included all covariates as well as adherence. The logistic regression estimates were pooled across five imputation samples using Rubin’s method [48].
Results
Sample Characteristics
Six hundred forty-one patients were found to be potentially eligible for the study based upon age and a new antidepressant prescription in a primary care clinic. We received provider permission and were able to contact 448 (82%) of these potential participants. Provider reasons for not referring patients to the study included terminal medical conditions, severe personality pathology, dementia, and aphasia. Three hundred three patients completed screening, and of these 211 were found to be eligible for study participation. Of the eligible patients, 94% (n=198) agreed to study participation and provided informed consent and completed baseline assessments (see Consort chart in Figure 1).
Figure 1.
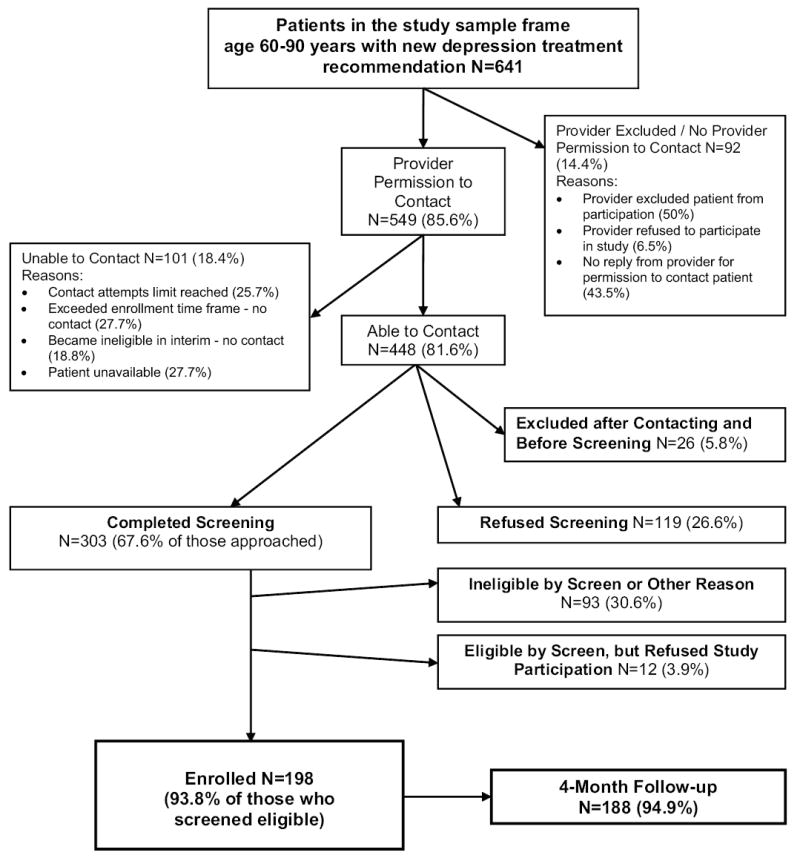
Study Flowchart
Table 1 illustrates demographic, illness, and functional variables for the study sample that completed four-month follow up (n=188). Subjects lost for follow-up (n=10) did not differ significantly from those who completed the follow up assessments by race (Chi-square=2.17, df=1, p=0.14) or gender (Chi-square=0.13, df=1, p=0.72). Of subjects who completed the four-month follow-up interview, 43.6% were African American (n=82) and 56.4% were white (n=106). Approximately 54% of the study participants were women. The mean age for the study completers was 67.3 years, with African-American males being somewhat younger than the other race/gender combinations. Approximately 62% of the sample had some college education, with white females having the highest rate of college education (70%). Almost half of the study participants were married or had a significant other, with African-American women having the lowest rate (31%) of these relationships.
Table 1.
Subjects’ characteristics at baseline
| African-American | White | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Female (N=45) | Male (N=37) | Total (N=82) | Female (N=57) | Male (N=49) | Total (N=106) | |
| Age* | ||||||
| 60-64 | 47% | 68% | 56% | 44% | 47% | 45% |
| 65-74 | 42% | 22% | 33% | 35% | 27% | 31% |
| 75-90 | 11% | 11% | 11% | 21% | 27% | 24% |
| Education | ||||||
| High school or below | 44% | 41% | 43% | 30% | 40% | 34% |
| Some college or above | 56% | 59% | 57% | 70% | 60% | 66% |
| Marital Status* | ||||||
| With partner/spouse | 31% | 49% | 39% | 49% | 65% | 57% |
| Without partner/spouse | 69% | 51% | 61% | 51% | 35% | 43% |
| With prior depression treatment* | 63% | 51% | 58% | 84% | 69% | 77% |
| Mean | ||||||
| Number of prescribed medications | 4.3 | 4.0 | 4.2 | 4.2 | 4.5 | 4.3 |
| Physical component summary of SF-12 (PCS) | 36.1 | 36.5 | 36.3 | 37.7 | 38.7 | 38.2 |
| Mental component summary of SF-12 (MCS)* | 36.2 | 35.3 | 35.8 | 38.9 | 39.0 | 39.0 |
| Patient Health Questionnaire (PHQ-9)* | 13.1 | 13.0 | 13.0 | 11.4 | 11.0 | 11.2 |
| Hospital anxiety depression scale, anxiety subscale (HADS-A) | 8.8 | 9.9 | 9.3 | 9.5 | 8.5 | 9.1 |
| Anxiety sensitivity index (ASI)* | 59.8 | 58.8 | 59.3 | 47.1 | 44.2 | 45.8 |
| Katz index of independence in activities of daily living (KATZ Total) | 5.6 | 5.6 | 5.6 | 5.7 | 5.7 | 5.7 |
| Instrumental activities of daily living scale (IADL Total) | 6.8 | 7.3 | 7.1 | 7.5 | 7.3 | 7.4 |
| Weschler LNS* | 6.8 | 7.8 | 7.3 | 10.4 | 8.7 | 9.6 |
p<0.05 for comparison between African-Americans and whites.
Over 60% of study completers reported having at least one episode of antidepressant treatment prior to the study, with white females having the highest rate (84%) of prior antidepressant treatment. The average number of prescribed medications and physical health status were similar between study subgroups based on race and race/gender. The overall average baseline PHQ was 12.0+5.7, with African-American subjects showing slightly higher levels of depression and lower self-rated mental health status (MCS score) than white subjects. While symptoms of anxiety as reflected on the Hospital Anxiety Depression Scale (HADS-A) were similar between study subgroups, rates of somatic anxiety as determined by the anxiety sensitivity index (ASI-R) were significantly higher in African-American subjects.
Finally, there were no differences found in baseline function with the exception of executive function; here, white subjects had higher scores (reflecting less impairment).
Four-month Adherence
At the four-month follow-up assessment, we found that 61.2% of the overall study sample had adequate adherence based on missing fewer than 2 daily doses in a week. In unadjusted analyses, African-American subjects had significantly lower adherence than white subjects (50.0% vs. 69.8%, Chi-square=7.64, df=1, p<0.01, results not shown). Exploratory analyses across the race by gender subgroups showed that African-American females had the lowest adherence (44.4%) followed by African-American males (56.8%), white males (65.3%) and white females (73.7%). Using African-American females as the reference group, adherence was highest in white females (OR 3.50, 95% CI 1.52-8.05, Wald Chi-square=8.70, df=1, p=0.003), followed by white males (OR 2.35, 95% CI 1.02-5.41, Wald Chi-square=4.07, df=1, p= 0.04) and African-African males (OR 1.64, 95% CI 0.68-3.94, Wald Chi-square=1.22, df=1, p=0.27).
Logistic regression models (Table 2) showed that significant differences in reported adherence between white and African-American subjects remained when controlling for demographic characteristics alone, and when controlling for demographic variables as well as prior treatment and illness burden. Race was no longer significantly associated with adherence when also adjusted for functional status variables.
Table 2.
Medication adherence at four-month follow-up.
| Adjusted for demographic characteristics1 | Adjusted for demographic characteristics and illness burden2 | Adjusted for demographic characteristics, illness burden, and functional status3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Group Comparison | Odds Ratio | 95%CI | Wald Test | P value | OddsRatio | 95%CI | Wald Test | p value | Odds Ratio | 95%CI | Wald Test | p value |
| African-American | 1.0 | -- | -- | -- | 1.0 | -- | -- | -- | 1.0 | -- | -- | -- |
| White | 2.47 | (1.32-- 4.62) | 2.82 | 0.0048 | 2.12 | (1.05-- 4.32) | 2.08 | 0.0372 | 2.02 | (0.95-- 4.30) | 1.82 | 0.0685 |
|
| ||||||||||||
| African-American female | 1.0 | -- | -- | -- | 1.0 | -- | -- | -- | 1.0 | -- | -- | -- |
| African-American male | 1.64 | (0.67-- 4.02) | 1.08 | 0.2807 | 1.76 | (0.69-- 4.53) | 1.18 | 0.2393 | 2.15 | (0.79-- 5.81) | 1.50 | 0.1329 |
| White male | 2.55 | (1.06-- 6.13) | 2.09 | 0.0368 | 2.31 | (0.89-- 6.00) | 1.72 | 0.0860 | 2.48 | (0.90-- 6.85) | 1.75 | 0.0805 |
| White female | 3.69 | (1.57-- 8.67) | 2.99 | 0.0028 | 3.26 | (1.27-- 8.33) | 2.46 | 0.0138 | 3.58 | (1.27-10.07) | 2.42 | 0.0157 |
adjusted for demographic variables of age, marital status, and education.
adjusted for demographic variables and illness burden variables of prior treatment of depression, number of prescribed medications, physical component summary score (PCS), mental component summary score (MCS), depression score on patient health questionnaire (PHQ total), hospital anxiety depression score (HADS total), and anxiety sensitivity index (ASI total).
adjusted for demographic variables, illness burden variables, and functional status variables of Katz index of independence in activities of daily living (KATZ total), instrumental activities of daily living (IADL total), and Weschler memory scale.
While we tested for a race by sex interaction and did not find it to be statistically significant (likelihood ratio test Chi-square statistic = 2.69, df=1, p = 0.10), because adherence differed significantly between race by gender subgroups, we constructed a number of models to further examine what factors might be contributing to the differences between subgroups. Here, we found the following significant differences in adherence rates between: 1) white and African-American female subjects, and between white male and African-American female subjects when controlling for demographic characteristics; 2) white and African-American female subjects when controlling for demographic characteristics, prior treatment and illness burden; and 3) white and African-American female subjects when controlling for demographic characteristics, prior treatment, illness burden, and functional status (Table 2). Thus, adequate adherence was significantly higher for white females compared with African-American females even after adjusting for all potential baseline explanatory variables.
Discussion
In this study, we followed older African-American and white subjects with depression who were prescribed antidepressant medication treatment in primary care, examining their rates of adherence at the end of the acute treatment period. Based upon prior studies finding racial differences in various components of depression care, we hypothesized that older African-American subjects would have significantly lower rates of four-month adherence than older white subjects. Consistent with prior work documented in the elderly [19], for the study population as a whole, we found that overall adherence was lower than optimal (approximately 60%). Older African-American adults had significantly lower rates of antidepressant adherence than white older adults in models adjusting for demographic characteristics and symptom variables, but not in models that also included functional status variables. In addition, older white women had the highest rates of adherence while older African-American women had the lowest, after controlling for baseline differences in a number of demographic, illness, and function variables. Controlling for such variables is a unique feature of this study, because such baseline differences are important potential confounders of the relationship between race and disparities in aspects of depression care.
In our overall study sample, approximately 40% of subjects were non-adherent to antidepressant treatment at four-month follow-up. Thus, while there is evidence that primary care providers are increasingly diagnosing later-life depression and recommending treatment for older patients [49, 50], there need to be greater efforts to ensure that patients actually initiate and continue appropriate care throughout the course of their depressive illness. Poor adherence to depression treatment is an important source of drug exposure variability but is often inadequately measured in research trials and clinical practice. In a number of cases, “treatment-resistant” depression may in fact represent undertreatment because of poor adherence [51]. Thus, even with successful screening and diagnosis in healthcare settings (such as that seen via dissemination of collaborative care interventions), treatment adherence represents an important “second-generation” problem that results in a large treatment gap for older adults.
To our knowledge, the current study is the first to demonstrate directly that African-American older adults have lower rates of depression medication treatment adherence than white older adults. In a prior study controlling for education and income, African-American older adults in the community were significantly less likely than white elderly to be taking SSRIs [28]. However, the methodology of this study, which included both depressed and non-depressed subjects did not allow the investigators to determine whether the differences in adherence rates by race were due to 1) lower diagnosis or prescription rates by providers, or 2) lower rates of initiation and adherence by African-American subjects. Another study using data from a collaborative care intervention (PROSPECT) found that non-White race was the factor most strongly associated with non-adherence to citalopram [52]. Finally, in a study comparing African-American (n=49) to Latino (n=52) subjects over the age of 55 who had been prescribed antidepressants in the prior year, Ayalon et al found that 52.6% of African-American subjects were non-adherent, similar to the number found in our study [53].
Interestingly, in the Ayalon et al study, the investigators divided adherence into “intentional” and “unintentional” categories and noted that 18% of the African-American sample were unintentionally non-adherent. Greater cognitive impairment was significantly predictive unintentional non-adherence in that study. In our sample, the baseline executive function of African-American subjects was measured to be significantly lower than white subjects; performance on the measure of executive function we used (Wechsler Letter Number Sequencing) has been shown to vary by level of educational attainment (which we did not measure) rather than years of education (which we did include) [54]. Once we controlled for baseline level of function (including executive function) as well as other variables including years of education, the difference in adherence between African-American and white subjects was no longer significant. Optimal adherence depends on patients taking the prescribed medication at the right time and in the correct manner [55]. Beyond working memory and encoding and storage of information, the organization and planning needed for medication adherence requires intact executive function. The results of our study may suggest that even in older adults without dementia, mild cognitive impairment may be a uniquely burdensome influence on adherence for some patients.
Marital status, prior depression treatment, and somatic anxiety also differed between African-American and white subjects in our study. African-American subjects were significantly less likely to be married than white subjects. To the extent that spouses may assist with adherence to depression treatment (e.g. via reminding or encouraging the individual to take medication), the lack of a partner in some subjects may have decreased adherence. Greater social support was found in one study to be associated with increased treatment adherence in older patients with depression [56]. African-American subjects in our study were also significantly less likely to have had prior depression treatment. Lack of familiarity with depression medications or possible side effect concerns could have influenced adherence behaviors. Finally, African-American subjects had significantly higher baseline ratings of somatic anxiety. Individuals with somatic anxiety may be hypervigilant regarding their bodily sensations, and overestimate the danger of medications or the severity of side effects [57]. Older patients with anxious depression frequently misattribute somatic symptoms of anxiety to adverse medication effects, contributing to both drop-out and poor response in antidepressant trials [58]. Additionally, older adults with anxiety/somatic focus may discount psychological explanations for psychiatric symptoms and refuse treatment [59]. Notably, however, racial differences in adherence rates persisted after controlling for marital status, prior depression treatment, and somatic anxiety.
After controlling for baseline demographic, clinical and functional variables, we no longer found significant racial differences in the overall study sample. However, differences did persist between African-American and white women. The relationship between race, gender and adherence is an intriguing issue that has received relatively little focus in the literature. Previous work describing greater rates of prior treatment and current antidepressant use in women rather than men may have come from predominately white samples. Thus, while conventional wisdom holds that women are more willing to engage in depression treatment than men, this may not be true across different racial and ethnic groups. In an exploratory analysis, we examined initiation (whether the patient started the antidepressant at all) separately from adherence. Here again, we found that African-American females had the lowest initiation rates as compared to the other study subjects.
Our results of lower adherence rates in African-American older adults, and particularly in African-American women, suggest the need for tailored depression care interventions that are sensitive to racial differences. While race and gender are not modifiable factors, some of the characteristics that are more often found in the African-American older adults in our study are clearly modifiable or amenable to adaptations in intervention strategies. For example, a patient who is unmarried may benefit from enhanced support in the early treatment phase more than a patient who has a spouse. A patient with significant somatic anxiety may need a treatment approach that includes psychoeducation to help distinguish underlying anxiety symptoms from drug side effects. Patients without prior treatment who are less familiar with depression medications also likely need more psychoeducation than those who have been previously treated. An individual with executive dysfunction could be aided by strategies to enhance adherence such as the use of pillboxes or use of newer computerized medication dispensing technologies. These types of tailored interventions should be feasible within primary care practices that have adopted Patient Centered Medical Home [60] principles to assist with the management of patients with chronic illness.
There are several potential limitations to the interpretation of our findings. The sample was drawn from a large number of primary care clinics in southeastern Michigan. It is possible that the results of our study may have been different if conducted in another geographic area. Additionally, we used a self-report measure to examine patient adherence. Although the self-report measure is a validated method, electronic monitoring or pill counts may have yielded different results.
These limitations notwithstanding, our study is one of the first to our knowledge to directly compare adherence behaviors in African-American and white older patients. Another notable strength of our study is that it focused specifically on patients who were diagnosed and treated for depression within primary care practices. As noted, primary care practices are the source of the majority of depression care for older adults [14-16].
In conclusion, our results provide support for racial and gender differences in adherence behaviors for depression medication treatment in the elderly. The choice of appropriate depression care interventions for the elderly population should take into account the potential impact of race and gender on adherence to prescribed medications.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health, 5R21MH073002. The funding organization had no role in any of the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors gratefully acknowledge the participating patients and physicians.
Appendix
Study Measures
Screening instruments
The sensitivity and specificity of the Six-item Screeneri is .89 and .88, with a cut-off of 3 errors.
The GDS-short form has been found to have a 92% sensitivity and an 81% specificity when using a cutoff score of 5 with older primary care patientsii.
Assessment instruments
The SF-12 is a shorter yet valid alternative to the SF-36; it contains two weighted summary scales—mental health and physical health; lower scores indicate more severe disabilityiii.
The Patient Health Questionnaire depression scale (PHQ-9iv) is a 9-item self-administered depression screening and diagnostic tool frequently used in primary care and other medical populations. The PHQ-9 is half the length of many other depression measures, has comparable sensitivity and specificity, and consists of the nine criteria on which the diagnosis of DSM-IV depressive disorders is based.
The Hospital Anxiety and Depression Scale, or HADSv was designed to provide a simple yet reliable tool for use in medical practice. The seven items comprising the anxiety subscale are relevant to generalized anxiety and are answered on a 4-point Likert scale (0-3, maximum score for each subscale 21), with higher scores indicating greater endorsement of symptoms.
The Anxiety Sensitivity Index-Revised (ASI-Rvi) was developed to measure anxiety-sensitivity, the fear of anxiety-related sensations based upon beliefs of their harmful consequences. The construct validity of anxiety sensitivity is supported by a large body of research documenting its role in the genesis of anxiety and panic. The ASI-R has been found to be highly internally consistent and composed of psychometrically acceptable items assessing the fears of somatic, social, and cognitive anxiety symptoms.
The Katz ADLvii tool assesses basic activities of daily living. Although no formal reliability and validity reports could be found in the literature, the tool is used extensively as a flag signaling functional capabilities of older adults in clinical and home environments.
The Lawton Instrumental Activities of Daily Living Scale (IADLviii) is a valid and reliable instrument to assess independent living skills. These skills are considered more complex than the basic activities of daily living as measured by the Katz ADL tool.
The Letter-Number Sequence (LNS) subtest of the WAIS-IIIix is a measure of executive function (working memory), in which subjects are verbally presented with a sequence of letters and numbers and then asked to reorganize the sequence (such that the letters are reported back first in alphabetical order followed by the numbers in numerical order). This task requires the subject to be able to hold all of the digits in memory while manipulating the order according to the rules. The LNS has high face validity; there is no minimum academic skill prerequisite other than knowing the numbers 1 through 9 and having a functional knowledge of the alphabet.
Footnotes
Callahan CM, et al: Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002;40:771-781
Lyness JM, et al. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med 1997;157(4):449-54.
Ware JE et al. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 1996;34(3):220-233.
Kroenke, K., et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 2001. 16(9): p. 606-13.
Zigmond, A.S. and R.P. Snaith, The hospital anxiety and depression scale. Acta Psychiatr Scand, 1983. 67(6): p. 361-70
Deacon, B.J., et al., The Anxiety Sensitivity Index - Revised: psychometric properties and factor structure in two nonclinical samples. Behaviour Research and Therapy, 2003. 41(12): p. 1427-1449.
Katz S, Down TD, Cash HR, et al: Progress in the development of an index of ADL. Gerontologist 1970;10:20-30
Lawton MP and Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969; 9:179-186.
Wechsler, D. (1997). Wechsler Adult Intelligence Scale–Third edition: Administration and scoring manual. San Antonio, TX:Harcourt Brace.
References
- 1.Sheeran T, et al. Does depression predict falls among home health patients? Using a clinical-research partnership to improve the quality of geriatric care. Home Healthc Nurse. 2004;22(6):384–9. doi: 10.1097/00004045-200406000-00007. quiz 390-1. [DOI] [PubMed] [Google Scholar]
- 2.Unutzer J, et al. Care for depression in HMO patients aged 65 and older. J Am Geriatr Soc. 2000;48(8):871–8. doi: 10.1111/j.1532-5415.2000.tb06882.x. [DOI] [PubMed] [Google Scholar]
- 3.Bruce ML, Leaf PJ. Psychiatric disorders and 15-month mortality in a community sample of older adults. Am J Public Health. 1989;79(6):727–30. doi: 10.2105/ajph.79.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallo JJ, et al. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. Am J Geriatr Psychiatry. 2005;13(9):748–55. doi: 10.1176/appi.ajgp.13.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallo JJ. in press. [Google Scholar]
- 6.Bruce ML, et al. Psychiatric status and 9-year mortality data in the New Haven Epidemiologic Catchment Area Study. Am J Psychiatry. 1994;151(5):716–21. doi: 10.1176/ajp.151.5.716. [DOI] [PubMed] [Google Scholar]
- 7.USDHHS. Mental Health: A Report of the Surgeon General. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; Rockville, MD: 1999. [Google Scholar]
- 8.Bruce ML, et al. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health. 1994;84(11):1796–9. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2008: Key Indicators of Well-Being. Washington, DC: 2008. [Google Scholar]
- 10.Abrams RC, et al. Predictors of self-neglect in community-dwelling elders. Am J Psychiatry. 2002;159(10):1724–30. doi: 10.1176/appi.ajp.159.10.1724. [DOI] [PubMed] [Google Scholar]
- 11.Sheline YI. High prevalence of physical illness in a geriatric psychiatric inpatient population. Gen Hosp Psychiatry. 1990;12(6):396–400. doi: 10.1016/0163-8343(90)90008-z. [DOI] [PubMed] [Google Scholar]
- 12.Unutzer J, et al. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. A 4-year prospective study. Jama. 1997;277(20):1618–23. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- 13.Druss BG, Rohrbaugh RM, Rosenheck RA. Depressive symptoms and health costs in older medical patients. Am J Psychiatry. 1999;156(3):477–9. doi: 10.1176/ajp.156.3.477. [DOI] [PubMed] [Google Scholar]
- 14.Luber MP, et al. Depression and service utilization in elderly primary care patients. Am J Geriatr Psychiatry. 2001;9(2):169–76. [PubMed] [Google Scholar]
- 15.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 16.Arean PA, et al. Would older medical patients use psychological services? Gerontologist. 2002;42(3):392–8. doi: 10.1093/geront/42.3.392. [DOI] [PubMed] [Google Scholar]
- 17.Alvidrez J, Arean PA. Physician willingness to refer older depressed patients for psychotherapy. Int J Psychiatry Med. 2002;32(1):21–35. doi: 10.2190/J26T-YQMJ-BF83-M05D. [DOI] [PubMed] [Google Scholar]
- 18.Datto CJ, et al. Pharmacologic treatment of depression in nursing home residents: a mental health services perspective. J Geriatr Psychiatry Neurol. 2002;15(3):141–6. doi: 10.1177/089198870201500305. [DOI] [PubMed] [Google Scholar]
- 19.Pampallona S, et al. Patient adherence in the treatment of depression. Br J Psychiatry. 2002;180:104–9. doi: 10.1192/bjp.180.2.104. [DOI] [PubMed] [Google Scholar]
- 20.Bell CC, McBride DF. A Commentary for Furthering Cultural Sensitivity within Research in Geriatric Psychiatry. American Journal of Geriatric Psych. 2011;19(5):397. doi: 10.1097/JGP.0b013e318214ad43. [DOI] [PubMed] [Google Scholar]
- 21.Kales HC, et al. Race and inpatient psychiatric diagnoses among elderly veterans. Psychiatric Services. 2000;51(6):795. doi: 10.1176/appi.ps.51.6.795. [DOI] [PubMed] [Google Scholar]
- 22.Leo RJ, et al. Geropsychiatric consultation for African-American and Caucasian patients. Gen Hosp Psychiatry. 1997;19(3):216–22. doi: 10.1016/s0163-8343(97)00004-2. [DOI] [PubMed] [Google Scholar]
- 23.Fabrega H, Jr, et al. Ethnicity and psychopathology in an aging hospital-based population. A comparison of African-American and Anglo-European patients. J Nerv Ment Dis. 1994;182(3):136–44. doi: 10.1097/00005053-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Mulsant BH, et al. Schizophrenia in late life: elderly patients admitted to an acute care psychiatric hospital. Schizophr Bull. 1993;19(4):709–21. doi: 10.1093/schbul/19.4.709. [DOI] [PubMed] [Google Scholar]
- 25.Cooper LA, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 26.Miranda J, Cooper LA. Disparities in care for depression among primary care patients. J Gen Intern Med. 2004;19(2):120–6. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown C, Palenchar D. Treatment of depression in African American primary care patients. African American Research Perspectives. 2004;10:55–56. [Google Scholar]
- 28.Blazer DG, et al. Marked differences in antidepressant use by race in an elderly community sample: 1986-1996. Am J Psychiatry. 2000;157(7):1089–94. doi: 10.1176/appi.ajp.157.7.1089. [DOI] [PubMed] [Google Scholar]
- 29.Pingitore D, et al. Persons with depressive symptoms and the treatments they receive: a comparison of primary care physicians and psychiatrists. INT’LJ. 2001;31(1):41–60. doi: 10.2190/6BUL-MWTQ-0M18-30GL. [DOI] [PubMed] [Google Scholar]
- 30.Gum AM, Iser L, Petkus A. Behavioral Health Service Utilization and Preferences of Older Adults Receiving Home-Based Aging Services. American Journal of Geriatric Psych. 18(6):491. doi: 10.1097/JGP.0b013e3181c29495. [DOI] [PubMed] [Google Scholar]
- 31.Neighbors HW, et al. Mental health service use among older African Americans: the National Survey of American Life. American Journal of Geriatric Psych. 2008;16(12):948. doi: 10.1097/JGP.0b013e318187ddd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seyfried L, et al. Enhanced identification of eligibility for depression research using an electronic medical record search engine. Int J Med Inform. 2009 doi: 10.1016/j.ijmedinf.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheikh JI, Yesavage JA. Clinical Gerontology : A Guide to Assessment and Intervention. NY: The Haworth Press; 1986. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version; pp. 165–173. [Google Scholar]
- 34.Callahan CM, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Sirey JA, et al. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–20. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 36.Sirey JA, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158(3):479–81. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- 37.Valenstein M, et al. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord. 2009;112(1-3):50–8. doi: 10.1016/j.jad.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Zigmond AS, S RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 40.Deacon BJ, et al. The Anxiety Sensitivity Index-Revised: Psychometric properties and factor structure in two nonclinical samples. Behaviour Research and Therapy. 2003;41(12):1427–1449. doi: 10.1016/s0005-7967(03)00065-2. [DOI] [PubMed] [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 43.Katz S, et al. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 44.Wechsler D. WMS-III: Wechsler memory scale administration and scoring manual. Psychological Corp 1997 [Google Scholar]
- 45.Svarstad BL, et al. The brief medication questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Education and Counseling. 1999;37(2):113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 46.Rickles NM, Svarstad BL. Relationships between multiple self-reported nonadherence measures and pharmacy records. Res Social Adm Pharm. 2007;3(4):363–77. doi: 10.1016/j.sapharm.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 47.Valenstein M, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care. 2002;40(8):630–9. doi: 10.1097/00005650-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Rubin DB. Wiley series in probability and mathematical statistics. Applied probability and statistics,0271-6232. xxix. New York: Wiley; 1987. Multiple imputation for nonresponse in surveys; p. 258. [Google Scholar]
- 49.Crystal S, et al. Diagnosis and treatment of depression in the elderly medicare population: predictors, disparities, and trends. J Am Geriatr Soc. 2003;51(12):1718–28. doi: 10.1046/j.1532-5415.2003.51555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mamdani M, et al. Mental health-related drug utilization among older adults: prevalence, trends, and costs. Am J Geriatr Psychiatry. 2005;13(10):892–900. doi: 10.1176/appi.ajgp.13.10.892. [DOI] [PubMed] [Google Scholar]
- 51.Mulsant BH, Pollock BG. Treatment-resistant depression in late life. J Geriatr Psychiatry Neurol. 1998;11(4):186–93. doi: 10.1177/089198879901100404. [DOI] [PubMed] [Google Scholar]
- 52.Bogner HR, Lin JY, Morales KH. Patterns of early adherence to the antidepressant citalopram among older primary care patients: the prospect study. Int J Psychiatry Med. 2006;36(1):103–19. doi: 10.2190/DJH3-Y4R0-R3KG-JYCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ayalon L, Arean PA, Alvidrez J. Adherence to antidepressant medications in black and Latino elderly patients. Am J Geriatr Psychiatry. 2005;13(7):572–80. doi: 10.1176/appi.ajgp.13.7.572. [DOI] [PubMed] [Google Scholar]
- 54.Ryan EL, et al. Neuropsychological impairment in racial/ethnic minorities with HIV infection and low literacy levels: Effects of education and reading level in participant characterization. 2005 doi: 10.1017/S1355617705051040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Insel K, et al. Executive function, working memory, and medication adherence among older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61(2):P102–7. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- 56.Voils CI, et al. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am J Geriatr Psychiatry. 2005;13(2):157–65. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- 57.Lenze EJ, et al. Somatic symptoms in late-life anxiety: treatment issues. J Geriatr Psychiatry Neurol. 2005;18(2):89–96. doi: 10.1177/0891988705276251. [DOI] [PubMed] [Google Scholar]
- 58.Lenze EJ, et al. Good treatment outcomes in late-life depression with comorbid anxiety. J Affect Disord. 2003;77(3):247–54. doi: 10.1016/s0165-0327(02)00177-5. [DOI] [PubMed] [Google Scholar]
- 59.Wetherell JL, et al. Mental health treatment preferences of older and younger primary care patients. International Journal of Psychiatry in Medicine. 2004;34(3):219–33. doi: 10.2190/QA7Y-TX1Y-WM45-KGV7. [DOI] [PubMed] [Google Scholar]
- 60.American Academy of Family Physicians, American College of Physicians, American Osteopathic Association, Editor. Joint Principles of the Patient Centered Medical Home in Patient Centered Primary Care Collaborative A.A.o.P. Patient Centered Primary Care Collaborative; Washington, DC: 2007. [Google Scholar]


