Abstract
Context:
For the first time in India, a Pain and Palliative Care policy to guide the community-based home care initiatives was declared by the Government of Kerala state. In Kerala, majority of the panchayats (local self-governments) are now conducting home-based palliative care as part of primary health care. National focus domain areas in palliative care research are structure and process, the physical aspects, and also the social aspects of care.
Aims:
The study was conducted to assess the patient's status and the services provided by palliative home care.
Settings and Design:
The descriptive study was conducted at Mavoor panchayat—Kozhikode district of Kerala, India by collecting information from the case records, nurses diary notes of all enrolled patients.
Materials and Methods:
Collecting information from the case records, nurses diary notes of all enrolled patients.
Statistical Analysis:
The data were entered using Microsoft excel for Windows XP and analyzed using SPSS 16.0 (Statistical Package for Social Sciences; SPSS Inc., Chicago, IL, USA).
Results:
Totally, 104 patients were enrolled. Diagnosis wise major category was degenerative diseases. There were 27% persons suffering from cerebrovascular accidents, 15.3% with malignancies, 8.7% with coronary artery disease, 5.8% with complications of diabetes, and 8.7% were with fracture of bones. The major complaints were weakness (41.3%), tiredness (31.7%), and pain (27%). Twenty-five percent persons complained of urinary incontinence, 12.5% complained of ulcer, 10.6% of edema, and 9.6% of mental/emotional agony. The activity of daily living status was as follows. Twenty-five percent subjects were completely bed ridden. 5.8% were feeding through Ryles tube, 16.3% had urinary incontinence, 9.6% were having no bowel control.
Conclusions:
The service could address most of the medical, psychosocial, and supportive needs of the patients and reduce their pain and symptoms. The interface between institutional-based care and home care needs more exploration and prospective studies.
Keywords: Activity of daily living, Community nurse, Home-based palliative care, Primary care, Quality of life
INTRODUCTION
Palliative care has been recognized as essential health care which should be comprehensive, accessible, and appropriate to the community they serve.[1] Changing demographic health transitions which brought burden on health care services are increasingly those due to chronic and incurable diseases. There are certain issues specific to Indian context that needs to be paid attention. Family is the most cherished social institution in India.[2] During the last years of life, the majority of time is spent at home, with family and community members providing much of the informal care. Social, psychological, religious, and spiritual networks are strongest at home. Family is the most vital non-formal social security, most preferred living arrangement, and also the most emotionally satisfying for the old.[2] Thus, in terms of patient and family preferences and appropriateness, provision of home care is a necessity for any palliative care service.[1] National policy is to promote the concept of “ageing in place or aging in own home and home care services and consider institutional care as the last resort.”[2] Some studies found out that palliative home care is better than hospital and also more cost-effective.[3]
For the first time in India, a Pain and Palliative Care policy to guide and facilitate the development of community-based home care initiatives under the leadership of local self-governments (LSGs) was declared by the Government of Kerala state.[1,4] The Arogyakeralam Palliative care project formulated in consonance with the policy has been quite successful in initiating such services with community participation in a large number of LSGI in all parts of Kerala. The initiative under the project aims to identify patients in need, offer guidance for appropriate treatment, provide care at home for the bed ridden, and incurably ill and equip the primary health care system to provide care including medicines.[4]
Since 1996, Kerala has been practicing decentralized planning, about 30% of the plan fund has been allocated to LSGs and the service sector including health was allotted more than 30% of the budget.[5] Ten percent is earmarked for the welfare services of disabled, old persons, women, and for palliative care.[6] In Kerala, majority of the panchayats (LSGs) are now conducting home-based palliative care as part of primary health care incorporating the LSGs and community based organizations (CBOs) with the primary health centres (PHCs). The point prevalence of persons requiring palliative care has been estimated to be 1/300 population with total projected for the state being 1 lakh.[7] So during the coming years, the palliative care program need to be scaled up. National focus domain areas in palliative care research are structure and process, the physical aspects, and also the social aspects of care.[8] In this context, the following study was conducted to assess the patient's status and the services provided by palliative home care and to determine the unmet needs.
MATERIALS AND METHODS
The study was conducted at Mavoor panchayat—Kozhikode district of Kerala, India. The area has a population of 30,961 living in 6,547 houses. In Mavoor panchayat, the community-based palliative care project was initiated by the LSG during the year 2010. Special fund was allotted from the annual plan fund for meeting the expenditure: Salary of nurse, medicines, supportive services, and logistics. A qualified nurse was selected from local community and underwent training from institute of palliative medicine, Calicut. The team consisting of a nurse, health volunteer, accredited social health activist, and a community member conduct home visits and palliative services are given. The field workers from the Department of Health Junior Public Health Nurse (JPHN), Junior Health Inspector (JHI) under five sub-centers also conduct periodic home visits to their areas. Emergency services are provided by doctors from the local PHC (Medical College Health MCH unit Cheruppa) which is a medical college training center.
A retrospective study was conducted by collecting information from baseline data at entry point, prospective case records, and nurse's diary notes of all patients who enrolled during the year 2010-2011 and received home-based palliative care services. The records contain baseline as well as follow-up information of the cohort which was timely entered by the home care nurse till the point of collection in July 2012. The collected variables include demographic, medical, physical, psychological, and social aspects of patients which indicate quality of life and the needs of patients/family, services provided by the team and its outcomes. For assessing activity of daily living, the mobility, feeding, bowel, and bladder control were examined. The complaints were subjective perception of the most annoying difficulties expressed by patients or immediate caretaker at home during entry point or subsequent visits. Most important complaints were listed in rank order and important ones selected for analysis. The services provided were medical, supportive, ulcer care, catheter services, and supply of accessories. The protocol of the study was approved by the Calicut medical college ethical committee and informed consent was collected from all subjects and those who are not able to give consent, consent was taken from their family care takers.
Statistical analysis
The data were entered using Microsoft excel for Windows XP and analyzed using SPSS 16.0. The quantitative variables are expressed as mean ± SD and discrete variables in frequencies or proportions. The significance was fixed at P value of 0.05.
RESULTS
During the period, totally 104 patients were enrolled. Age ranged from 12 to 100 years with mean 66.9 ± 19.5 years. (M: 63.8 ± 20, F: 68.8 ± 18.5, P = 0.2). There were 42 males and 82 females; the sex ratio was 40:60 (1,476 for 1,000 males). The average family size was 4.95 ± 2.49% were married and living with spouse. Spouse had passed away in 43% cases and 8% were unmarried. The mean period in years for getting palliative service after the onset of present illness was 2.2 ± 1.5 years.
Diagnosis wise major category was degenerative diseases. There were 28 (27%) persons suffering from cerebrovascular accidents, 16 (15.3%) with malignancies, 9 (8.7%) with coronary artery disease, and 6 (5.8%) with complications of diabetes. Nine (8.7%) were bed ridden due to fracture of bones of which majority were of very old age category with history of fall from home. Six (5.8%) were with mental illness. Fourteen (13.5%) were in the geriatric group without any specific diagnosis. The major sites of malignancies in the rank order were as follows: Cervix, 4; gastrointestinal tract, 3; oropharynx, 3; and lungs, 2.
The major complaint was weakness (43, 41.3%), i.e., motor dysfunction or inability to move any part of the body. The second was tiredness (33, 31.7%) and third was pain (28, 27%). Twenty-six (25%) persons complained of urinary incontinence, 13 (12.5%) complained of ulcer, 11 (10.6%) of edema, and 10 (9.6%) of mental/emotional agony. Eight (7.7%) persons each complained of insomnia or breathlessness, five (4.8%) complained of bleeding from anybody orifices. Six (5.8%) are having dysphasia or aphasia.
Mobility: Twenty-six (25%) subjects were completely bed ridden and 26 persons could move independently and rest 26 (25%) each needed some help to move.
Feeding: Forty-nine (47.1%) subjects could take food without help, 18 (17.3%) needed full help. Six (5.8%) were feeding through Ryles tube and 12 (11.5%) were able to swallow only liquid food.
Bladder: Fifty-one (49%) were having good bladder control, 13 (12.5%) had some control, 17 (16.3) had urinary incontinence, and 23 (22%) had undergone catheterization.
Bowel: Forty-four (42.3%) had good control of their bowel, 10 (9.6%) were having no bowel control, and 50 (48%) were having constipation.
Sleep: Fifty-five (52.8%) were having insomnia, five needed sedatives for sleeping, and nine (8.7%) were having over sleep.
Body care: Eighty-nine (85.6%) had good oral hygiene and 92 (88.5%) had good perineal hygiene. Eighteen (17.3%) had pressure ulcers in some parts of the body.
Treatment undergone: The data about the current or immediate past treatment undergone by the patients for the specific disease were as follows: 78 (77.3%) medical, 6 (6%) radiation, 2 (2%) surgical, and 1 dialysis. Eighteen (17.8%) were not undergoing any treatment.
Home care given: Sixty-three (60.6%) had received medical care, which included drugs for their symptoms and specific diseases. Sixty-nine (66.3%) had received some forms of supportive services like cash or kinds. Four had received water beds, two received walkers, and one received wheel chair. Thirty-one (29.8) received catheter care which included putting, changing, or bladder wash during this period. Seven (6.7%) were receiving ulcer care and two (1.9%) were receiving infection care.
Outcome: From this cohort, 38 (36.5%) expired during this time period. The mean duration of care received by the expired was 7.8 ± 5.7 months (M: 2.4 ± 1.7, F: 2.1 ± 1.3, P = 0.837). Only one person had recovered from the illness which was a case of paraplegia due to fall. There was no lost to follow-up.
DISCUSSION
The program was launched in October 2010. During this period studied, totally 104 patients enrolled. As per the estimation, according to the population, we expected around 100 patients.[7] So the uptake of the program was good. Seventy-two percent of persons belonged to >60 age group. The less proportion of male patients (40:60) with lower mean age was due to similar sex ratio in the geriatric population and higher life expectancy among females. At the country level also compared to men more women are confined to bed, exacerbated by life time gender-based discrimination.[9]
The average family size corresponds with value for the area, 4.7 persons per house. Among the study subjects, the proportion of married people was higher than reported from Delhi (67%).[10] The spouses had expired in 43% subjects and there were more widows than widower [Table 1], which was statistically significant. This was due to age differences among couples at the time of marriage and less life expectancy among males (M: 72 and F: 76 years). Compared to men, the incidence of widowhood among women >60 years was five times higher in the state. This was four times at national level.[9,11]
Table 1.
Gender wise details of the patients who received palliative care
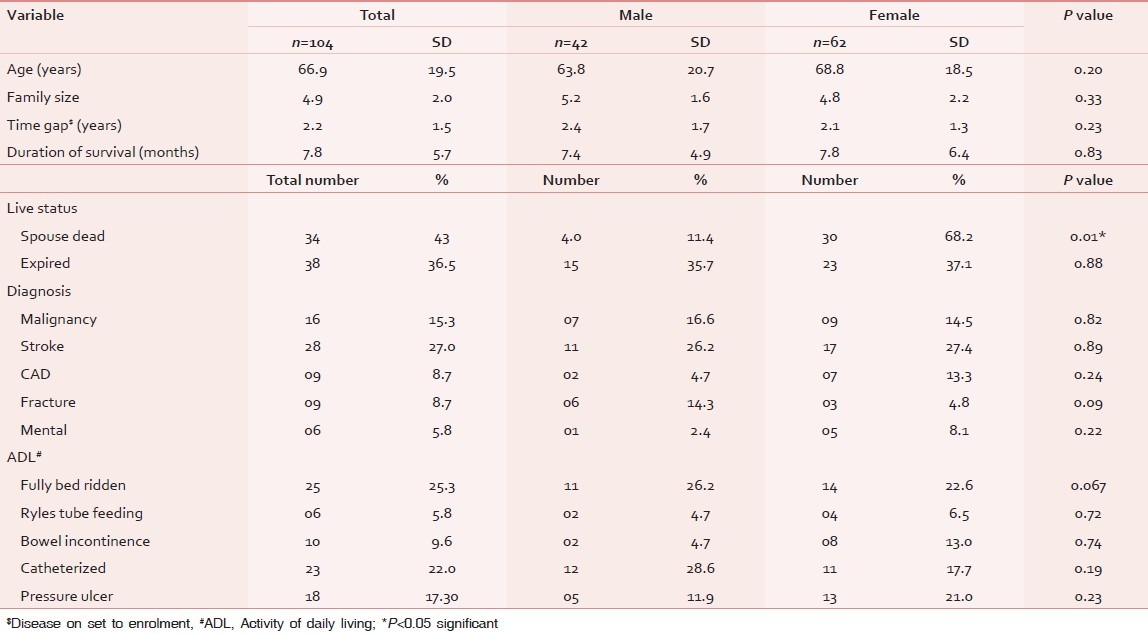
The reported prevalence of stroke was 1.2 per 1,000 in the area. Though 18 (54%) of the subjects were completely bed ridden, only 14% had reported pressure ulcer reflecting the quality of care like use of water bed. Fifty percent of those with malignancy belonged to 60-80 age group. Among females, the cervix was the major site. Other studies by pooling the data of 159 palliative care centers in the state, state cancer registry by Regional Cancer Centre and from Delhi reported that the breast was the major site.[1,10] In males, lungs was the major site which was similar to the report from the state pooled data.[1] Concordant with other studies, most of the cancers in males are closely related to personal habits and life styles and in females related to reproductive organs.[12]
With contrary to the incidence of coronary artery disease, the little female predominance non significant (NS) attributed due to survival bias. From this category, 45% had died during this period. Those bed ridden due to fracture of bones, majority are of very old age category with osteoporosis and history of fall from home.[12] In the state pooled data, 60% of cases were from fall from height.[1] All of them are immobile and 50% had pressure ulcers. The maximum death rate was (78%) reported from this group. Fourteen (13.5%) were in the geriatric group without any specific diagnosis which corresponds to geriatric population (12%) of the area and also the state.
The listed complaints are the felt needs of the patient community which include physical, mental, social, and economic problems. The major complaints (41.3%) were weakness, tiredness (31.7%), pain (27%), and urinary in continence (25%). For meeting these needs, a full time care taker is required who would not need to go for work outside home leading to economic problems. Only 50% of the cancer patients complained of pain which indicated good pain management. The low incidence of pressure ulcer (12%) among this bed ridden population reflects the quality of care, community empowerment of family members/care takers. For preventing pressure sores, a “revolving water bed bank” was functioning under local PHC. Out of the (10.6%) edema cases, each one was due to filariasis and chronic kidney disease and all others were dependent edema owing to immobility. Though the patients were affected with incurable terminal illness, the team could reduce the mental agony (9.6%) due to better counseling and communication skills. Sedatives were given (7.7%) to those with insomnia and suitable positioning/medicines were advised for those with breathlessness (4.8%). Most of the cases with bleeding were due to cancers particularly cervical cancers. Sixty-five percent of the family had communicated about their economic problem. As per the recent study reports conducted in the state, the out-of-pocket expenditure for curative care was rupees five thousand two hundred and sixty-nine (INR: 5,269) which was 13.4% of non-food expenditure. Out of this, 60% was for non-communicable disease.[13] The mean annual per capita expenditure for cancer care is rupees 143,000 and for coronary artery disease, rupees 23,900.[13] Mobility is a proxy indicator of severity of disease. Out of the 25 persons who were completely bed ridden, 17 (68%) died during this period. The prevalence of ulcer was 21% with those with restricted mobility. Fifty-five (51%) persons needed help for feeding of which six were on ryles tube feeding. Of these, five were catheterized and five died during this period (P = 0.001).
Forty-nine percent were having good bladder control and the rest 51% had either incontinence or underwent catheterization, 9.6% were having no bowel control and passed motion unknowingly. Forty-eight percent suffered from constipation and needed digital evacuation or laxatives and 17.3% had pressure ulcers in any part of the body. Females reported higher prevalence (21%) than males (12%), but it was not statistically significant (P = 0.230). Most of them (77.3%) had undergone some mode of treatment from the nearby tertiary care centers. The surgical and radiation treatments were for malignancy. In geriatric groups, many problems are accepted as a part of ageing process.[12] 17.8% were not undergoing any treatment, probably due to the above perception. In males, though the prevalence of this group was high, it was not statistically significant [Table 1].
Majority (60.6%) received medical care, may be drugs for their symptoms or for the specific disease. This need was less than reported from another study (90%) from Kerala.[14] Inpatient service was given from the PHC whenever necessary. 66.3% received some supportive services like cash or kinds. This supply of accessories was higher than reported earlier from the state as 2.1%,[14] which shows the strength of the system to meet the non-medical needs. 29.8% had received catheter care either putting, changing, or bladder washes during this period. Due to reluctance of the family members or non-co-operation of patients, all who need it were not catheterized. Among those above 80 years, 36% are catheterized. Though 17.3% had pressure sores, only 6.7% had received ulcer care from the team, the rest was cared by the family members which reflect the community capacity building of the program. The patients are elderly with malignant or pressure ulcers but even then only 1.9% required infection care during this period which reflects the good practices of wound care in the home settings. Forty-six percent of families belonged to below poverty line (BPL) category. More than 65% of the families were having financial problems. The team arranged financial help through charity organizations and philanthropists. Due to the absence of universal health care or insurance, the families have to spend out-of-pocket during treatment of its members. It was reported from the state that 56.5% met the expenses from their own family savings, 39% borrowed money, and 4.5% had to sell their property to meet the health expenditure.[15] The palliative care has reduced the financial burden and chances of falling in debt in this area. The death rate of the area was 5.4/1,000. 36.5% expired in this cohort. In the >60 age group, the death rate was 50%, compared to below 60 group (OR =3.5, P = 0.003). There was no lost to follow-up. In institution-based palliative care, the dropout rate has been reported to be 25%.[14] The aim of palliative care is to get the highest quality of life for patient and their families.[16] As expressed by the 78% of the responders of a community study,[3] home care improves the quality of life.
CONCLUSION
Palliative care has been defined by the World Health Organization as “the total active care of patients whose disease is not responsive to curative treatment. Control of pain and other symptoms, and addressing psychological, social, and spiritual problems, is paramount. The goal of palliative care is achievement of the best quality of life for patients and their families.”[16] In the study, we looked at the health status of patients undergoing palliative care and services given to them through the home-based program and found that in resource poor settings, most of their family needs can be cost effectively delivered through home care services. The service could address most of the medical, psychosocial, and supportive needs of the patients[16] and reduce their pain and symptoms. Among the bed ridden patients, small proportion developed pressure ulcers most of which are managed by home care takers and infection rate was found to be low. Similarly, low proportion of cancer patients complained of pain, very few expressed their mental agony, and large proportion received supportive services. Contrary to the existing conventional expensive hospital care model, LSG supported home-based palliative care conducted by local primary health care system to certain extend can give comprehensive health care to bed ridden patients and thus improve the quality of life. For comparison of the results, similar studies were not available from the state. For the evaluation of the program, further follow-up studies are needed. Though the study was limited by its retrospective nature, this was the first attempt to study different aspects of palliative care in the area. The interface between institutional-based care and home care needs more exploration and prospective studies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Sallnow Libby, Kumar Suresh. Kerala, India: Institute of Palliative Medicine; 2008. Work book Second International Workshop on Community Participation in Palliative care: Home based care; pp. 7–35. [Google Scholar]
- 2.Ministry of Social Justice Government of India: National Policy for Senior Citizen. 2011. [Last accessed on 2012 Aug 01]. Available from: http://www.Social Justice.nic.in/pdf/dnpc.pdf .
- 3.Joseph N, S J, Kotian S. A comparative study to assess the awareness of palliative care between urban and rural areas of ernakulum district, kerala, India. Indian J Palliat Care. 2009;15:122–6. doi: 10.4103/0973-1075.58457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Rural Health Mission. Kerala state. [Last accessed on 2012 July 25]. Available from: http://www.arogyakeralam.gov.in/index.php/special-initiaves/palliative-care-project .
- 5.State Planning Board Government of Kerala: Economic review, Thiruvananthapuram: Government of Kerala. 2010 [Google Scholar]
- 6.Thrissur: LSG Department, Government of Kerala; 2012. Guideline for Local self Governments for preparing projects. KILA; p. 11. [Google Scholar]
- 7.Koshy C. The palliative care movement in India: Another freedom struggle or a silent revolution? Indian J Palliat Care. 2009;15:10–3. doi: 10.4103/0973-1075.53495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohanti BK. Research focus in palliative care. Indian J Palliat care. 2011;17:8–11. doi: 10.4103/0973-1075.76231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Sample Survey Organization 60th Round (2004). Report No. 507. Ministry of Statistics and Programme Implementation, Government of India: New Delhi. 2006. [Last accessed on 2012 Aug 3]. Available from: http://www.mospi.gov.in/national.data.bank/pdf/NSS.60th Round.507.pdf .
- 10.Singh DP. Quality of life in cancer patients receiving palliative care. Indian J Palliat Care. 2010;16:36–43. doi: 10.4103/0973-1075.63133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Old age policy Social welfare department: Information and Public relation Government of Kerala. 2006. [Last accessed on 2012 August 02]. Available from: http://www.swd.kerala.gov.in .
- 12.Vibha, Laskar AR. Women's health: Beyond reproductive years. Indian J Public Health. 2011;55:247–51. doi: 10.4103/0019-557X.92399. [DOI] [PubMed] [Google Scholar]
- 13.Health expenditure of Kerala: Study report. Kerala Shastra Sahithya Parishath (Malayalam) Unpublished 2012
- 14.Unni K, Edasseri D. A prospective survey of patient drop-outs in a palliative care setting. Indian J Palliat Care. 2012;18:27–30. doi: 10.4103/0973-1075.97345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jayakrishnan T, Jeeja MC. Kerala: Society for Social Health Action and Research; 2007. Disease burden of Kerala – Study paper; pp. 10–27. [Google Scholar]
- 16.Hubert R, Jochan RN, Theo Dassan. Evaluating Palliative Care.A review of literature. Palliative Care: Res Treat. 2009;3:5–12. [Google Scholar]


