Abstract
BACKGROUND AND OBJECTIVE:
Physicians may experience periods of acute sleep deprivation while on-call, in addition to baseline chronic sleep deprivation which may affect physicians’ performance and patients’ safety. The purpose of this study was to determine the effect of acute sleep deprivation due to working long on-call shifts on mood and alertness, both of which may impair physicians’ performance.
METHODS:
Eighty-eight junior physicians working in one university hospital completed a questionnaire, before and after completion of a shift, that collected data regarding socio-demographic factors, patterns of work and sleep, Profile of Mood States (POMS), and Stanford Sleepiness Scale. Based on duration of sleep the physicians had during on-call in comparison to their usual average sleep, the participants were categorized into group 1 (those who slept many fewer hours), group 2 (those who slept fewer hours), or group 3 (those who slept the same number of hours).
RESULTS:
More than 87% of the participant slept 5 or fewer hours while working an on-call shift. Among all participants, the percentage of physicians who were alert post-on-call was significantly reduced compared to the percentage pre-on-call (P = 0.001). The post-on-call total POMS scores of groups 1 and 2 were significantly worse than their pre-on-call scores (P = 0.001 and 0.038, respectively), while there was no significant difference between the pre- and post-on-call POMS scores of group 3 (P = 0.165).
CONCLUSION:
Acute sleep loss due to working long on-call shifts significantly decreases daytime alertness and negatively affects the mood state of junior physicians.
Keywords: Acute sleep deprivation, alertness, profile of mood states, sleepiness
Acute sleep deprivation due to extended work hours and circadian disruption has long been a concern among health care givers,[1] particularly among junior physicians. Although such work requires high levels of psychomotor performance, cognitive function, and emotional equilibrium,[2] junior physicians are often scheduled to work in shifts that are excessively long, often ranging from 24 to 30 h.[3] During these long shifts, their sleep is often limited and fragmented, leading to acute sleep deprivation, which may result in significant changes in cognitive functioning, alteration of mental status in a manner resembling depression or anxiety, and difficulty with short-term memory.[4] Indeed, several studies have found that such sleep deprivation significantly affects physician performance and patient safety,[2,5–7] with one study revealing that interns working a traditional schedule of more than 76 h per week made 36% more serious medical errors than when working an average of 65 h per week.[6]
Several researchers have examined the effect of working long on-call hours on performance and cognitive functioning.[3,8–10] Despite the fact that working extended shifts may also result in impaired mood and decreased alertness, which can impair cognitive functioning and physician performance with negative impact on patients’ and doctors’ safety, very few researchers have studied these effects.[11,12] To fill this research gap, this study examined the effect of acute sleep deprivation due to working extended on-call hours on both mood and alertness in junior physicians in a teaching hospital.
Methods
This cross-sectional comparative study was conducted at King Abdul-Aziz University Hospital (KAUH) in Jeddah, Kingdom of Saudi Arabia (May 2009-April 2010). As the number and duration of on-call shifts are similar for all junior physicians (junior residents and interns) in the Departments of Medicine, Surgery, Pediatrics, and Obstetrics, all junior physicians in these departments were included. The participants were recruited after they had worked for 1 month in their rotation to ensure that they were accustomed to the working environment before their performance was observed. As the duration of on-call shifts during weekends and national vacations is generally briefer, the participants were not assessed during these shifts.
Consent was obtained from all participants and confidentiality maintained to the greatest extent possible. As each participant was interviewed before and after completing his/her shift, each served as his/her own control. Assessment was performed both before and after completion of a shift using a questionnaire that collected data regarding socio-demographic factors, patterns of work and sleep, and daily activity during shifts (e.g., eating, praying, and driving), and that contained both the Profile of Mood States (POMS) and the Stanford Sleepiness Scale (SSS). Additional questions to assess sleep pattern and quality during the on-call night were added to the post-on-call assessment instrument. The pre-on-call interview was conducted between 2:00 and 5:00 p.m. and the post-on-call assessment immediately before the physician left the hospital.
According to the Saudi Commission for Health Specialties (SCHS), the body responsible for the accreditation of resident training programs within the Kingdom of Saudi Arabia, residents are allowed to work no more than 29 h of continuous on-call duty.[13] However, no such regulations apply to interns or physicians who are not enrolled in the SCHS training program.
Instruments
Profile of mood states
Since 1971, when the original POMS was published as a means of measuring the immediate mood states of individuals,[14,15] numerous studies have provided evidence of the predictive and construct validity of the POMS Standard, and the POMS Brief, a short form of the POMS, was developed in 1983.[16] The version of the POMS questionnaire used in this study was the original English version of the POMS Brief, which contains 37 self-report items measuring the subscales of depression, anger, tension, confusion, fatigue, and vigor to which the participants respond using a 5-point Likert Scale ranging from 1 (not at all) to 5 (extremely).[17] Each of these symptoms has its own scale. The higher the score the worse is depression, anger, tension, etc. However, in case of vigor, the higher the score the better is the vigor feeling. Total POMS score determines the mood status. The higher the score the worse is the mood status (ranges from 0 to 144). Total POMS is calculated by adding up the scores obtained for depression, anger, tension, confusion, and fatigue, and then subtracting the vigor score. An increment in total score is an indication of worsening mood.
Stanford sleepiness scale
This is a well-validated instrument used to measure the impact of short-term acute sleep loss on subjective sleepiness.[18,19] It consists of seven statements to which subjects respond by selecting one of these statements that best describes individual's level of sleepiness or alertness:
1 = feeling active, vital, alert, wide awake
2 = functioning at a high level, not at peak, able to concentrate
3 = relaxed, awake, not at full alertness, responsive
4 = a little foggy, not at peak, let down
5 = fogginess, losing interest in remaining awake, slowed
6 = sleepiness, prefer to be lying down, fighting sleep, woozy
7 = almost in reverie, sleep onset soon, losing struggle to remain awake.
Items 1-3 indicate an alertness status, while items 4-7 indicate a sleepiness status.[20]
Statistical analysis
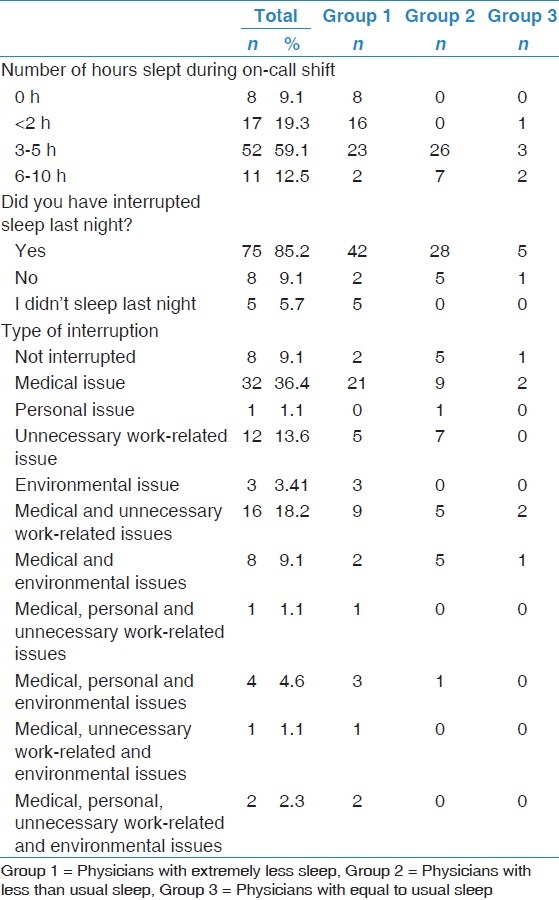
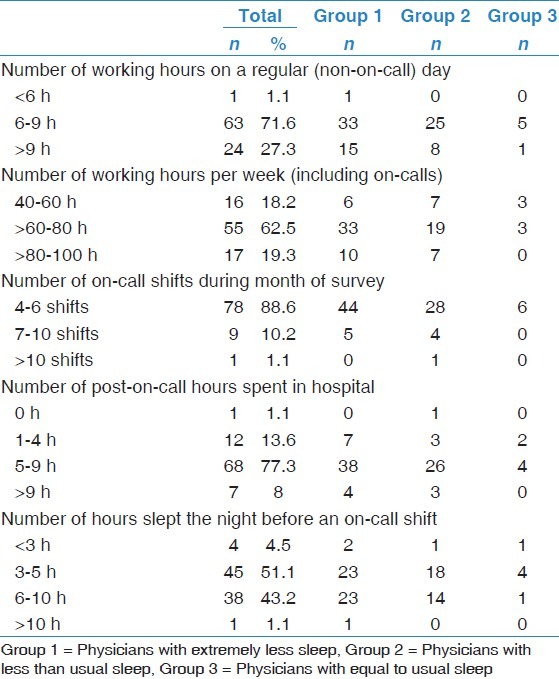
All data were analyzed using the Statistical Package for the Social Sciences (SPSS) software package, version 16. Paired Student's t-test was performed for SSS and Wilcoxon signed-rank test was used for the non-parametric results. A P value of less than 0.05 was considered an indication of statistical significance. The study population was divided into three groups according to the relative amount of sleep that they obtained on the days on which they were on-call. Group 1 was composed of physicians who slept many fewer hours of sleep compared to days on which they were not on-call, group 2 slept fewer hours, and group 3 slept the same number of hours [Table 1].
Table 1.
Sleep patterns during on-call shifts
Results
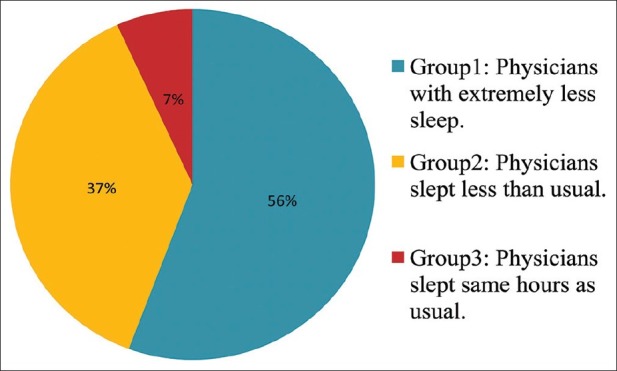
A total of 100 physicians were initially eligible for study participation. One physician who refused to participate and 11 physicians who failed to complete the post-on-call assessment due to miscommunication were excluded from the final analysis, resulting in a study sample size of 88 participants, of whom 48 (55%) were men and 40 (45%) were women [Table 2]. Figure 1 illustrates the classification of participants based on comparison of duration of sleep during the days on which they were on-call to the days on which they were not on-call. Characteristic of working hours of regular and on-call days and sleep patterns during on-call shifts are illustrated in Tables 1 and 3, respectively. More than two-thirds of participants work for 6-9 h daily and 60-80 h weekly. The vast majority had 4-6 on-call shifts during the month of the study and remained in hospital post-on-call for ≥5 h. Surprisingly, more than half of participants slept for ≤5 h during the pre-on-call night. However, one third reported sleeping for less than 2 h during the on-call shift, while about two thirds slept for 3-5 h only. Ninety-one percent had interrupted sleep or did not sleep at all, however, only 36.4% of participants had merely genuine medical care related issues as causes of sleep interruptions.
Table 2.
Demographic data
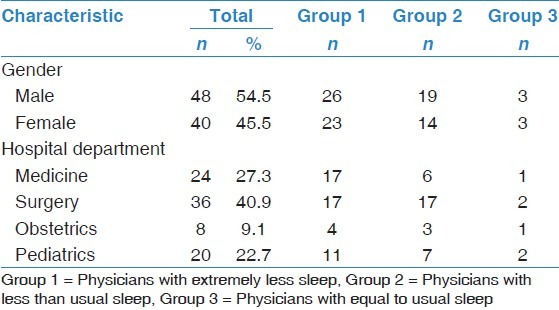
Figure 1.
Classification of study population based on duration of sleep during an on-call night in comparison to usual night sleep
Table 3.
Number of working and sleeping hours on regular and on-call days
Of all participants, the percentage of alert physicians post-on-call was significantly reduced compared to the percentage pre-on-call (P = 0.001) [Table 4, Figure 2]. Although the pre-on-call alertness status was similar among the three groups, there was significant difference in the post-on-call status (P = 0.796, 0.007 respectively) [Table 4]. Specifically, 86% and 55% reported that their workload sometimes forced them to delay prayers or miss meals, respectively, during on-call days. More than 10% of male participants reported experiencing a car accident while driving home after working on-call shift (females cannot drive according to local rules and regulations).
Table 4.
Pre-and post-on-call alertness/sleepiness based on stanford sleepiness scale score
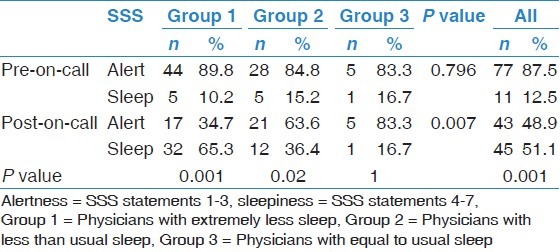
Figure 2.
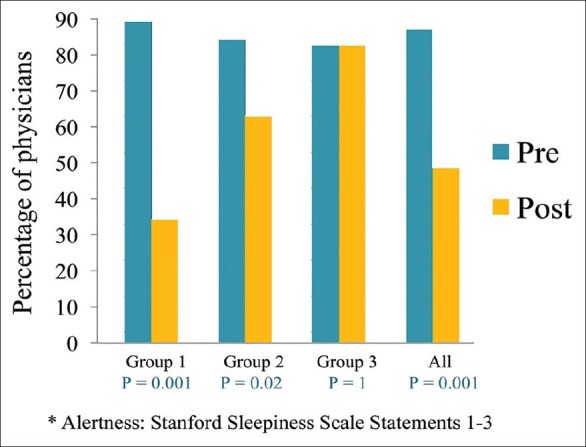
Percentage of alert * physicians pre- and post-on-call
A significant difference was found between pre- and post-on-call total POMS scores of groups 1 and 2, but not those of group 3 (P = 0.001, 0.038, and 0.165, respectively) [Table 5, Figure 3]. However, analysis of the results of the entire study population revealed a significant increase in post-on-call total POMS score as well as post-on-call confusion and fatigue sub-scores, with a decrease in the vigor sub-score, compared to the pre-on-call scores (P = 0.001).
Table 5.
Comparison of pre- and post-on-call POMS scores
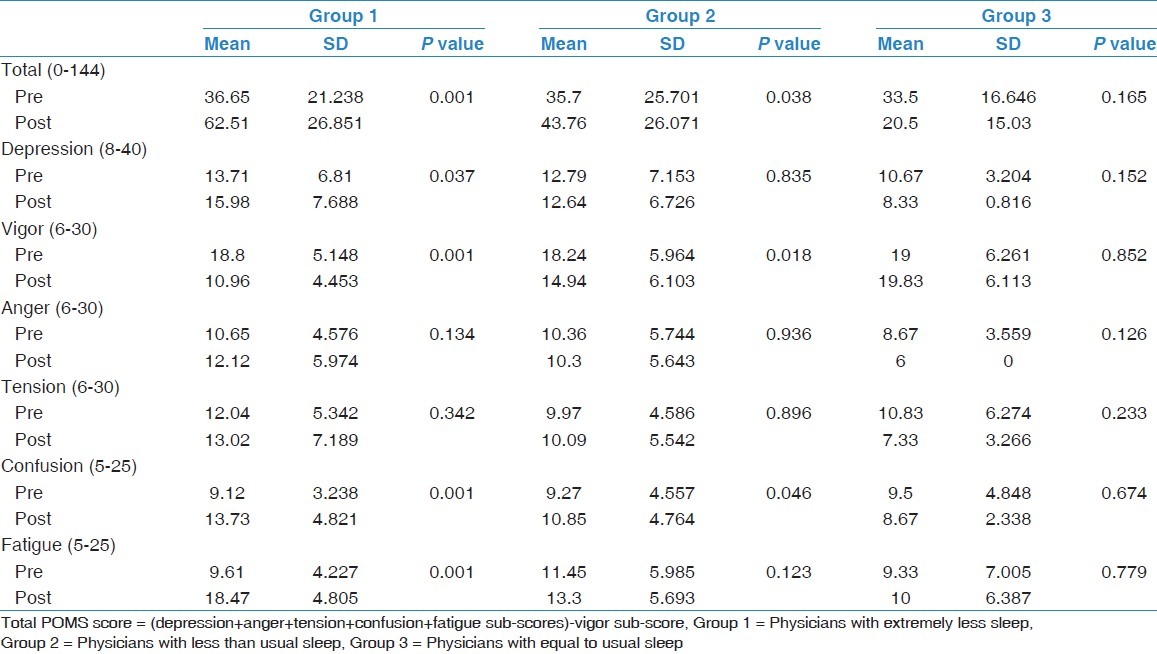
Figure 3.
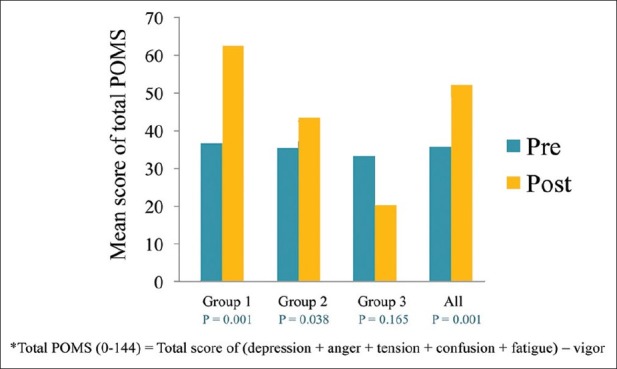
Pre- and post-on-call *profile of mood states scores
Discussion
The findings of this study indicate that majority of junior physicians examined suffer from acute sleep deprivation during the days on which they are on-call, leading to significant daytime sleepiness and impaired mood status. Specifically, more than 25% of the participants reported sleeping fewer than 2 h during on-call days and 93% reported obtaining fewer or many fewer hours of sleep than usual during on-call days (groups 1 and 2) [Tables 1 and 2]. Their lack of sleep was reflected in their SSS scores, which indicated that they experienced a significantly increased level of sleepiness post-on-call compared to pre-on-call (P = 0.001 and 0.02, respectively) [Table 4].
Interestingly, over 50% of the participants reported sleeping for fewer than 5 h the night preceding an on-call shift, which may reflect their exposure to chronic sleep deprivation, a common phenomenon of modern society. Therefore, most of these physicians suffer from acute on top of chronic sleep deprivation post-on-calls, with all possible consequences including decreased alertness and concentration, and impaired judgment, which pose risks to patient care and physician safety.[21–25] Indeed, more than 10% of the male participants in this study reported having experienced a car accident while driving home after completing an on-call shift, reflecting the danger of excessive daytime sleepiness.
The identification of a correlation between increased sleep deprivation and increased risk of accidents in this study supports previous findings, including those of Marcus et al.,[26] who found that 50% of interns reported frequently falling asleep at the wheel after completing an on-call shift. Supporting Barger et al.'s[7] conclusion that working shifts of extended duration pose a safety hazard for interns, Wilhelm et al.[27] found that experiencing even partial sleep deprivation after one on-call night leads to remarkably reduced alertness and associated hazards. These findings support the research of Reddy et al.[28] who recently reported that residents working in medical intensive care units experienced severe sleepiness on post-on-call days despite adherence to the guidelines set by Accreditation Council for Graduate Medical Education (ACGME).[29] Reddy et al. also concluded that the short sleep latency experienced by some participants was an indication of chronic sleep deprivation among residents in general.[28] An interesting finding of this study was the lack of a correlation between post-on-call sleepiness as assessed subjectively by SSS score and objectively by a modified multiple sleep latency test.[28] This finding suggests that residents may have a poor perception of, and hence underestimate, the extent of their sleepiness during a post-on-call day.
Restrictions on hours worked by medical trainees have been in effect in the United Kingdom since 1996 and across the United States since 2003. In a similar effort to decrease fatigue and sleepiness among local residents, the SCHS issued a statute that mandated work hour limitations (WHLs) in 2004.[13] However, the effect of such WHLs on patient safety remains unclear; whereas some researchers have found that adherence to WHLs does not prevent excessive daytime sleepiness post-on-call shifts,[28] others have found that reducing the number of in-training working hours improves alertness and reduces medical errors.[1,2] Yet others have obtained mixed results, including Goitein et al.[21] whose survey study of internal medicine residents in a university-based residency training program revealed that although the residents expressed approval of the WHLs overall and reported that WHL implementation has benefited their well-being, they also reported that implementation has had negative effects on patient care and resident education.[21] In a systematic review of 64 studies examining shift length, protected sleep time, and night float over the last two decades, Reed et al.[30] found that although most supported reductions in shift lengths, they did not specify optimal shift durations. Although the three studies that examined the relationship between shift length and mortality found no relationship between these factors and the six studies that examined the relationship between shift length and medical errors suggested that fewer errors are associated with shorter shifts, these studies had significant methodological limitations.[30] Based on a systematic review of 72 studies that assessed the impact of a change in working hours on postgraduate medical training, patient safety, or clinical outcomes, Moonesinghe et al.[31] concluded that restricted working hours to fewer than 80 per week has no negative impact on patient care and medical education. However, they also concluded that because studies of the impact of European legislation limiting working hours to fewer than 56 or 48 h a week were of poor quality and offered conflicting results, firm recommendations regarding optimal shift duration could not be made.[31] In brief, the evidence regarding the effect of on-call shift duration on healthcare provider performance and quality of patient care is insufficient and inconclusive, calling for more well-designed research into these factors.[22,32]
Of the several factors that may have contributed to the limited success of WHL implementation, poor adherence to SCHS rules by residents and lax application of WHLs by residency programs may be particularly important.[33] The importance of these factors is reflected in the findings of this study; specifically, 12% of the participants reported working more on-call shifts than permitted; 85% reported continuing to work for more than 5 h after their on-call shift had ended; and almost 20% reported working more than the maximum permitted hours per week, including on-call hours (80 h), all of which are clear SCHS violations[13] [Table 3]. Another factor that may have limited the success of WHL implementation is that junior physicians do not appear to compensate for sleep debt resulting from working on-call days by obtaining adequate sleep on their non-on-call days. This factor was reflected in the finding that more than 50% of the participants of this study reported sleeping fewer than 5 h on the night before an on-call night, as well as Reddy et al.'s finding that the average duration of sleep for the two successive nights preceding an on-call night was approximately 7 h, a quantity insufficient to compensate for the sleep debt resulting from one on-call night.[28]
Effective performance by hospital physicians requires high levels of concentration and cognitive performance, rapid judgment, prompt and correct decision-making, and fine motor skills. This study found a significant increase in POMS score, an indication of worsening mood, post-on-call compared to pre-on-call among physicians in groups 1 and 2. In a similar study of interns in Singapore, 89.5% of participants were found to have experienced adversely affected mood and increased daytime sleepiness after working an on-call night shift as more time spent at work after calls.[34] In a study of the results of four standard tests of cognitive function administered to 23 university hospital staff members at rest, following one on-call night and following another night of recovery sleep, Robbins et al.[2] found that the results of three tests indicated a statistically significant deterioration in functioning after the on-call night. The results of this and other studies indicate that the stress produced by acute sleep deprivation and prolonged fatigue among physicians leads to reduced alertness and concentration, which, in turn, leads to prolonged and suboptimal decision-making and impaired judgment, both of which impair physician performance and jeopardize patient and physician safety.[2,21–25]
The results of this study indicate that factors that significantly affect post-on-call POMS score are the number of hours slept while working on-call (P = 0.03), the extent of workload as reflected by the number of meals missed (P = 0.019), the extent to which prayer must be postponed or missed (P = 0.012), and the degree of sleepiness (P = 0.001). Therefore, minimizing the number of unnecessary disturbances to sleep may improve quantity and quality of sleep, and hence post-on-call POMS score. As only one-third of the participants in this study reported genuine medical issues as the reasons for their sleep disturbance, decreasing sleep disturbance among physicians is a realistic goal. In addition, reducing workload by ensuring that an adequate number of physicians are working on each shift may increase the number of hours for sleep and leisure available to each physician.
In conclusion, acute sleep deprivation resulting from working long on-call shifts often results in dose-dependent impairment of alertness and mood. These findings suggest the need to reappraise the efficacy and feasibility of current policy regulating the scheduling of junior physicians and, if warranted, placing further limitations on working hours and increasing the number of junior physicians working each on-call shift as possible solutions.
Acknowledgments
The author is appreciative of the assistance of the following physicians in collecting the data: Basem El Deek, Bara’a K Al-Nabulsi, Aisha M. Farhan, Rawa’a K. Al-Nabulsi, Omer A. Qashqary, Fareed A. Sindi, Sami Y. Sa’ad, and Omniah M. Andijani.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Friedman RC, Kornfeld DS, Bigger TJ. Psychological problems associated with sleep deprivation in interns. J Med Educ. 1973;48:436–41. doi: 10.1097/00001888-197305000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Robbins J, Gottlieb F. Sleep deprivation and cognitive testing in internal medicine house staff. West J Med. 1990;152:82–6. [PMC free article] [PubMed] [Google Scholar]
- 3.David M, Steven K. Fatigue among clinician and safety of patients. N Engl J Med. 2002;347:1249–55. doi: 10.1056/NEJMsa020846. [DOI] [PubMed] [Google Scholar]
- 4.Killgore WD, Killgore DB, Day LM, Li C, Kamimori GH, Balkin TJ. The effects of 53 hours of sleep deprivation on moral judgment. Sleep. 2007;30:345–52. doi: 10.1093/sleep/30.3.345. [DOI] [PubMed] [Google Scholar]
- 5.Knauth P. In: Design of shift work systems. Colquhoun WP, Costa G, Folkard S, Knauth P, editors. Vol. 27. Frankfurt am Main and New York: Shift Work Problems and Solutions; 1996. pp. 33–44. [Google Scholar]
- 6.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 7.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Harvard work hours, health, and safety group. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–34. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 8.Leung L, Becker CE. Sleep deprivation and house staff performance: Update 1984-1991. J Occup Med. 1992;34:1153–60. [PubMed] [Google Scholar]
- 9.Owens JA. Sleep loss and fatigue in medical training. Curr Opin Pulm Med. 2001;7:411–8. doi: 10.1097/00063198-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, Duncan BW, Bates DW. Fatigue, sleepiness, and medical errors. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM, editors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment No. 43. Rockville, Md: Agency for Healthcare Research and Quality; 2001. pp. 519–31. [Google Scholar]
- 11.Weinger MB, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. 2002;287:955–7. doi: 10.1001/jama.287.8.955. [DOI] [PubMed] [Google Scholar]
- 12.Howard SK, Rosekind MR, Katz JD, Berry AJ. Fatigue in anesthesia: Implications and strategies for patient and provider safety. Anesthesiology. 2002;97:1281–94. doi: 10.1097/00000542-200211000-00035. [DOI] [PubMed] [Google Scholar]
- 13.Saudi Council for Heath Specialties. [Last accessed on 2010 Oct 01]. Available from: http://www.english.scfhs.org.sa/Book/T.bdf.2010/SB.21.pdf .
- 14.McNair DM, Lorr M, Droppleman LF. Manual for the profile of mood states. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 15.McNair DM, Lorr M, Droppleman LF. Revised manual for the profile of mood states. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 16.Nyenhuis DL, Yamamoto C, Luchetta T, Terrien A, Parmentier A. Adult and geriatric normative data and validation of the profile of mood states. J Clin Psychol. 1999;55:79–86. doi: 10.1002/(sici)1097-4679(199901)55:1<79::aid-jclp8>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 17.Curranv SL, Shelly L, Andrykowski MA, Michael A, Studts JL, Jamie L. Short form of the profile of mood states (POMS-SF): Psychometric information. Psychol Assess. 1995;7:80–3. [Google Scholar]
- 18.Mitler MM, Miller JC. Methods of testing for sleepiness [corrected] Behav Med. 1996;21:171–83. doi: 10.1080/08964289.1996.9933755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: A new approach. Psychophysiology. 1973;10:431–6. doi: 10.1111/j.1469-8986.1973.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 20.Stanford Sleepiness Scale. [Last accessed on 2010 Oct 01]. Available from: http://www.stanford.edu/~dement/sss.html .
- 21.Goitein L, Shanafelt TD, Wipf JE, Slatore CG, Back AL. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165:2601–6. doi: 10.1001/archinte.165.22.2601. [DOI] [PubMed] [Google Scholar]
- 22.Estabrooks CA, Cummings GG, Olivo SA, Squires JE, Giblin C, Simpson N. Effects of shift length on quality of patient care and health provider outcomes: Systematic review. Qual Saf Health Care. 2009;18:181–8. doi: 10.1136/qshc.2007.024232. [DOI] [PubMed] [Google Scholar]
- 23.Parshuram CS, Dhanani S, Kirsh JA, Cox PN. Fellowship training, workload, fatigue and physical stress: A prospective observational study. CMAJ. 2004;170:965–70. doi: 10.1503/cmaj.1030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296:1055–62. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 25.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–34. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 26.Marcus CL, Loughlin GM. Effect of sleep deprivation on driving safety in housestaff. Sleep. 1996;19:763–6. doi: 10.1093/sleep/19.10.763. [DOI] [PubMed] [Google Scholar]
- 27.Wilhelm BJ, Widmann A, Durst W, Heine C, Otto G. Objective and quantitative analysis of daytime sleepiness in physicians after night duties. Int J Psychophysiol. 2009;72:307–13. doi: 10.1016/j.ijpsycho.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Reddy R, Guntupalli K, Alapat P, Surani S, Casturi L, Subramanian S. Sleepiness in medical ICU residents. Chest. 2009;135:81–5. doi: 10.1378/chest.08-0821. [DOI] [PubMed] [Google Scholar]
- 29.Accreditation Council for Medical Education Common Program requirements. [Last accessed on 2008 Oct 10]. Available from: http://www.acgme.org/acWebsite/dutyIIours/dh_dutyIIoursCommonPR.Pdf .
- 30.Reed DA, Fletcher KE, Arora VM. Protected sleep time, and night float with patient care, residents’ health, and education: Systematic review. Ann Intern Med. 2010;153:829–42. doi: 10.7326/0003-4819-153-12-201012210-00010. [DOI] [PubMed] [Google Scholar]
- 31.Moonesinghe SR, Lowery J, Shahi N, Millen A, Beard JD. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients’ outcomes: Systematic review. BMJ. 2011;342:d1580. doi: 10.1136/bmj.d1580. [DOI] [PubMed] [Google Scholar]
- 32.Fletcher KE, Davis SQ, Underwood W, Mangrulkar RS, McMahon LF, Saint S. Systematic review: Effects of resident work hours on patient safety. Ann Intern Med. 2004;141:851–7. doi: 10.7326/0003-4819-141-11-200412070-00009. [DOI] [PubMed] [Google Scholar]
- 33.Landrigan CP, Barger LK, Cade BE, Ayas NT, Czeisler CA. Interns’ compliance with accreditation council for graduate medical education work-hour limits. JAMA. 2006;296:1063–70. doi: 10.1001/jama.296.9.1063. [DOI] [PubMed] [Google Scholar]
- 34.Puvanendran K, Venkatramani J, Jain A, Farid M. Sleep deprivation in junior doctors–house officers in Singapore. Ind Health. 2005;43:129–32. doi: 10.2486/indhealth.43.129. [DOI] [PubMed] [Google Scholar]


