Abstract
Context:
Metastatic bone disease is a commonly encountered problem in oncology practice. The most useful and cost effective treatment is radiotherapy (RT). Different fractionation schedule of RT can be used to treat such condition.
Aims:
Assessment of pain response in patients with vertebral bone metastasis after treating them with various radiation fractionations and to compare the toxicity profile in the treatment arms.
Settings and Design:
A prospective randomized study was designed to include total 64 patients from July 2010 to May 2011. Patients with histopathologically proven primary malignancy having symptomatic secondary deposits to vertebra were selected for the study. Patients were randomized to two arms receiving multiple fraction of RT with 30 Gy in 10 fractions and 8 Gy in single fraction RT, respectively.
Materials and Methods:
Patients with age >75 years, Karnofsky Performance Status (KPS) <40, features of cord compression were excluded from study. Initial pain response was assessed using Visual Analogue Scale (VAS) and compared using the same scale at weekly interval up to 1 month after treatment completion.
Results:
Arm A comprised of 33 patients while 31 patients were enrolled in Arm B. Baseline patient characteristics were comparable. Eleven patients were lost to follow-up. Initial pain scores were 7.23 ± 0.765 and 7.51 ± 0.55 in arm A and arm B, respectively. Pain scores reduced significantly in both the arms after 1 month (4.39 ± 1.82 in arm A; 5.25 ± 2.39 in arm B). Time of initiation of pain response was earlier in arm A (P = 0.0281), statistically significant. Mild G-I toxicity was noted in both the arms but differences in two arms were not statistically significant (P = 0.49), no interruption of treatment was required because of side effects.
Conclusions:
Different fractionation of radiation has same response and toxicity in treatment of vertebral bone metastasis. Single fraction RT may be safely used to treat these cases as this is more cost effective and less time consuming. Studies may be conducted to find out particular subgroup of patients to be benefitted more by either fractionation schedule; however, our study cannot comment on that issue.
Keywords: Single fraction of radiotherapy, Multiple fraction of radiotherapy, Vertebral bone metastasis, Pain scores, G-I toxicity
INTRODUCTION
Metastatic bone disease is a commonly encountered problem in oncology practice. Many patients with cancer, though heavily treated, ultimately metastasize and a large number of patients present as metastatic disease from the beginning. One of the important sites of metastasis is bone. Different metastatic foci to bone including vertebral bone metastases cause severe debilitating effects such as pain, pathological fracture, and spinal cord compression.[1] Treatment of bone metastasis is important issue to alleviate symptoms. Radiotherapy (RT) is a modality frequently used for bone metastasis, usually as an outpatient treatment. However, RT requires daily hospital attendance at a specialized center that may be some distance from the patient's home. A protracted course of RT may cause considerable problems for patients, especially those with poor performance status and limited life expectancy. It also increases the workload of the treatment center.[2]
In patients with bone metastasis use of single versus multiple fraction of RT cause similar results as per published data worldwide. Though high level of evidence using single fraction RT is there, it is not a common practice till now. This discordance between the results of randomized trials and patterns of practice has been highlighted in several practice-pattern surveys.[3–5]
In the present study, we address the clinical effects of fractionation schedules in palliative RT to bone metastases in a tertiary care hospital of eastern India. A prospective study to compare most commonly used RT protocol of 30 Gy in 10 fractions with 8 Gy in single fraction as a treatment of vertebral bone metastases was undertaken herein. The responses in patients were compared with those mentioned in international literature.
Aims and objectives
Our aim of the study was to compare the ability of different fractionation of radiation therapy in patients with vertebral metastases for response assessment with respect to the pain relief and to compare acute toxicities of these schedules.
MATERIALS AND METHODS
Adult patients of age not exceeding 75 years with painful uncomplicated radiologically proven bone metastases requiring palliative RT were eligible for the study. Patients were kept on WHO analgesic ladder II as per inclusion criteria. According to our institutional protocol they were given Non steroidal anti-inflammatory drugs (NSAID) combined with opioids. Patients had Karnofsky Performance Status (KPS) ≥40 were included in study. All patients had histopathologically proven primary malignancy. Patients with cord compression or existing or impending pathologic fracture and patients with wide area of multiple spinal metastases, existing bone disease, previous radiation to spine or any site overlapping the treatment site were not accrued into the study. After written informed consent, patients were randomized to palliative RT with either 30 Gy in 10 fractions over 2 weeks (arm A) or 8 Gy in a single fraction (arm B).
Patients’ pain was evaluated just before start of treatment using Visual Analogue Scale (VAS) for assessment of pain intensity. A 10 cm straight line was drawn with 0 at one end and 10 at other end. Patient was asked to mark his or her present pain intensity assuming 10 as worst pain and 0 to be no pain. Then patients were planned for radiation treatment.
Clinically tender spines were first identified and vertebral levels were anatomically found out. Superior and inferior field borders were kept on one uninvolved vertebra on both sides. Lateral borders taken touching tips of transverse processes. Field borders were marked by metal wires and X-ray done. After confirmation of desired field borders by radiologic picture plans were accepted.
Endpoints are defined as follows: Complete response: Complete subjective response without analgesic increase. Partial response: Reduction of 2 or more points (0-10 point scale) without analgesic increase. Pain progression: Increase in pain score 2 or more points with stable analgesic.
Acute toxicities were assessed using the Radiation Therapy Oncology Group (RTOG) criteria for adverse events. We have assessed acute Gastro intestinal (G-I) toxicity in both treatment arms. Patients were followed every week of treatment and at the end of 1 month of treatment. For the patients of single fraction arm telephonic follow-up was done weekly up to 1 month for response assessment.
Statistical analysis
Statistical analysis was done by MedCalc Software Version 11.6.1© 1993-2011 (Last modified: June 6, 2011). Chi-square and independent samples t-tests were used for comparison between the patient groups. Mann–Whitney test was done for independent samples to compare pain response at 1 month and G-I toxicities.
RESULTS
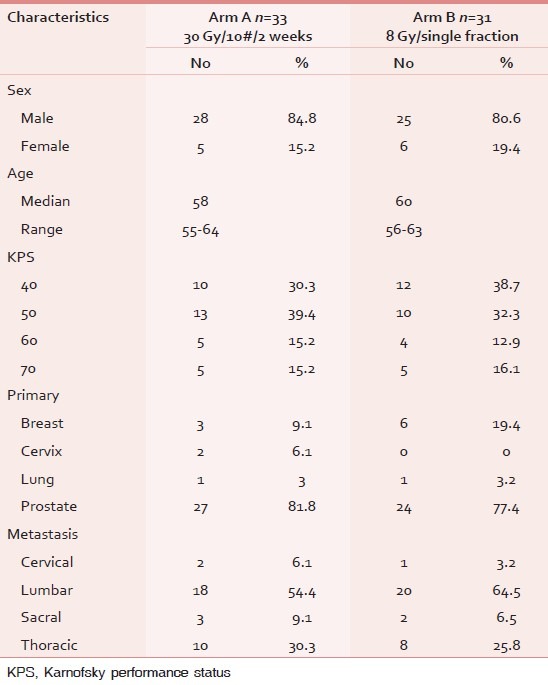
We have randomized 64 patients in our treatment arms from July 2010 to May 2011. Arm A comprised of 33 patients while 31 patients were enrolled in arm B. Baseline patient characteristics were comparable in both the arms. Median age was 58 years (range 55-64) and 60 years (range 56-63) in arm A and arm B, respectively. Male patients were predominant in both the arms (84.8% in arm A, 80.6% in arm B), patients with KPS score 40 and 50 were predominant in both the arms. Most of the patients had primary site of malignancy from prostate (81.8% in arm A and 77.4% in arm B). Most common metastatic sites were thoracic and lumbar spine in both the arms [Table 1].
Table 1.
Baseline demographic and clinical characteristics of the study population
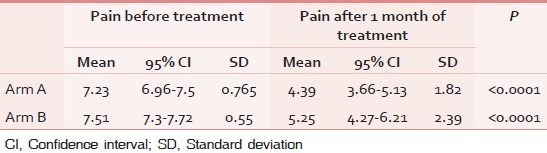
Unfortunately 11 patients (7 in arm A and 4 in arm B) did not come for follow-up and could not be contacted and one patient after randomisation did not come for treatment. Total 56 patients (87.5%) came for follow up after 1 month. Initial pain scores were 7.23 ± 0.765 and 7.51 ± 0.55 in arm A and arm B, respectively. Grade of pain was significantly reduced in both the arms after treatment [Table 2]. According to VAS pain score progressive pain were seen in 15.4% (n = 4) in arm A and 23.1% (n = 6) in arm B. Other patients reported to have partial pain response (84.6% in arm A and 76.9% in arm B). Those having partial pain response were shifted to changed analgesic regime. Two patients from arm A and three from arm B claimed no need for analgesics, 22 patients (12 in arm A and 10 in arm B) could be kept on NSAIDs and 15 (7 in arm A, 8 in arm B) still needed opiods.
Table 2.
Comparison of pain score before and after treatment
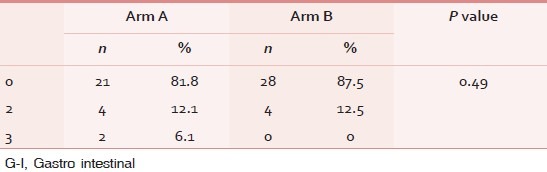
All patients finished their scheduled course of RT without incident. Side effects included only mild gastrointestinal disturbances. Eight patients (12.1%) suffered from grade 2 toxicities while only two (3%) faced grade 3 G-I adverse effects [Table 3]. Differences in two arms were not statistically significant (P = 0.49) no interruption of treatment was required because of side effects.
Table 3.
G-I toxicities
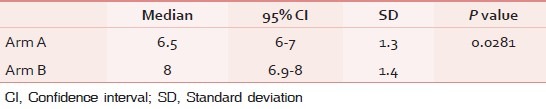
After 1 month of treatment using the same VAS scale we found median pain scores were four (95% CI 3.25-4.89) and five (95% CI 4.2-5.47) in arm A and arm B, respectively, but statistically non-significant (P = 0.1032). Time of initiation of pain response was earlier in arm A (P = 0.0281), statistically significant [Table 4].
Table 4.
Time of response from D1 of treatment
Patients having partial pain response were 44.23% (n = 23) in age >60 years and 36.53% (n = 19) in age <60 years (P = 0.9351). Linear trend of grade of pain reduction was found with increasing age but statistically non-significant.
DISCUSSION
Two large contemporary multicentric randomized trials[2,6] and a meta-analysis of 16 randomized trials, 4 have found no significant difference in the probability of achieving pain relief with different fractionation schedules of localized RT in painful uncomplicated bone metastases. Published results of a North American multicenter trial (RTOG 97-14)[7] and a meta-analysis of 12 randomized trials[8] have confirmed those findings. Hartsell et al. found the results between single versus multiple fractionation comparable in terms of toxicity. They reported 3-month complete pain relief in 8/1 fraction 15% versus 18% in multiple fraction (statistically non-significant [NS]); partial 50% versus 48% (NS); stable 26% versus 24%; progressive 9% versus 10%. Acute toxicity was significantly high in 30/10 fraction than 8/1 fraction arm: 17% versus 10%. Retreatment was higher in single fraction arm 18% versus 9%.[7]
Konski et al. published results from retreatment data of RTOG 97-14 and concluded patients receiving 8 Gy in a single fraction had significantly higher retreatment rates compared with patients receiving 30 Gy in 10 fractions.[9] Randomized multicentric trial done by Kaasa et al. reported no difference in pain intensity, global quality of life (QoL), fatigue, or opioid/non-opioid analgesics (NS). Median overall survival 8 Gy 9.6 months versus 30 Gy 7.9 months (NS).[10]
One study differs slightly in results. Roos et al. found better outcome in multiple fraction arm when 20 Gy/5 fractions was used. 8/1 was not shown to be as effective as 20/5, nor was it statistically significantly worse. Outcomes were generally poorer for 8/1, although the quantitative differences were relatively small.[11] Dutch Bone Metastasis Study in 2010 has shown that pain responded in ~50% of patients with short survival, regardless of fractional schema. Single fraction should be preferred, and additional palliative measure remain essential.[12]
Our findings are also in agreement, showing no significant difference in the degree of pain relief or in the response rate with treatment using either 8 Gy in 1 fraction or 30 Gy in 10 fractions in patients.
Despite the high-level evidence published in international literature, several practice-pattern surveys conducted among radiation oncologists in various countries have shown limited use of single fractions for bone metastases.[3–5] Haddad et al. studied a Canadian specialized academic palliative RT program and demonstrated that only one-third of palliative RT courses for bone metastases were prescribed using a single fraction.[13] Chow et al. argued that, instead of further dose fractionation trials in bone metastases, perhaps resources could be better invested in other research areas.[14] For example, the strong preference of clinicians to use multiple fractions for spinal metastases is likely a result of concern for the intermediate complications of bone metastases such as sub-acute cord compression and pathologic fracture. A systematic review by Sze et al.[8] demonstrated a rate of pathologic fracture in single-fraction RT patients that was 1.82 times the rate in multi-fraction patients, although the absolute rate of difference was only 1.3%. In addition, the meta-analysis mentioned earlier showed a trend for increasing rates of spinal cord compression in both single- and multi-fraction patients, but the number of events was too small to allow for testing of the difference.
Price et al. has previously also showed no difference in speed of onset, duration of pain relief at 12 weeks. Pain relief was independent of histology. Re-irradiation was possible more likely with 8/1 schedule but increased analgesic use in 30/10.[15]
In the report of Tong et al. new fractionation was used like 15 Gy/3 fractions for multiple metastases and reported 90% with some pain relief. 54% eventually had complete pain relief. No difference between RT regimens in pain relief. No difference among regimens in promptness of pain relief, except there was an association between the dose and the promptness to complete pain relief (fastest in 15 Gy, slowest in 25 Gy group); no difference in the duration of pain relief.[16]
CONCLUSION
In our study, we found both the radiation fractionation schedule for palliative vertebral mets treatment is equally effective in pain control. These findings match with the present literatures. Mild G-I toxicities are comparable in both the arms. Percentage of patients with partial pain response was greater in age >60 years in both the group but these finding did not reach statistical significance. Time of initiation of pain response was earlier in arm A (multiple fractions RT) which was the only significant finding.
Multiple fractions RT for treatment of metastatic bone disease are a common practice still in many institutions. We think single fraction RT for this purpose can safely be administered without any hesitation because standard literature supports for it and our study is also pointing to the similar results. The area which needs to be explored is any association between treatment outcome and patient characteristics such as age, primary, and sites of metastasis. If this sort of studies is conducted in future, subgroup of patients likely to be benefitted from any particular fractionation RT could be identified.
ACKNOWLEDGEMENTS
We are thankful to all of the patients who participated in the study. This work would not have been possible without the constant and vigilant support of members of palliative care team, Department of Radiotherapy, Medical College Kolkata. We would like to pay my humble gratitude to my respected teachers Prof. Shyamal Kumar Sarkar, Dr. Niladri Bihari Patra, Amitava Manna, and Dr. Subrata Chatterjee.
We express thanks to the following respected members of Department of Radiotherapy, Medical College Kolkata: Prof. Prabir Kumar Sur, Dr. Santanu Pal, Dr. Debabrata Mitra, Dr. Shyamsundar Adhikary, Dr. K.S. Manir, Dr. K. Bhadra, Dr. A. Saha, Dr. B. Bhattacharya, Dr. G. Kumar, Dr. A Mukherjee, Dr. J. Basu, Dr. Md. Azam, Dr. S.K.Kundu, and all other junior and senior colleagues.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Agarawal JP, Swangsilpa T, van der Linden Y, Rades D, Jeremic B, Hoskin PJ. The role of external beam radiotherapy in the management of bone metastases. Clin Oncol (R Coll Radiol) 2006;18:747–60. doi: 10.1016/j.clon.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Steenland E, Leer JW, van Houwelingen H, Post WJ, van den Hout WB, Kievit J, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: A global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52:101–9. doi: 10.1016/s0167-8140(99)00110-3. [DOI] [PubMed] [Google Scholar]
- 3.Chow E, Danjoux C, Wong R, Szumacher E, Franssen E, Fung K, et al. Palliation of bone metastases: A survey of patterns of practice among Canadian radiation oncologists. Radiother Oncol. 2000;56:305–14. doi: 10.1016/s0167-8140(00)00238-3. [DOI] [PubMed] [Google Scholar]
- 4.Ben-Josef E, Shamsa F, Williams AO, Porter AT. Radiotherapeutic management of osseous metastases: A survey of current patterns of care. Int J Radiat Oncol Biol Phys. 1998;40:915–21. doi: 10.1016/s0360-3016(97)00927-9. [DOI] [PubMed] [Google Scholar]
- 5.Roos DE. Continuing reluctance to use single fractions of radiotherapy for metastatic bone pain: An Australian and New Zealand practice survey and literature review. Radiother Oncol. 2000;56:315–22. doi: 10.1016/s0167-8140(00)00250-4. [DOI] [PubMed] [Google Scholar]
- 6.8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: Randomised comparison with a multifraction schedule over 12 months of patient follow-up. Bone Pain Trial Working Party. Radiother Oncol. 1999;52:111–21. [PubMed] [Google Scholar]
- 7.Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, Roach M, 3rd, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst. 2005;97:798–804. doi: 10.1093/jnci/dji139. [DOI] [PubMed] [Google Scholar]
- 8.Sze WM, Shelley MD, Held I, Wilt TJ, Mason MD. Palliation of metastatic bone pain: Single fraction versus multifraction radiotherapy.A systematic review of randomised trials. Clin Oncol (R Coll Radiol) 2003;15:345–52. doi: 10.1016/s0936-6555(03)00113-4. [DOI] [PubMed] [Google Scholar]
- 9.Konski A, Desilvio M, Hartsell W, Watkins-Bruner D, Coyne J, Scarantino C, et al. Continuing evidence for poorer treatment outcomes for single male patients: Retreatment data from RTOG 97-14. Int J Radiat Oncol Biol Phys. 2006;66:229–33. doi: 10.1016/j.ijrobp.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Kaasa S, Brenne E, Lund JA, Fayers P, Falkmer U, Holmberg M, et al. Prospective randomised multicenter trial on single fraction radiotherapy (8 Gy ×1) versus multiple fractions (3 Gy ×10) in the treatment of painful bone metastases. Radiother Oncol. 2006;79:278–84. doi: 10.1016/j.radonc.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Roos DE, Turner SL, O’Brien PC, Smith JG, Spry NA, Burmeister BH, et al. Randomized trial of 8 Gy in 1 versus 20 Gy in 5 fractions of radiotherapy for neuropathic pain due to bone metastases (Trans-Tasman Radiation Oncology Group, TROG 96.05) Radiother Oncol. 2005;75:54–63. doi: 10.1016/j.radonc.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 12.Meeuse JJ, van der Linden YM, van Tienhoven G, Gans RO, Leer JW, Reyners AK, et al. Efficacy of radiotherapy for painful bone metastases during the last 12 weeks of life: Results from the Dutch Bone Metastasis Study. Cancer. 2010;116:2716–25. doi: 10.1002/cncr.25062. [DOI] [PubMed] [Google Scholar]
- 13.Haddad P, Wong RK, Pond GR, Soban F, Williams D, McLean M, et al. Factors influencing the use of single vs multiple fractions of palliative radiotherapy for bone metastases: A 5-year review. Clin Oncol (R Coll Radiol) 2005;17:430–4. doi: 10.1016/j.clon.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Chow E, Lutz S, Beyene J. A single fraction for all, or an argument for fractionation tailored to fit the needs of each individual patient with bone metastases? Int J Radiat Oncol Biol Phys. 2003;55:565–7. doi: 10.1016/s0360-3016(02)04148-2. [DOI] [PubMed] [Google Scholar]
- 15.Price P, Hoskin PJ, Easton D, Austin D, Palmer SG, Yarnold JR. Prospective randomised trial of single and multifraction radiotherapy schedules in the treatment of painful bony metastases. Radiother Oncol. 1986;6:247–55. doi: 10.1016/s0167-8140(86)80191-8. [DOI] [PubMed] [Google Scholar]
- 16.Tong D, Gillick L, Hendrickson FR. The palliation of symptomatic osseous metastases: Final results of the study by the Radiation Therapy Oncology Group. Cancer. 1982;50:893–9. doi: 10.1002/1097-0142(19820901)50:5<893::aid-cncr2820500515>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]


